Abstract
In April 2015, the Division of Microbiology and Infectious Diseases of the National Institute of Allergy and Infectious Diseases hosted an experts technical consultation on bacterial vaginosis (BV), where data regarding controversies over the pathogenesis of BV were discussed. The discussion on the epidemiology and pathogenesis of BV is presented here, and several hypotheses on its pathogenesis are critiqued. Rigorous hypothesis-driven studies are needed to ultimately determine the cause of BV. This information is vital for the prevention and control of this important infection and its adverse public health consequences.
Keywords: bacterial vaginosis, Gardnerella, vaginal flora
Bacterial vaginosis (BV) is the most common vaginal infection worldwide and is associated with important public health issues, such as preterm labor and the acquisition and transmission of sexually transmitted infections (STIs) and human immunodeficiency virus [1–3]. Despite its public health importance, however, the pathogenesis of BV remains unclear, so much so that some refer to this condition not as an infection but rather as a dysbiosis, a microbial imbalance in the vaginal flora that can precipitate changes in the normal activities of the vagina [4, 5]. BV is characterized by a shift from a lactobacillus-predominant vaginal flora to one in which the lactobacilli dramatically decline and facultative and strict anaerobes abound [6]. Despite this dramatic shift, some women with BV do not experience symptoms [7, 8]. There is agreement that the shift away from an optimal vaginal flora consisting of lactobacilli is the biological risk factor for associated adverse outcomes of BV. Disagreement exists, however, as to how this change comes about—is it the introduction of single or multiple pathogens or do other factors lead to the “overgrowth” of BV-associated anaerobes? Determining the trigger for the development of BV is crucial to improving the treatment, management, and prevention of this important condition. In this review, we present various current hypotheses for the pathogenesis of BV that have been discussed over the years.
HYPOTHESIS: RACIAL AND SOCIETAL DIFFERENCES CAUSE INHERENT DIFFERENCES IN THE VAGINAL FLORA
Rates of BV are higher in underserved minority populations [9]. This has led some to consider that vaginal flora patterns may be influenced by genetics and race [10, 11]. Although in one study vaginal pH was found to be higher in pregnant African American women than in pregnant white women [12], this difference was probably confounded by the higher rates of BV in the African American women [13]. In a study comparing African American women with those of European ancestry, with or without BV, significant differences were found in the vaginal microbiota. Women of European ancestry without BV were more likely to have a lactobacillus-predominant vaginal flora, whereas African American women were more likely to have a vaginal microbiota composed of a variety of strict anaerobes, including Anaerococcus, BV-associated bacterium (BVAB) 1, BVAB2, Dialister, Peptoniphilus, Coriobacteriaceae, Parvimonas, Megasphaera, Sneathia, Prevotella amnii, Atopobium, and Gardnerella vaginalis. Comparison of subjects with BV revealed that African American women were more likely to be colonized by BVAB1 and BVAB3, Gemella, Bulleidia, Dialister, and Sneathia, whereas those of European ancestry were more likely to be colonized by Mycoplasma hominis and Corynebacterium. In this study, women were screened for BV only if they reported symptoms. Thus, women with asymptomatic BV may have been included in the group of women “without BV” [14].
Investigators have also examined societal factors associated with BV among minority women in the United States, notably socioeconomic status and psychosocial stress, without definitive conclusions [15]. Nutritional factors have also been implicated in the development of BV. Neggers et al [16] showed a significant relationship between dietary fat intake and BV and an inverse relationship of BV with folate, vitamin E, and calcium. Thus, it is possible that high-fat diets, which are common in populations of lower socioeconomic status, could help explain racial differences in BV rates.
It is also possible that the concept of sexual networks may explain the racial disparity of BV prevalence if BV is an STI (see below in “Hypothesis: BV is an STI”) [17, 18]. Peipert et al [18] evaluated whether the association of BV and incident STI was modified by race, even after adjustment for sexual practices and other potential confounding variables. They found that race and the presence of BV seemed to act synergistically to increase the risk of STI acquisition. Similarly, Klebanoff et al [19] found a significant association with sexual partner race and BV; white women with African American male partners had a 2-fold increased risk of BV compared with white women with white male sex partners. Paternal black race has also been found to be associated with BV in pregnancy [20]. These findings suggest that BV risk is influenced by sexual networks and may explain the association of BV with being African American.
