Abstract
Hip arthroplasty in young patients requires thoughtful preoperative planning. Patients with proximal femoral bone loss complicate this planning and may require a staged procedure to optimize implant insertion. We report on a case of a 26-year-old woman with secondary hip arthritis from developmental dysplasia of the hip and a large pertrochanteric bone cyst that was treated with staged total hip arthroplasty. The cyst was decompressed and filled with an osteoconductive and osteoinductive bone graft substitute called EquivaBone. One year later, the patient underwent a successful primary total hip arthroplasty. Fifteen-month follow-up after her hip replacement revealed resolution of postoperative pain and significant functional improvement.
Keywords: Hip arthroplasty in young patients, Equivabone, Bone graft substitute, Bone cyst, Staged primary total hip arthroplasty
Introduction
Total hip arthroplasty (THA) became popularized in the 1960s by Sir John Charnley for the purpose of relieving pain and restoring function in elderly patients with degenerative hip arthritis 1, 2. Over time, the indications have broadened to include young adults with severe degenerative changes secondary to various pediatric hip disorders; in these patients, success rates are excellent 3, 4, 5, 6, 7, 8, 9. When performing arthroplasty in this young patient population, the treating surgeon must consider the need for eventual revision arthroplasty, as younger age and higher activity are thought to contribute to increased wear and risk of revision surgery 8, 9. An ideal implant in this young patient population would be a proximally loading tapered femoral stem, as it avoids proximal stress shielding and allows for preservation of more distal bone stock should revision surgery be required [10]. However, fundamental to the stability of this type of implant is strong metaphyseal bone that would allow for rigid fixation and biologic ingrowth 10, 11.
We present a case of a 26-year-old female with severe secondary hip arthritis due to developmental hip dysplasia, who presents with a slowly enlarging pertrochanteric bone cyst. The lesion was decompressed and filled with a new biological bone graft substitute, EquivaBone (ETEX, Cambridge, MA), to allow for restoration of bone stock in her proximal femur as part of a staged THA.
Case history
The patient first presented to adult reconstruction clinic seeking evaluation for a left hip pain at the age of 23 years. The patient provided full consent for use of this case for research purposes and publication. She has history of developmental dysplasia of her left hip, which was first dislocated at the age of 4 months. She also has a positive family history of Legg-Calve-Perthes disease. Before the age of 6 months, she underwent open reduction and hip spica casting, which was successful in obtaining a reduction. However, at the age of 3, a Salter osteotomy was performed to provide improved femoral head coverage for her dysplastic hip. She did relatively well for several years but began having increasing amounts of hip pain during daily activity in her mid- to late-teenage years. She was indicated for a periacetabular osteotomy (PAO) at the age of 20 years. A left hip arthroscopy was performed before this to evaluate the integrity of her cartilage, which was found to be so damaged that the PAO was aborted. She was told there were no other surgical options for her left hip short of an arthroplasty or arthrodesis.
When seen in our clinic at the age of 23, she had functional hip pain with most daily activities. On physical examination, her left leg was approximately 1-cm shorter than her right by block testing. She had a 15 degree left hip flexion contracture, with passive range of motion to 95 degrees flexion, 10 degrees external rotation, and 5 degrees internal rotation. Radiographs at this time (Fig. 1a) showed markedly aspherical left femoral head and an eroded acetabular articular surface with severe joint space narrowing, subchondral sclerosis, and cysts, with underlying acetabular dysplasia and postosteotomy deformity. Notably, lateral center-edge ankle of the left hip measured 0 degrees. Her right hip was also mildly dysplastic with a lateral center-edge angle of 23 degrees; however, she reported no pain so no further work-up or intervention was pursued.
Figure 1.
Serial anteroposterior and lateral left hip radiographs reveal aspherical left femoral head and an eroded acetabular articular surface with severe joint space narrowing, subchondral sclerosis and cysts, and underlying acetabular dysplasia and postosteotomy deformity. The images, in order from left to right, were taken when the patient was 23 years old (a), 25 years old (b), and 26 years old (c; 9 months after cyst curretage and grafting). The pertrochanteric cyst appeared to show graft incorporation and osseous remodeling of her proximal femoral metaphysis.
