Abstract
Anxiety and depression are often highly correlated with each other. To explain this connection, the present study examined the longitudinal relationship between earlier anxiety and later depression, using avoidance as a mediator and trauma as a moderator. Participants (N = 6504 adolescents) completed baseline measures of anxiety and depression, a measure of avoidance one year later, a measure of trauma six to eight years later, and a measure of depression 12–14 years later. Analyzed with structural equation models, the results showed that anxiety predicted later depression, and this relationship was partially mediated by avoidance. The relationship between avoidance and depression was not moderated by trauma. Together, these findings suggest that anxiety may influence later depression through avoidance, and this relationship remains unaffected by experiencing a traumatic experience.
Keywords: Anxious, Depressive, Negative affect, Longitudinal, Mediational
1. Introduction
Anxiety and depressive disorders are frequently comorbid with one another, yielding lifetime prevalence estimates from 16 to 50% (Angold, Costello, & Erkanli, 1999; Seligman & Ollendick, 1998). Seventy-three percent of persons with major depression have comorbid lifetime anxiety disorders, whereas 27–77% of those with a principal diagnosis of an anxiety disorder develop a lifetime diagnosis of depression (Brown, Campbell, Lehman, Grisham, & Mancill, 2001). In comparison to those with pure diagnoses, individuals with comorbid anxiety and depressive disorders experience greater chronicity and severity of each diagnosis; poorer work and psychosocial functioning; lower perceived quality of life; and a heightened risk of suicide (Brown, Schulberg, Madonia, Shear, & Houck, 1996; Kessler et al., 1998; Olfson et al., 1997; Pfeiffer, Ganoczy, Ilgen, Zivin, & Valenstein, 2009; Sherbourne, Wells, Meredith, Jackson, & Camp, 1996). Hence, a greater understanding of the mechanisms behind this comorbidity is imperative.
Concurrent anxiety and depression are highly correlated with one another (r ranges .45–.73) when measured on a continuum (Bjelland, Dahl, Haug, & Neckelmann, 2002; Cannon & Weems, 2006; Morgan, Wiederman, & Magnus, 1998; Norton, Cosco, Doyle, Done, & Sacker, 2013; Watson, Weber, et al., 1995). Based on this high correlation, anxiety and depression are often conceptualized as slightly variant manifestations of the same underlying phenomena with a shared diathesis (Barlow & Campbell, 2000; Clark & Watson, 1991; Grunhaus, 1988; Kendler, 1996; Kendler, Neale, Kessler, Heath, & Eaves, 1992). The research on the concurrent focus of anxiety and depression has yielded several highly related models including Clark and Watson’s (1991) tripartite model, Barlow’s (1988) hierarchical model of anxiety and depression, Mineka, Watson, and Clark’s (1998) integrative hierarchical model of anxiety and depression, and Watson’s (2005) revised hierarchical model of anxiety and depressive disorders. Fundamentally, each of these prominent models suggests that both anxiety and depression are best represented by the same underlying construct, termed negative affect.
Despite the high concurrent relationships between anxiety and depression, these hierarchical models also allow for anxiety and depression to be distinguished from one another. Specifically, across each of the predominant models, arousal is characteristic of anxiety but not depression, and anhedonia (lack of positive affect) is consistent with depression but not anxiety (Barlow, 1988; Clark & Watson, 1991; Mineka et al., 1998; Watson, 2005). The ability to distinguish between anxiety and depression has also gained empirical support as arousal and fear are associated with anxiety, but not depression; and anhedonia is associated with depression but not anxiety (Barlow, Chorpita, & Turovsky, 1996; Bjelland et al., 2002; Brown et al., 2001; Cannon & Weems, 2006; Chorpita, Albano, & Barlow, 1998; Clark & Watson, 1991; Morgan et al., 1998; Tellegen, 1985; Watson, Weber, et al., 1995). Thus, despite these predominant models’ higher order structure, anxiety and depression can be reliably distinguished from each other.
The evidence used to support the models of shared symptomatology derives overwhelmingly from concurrent correlations between anxiety and depression using factor analyses (Brown, Chorpita, & Barlow, 1998; Chorpita et al., 1998; Clark, Beck, & Stewart, 1990; Joiner, 1996; Jolly, Dyck, Kramer, & Wherry, 1994; Jolly & Kramer, 1994; Watson, Clark, et al., 1995). However, all research in support of negative affect to date is fundamentally unable to rule out alternative explanations for these findings. Specifically, these methodologies are not able to address the potential relationships between anxiety and depression predicting one another over time (e.g. one way to rule out this alternative explanation is through a longitudinal factor model, which has never before been conducted in this domain).
The limitations of the shared symptomatology models are further highlighted by the literature on the temporal precedence of anxiety and depression. Research on temporal precedence reliably shows that current anxiety significantly predicts later depression (see Jacobson & Newman, 2012a for a meta-analysis). Using continuous measures of anxiety and depression, researchers found that anxiety positively predicted depression with correlations ranging from r = .16 to .45 (without controlling for earlier depression). Further, the hazards ratio range for those with an anxiety disorder to develop a later depressive disorder is 1.49–7.1 (Jacobson & Newman, 2012a). Additionally, anxiety predicts depression across years (Wilson & Hayward, 2005), months (Lockefeer & De Vries, 2012), weeks (Wittchen, Becker, Lieb, & Krause, 2002), days (Jacobson & Newman, 2012b; Starr & Davila, 2012a, 2012b; Swendsen, 1997), and hours (Jacobson & Newman, 2012b; Swendsen, 1998). Although third variables still need to be ruled out, this research suggests that anxiety may be a risk factor for depression, and this longitudinal relationship may explain shared symptomatology models (as levels of anxiety predicting depression may appear to occur at the same time point if only measured once across a retrospective period of time).
Despite the vast literature demonstrating that anxiety predicts later depression, only three studies have examined this within a prospective mediational analysis, and hence examined possible mechanisms of how high anxiety leads to increased depression. Firstly, Joiner, Katz, and Lew (1999) examined negative life events and reassurance-seeking as mediators between anxiety and depression; however, these authors did not find that either variable significantly mediated the relationship. Likewise, Ceyhan (2009) studied whether locus of control and problem-solving skills mediated the relationship between earlier anxiety and later depression, but neither variable mediated the relationship. Moitra, Herbert, and Forman (2008) examined behavioral avoidance as a mediator between social anxiety and depressive symptoms over the course of treatment and found that behavioral avoidance partially mediated the relationship. However, the effects of this study may have been due to the order of treatment techniques in the therapies (e.g. anxiety was targeted first, followed by avoidance, followed by depression). Although some mediational variables have been tested, the mechanism through which anxiety might affect later depression is currently unknown in naturalistic settings.