HYPOTHESIS: INTRAVAGINAL PRACTICES ARE TRIGGERS FOR BV DEVELOPMENT
Numerous intravaginal practices have been suggested as triggers for the development of BV by causing disruption of the normal vaginal flora. These include exposure to alkaline semen, tampon use, douching, soaps, cloths, herbs, and flowers [21, 22]. Exposure to semen with its pH of 7.2 has been hypothesized to alter the normally acidic pH of the vaginal secretions and encourage the growth of BVAB. However, many women have frequent exposure to semen and do not develop BV, so, it could be reasoned that this might be a cofactor along with other exposures. On the other hand, a case report of heterosexual transmission of BV without semen exposure [23] and the high prevalence of BV in women who have sex with women [24, 25] cast doubt on this hypothesis. Intravaginal product use, other than douching, as well as other hygiene practices, including use of pads, panty liners, sprays, powders, and towelettes were not related to the development of BV, as shown in a large longitudinal study of vaginal flora [26].
Douching has been found to be significantly associated with BV in cross-sectional and longitudinal studies [27–30]. However, in most of these studies women reported douching for symptoms or hygiene, making it difficult to establish cause-and-effect relationships. Douching is also strongly linked to sexual behavior, again leading to confounding [30]. Brotman et al [31] used a marginal structural model, which assumes the absence of unmeasured confounding, and found that douching was associated with BV; however, they commented that the model may not completely account for all covariates. In a prospective study of douching stratified by intermediate/abnormal versus normal vaginal flora, douching was associated with the development of BV only among women with intermediate vaginal flora. Furthermore, douching was not associated with acquisition of BVAB among women without evidence of BVAB at baseline [32]. Thus, douching may be a cofactor in the development of BV but is probably not the inciting factor. Because it is not clear that douching causes BV or pelvic inflammatory disease (which has also been suggested), conducting a prospective study of women with normal vaginal flora randomized to douching versus observation could be considered, but the ethical implications of such a study would need to be carefully considered.
HYPOTHESIS: BV IS AN STI
The majority of epidemiologic data support the hypothesis that BV is a STI [33]. The most significant risk factor for incident BV is a new sexual partner [27, 34], and for recurrent or persistent BV it is sex with the same partner [35]. Additional support for the sexual transmission of BV can be found in studies in which the use of condoms was protective against BV. Sanchez et al [36] found that rates of recurrent BV after BV treatment were significantly higher among women who resumed unprotected sex than in those who were abstinent or used condoms. Prospective studies of vaginal flora patterns have confirmed that consistent condom use significantly decreased the incidence and prevalence of BV, especially among those women with normal vaginal flora at baseline [19, 37, 38].
A few studies have found BV or G. vaginalis (a bacterium highly associated with BV) in virginal girls. However, these studies were based on self-report of sexual activity from this vulnerable population of young women and lacked investigation into potential biomarkers of unprotected sex with male partners (eg, Y chromosome or prostate-specific antigen) or a history of sex with female partners [39, 40]. Although previous studies have failed to find a significant effect of treatment of the male sexual partner on women with recurrent BV, a 2012 meta-analysis demonstrated design flaws in these older studies [41]. New phase 3 clinical trials are needed that overcome the methodologic flaws of prior studies.
Assuming that sexual transmission plays a key role in the pathogenesis of BV, the next question concerns the transmitted pathogen(s). Decades ago, Gardner and Dukes [42] postulated that Haemophilus vaginalis (now Gardnerella vaginalis) was the pathogen that causes BV. With improvement in anaerobic culture, it was shown that multiple anaerobic bacteria were also associated with BV [43]. More recently it was shown that previously unrecognized, unculturable bacteria are also part of the BV flora [44]. Although it is highly likely that anaerobes contribute to the symptoms of BV, there has been renewed interest in the hypothesis that G. vaginalis is the inciting pathogen, with studies confirming its virulence factors (ability to adhere to host receptor sites on vaginal epithelial cells, production of cytotoxic substances specific for host cells, and biofilm formation) as well as its concordance in sexual partners [45–47].