It was discussed that her gender and dysplastic anatomy make her a poor candidate for hip resurfacing given her higher risk of complications. A PAO was again considered an option but a magnetic resonance arthrogram obtained several weeks later (Fig. 2) demonstrated significant chondral damage on both the femoral and acetabular surfaces as well as a large pertrochanteric simple bone cyst. She was thus instructed that her best surgical option would be a THA but that she should delay as long as possible due to the high likelihood of requiring revision surgery during her life. The patient agreed to pursue our conservative treatment plan as long as she could tolerate the pain.
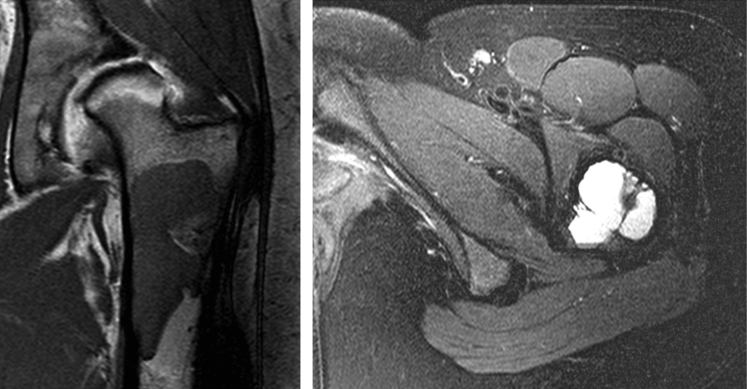
Figure 2.
Coronal T1 and axial T2 images of an magnetic resonance arthrogram demonstrating a large bone cyst measuring 8 × 3 × 3 cm in the proximal femur. MRA, magnetic resonance arthrogram.
Over the next 2 years she had slowly progressive pain and increased functional limitations, walking with a Trendelenburg gait. She had several intra-articular corticosteroid injections that provided moderate relief for 2-4 months but with diminishing returns as she progressed. Serial radiographs demonstrated progression of her pertrochanteric bone cyst (Fig. 1b). Several discussions had occurred regarding this cyst affecting the quality of proximal femoral bone stock. The concern was that her abnormal osseous architecture would not be strong enough to support a proximally loading femoral implant and that she would require a fully porous coated implant with diaphyseal fixation. Although a suitable choice of fixation, this type implant is less ideal as it would threaten more significant bone loss should she ever require revision of her femoral component, which was highly likely given her age. Because she was interested in undergoing a THA in the near future, the decision was made to undergo cyst decompression and a bone grafting procedure to restore the osseous integrity of her proximal femur as the first part of a staged arthroplasty.
In June 2011, she underwent curettage and bone grafting of her pertrochanteric cyst, which measured 8 × 3 × 3 centimeters. A burr was used to make a small lateral cortical window, to which a curette was inserted and used for cyst decompression. Subsequently, 40 cc of EquivaBone, an osteoconductive and osteoinductive bone graft substitute, was then injected into the defect. This procedure went without complication.
She was closely followed at regular clinic visits with repeat radiographs to evaluate for osseous incorporation of EquivaBone into the previous lesion. She was ambulating pain free without an assistive device several weeks after her procedure, reporting improved functional abilities when compared to before her surgery. Radiographs at 9 months postoperatively showed bone graft incorporation and osseous remodeling in her left pertrochanteric region (Fig. 1c). As time progressed, her left hip became more symptomatic and she was indicated to undergo THA with an uncemented proximally loading femoral implant.
THA was performed in June 2012 through a posterior approach using standard primary arthroplasty implants (Zimmer Continuum acetabular shell, Zimmer trabecular metal femoral stem with standard offset, and Biolox delta ceramic femoral head). During the operation, the acetabulum was found to have severe superolateral bone loss from the pseudosubluxation and coxa magna of the femoral head. To optimize bony contact with the acetabular implant, the cup was placed in a slightly more vertical position than typically desired. The abduction angle measures 60 degrees from the horizontal. This cup position may predispose to increased polyethylene wear due to the potential for edge loading; however, a 10 degree elevated hood liner was placed superolaterally to mitigate this risk.