Avoidance is a promising mechanism for explaining the naturalistic longitudinal relationship between anxiety and depression (Moitra et al., 2008). Anxiety is considered an uncomfortable state of physiological activation elicited by a perceived external threat (Nesse & Williams, 1996), and persons who experience anxiety limit their exposure (avoid) to these perceived threats to reduce their levels of discomfort. However, avoiding feared circumstances may also reduce one’s exposure to both positive and corrective experiences. For example, if one avoids a social event due to social anxiety, one may not experience social support. Similarly, if someone has agoraphobia and is afraid of leaving his/her house, he or she may not experience the positive physical and psychological health outcomes of nature (Hartig et al., 2011). A lack of such positive life experiences has been shown to coincide with increased depression (Harris & Curtin, 2002; Spinhoven et al., 2011). Thus, depression may develop from increased pessimism and hopelessness about the future due to a skewed sense of reality based on one’s exposure to fewer positive events. Although no studies have examined anxiety, depression, and avoidance together longitudinally in a naturalistic setting, research has shown that previous levels of anxiety predict future levels of avoidance (Rinck et al., 2010), and past avoidance predicts later depression (Brewin, Reynolds, & Tata, 1999; Cloninger, Svrakic, & Przybeck, 2006; Plant & Devine, 2003; Wittchen, Kessler, Pfister, Höfler, & Lieb, 2000). Thus, in the current study, avoidance was examined as a possible mediator of anxiety and later depression.
Further, trauma may moderate the relationship between avoidance and depression. Those who regularly cope without avoidance may naturally employ real-life exposure hierarchies (Richard & Lauterbach, 2011). Consequently, the ability to cope with daily stressful events may help one to cope with trauma and enhance one’s self-efficacy in dealing with traumas. However, those who employ avoidance behaviors to cope with life events may not learn to deal with distress (Tryon, 2005). For these persons, experiencing a traumatic event may be similar to the initial distress associated with the beginning of flooding therapy (exposure to individuals’ most feared event) without the prolonged exposure to teach them that they can cope with their distress (Sundel & Sundel, 2004). Based on the theory that individuals employing avoidance may be more likely to react to trauma with hopelessness and with the belief that they will never have control over their lives otherwise, we hypothesized that trauma may moderate the relationship between avoidance and depression (Alloy, Kelly, Mineka, & Clements, 1990). Accordingly, we will investigate trauma as a moderator between avoidance and depression.
The current study investigated the relationship between anxiety and depression over time to examine whether avoidance mediated the relationship between anxiety and depression, and whether trauma moderated the relationship between avoidance and depression. This study used a nationally representative longitudinal sample beginning in adolescence and carrying through to early adulthood. We hypothesized that (1) anxiety would predict later depression 12–14 years later; (2) anxiety and depression would be mediated by avoidance, such that anxiety would predict positively avoidance one to two years later and avoidance would predict depression 10–13 years later; and (3) the relationship between avoidance and depression would be moderated by trauma, such that experiencing a trauma five to six years after the avoidance would significantly increase the positive relationship between avoidance and depression.
2. Method
2.1. Participants
The participants for this study were collected through the National Longitudinal Study of Adolescent Health (Add Health) public use dataset (Harris & Udry, 2013). There were four waves of data collection: the first occurred during 1994–1995; the second occurred during 1995–1996; the third wave occurred during 2001–2002; and the fourth wave occurred during 2007–2008. The data was collected through interviews with participants. The first wave of participants (N = 6504, 48% male, M age = 16.04, 66% Caucasian, 25% African American, 1% American Indian, 4% Asian/Pacific Islander, 5% Other) continued with little dropout over the second (N = 4834, 48% male, M age = 16.53, 67% Caucasian, 23% African American, 1% American Indian, 4% Asian/Pacific Islander, 5% Other), third (N = 4882, 46% male, M age = 22.32, 66% Caucasian, 24% African American, 1% American Indian, 4% Asian/Pacific Islander, 5% Other), and fourth waves (N = 5114, 46% male, M age = 28.89, 68% Caucasian, 24% African American, 1% American Indian, 3% Asian/Pacific Islander, 4% Other).
2.2. Measures
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D is a brief self-report questionnaire designed to measure depressive symptoms in the general population (Radloff, 1977). A portion of the CES-D was given to subjects in the Add Health study at waves one and four (see Walsemann, Bell, & Goosby, 2011 for all items included). To test if the CES-D scale would accurately be reflected as one construct, a confirmatory factor analysis was performed on the 10 CES-D items at wave one. The one factor model resulted in adequate fit (χ2 = 1125.61, p < .01, RHO = 0.971, CFI = 0.976, RMSEA = 0.071). Methods used in the confirmatory factor analysis are detailed below. The full scale has been shown to have adequate concurrent validity (r = .73–.89 compared to the Symptom Checklist depression scale) (Weissman, Sholomskas, Pottenger, Prusoff, & Locke, 1977). The retest reliability for the full scale is adequate (r = .57 averaged from 2 to 8 weeks) (Radloff, 1977). There was also good internal consistency (α = .979) for these ten items in the current sample. See Table 1 for items. Additionally, a confirmatory factor analysis was performed which included items from the anxiety scale (listed below). This second confirmatory factor analysis yielded identical good model fit with distinct CES-D and anxiety factors (χ2 = 1650.44, p < .01, RHO = 0.977, CFI = 0.980, RMSEA = 0.050). This suggests that the reduced CES-D scale is distinct from anxiety.
Table 1.