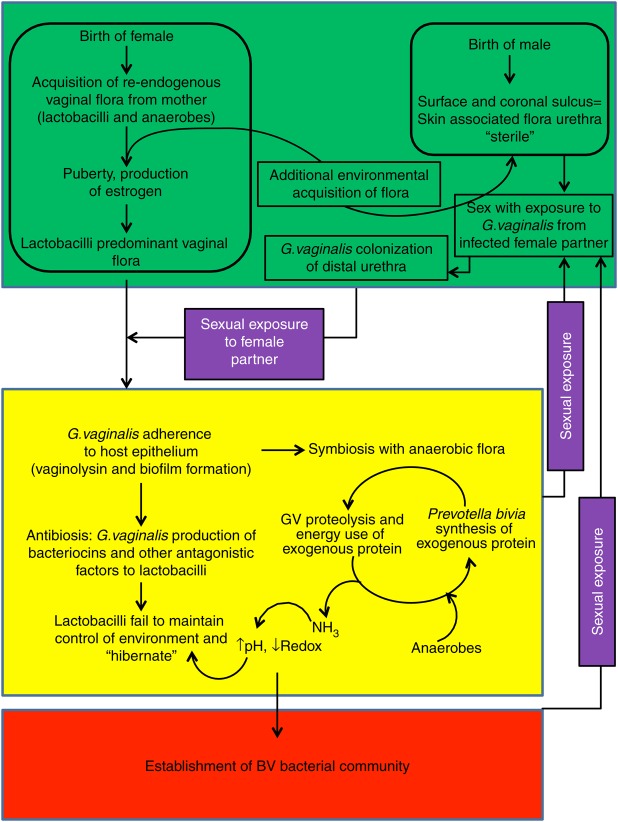
In 2014, Schwebke et al [48] presented a conceptual model for the pathogenesis of BV with G. vaginalis as the founder or keystone pathogen (Figure 1). Similar to the involvement of facultative anaerobes in the initiation of oral disease [49], it is possible that G. vaginalis, through its metabolic pathways and ability to form a biofilm, lowers the reduction-oxidation potential in the vaginal microbiome. This alteration would then cause a marked decrease in lactobacilli and an increase in other BVAB, acquired shortly after birth from maternal and environmental sources [50] and normally present in very low concentrations, leading to the BV syndrome. This model is in keeping with the current model for periodontal disease in which keystone pathogens are aided by accessory pathogens (commensal bacteria that are not pathogenic by themselves in a given niche but can enhance the virulence of keystone pathogens) [4]. This synergistic relationship creates the dysbiosis characteristic of periodontal disease, and a similar scenario might also explain BV.
Figure 1.
As depicted in the model, Gardnerella vaginalis is not part of the normal vaginal flora acquired at birth but is transmitted through sexual activity with an infected partner. It has the necessary virulence factors to adhere to host vaginal epithelium and successfully compete with normal vaginal flora for dominance. Infection with G. vaginalis results in increased pH and decreased reduction-oxidation (redox) potential, favoring increased growth of host anaerobes and suppression of lactobacilli. Reproduced with permission from Schwebke et al [48]. Abbreviations: BV, bacterial vaginosis; NH3, ammonia.
Others have hypothesized that BV is caused by a polymicrobial consortium of microorganisms [51]. Clue cells, sloughed epithelial cells from the microbial complex biofilm community of BV, have been shown to carry not only G. vaginalis but also a mixed array of anaerobes which vary among individuals [52]. This consortium of bacteria is thought to enhance the transmission of BV. Clue cells have been identified in male as well as female subjects [53].
Treatment of symptomatic women with BV is recommended [54]; however, despite initial response, BV recurs or persists in a significant proportion of women [35, 36, 55]. This is probably due to the persistence of the biofilm, which has been documented by vaginal biopsy after therapy with metronidazole [56] and moxifloxacin [57]. Alternative approaches to BV treatment, which target the biofilm, are needed [58].
CONCLUSIONS
Unraveling the mystery of BV pathogenesis is essential if we are to make progress in the control and prevention of this common, important condition. Epidemiologic data strongly support the sexual transmission of BV. As with other STIs, sexual networks could help explain the racial disparities noted in women with BV. Similarities between the pathogenesis of periodontitis and BV are striking and may help guide future research concerning microbial interactions in BV. Establishment of conceptual models with testable hypotheses is needed, as well as animal models in which to test them. Bench researchers and clinicians should work closely together on these projects, because both bring needed perspective and unique knowledge to the table. The time is right to solve this important public health problem.