After the femoral neck cut was made and on investigation of the medullary bone, complete ingrowth of the EquivaBone (placed 1 year prior) was achieved. The cancellous bone was more dense than usual and there was some difficulty passing the canal finder, although it was still safely accomplished under manual pressure. Based on the postoperative radiographs, the femoral component does appear to be undersized on the anteroposterior view, but we believe this is due to the underlying proximal femoral dysplasia. After final broaching and placement of the implant, a strong press fit was accomplished with medial calcar contact, and there was excellent torsional stability. On the lateral radiograph, the component appears to be well sized within the femur.
Within 2 months post THA and 14 months after bone grafting of the metaphyseal cyst, she was completely pain free in her left hip and able to walk several miles without pain. Four months after THA and 16 months after bone grating, the patient continued to progress well and was able to work out at her gym, reporting only minimal discomfort with leg presses. She was 4 weeks pregnant at this visit; however, she was unaware that she had conceived. Radiographs showed a well positioned implant with evidence of osseous integration into the implant, without subsidence or signs of osteolysis (Fig. 3a). Her hip flexion contracture had resolved and hip range of motion was painless, ranging from 0 degrees extension to 120 degrees flexion, 40 degrees internal rotation, and 30 degrees external rotation.
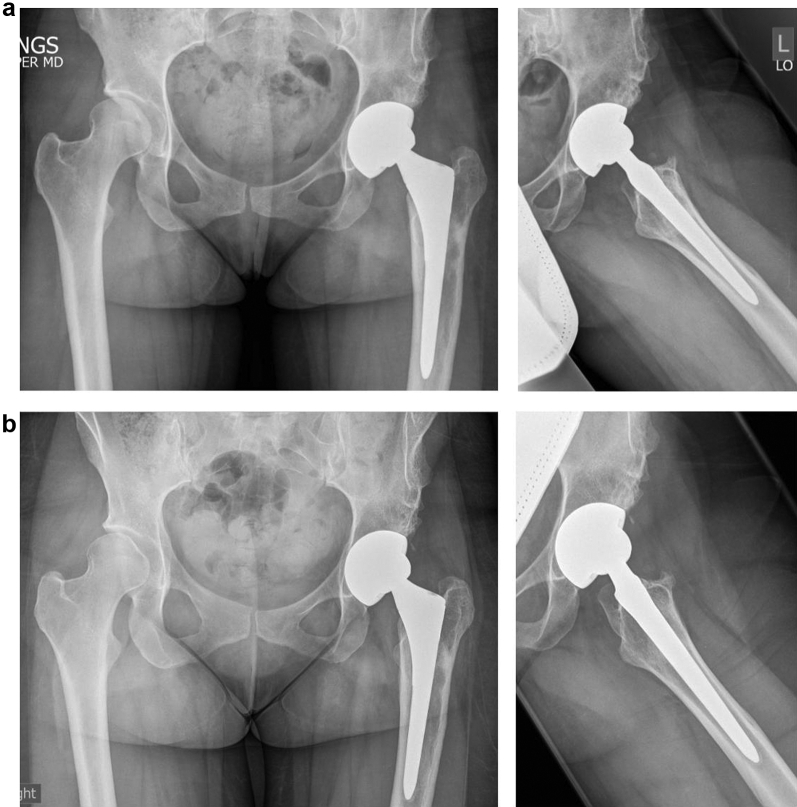
Figure 3.
Anteroposterior pelvis and frog-leg lateral left hip (a) taken 4 months after THA and (b) 15 months after her THA. Radiographs demonstrate evidence of component integration without subsidence or signs of osteolysis.
At 15 months after her THA and 2 months post partum with an uncomplicated vaginal delivery, her left hip remained pain free. She reported no problems with her hip and felt that she was not limited in any way. Her Trendelenburg gait had resolved and her range of motion was 0 degrees hip extension, 100 degrees of flexion, 50 degrees internal rotation, 40 degrees of external rotation. Her Harris Hip Score was 100. Radiographs revealed a stable implant, unchanged from prior imaging (Fig. 3b). The plan is to follow her every 2 years for surveillance.
Discussion
THA has been successfully used in young adults for multiple end-stage pediatric hip disorders including osteonecrosis, inflammatory arthroses, post-traumatic arthritis, developmental hip dysplasia, Legg-Calve-Perthes disease, slipped capital femoral epiphysis, multiple epiphyseal dysplasia, and several other conditions 3, 4, 5, 6, 7, 8, 9. However, when planning the primary arthroplasty, surgeons should consider multiple factors with respect to the need for future revision surgery during the patient’s lifetime: implant material, bearing surface, bone quality, and so forth. One additional factor is the preservation of remaining femoral and acetabular bone stock, which is commonly abnormal and/or deficient in these pediatric deformities.