Anxiety, depression, and avoidance scales.
| Measure | Item | Waves | Scale |
|---|---|---|---|
| CES-D | You were happy (reverse coded). | 1, 2, 4 | Never 0–3 most/all of the time |
| You could not shake the blues, even with help from your friends and family. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You enjoyed life (reverse coded). | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You felt depressed. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You felt that you were just as good as other people (reverse coded). | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You felt sad. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You were bothered by things that usually don’t bother you. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You didn’t feel like eating, your appetite was poor. | 1, 2 | Never 0–3 most/all of the time | |
| You had trouble keeping your mind on what you were doing. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You felt that you were too tired to do things. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| You felt hopeful about the future (reverse coded). | 1, 2 | Never 0–3 most/all of the time | |
| You thought your life had been a failure. | 1, 2 | Never 0–3 most/all of the time | |
| You felt fearful. | 1, 2 | Never 0–3 most/all of the time | |
| You were happy (reverse coded). | 1, 2, 4 | Never 0–3 most/all of the time | |
| You talked less than usual. | 1, 2 | Never 0–3 most/all of the time | |
| You felt lonely. | 1, 2 | Never 0–3 most/all of the time | |
| People were unfriendly to you. | 1, 2 | Never 0–3 most/all of the time | |
| You felt that people disliked you. | 1, 2, 3, 4 | Never 0–3 most/all of the time | |
| It was hard to get started doing things. | 1, 2 | Never 0–3 most/all of the time | |
| Anxiety | Feeling hot all over suddenly, for no reason. | 1, 2 | Never 0–4 every day |
| Cold sweats. | 1, 2 | Never 0–4 every day | |
| Chest pains. | 1, 2 | Never 0–4 every day | |
| Fearfulness. | 1, 2 | Never 0–4 every day | |
| A stomach ache or an upset stomach. | 1, 2 | Never 0–4 every day | |
| Trouble relaxing. | 1, 2 | Never 0–4 every day | |
| Avoidance | You usually go out of your way to avoid having to deal with problems in your life (reverse coded). | 1, 2 | Strongly agree 1–5 Strongly disagree |
Note: This table represents the items from the Center for Epidemiologic Studies Depression Scale (CES-D), the constructed anxiety scale, and the avoidance item. The wave column indicates which wave that the item was administered (not all items were administered at all waves in the Add Health).
Anxiety Scale
Six items that were given in the Add Health constituted a physiological symptom-based measure of anxiety. Although these items have not been used prior to the Add Health administration, the content represented in these scales is analogous to other measures of anxiety, such as the Beck Anxiety Inventory (Steer & Beck, 1997). To investigate how the items grouped as a factor, a confirmatory factor analysis was performed on this scale. Based on the model fit, the factors held together on a single scale (χ2 = 143.14, p < .01, RHO = 0.974, CFI = 0.986, RMSEA = 0.053). Methods used in the confirmatory factor analysis are detailed below. The internal consistency of this scale was adequate (α = .62) in this study. See Table 1 for items.
Avoidance Item
One item was administered in wave two to assess avoidance. This item was reverse-coded so that a higher level of avoidance represented a higher score on the scale. The avoidance item was: “You usually go out of your way to avoid having to deal with problems in your life.” The scale was rated on a one (anchor: “Strongly Agree”) to five (anchor: “Strongly Disagree”) Likert scale. The item in question appears to be a face valid measure of avoidance and semantically similar to items on previously validated avoidance scales (e.g. “out of my way” is used in the Behavioral Avoidance System scales (Carver & White, 1994), “problems in my life” is a central part of the directions in the Cognitive–Behavioral Avoidance Scale (Ottenbreit & Dobson, 2004)).
Trauma Grouping Variable
Add Health inquired about 13 types of trauma including whether a participant had been a victim of assault, rape, knifing, or gunshots; witnessed an assault, knifing, or gunshots; and had a family member or friend commit suicide (see Table 2). This trauma scale was originally formed by Roberts, Fuemmeler, McClernon, and Beckham (2008). These items were summed and dichotomized based on a median split. The median occurred between endorsing none of the items and endorsing one or more on each scale, which is an accepted cutpoint in trauma research (e.g. Scheeringa, Zeanah, Myers, & Putnam, 2003; Tedeschi & Calhoun, 1996). Thus, the trauma group contained 2013 subjects, whereas the no trauma group contained 3765 subjects. This scale was administered in the third and fourth waves of data collection.
Table 2.
Frequency of traumatic events.
| Number | Questions | Percentage of sample experienced |
|---|---|---|
| 1 | Has someone slapped, hit, choked, or kicked you? | 9.30% |
| 2 | Has [your partner] threatened you with violence, pushed or shoved you, or thrown something at you that could hurt? | 7.90% |
| 3 | Has [your partner] slapped, hit, or kicked you? | 5.80% |
| 4 | You saw someone shoot or stab another person | 5.40% |
| 5 | Someone pulled a gun on you | 4.20% |
| 6 | Has [your partner] insisted on or made you to have sexual relations with [him/her] when you didn’t want to? | 3.90% |
| 7 | Someone pulled a knife on you | 3.60% |
| 8 | You were beaten up, but nothing was stolen from you | 2.30% |
| 9 | Have any of your friends tried to kill themselves and die as a result? | 2.30% |
| 10 | Someone stabbed you | 0.80% |
| 11 | Have any of your family members tried to kill themselves and die as a result? | 0.80% |
| 12 | You were beaten up and something was stolen from you | 0.70% |
| 13 | Someone shot you | 0.50% |
Note: This table presents the percentage of each of the traumatic events that happened in the sample.
Reported Diagnoses
In the fourth wave of data collection, persons were asked if they had been diagnosed with an anxiety or depressive disorder by their doctor, nurse, or health care provider. These diagnoses were compared to the anxiety and depression scales to test whether higher scores on the scales were associated with reported clinical diagnoses. As the anxiety questionnaire was only administered in the first and second waves of data collection, anxiety scores were compared with reported diagnoses longitudinally rather than concurrently.
Planned Analyses
Prior to the principal analysis, the means of the constructs at each wave were examined (see Table 3). Additionally, the number of psychiatric diagnoses in the fourth wave was examined. Using independent samples t-tests, anxiety and depressive diagnoses as the independent variables were analyzed to see if the presence of these diagnoses were associated with higher scores on the anxiety and depression scales, respectively. Area under the receiver operator analyses (ROC) were then examined to determine scale cutpoints and the number of diagnoses at earlier time-points.
Table 3.