Notes
Supplement sponsorship. This article appears as part of the supplement “Proceedings of the 2015 NIH/NIAID Bacterial Vaginosis Expert Consultation,” sponsored by the Division of Microbiology and Infectious Diseases of the National Institute of Allergy and Infectious Diseases in partnership with the University of Alabama at Birmingham Sexually Transmitted Infections Clinical Trials Group; contract HHSN272201300012I.
Potential conflict of interest. Both authors: No potential conflicts of interest. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Eschenbach DA. Bacterial vaginosis and anaerobes in obstetric-gynecologic infection. Clin Infect Dis 1993; 16(suppl 4):S282–7. [DOI] [PubMed] [Google Scholar]
- 2.Hillier SL, Nugent RP, Eschenbach DA et al. Vaginal Infections and Prematurity Study Group. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. N Engl J Med 1995; 333:1737–42. [DOI] [PubMed] [Google Scholar]
- 3.Hillier S. The vaginal microbiol ecosystem and resistance to HIV. AIDS 1998; 14:17–21. [PubMed] [Google Scholar]
- 4.Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol 2015; 15:30–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson TM, Borgogna JL, Brotman RM, Ravel J, Walk ST, Yeoman CJ. Vaginal biogenic amines: biomarkers of bacterial vaginosis or precursors to vaginal dysbiosis? Front Physiol 2015; 6:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hillier SL. Diagnostic microbiology of bacterial vaginosis. Am J Obstet Gynecol 1993; 169:455–9. [DOI] [PubMed] [Google Scholar]
- 7.Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol 1988; 158:819–28. [DOI] [PubMed] [Google Scholar]
- 8.Klebanoff MA, Schwebke JR, Zhang J, Nansel TR, Yu KF, Andrews WW. Vulvovaginal symptoms in women with bacterial vaginosis. Obstet Gynecol 2004; 104:267–72. [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg RL, Klebanoff MA, Nugent R, Krohn MA, Hillier S, Andrews WW; Vaginal Infections and Prematurity Study Group. Bacterial colonization of the vagina during pregnancy in four ethnic groups. Am J Obstet Gynecol 1996; 174:1618–21. [DOI] [PubMed] [Google Scholar]
- 10.Newton ER, Piper JM, Shain RN, Perdue ST, Peairs W. Predictors of the vaginal microflora. Am J Obstet Gynecol 2001; 184:845–55. [DOI] [PubMed] [Google Scholar]
- 11.Ness RB, Hillier S, Richter HE et al. Can known risk factors explain racial differences in the occurrence of bacterial vaginosis? J Natl Med Assoc 2003; 95:201–12. [PMC free article] [PubMed] [Google Scholar]
- 12.Royce RA, Jackson TP, Thorp JM Jr et al. Race/ethnicity, vaginal flora patterns, and pH during pregnancy. Sex Transm Dis 1999; 26:96–102. [DOI] [PubMed] [Google Scholar]
- 13.Fiscella K, Klebanoff MA. Are racial differences in vaginal pH explained by vaginal flora? Am J Obstet Gynecol 2004; 191:747–50. [DOI] [PubMed] [Google Scholar]
- 14.Fettweis JM, Brooks JP, Serrano MG et al. Differences in vaginal microbiome in African American women versus women of European ancestry. Microbiol 2014; 160:2272–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paul K, Boutain D, Manhart L, Hitti J. Racial disparity in bacterial vaginosis: the role of socioeconomic status, psychosocial stress, and neighborhood characteristics, and possible implications for preterm birth. Soc Sci Med 2008; 67:824–33. [DOI] [PubMed] [Google Scholar]
- 16.Neggers YH, Nansel TR, Andrews WW et al. Dietary intake of selected nutrients affects bacterial vaginosis in women. J Nutr 2007; 137:2128–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothenberg R. Maintenance of endemicity in urban environments: a hypothesis linking risk, network structure and geography. Sex Transm Infect 2007; 83:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peipert JF, Lapane KL, Allsworth JE, Redding CA, Blume JD, Stein MD. Bacterial vaginosis, race, and sexually transmitted infections: does race modify the association? Sex Transm Dis 2008; 35:363–7. [DOI] [PubMed] [Google Scholar]