Use of a proximally loading femoral stem is advantageous for several reasons. According to Wolfe's law, increases in load result in maintenance of bone mass and an increase in the qualitative and quantitative bone properties. Thus, a proximally loading implant with rigid fixation maintains the proximal bone stock and avoids proximal stress shielding, osteopenia, and bone resorption 10, 12. In addition, it obviates the need for diaphyseal fixation, which not only leads to the aforementioned problem of proximal stress shielding but can result in significant iatrogenic bone loss during implant removal in the setting of revision surgery. A requirement for a proximally loading femoral stem is adequate proximal bone stock to allow for rigid fixation and biologic ingrowth. This concept of initial rigid fixation is well established in the arthroplasty literature, with a goal of <50 microns of micromotion at the implant—cortical bone interface 10, 11, 12. Fixation of this strength allows osseous ingrowth and provides stability against the axial and rotational forces of daily living and leads to a greater likelihood of successful arthroplasty. However, use of a proximally loading implant in a femur with insufficient osseous integrity would have a greater risk of increased stem micromotion, fibrous ingrowth, instability to torsional and axial forces, and eventual implant failure.
The case presented in this report is a young adult with inadequate proximal bone stock due to a large bone cyst. THA with an uncemented, proximally loading stem would be at high risk of failure in this setting, as her bone quality would likely be unable to provide for stable, biologic fixation against the forces acting on it. We, therefore, had to fill her osseous defect and to allow future successful arthroplasty implantation.
In the presence of osseous defects during hip arthroplasty, the surgeon can choose to fill the void with autograft, allograft chips, or one of several bone graft substitutes. Each has its own advantages and disadvantages, with varying amounts of strength and osteogenic potential 10, 13, 14. The ideal graft would have a combination of both osteoconductive and osteoinductive properties and would allow for restoration of osseous architecture for future ingrowth into the arthroplasty component. Much research has focused on the use of morselized bone graft, with or without augmentation of bioceramics such as hydroxyapatite or tricalciumphosphate, in cases of femoral or acetabular component revision arthroplasty 10, 15, 16, 17, 18. However, there is little information on the efficacy and use of bone graft or bone graft substitute to restore bone stock for primary THA.
EquivaBone (ETEX) is a new US Food and Drug Administration–approved hard-setting osteoinductive bone graft substitute combined with an osteoconductive nanocrystalline calcium phosphate scaffold. Its composition of calcium phosphate provides a stable matrix that is gradually remodeled in a manner similar to bone remodeling through osteoclast resorption [19]. When compared to cancellous bone grafts and other bone graft substitutes, calcium phosphate is known to have a much higher compressive strength which provides stable fixation [19]. However, it has unique osteoinductive properties as well, which signal host stem cells to differentiate along osteoblastic lines 19, 20. Because of these properties, we used this bone graft substitute to fill the cystic cavity in the proximal femur, as we felt it would provide the best opportunity for osseous regrowth. And as expected, radiographs over the next year showed remodeling of her proximal femur and bone graft incorporation, strong enough to support THA with a proximally loading, tapered femoral stem just one year later.
Summary
Proximal femoral bone loss is a complicated problem for patients planning to undergo hip replacement. This is compounded in young patients where the use of proximally loaded press fit femoral stems are greatly preferred due to their biomechanical properties and risk of future revision. To our knowledge, this is the first description of EquivaBone in the arthroplasty literature. Based on its biological and mechanical properties, and successful use in this case report, we feel that EquivaBone merits further study as a potential bone graft substitute in cases of THA. Future studies with a larger number of patients, long-term follow-up, and osseous defects in a variety of acetabular and femoral locations should be evaluated.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.03.002.