Descriptive statistics.
| Waves | Scale | Sum (SD) | M per item |
|---|---|---|---|
| 1 | CES-D (18-items) | 15.08 (5.10) | 0.84 |
| 2 | CES-D (18-items) | 15.16 (4.97) | 0.84 |
| 3 | CES-D (7-items) | 7.90 (2.81) | 1.13 |
| 4 | CES-D (10-items) | 10.45 (2.69) | 1.05 |
| 1 | Anxiety (7-items) | 3.51 (2.67) | 0.50 |
| 2 | Anxiety (7-items) | 3.53 (2.47) | 0.50 |
| 1 | Avoidance (1-item) | 2.15 (1.06) | 2.15 |
| 2 | Avoidance (1-item) | 2.41 (1.12) | 2.41 |
Note: This table presents the sum, standard deviation, and item means for the depression, anxiety, and avoidance scales.
Analyses were conducted in LISREL 8.8, using latent variable modeling with anxiety (wave one, hereafter referred to as W1) as a predictor, avoidance as a mediator, and depression (wave four, hereafter referred to as W4) as a dependent variable.1 Mediation was determined based on the joint significance test, wherein partial mediation was determined by significant regression weights between anxiety and avoidance, and avoidance and depression (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). Full mediation was determined by a lack of significance of the direct relationship between anxiety and depression when avoidance was included in the model.
In the current application, all manifest variables from the anxiety, depression, and avoidance scales are ordinal, and not continuous. As such, all analyses were conducted using the diagonally weighted least squares (WLSMV) estimator with mean and variance adjusted chi-squares, treating all manifest variables as ordinal (Jöreskog & Sörbom, 1996).
Differences between the no trauma group and the trauma group were then examined to test whether the role of avoidance in predicting depression was impacted by the experience of a traumatic event. Note that the trauma measure was dichotomized to facilitate the examination of group differences in model invariance. Differences between the trauma groups were observed by constraining factor loadings and beta weights to be equal across groups and by examining the change in fit statistics. Missing data (approximately 6.6% missingness for the full sample) was handled using full information maximum likelihood (FIML) (the only exception to this was the 726 participants who were missing all of the trauma variables from wave three and could not be imputed by LISREL’s FIML procedure and thus were discarded for the between group analyses).
3. Results
3.1. Anxiety and depression measures compared to reported diagnoses
In the fourth wave, 16.2% of the sample reported that they had been diagnosed with major depression by a doctor, nurse, or other healthcare provider. Persons who reported that they had been diagnosed with depression had significantly, t(993) = 19.01, p < .001, d = 0.80, higher scores on the reduced CES-D depression (W4) scale (M = 9.56, SD = 5.82) than those who reported that they had not been diagnosed with depression (M = 5.43, SD = 4.14). Receiver operator curve (ROC) analyses were conducted to determine the optimal cut-point. A cutpoint of 7.5 produced the highest Youden’s index, with a sensitivity of .74 and a specificity of .58 (Youden, 1950). Using this value yielded an estimated prevalence of 24.4% of the sample with a diagnosis of depression based on participants’ self-reported depression scores in wave four. When this criterion was applied to wave one, results showed that 10.1% of the sample would be diagnosed with depression.
In the fourth wave, 12.5% of the sample reported that they had been diagnosed with an anxiety disorder. Participants with an anxiety disorder at time four had a significantly, t(762) = 8.35, p < .001, d = 0.40, higher score on the anxiety scale at time one (M = 4.33, SD = 2.91) than those who did not report having an anxiety disorder at time four (M = 3.26, SD = 2.35). Similarly, those who had an anxiety disorder at time four had significantly, t(594) = 8.35, p < .001, d = 0.43, higher scores on the anxiety scale at time two (M = 3.98, SD = 2.43) than those who reported that they did not have an anxiety disorder at time four (M = 3.02, SD = 1.96). Because the anxiety diagnosis measure and the anxiety scale were not administered at the same time point the ROC yielded poor predictive validity. Specifically, the approach using the ROC from the anxiety scores at wave two suggested a cutpoint of 2.5 based on the Youden’s index, with a sensitivity of .71 and a specificity of .48. When this cutoff was applied to the first wave, the results showed that 55.8% would be diagnosed with an anxiety diagnosis. Thus, the number of anxiety disorders is unknown until wave four; however, the scales at wave one and wave two significantly predicted higher rates of anxiety diagnoses at wave four.
3.2. Testing primary model assumptions
Prior to each analysis, the model’s assumptions were tested. Specifically, the model’s identification was tested by comparing the model’s completely standardized solutions against typically acceptable loadings (Graham, 2005; Jöreskog & Sörbom, 1996). Based on factor loadings in the completely standardized solutions, the identification status of the primary model was considered identified. After testing the identification status, the goodness of fit for the model was examined. To test the goodness of fit, the practical indices of goodness of fit were used: RHO (also titled NNFI) (Bentler & Bonett, 1980; Tucker & Lewis, 1973), CFI (also titled RNI) (Bentler, 1990; McDonald & Marsh, 1990), and RMSEA (Browne & Cudeck, 1993; Steiger, 1990). Practical indices of goodness of fit were used in place of the chi-square fit statistics as the chi-square values are highly affected by large sample sizes, as in the present dataset.
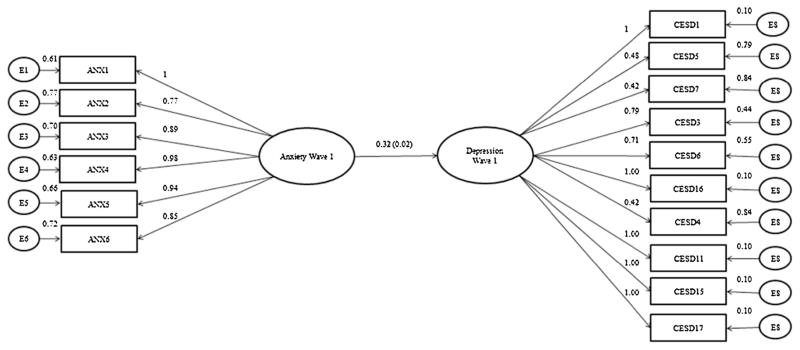
3.3. Anxiety predicting depression
The first hypothesis, that anxiety (W1) would predict later depression (W4), was tested by predicting later depression from earlier anxiety. The goodness of fit indices for this analysis were χ2 = 7021.51, p < .01, RHO = 0.953, CFI = 0.944, RMSEA = 0.10, reflected an adequate fit. The results of the model showed that anxiety (W1) significantly (β = 0.32, SE = 0.02, Z = 16.36, p < .001) predicted later depression (W4) (see Fig. 1).