- 19.Klebanoff MA, Andrews WW, Zhang J et al. Race of male sex partners and occurrence of bacterial vaginosis. Sex Transm Dis 2010; 37:184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simhan HN, Bodnar LM, Krohn MA. Paternal race and bacterial vaginosis during the first trimester of pregnancy. Am J Obstet Gynecol 2008; 198:196 e1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallo MF, Warner L, King CC et al. Association between semen exposure and incident bacterial vaginosis. Infect Dis Obstet Gynecol 2011; 2011:842652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alcaide ML, Chisembele M, Malupande E, Arheart K, Fischl M, Jones DL. A cross-sectional study of bacterial vaginosis, intravaginal practices and HIV genital shedding; implications for HIV transmission and women's health. BMJ Open 2015; 5:e009036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muzny CA, Schwebke JR. Suspected heterosexual transmission of bacterial vaginosis without seminal fluid exposure. Sex Transm Dis 2014; 41:58–60. [DOI] [PubMed] [Google Scholar]
- 24.Marrazzo JM, Koutsky LA, Eschenbach DA, Agnew K, Stine K, Hillier SL. Characterization of vaginal flora and bacterial vaginosis in women who have sex with women. J Infect Dis 2002; 185:1307–13. [DOI] [PubMed] [Google Scholar]
- 25.Evans AL, Scally AJ, Wellard SJ, Wilson JD. Prevalence of bacterial vaginosis in lesbians and heterosexual women in a community setting. Sex Transm Infect 2007; 83:470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klebanoff MA, Nansel TR, Brotman RM et al. Personal hygienic behaviors and bacterial vaginosis. Sex Transm Dis 2010; 37:94–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawes SE, Hillier SL, Benedetti J et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 1996; 174:1058–63. [DOI] [PubMed] [Google Scholar]
- 28.Ness RB, Hillier SL, Richter HE et al. Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol 2002; 100:765. [DOI] [PubMed] [Google Scholar]
- 29.McClelland RS, Richardson BA, Graham SM et al. A prospective study of risk factors for bacterial vaginosis in HIV-1-seronegative African women. Sex Transm Dis 2008; 35:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwebke JR, Desmond RA, Oh MK. Predictors of bacterial vaginosis in adolescent women who douche. Sex Transm Dis 2004; 31:433–6. [DOI] [PubMed] [Google Scholar]
- 31.Brotman RM, Klebanoff MA, Nansel TR et al. A longitudinal study of vaginal douching and bacterial vaginosis—a marginal structural modeling analysis. Am J Epidemiol 2008; 168:188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hutchinson KB, Kip KE, Ness RB; Gynecologic Infection Follow-Through Investigators. Vaginal douching and development of bacterial vaginosis among women with normal and abnormal vaginal microflora. Sex Transm Dis 2007; 34:671–5. [DOI] [PubMed] [Google Scholar]
- 33.Fethers KA, Fairley CK, Hocking JS, Gurrin LC, Bradshaw CS. Sexual risk factors and bacterial vaginosis: a systematic review and meta-analysis. Clin Infect Dis 2008; 47:1426–35. [DOI] [PubMed] [Google Scholar]
- 34.Schwebke JR, Desmond R. Risk factors for bacterial vaginosis in women at high risk for sexually transmitted diseases. Sex Transm Dis 2005; 32:654–8. [DOI] [PubMed] [Google Scholar]
- 35.Bradshaw CS, Morton AN, Hocking J et al. High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J Infect Dis 2006; 193:1478–86. [DOI] [PubMed] [Google Scholar]
- 36.Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal metronidazole gel versus metronidazole plus nystatin ovules for bacterial vaginosis: a randomized controlled trial. Am J Obstet Gynecol 2004; 191:1898–06. [DOI] [PubMed] [Google Scholar]
- 37.Hutchinson KB, Kip KE, Ness RB. Condom use and its association with bacterial vaginosis and bacterial vaginosis-associated vaginal microflora. Epidemiol 2007; 18:702–8. [DOI] [PubMed] [Google Scholar]