Appendix A. Supplementary data
References
- 1.Charnley J. Total hip replacement. JAMA. 1974;230:1025. [PubMed] [Google Scholar]
- 2.Siopack J.S., J H. Total hip arthroplasty. West J Med. 1995;162:243. [PMC free article] [PubMed] [Google Scholar]
- 3.Pavone V., Costarella L., Privitera V., Sessa G. Bilateral total hip arthroplasty in subjects with multiple epiphyseal dysplasia. J Arthroplasty. 2009;24:868. doi: 10.1016/j.arth.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Costa C., Johnson A.J., Mont M.A. Use of cemented, tapered femoral stems in patients who have a mean age of 20 years. J Arthroplasty. 2012;27:497. doi: 10.1016/j.arth.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Bilsel N., Gokce A., Kesmezacar H. Long-term results of total hip arthroplasty in patients with juvenile rheumatoid arthritis. Acta Orthop Traumatol Turc. 2008;42:119. doi: 10.3944/aott.2008.42.2.119. [DOI] [PubMed] [Google Scholar]
- 6.Restrepo C., Lettich T., Roberts N. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg. 2008;74:615. [PubMed] [Google Scholar]
- 7.Kim Y.H., Park J.W., Kim J.S. Cementless metaphyseal fitting anatomic total hip arthroplasty with a ceramic-on-ceramic bearing in patients thirty years of age or younger. J Bone Joint Surg Am. 2012;94A:1570. doi: 10.2106/JBJS.K.00697. [DOI] [PubMed] [Google Scholar]
- 8.Kitsoulis P.B., Stafilas K.S., Siamopoulou A. Total hip arthroplasty in children with juvenile chronic arthritis: long term results. J Pediatr Orthop. 2006;26:8. doi: 10.1097/01.bpo.0000187997.84213.d9. [DOI] [PubMed] [Google Scholar]
- 9.Chmell M.J., Scott R.D., Thomas W.H. Total hip arthroplasty with cement for juvenile rheumatoid arthritis: results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am. 1997;79A:44. doi: 10.2106/00004623-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Callaghan J.J., Rosenberg A.G., Rubash H.E., editors. The adult hip. 2nd Edition. Lippincott Williams & Wilkins; Philadelphia, PA: 2007. [Google Scholar]
- 11.Jasty M., Bragdon C., Burke D. In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Joint Surg Am. 1997;79A:707. doi: 10.2106/00004623-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Otani T., W L. Failure of cementless fixation of the femoral component in total hip arthroplasty. Orthop Clin North Am. 1992;23:335. [PubMed] [Google Scholar]
- 13.Barrack R.L. Bone graft extenders, substitutes, and osteogenic proteins. J Arthroplasty. 2005;20(Supp 2):94. doi: 10.1016/j.arth.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 14.Gazdag A.R., Lane J.M., Glaser D., Forster R.A. Alternatives to autogenous bone graft: efficacy and indications. J Am Acad Orthop Surg. 1995;3:1. doi: 10.5435/00124635-199501000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Bolder S.B., Verdonschot N., Schreurs B.W., Buma P. The initial stability of cemented acetabular cups can be augmented by mixing morsellized bone grafts with tricalciumphosphate/hydroxyapatite particles in bone impaction grafting. J Arthroplasty. 2003;18:1056. doi: 10.1016/s0883-5403(03)00408-x. [DOI] [PubMed] [Google Scholar]
- 16.Howie D.W., McGee M.A., Callary S.A. A preclinical study of stem subsidence and graft incorporation after femoral impaction grafting using porous hydroxyapatite as a bone graft extender. J Arthroplasty. 2011;26:1050. doi: 10.1016/j.arth.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Oshima S., Yasunaga Y., Yamasaki T. Midterm results of femoral impaction bone grafting with an allograft combined with hydroxyapatite in revision total hip arthroplasty. J Arthroplasty. 2012;27:470. doi: 10.1016/j.arth.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 18.de Roeck N.J., Drabu K.J. Impaction bone grafting using freeze-dried allograft in revision hip arthroplasty. J Arthroplasty. 2001;16:201. doi: 10.1054/arth.2001.20250. [DOI] [PubMed] [Google Scholar]
- 19.Hak D.J. The use of osteoconductive bone graft substitutes in orthopaedic trauma. J Am Acad Orthop Surg. 2007;15:525. doi: 10.5435/00124635-200709000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Grabowski G., Cornett C.A. Bone graft and bone graft substitutes in spine surgery: current concepts and controversies. J Am Acad Orthop Surg. 2013;21:51. doi: 10.5435/JAAOS-21-01-51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.