Fig. 1.
N = 6504. In this figure, anxiety at wave one is predicting depression at wave four. Solid lines represent significant connections (p < .05).
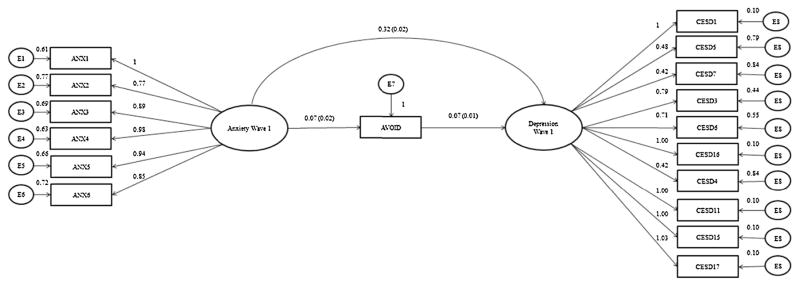
3.4. Anxiety and depression mediated by avoidance
After anxiety was shown significantly and positively to predict depression 12–14 years later, the next model tested if the relationship between anxiety (W1) and depression (W4) was mediated by avoidance. We first examined if anxiety (W1) predicted both avoidance (W2) and depression (W4), and if avoidance (W2) predicted later depression (W4). The goodness of fit indices for this analysis were χ2 = 662.84, p < .01, RHO = 0.995, CFI = 0.996, RMSEA = 0.028, suggesting a good fit. In this model, anxiety (W1) significantly (β = 0.07, SE = 0.02, Z = 3.22, p < .001) predicted avoidance (W2), and avoidance significantly (β = 0.07, SE = 0.01, Z = 5.03, p < .001) predicted depression (W4) (see Fig. 2). Additionally, the residual direct effect showed that anxiety (W1) significantly (β = 0.32, SE = 0.02, Z = 13.00, p < .001) directly predicted depression (W4). As such, based on the joint significance test, avoidance partially mediated the relationship between anxiety and depression (MacKinnon et al., 2002). Please note that the magnitude of the mediation explained was 5.1% of the variation between anxiety (W1) predicting depression (W4) (determined by dividing the explained variance of anxiety predicting avoidance by the total degree of variance between anxiety predicting depression).
Fig. 2.
N = 6504. In this figure, anxiety at wave one is predicting avoidance at wave two. Additionally, anxiety at wave one and avoidance at wave two are predicting depression at wave four.
This model was re-analyzed examining between-group differences between those with and without diagnosed depressive disorders at wave four, and there were no group differences in any loadings. Specifically, when those with depressive disorders were constrained to have equal factor loadings, the difference in fit between the unconstrained group loadings was , pdiff < .01, RHOdiff = −0.006, CFIdiff = −0.002, RMSEAdiff = −0.001, which showed that the difference in fit was not practically different. Additionally, when the regression parameters were constrained to be equal, the difference in fit between the chi-square of the partially constrained model and the model with the unconstrained betas was , pdiff > .05. Please note that indices of practical fit are not appropriate to test differences in the betas, as chi-squared differences in the betas are not affected by large sample sizes (Graham, 2005). Thus, there were no differences between the structural equation model for those with clinical levels of depression compared to those without clinical depression. Additionally, the model was re-analyzed examining between-group differences in those with anxiety disorders at wave four, and there were also no between-group differences. The difference between the unconstrained model and the model constraining the anxiety disorders group and the non-anxiety disorders group resulted in fit indices of , pdiff < .01, RHOdiff = −0.002, CFIdiff = 0.005, RMSEAdiff = −0.001. The fit statistics showed that there were no differences in the practical model fit. Lastly, when the beta-weights were constrained to be equal the difference in fit statistics was , pdiff > .05. This means that results for the groups with and without clinical anxiety were not practically different from one another.
3.5. Anxiety and depression mediated by avoidance, moderated by trauma
After showing that avoidance partially mediated the relationship between anxiety and depression within the whole sample, the hypothesis that trauma would moderate the relationship between avoidance and depression was tested. This was done through a series of four two-group models each with greater constraints. The first two-group model examined the fit when all of the factor loadings and beta relationships were unconstrained between the groups. The fit indices for the first model were χ2 = 541.88, p < .01, RHO = 0.996, CFI = 0.997, RMSEA = 0.015, suggesting a good fit. When the factor loadings were constrained to be equal, the model fit indices were χ2 = 542.40, p < .01, RHO = 0.997, CFI = 0.997, RMSEA = 0.014. By comparison, the latter model fit was not significantly different with the former one ( , pdiff > .05, RHOdiff = 0.000, CFIdiff = 0.000, RMSEAdiff = −0.001), which is note-worthy given the high potential for significance due to the large sample and the constraints on factor loadings. This means that all of the factors can be said to be functioning equivalently in both the high and low trauma groups.
Next, the betas were tested between groups. All of the pathways, except the pathway between avoidance (W2) (as this was the apriori hypothesis) and predicting depression (W4) were constrained to be equal. This model was compared to the previous model, where the factor loadings were constrained. The goodness of fit indices for the partially constrained model was χ2 = 545.85, p < .01. The chi-square of the partially constrained model was subtracted by the model with unconstrained betas showing a difference of , pdiff > .05. This means that there were no significant differences in the betas across the two groups, aside from any group difference between the two groups in the beta for avoidance predicting depression (W4).
Subsequently, the apriori hypothesis that high trauma would predict a significantly stronger relationship between avoidance and later depression than the relationship between avoidance and depression in the low trauma group (W4) was tested by constraining all of the pathways to be equal across groups. Then, the model with all the pathways constrained, except avoidance predicting depression (W4), was subtracted from the fully constrained pathway model. The fully constrained pathway model’s goodness of fit indices were χ2 = 547.77, p < .01. The difference between the partially and fully constrained model was , pdiff = .08. Accordingly, there were no significant differences between the high and low trauma groups for the coefficient of avoidance predicting later depression. As such, trauma did not moderate the relationship between avoidance and depression.