- 38.Yotebieng M, Turner AN, Hoke TH, Van Damme K, Rasolofomanana JR, Behets F. Effect of consistent condom use on 6-month prevalence of bacterial vaginosis varies by baseline BV status. Trop Med Int Health 2009; 14:480–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bump RC, Buesching WJ III. . Bacterial vaginosis in virginal and sexually active adolescent females: evidence against exclusive sexual transmission. Am J Obstet Gynecol 1988; 158:935–9. [DOI] [PubMed] [Google Scholar]
- 40.Hickey RJ, Zhou X, Settles ML et al. Vaginal microbiota of adolescent girls prior to the onset of menarche resemble those of reproductive-age women. MBio 2015; 6:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mehta SD. Systematic review of randomized trials of treatment of male sexual partners for improved bacteria vaginosis outcomes in women. Sex Transm Dis 2012; 39:822–30. [DOI] [PubMed] [Google Scholar]
- 42.Gardner HL, Dukes CD. Haemophilus vaginalis vaginitis: a newly defined specific infection previously classified non-specific vaginitis. Am J Obstet Gynecol 1955; 69:962–76. [PubMed] [Google Scholar]
- 43.Spiegel CA, Amsel R, Eschenbach D, Schoenknecht F, Holmes KK. Anaerobic bacteria in non-specific vaginitis. N Engl J Med 1980; 303:601–7. [DOI] [PubMed] [Google Scholar]
- 44.Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med 2005; 353:1899–11. [DOI] [PubMed] [Google Scholar]
- 45.Patterson JL, Stull-Lane A, Girerd PH, Jefferson KK. Analysis of adherence, biofilm formation and cytotoxicity suggests a greater virulence potential of Gardnerella vaginalis relative to other bacterial-vaginosis-associated anaerobes. Microbiol 2010; 156:392–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Teixeira GS, Soares-Brandao KL, Branco KM et al. Antagonism and synergism in Gardnerella vaginalis strains isolated from women with bacterial vaginosis. J Med Microbiol 2010; 59:891–7. [DOI] [PubMed] [Google Scholar]
- 47.Eren AM, Zozaya M, Taylor CM, Dowd SE, Martin DH, Ferris MJ. Exploring the diversity of Gardnerella vaginalis in the genitourinary tract microbiota of monogamous couples through subtle nucleotide variation. PLoS One 2011; 6:e26732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schwebke JR, Muzny CA, Josey WE. Role of Gardnerella vaginalis in the pathogenesis of bacterial vaginosis: a conceptual model. J Infect Dis 2014; 210:338–43. [DOI] [PubMed] [Google Scholar]
- 49.Ruby J, Goldner M. Nature of symbiosis in oral disease. J Dent Res 2007; 86:8–11. [DOI] [PubMed] [Google Scholar]
- 50.Rotimi VO, Duerden BI. The development of the bacterial flora in normal neonates. J Med Microbiol 1981; 14:51–62. [DOI] [PubMed] [Google Scholar]
- 51.Srinivasan S, Fredricks DN. The human vaginal bacterial biota and bacterial vaginosis. Interdiscip Perspect Infect Dis 2008; 2008:750479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Swidsinski A, Mendling W, Loening-Baucke V et al. Adherent biofilms in bacterial vaginosis. Obstet Gynecol 2005; 106:1013–23. [DOI] [PubMed] [Google Scholar]
- 53.Swidsinski A, Loening-Baucke V, Mendling W et al. Infection through structured polymicrobial Gardnerella biofilms (StPM-GB). Histol Histopathol 2014; 29:567–87. [DOI] [PubMed] [Google Scholar]
- 54.Workowski KA. Centers for disease control and prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis 2015; 61(suppl 8):S759–62. [DOI] [PubMed] [Google Scholar]
- 55.Sobel JD, Ferris D, Schwebke J et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol 2006; 194:1283–9. [DOI] [PubMed] [Google Scholar]
- 56.Swidsinski A, Mendling W, Loening-Baucke V et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol 2008; 198:97 e1–6. [DOI] [PubMed] [Google Scholar]
- 57.Swidsinski A, Dorffel Y, Loening-Baucke V, Schilling J, Mendling W. Response of Gardnerella vaginalis biofilm to 5 days of moxifloxacin treatment. FEMS Immunol Med Microbiol 2011; 61:41–6. [DOI] [PubMed] [Google Scholar]
- 58.Muzny CA, Schwebke JR. Biofilms: an underappreciated mechanism of treatment failure and recurrence in vaginal infections. Clin Infect Dis 2015; 61:601–6. [DOI] [PMC free article] [PubMed] [Google Scholar]