4. Discussion
Supporting our first hypothesis, the results of this study showed that anxiety significantly positively predicted later depression over a decade later, with anxiety at wave one explaining approximately 23% of the variance in depression at wave four. These results are consistent with previous findings suggesting that anxiety predicts later depression (Jacobson & Newman, 2012a).
Moreover, this study also extends previous findings and helps to explain how anxiety and later depression may relate to one another. Supporting our second hypothesis, anxiety and depression were partially mediated by avoidance. This is the first study to find a significant mediational relationship between earlier anxiety and later depression in a naturalistic setting. Consistent with previous research (Moitra et al., 2008; Rinck et al., 2010), these results may support the conceptualization that persons who are anxious employ avoidance as a coping strategy to lessen their negative feelings of anxiety. Also consistent with previous research (Brewin et al., 1999; Cloninger et al., 2006; Moitra et al., 2008; Plant & Devine, 2003; Wittchen et al., 2000), those who employed avoidance had higher levels of later depression. It is possible that avoidance may reduce the likelihood of experiencing positive events and activities. Fewer positive events would then lead to depression as theorized by Lewinsohn (1975) and demonstrated in prior studies (Cohen & Hoberman, 1983; Needles & Abramson, 1990). However, further research is needed to test this theoretical mediational chain.
In contrast to our third hypothesis, there were no significant differences in the relationship between avoidance and depression for those who had experienced a traumatic event versus persons who had not experienced trauma These results are inconsistent with the conceptualization that those who employ avoidance may not be as prepared to cope with a traumatic event compared to those who do not employ avoidance.
There were no differences in any of the model paths when comparing those with depression diagnoses at the fourth wave against controls. Similarly, there were no group differences between those with anxiety diagnoses at the fourth wave and controls. Thus, anxiety predicting later depression, and avoidance mediating the relationship between anxiety and depression appear to apply both to those in the normal population and those with clinical levels of anxiety and depressive disorders. This makes sense given that both clinical and nonclinical anxiety and depression are considered to be dimensional constructs (Shankman & Klein, 2002; Shear, Bjelland, Beesdo, Gloster, & Wittchen, 2007).
This study has many theoretical and practical implications. By finding the first significant mediational relationship, this study helps to further establish anxiety as a risk factor for later depression and begins to map the potential causal chain between these two constructs (Wu & Zumbo, 2008). In regard to treatment and prevention implications, this study further suggests that interventions targeting heightened subthreshold levels of anxiety in adolescents may prevent high levels of avoidance, and ultimately prevent high levels of depression in early adulthood. Additionally, it suggests that interventions targeting anxiety may also benefit from avoidance and depression as process and outcome variables in later assessments, such that if an intervention is successful there may be reduced levels of avoidance and depression at later times. It also suggests that targeting both subclinical anxiety and tendencies toward avoidance may be helpful. Given the robust effect of anxiety in predicting later depression, treating early subthreshold anxiety in adolescents may be associated with preventing the negative effects of comorbidity between anxiety and depression in adulthood, such as improving psychosocial and work functioning, heightening perceived quality of life, and reducing rates of suicide (Brown et al., 1996; Kessler et al., 1998; Olfson et al., 1997; Pfeiffer et al., 2009; Sherbourne et al., 1996).
Despite the important theoretical and practical applications, this study has limitations. Although there was a significant mediational relationship between anxiety and depression, the degree to which avoidance explained the relationship between anxiety and later depression was relatively small (5.1% of the total variance between anxiety predicted depression). This small variance could have been due to the use of a single item avoidance measure with no previous psychometric validation. In addition, although this study included some individuals at clinical levels of anxiety and depression, most persons in the sample did not have clinical levels of anxiety and depression. Diagnoses were measured via self-report, rather than a diagnostic interview, which may limit their reliability.
Many studies have shown that anxiety predicts later depression, and not vice versa (Jacobson & Newman, 2012a). As an additional limitation to the current study, the Add Health study did not re-administer the anxiety scale at wave four. Accordingly, we were unable to test whether depression had similar effects in predicting later anxiety for this sample. Thus we could not determine whether anxiety uniquely predicted later depression, or whether depression also predicted later anxiety for this sample. An additional limitation of this study was that we used a measure of general anxiety as opposed to a measure of posttraumatic stress to examine the relationship between anxiety and depression as a function of trauma. As such, it is unknown if the current findings would generalize to posttraumatic stress symptoms in particular.
Additional research needs to be conducted to examine how anxiety and depression relate to each other over time. For example, the following variables should be examined as possible mediators over time: helplessness and hopelessness (anxiety being associated with a state of helplessness, and helplessness gradually developing into a state of hopelessness, hopelessness then is related to the development of depression) (Alloy et al., 1990); attachment/separation (wherein persons respond to separation from an attachment figure first with anxiety and subsequently develop a sense of loss from the relationship coinciding with depression) (Bowlby, 1980); arousal/fatigue (such that anxiety is associated with physiological activation which decreases one’s energy levels to produce fatigue, and the low level of energy produces depression) (Akiskal, 1985); and attentional/interpretive biases (such that anxiety is associated with a focus on threat cues, and over time the threat cues lead to a memory bias such that persons can only recall negative events; this recall of only negative events then could lead to the onset of depression) (Butler & Mathews, 1983; MacLeod & Byrne, 1996).
In conclusion, the current study found that anxiety significantly predicted later depression 12–14 years later. Additionally, the relationship between anxiety and depression was jointly positively mediated by avoidance. More research is needed to examine the causal relationship between anxiety and depression, using avoidance and other previously hypothesized causal mechanisms.
Acknowledgments
The data used in this publication were made available by the Data Archive on Adolescent Pregnancy and Pregnancy Prevention, Sociometrics Corporation, 170 State Street, Suite 260, Los Altos, CA 94022-2812. The study entitled The National Longitudinal Study of Adolescent Health (Add Health), study waves from 2001 to 2002 was conducted by J. Richard Udry of the Carolina Population Center, University of North Carolina atChapel Hill. Funding for the data collection was provided by the National Institute of Child Health and Human Development (NICHD) under grant no. P01-HD31921. Funding for the work done by the Data Archive on Adolescent Pregnancy and Pregnancy Prevention to prepare the data for public use was provided by the National Institute for Child Health and Human Development (NICHD) under contract no. N01-HD-9-3306 to Sociometrics Corporation. The original investigators, funding agency, and DAAPPP are not responsible for the analyses or interpretations presented here.
Footnotes
Depression (W1) was also originally included in the model, but it was removed due to substantial multicollinearity issues. Multicollinearity was deemed to be present based on the high correlation between anxiety and depression, and unstable model coefficients. Specifically, the estimate of anxiety (W1) predicting depression (W4) varied widely when depression (W1) was added to the model. Without depression (W1), anxiety (W1) significantly (β = 0.32, SE = 0.02) positively predicted depression (W4). However when depression (W1) was added to the model and predicted depression (W4), the relationship between anxiety (W1) predicting depression (W4) became significantly negative (β = −0.20, SE = 0.04). Unstable estimates, such as those noted in this study, are symptomatic of multicollinearity (Lin, 2008; Wax, 1992). Additionally, there was a moderately high correlation between anxiety (W1) and depression (W1).
References
- Akiskal HS. Anxiety: definition, relationship to depression, and proposal for an integrative model. In: Tuma H, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Lawrence Erlbaum Associates; 1985. pp. 787–797. [Google Scholar]
- Alloy LB, Kelly KA, Mineka S, Clements CM. Comorbidity of anxiety and depressive disorders: a helplessness–hopelessness perspective. Washington, DC, US: American Psychiatric Association; 1990. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. http://dx.doi.org/10.1111/1469-7610.00424. [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. New York, NY, US: Guilford Press; 1988. [Google Scholar]
- Barlow DH, Campbell LA. Mixed anxiety-depression and its implications for models of mood and anxiety disorders. Comprehensive Psychiatry. 2000;41(2 Suppl 1):55–60. doi: 10.1016/s0010-440x(00)80009-7. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Chorpita BF, Turovsky J. Fear, panic, anxiety, and disorders of emotion. Lincoln, NE, US: University of Nebraska Press; 1996. [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88(3):588. [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. http://dx.doi.org/10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss. New York, NY, US: Basic Books; 1980. [Google Scholar]
- Brewin CR, Reynolds M, Tata P. Autobiographical memory processes and the course of depression. The Journal of Abnormal Psychology. 1999;108(3):511. doi: 10.1037//0021-843x.108.3.511. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. American Journal of Psychiatry. 1996;153(10):1293. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. The Journal of Abnormal Psychology. 2001;110(4):585. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. The Journal of Abnormal Psychology. 1998;107(2):179–192. doi: 10.1037//0021-843x.107.2.179. http://dx.doi.org/10.1037/0021-843X.103.4.645. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. SAGE Focus Editions. 1993;154:136. [Google Scholar]
- Butler G, Mathews A. Cognitive processes in anxiety. Advances in Behaviour Research & Therapy. 1983;5(1):51–62. http://dx.doi.org/10.1016/0146-6402(83)90015-2. [Google Scholar]
- Cannon MF, Weems CF. Do anxiety and depression cluster into distinct groups?: a test of tripartite model predictions in a community sample of youth. Depression & Anxiety. 2006;23(8):453–460. doi: 10.1002/da.20215. http://dx.doi.org/10.1002/da.20215. [DOI] [PubMed] [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS Scales. Journal of Personality and Social Psychology. 1994;67(2):319–333. http://dx.doi.org/10.1037/0022-3514.67.2.319. [Google Scholar]
- Ceyhan A. Relationship between early separation anxiety and depressive symptoms: the mediating role of locus of control and problem solving skills. Pakistan Journal of Social and Clinical Psychology. 2009;7(1):3. [Google Scholar]
- Chorpita BF, Albano AM, Barlow DH. The structure of negative emotions in a clinical sample of children and adolescents. The Journal of Abnormal Psychology. 1998;107(1):74–85. doi: 10.1037//0021-843x.107.1.74. [DOI] [PubMed] [Google Scholar]
- Clark DA, Beck AT, Stewart BL. Cognitive specificity and positive-negative affectivity: complementary or contradictory views on anxiety and depression? The Journal of Abnormal Psychology. 1990;99(2):148–155. doi: 10.1037//0021-843x.99.2.148. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psycho-metric evidence and taxonomic implications. The Journal of Abnormal Psychology. 1991;100(3):316–336. doi: 10.1037//0021-843x.100.3.316. http://dx.doi.org/10.1037/0021-843X.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. Can personality assessment predict future depression? A twelve-month follow-up of 631 subjects. Journal of Affective Disorders. 2006;92(1):35–44. doi: 10.1016/j.jad.2005.12.034. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13(2):99–125. http://dx.doi.org/10.1111/j.1559-1816.1983.tb02325.x. [Google Scholar]
- Graham JW. Structural equation modeling. The Pennsylvania State University; 2005. Unpublished manuscript. [Google Scholar]
- Grunhaus L. Clinical and psychobiological characteristics of simultaneous panic disorder and major depression. American Journal of Psychiatry. 1988;145(10):1214–1221. doi: 10.1176/ajp.145.10.1214. [DOI] [PubMed] [Google Scholar]
- Harris AE, Curtin L. Parental perceptions, early maladaptive schemas, and depressive symptoms in young adults. Cognitive Therapy and Research. 2002;26(3):405–416. [Google Scholar]
- Harris KM, Udry JR. National Longitudinal Study of Adolescent Health (Add Health), 1994–2008. Inter-university Consortium for Political and Social Research (ICPSR); 2013. (distributor) [Google Scholar]
- Hartig T, van den Berg AE, Hagerhall CM, Tomalak M, Bauer N, Hansmann R, et al. Forests, trees, and human health. New York, NY: Springer Netherlands; 2011. Health benefits of nature experience: psychological, social and cultural processes. [Google Scholar]
- Jacobson NC, Newman MG. The temporal relationship between anxiety and depression: a meta-analysis. Paper presented at the Association for Behavioral and Cognitive Therapies; 18 November 2012; National Harbor, Maryland. 2012a. [Google Scholar]
- Jacobson NC, Newman MG. Anxiety as a temporal predictor of depression during brief time periods: an ecological momentary assessment. Paper presented at the Association for Behavioral and Cognitive Therapies; National Harbor, Maryland. 2012b. [Google Scholar]
- Joiner T., Jr A confirmatory factor-analytic investigation of the tripartite model of depression and anxiety in college students. Cognitive Therapy and Research. 1996;20(5):521–539. http://dx.doi.org/10.1007/BF02227911. [Google Scholar]
- Joiner TE, Katz J, Lew A. Harbingers of depressotypic reassurance seeking: negative life events, increased anxiety, and decreased self-esteem. Personality and Social Psychology Bulletin. 1999;25(5):632–639. http://dx.doi.org/10.1177/0146167299025005008. [Google Scholar]
- Jolly JB, Dyck MJ, Kramer TA, Wherry JN. Integration of positive and negative affectivity and cognitive content-specificity: improved discrimination of anxious and depressive symptoms. The Journal of Abnormal Psychology. 1994;103(3):544–552. doi: 10.1037//0021-843x.103.3.544. [DOI] [PubMed] [Google Scholar]
- Jolly JB, Kramer TA. The hierarchical arrangement of internalizing cognitions. Cognitive Therapy & Research. 1994;18(1):1–14. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: user’s reference guide. Lincolnwood, IL: Scientific Software International; 1996. [Google Scholar]
- Kendler KS. Major depression and generalised anxiety disorder same genes, (partly) different environments—revisited. British Journal of Psychiatry. 1996;168(Suppl 30):68–75. http://dx.doi.org/10.1192/bjp.168.1.68. [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and generalized anxiety disorder: same genes, (partly) different environments? Archives of General Psychiatry. 1992;49(9):716–722. doi: 10.1001/archpsyc.1992.01820090044008. http://dx.doi.org/10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang PE, Wittchen HU, Ustun TB, Roy-Burne PP, Walters EE. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Archives of General Psychiatry. 1998;55(9):801. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. Engagement in pleasant activities and depression level. The Journal of Abnormal Psychology. 1975;84(6):729–731. doi: 10.1037//0021-843x.84.6.729. http://dx.doi.org/10.1037/0021-843x.84.6.729. [DOI] [PubMed] [Google Scholar]
- Lin FJ. Solving multicollinearity in the process of fitting regression model using the nested estimate procedure. Quality & Quantity. 2008;42(3):417–426. http://dx.doi.org/10.1007/s11135-006-9055-1. [Google Scholar]
- Lockefeer JPM, De Vries J. What is the relationship between trait anxiety and depressive symptoms, fatigue, and low sleep quality following breast cancer surgery? Psycho-Oncology. 2013;22:1127–1133. doi: 10.1002/pon.3115. http://dx.doi.org/10.1002/pon.3115. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod AK, Byrne A. Anxiety, depression, and the anticipation of future positive and negative experiences. The Journal of Abnormal Psychology. 1996;105(2):286–289. doi: 10.1037//0021-843x.105.2.286. http://dx.doi.org/10.1037/0021-843x.105.2.286. [DOI] [PubMed] [Google Scholar]
- McDonald RP, Marsh HW. Choosing a multivariate model: noncentrality and goodness of fit. Psychological Bulletin. 1990;107(2):247. [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. http://dx.doi.org/10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moitra E, Herbert JD, Forman EM. Behavioral avoidance mediates the relationship between anxiety and depressive symptoms among social anxiety disorder patients. Journal of Anxiety Disorders. 2008;22(7):1205–1213. doi: 10.1016/j.janxdis.2008.01.002. http://dx.doi.org/10.1016/j.janxdis.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Morgan CD, Wiederman MW, Magnus RD. Discriminant validity of the SCL-90 dimensions of anxiety and depression. Assessment. 1998;5(2):197–201. doi: 10.1177/107319119800500210. http://dx.doi.org/10.1177/107319119800500210. [DOI] [PubMed] [Google Scholar]
- Needles DJ, Abramson LY. Positive life events, attributional style, and hopefulness: testing a model of recovery from depression. The Journal of Abnormal Psychology. 1990;99(2):156–165. doi: 10.1037//0021-843x.99.2.156. http://dx.doi.org/10.1037/0021-843X.99.2.156. [DOI] [PubMed] [Google Scholar]
- Nesse RM, Williams GC. Why we get sick: the new science of Darwinian medicine. New York, NY: Vintage; 1996. [Google Scholar]
- Norton S, Cosco T, Doyle F, Done J, Sacker A. The hospital anxiety and depression scale: a meta confirmatory factor analysis. Journal of Psychosomatic Research. 2013;74(1):74–81. doi: 10.1016/j.jpsychores.2012.10.010. http://dx.doi.org/10.1016/j.jpsychores.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, et al. Mental disorders and disability among patients in a primary care group practice. American Journal of Psychiatry. 1997;154(12):1734. doi: 10.1176/ajp.154.12.1734. [DOI] [PubMed] [Google Scholar]
- Ottenbreit ND, Dobson KS. Avoidance and depression: the construction of the Cognitive-Behavioral Avoidance Scale. Behaviour Research and Therapy. 2004;42(3):293–313. doi: 10.1016/S0005-7967(03)00140-2. http://dx.doi.org/10.1016/s0005-7967(03)00140-2. [DOI] [PubMed] [Google Scholar]
- Pfeiffer PN, Ganoczy D, Ilgen M, Zivin K, Valenstein M. Comorbid anxiety as a suicide risk factor among depressed veterans. Depression and Anxiety. 2009;26(8):752–757. doi: 10.1002/da.20583. http://dx.doi.org/10.1002/da.20583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant EA, Devine PG. The antecedents and implications of interracial anxiety. Personality and Social Psychology Bulletin. 2003;29(6):790–801. doi: 10.1177/0146167203029006011. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Richard DC, Lauterbach D. Handbook of exposure therapies. New York, NY: Academic Press; 2011. [Google Scholar]
- Rinck M, Rörtgen T, Lange WG, Dotsch R, Wigboldus DHJ, Becker ES. Social anxiety predicts avoidance behaviour in virtual encounters. Cognition and Emotion. 2010;24(7):1269–1276. [Google Scholar]
- Roberts ME, Fuemmeler BF, McClernon FJ, Beckham JC. Association between trauma exposure and smoking in a population-based sample of young adults. Journal of Adolescent Health. 2008;42(3):266–274. doi: 10.1016/j.jadohealth.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(5):561–570. doi: 10.1097/01.CHI.0000046822.95464.14. http://dx.doi.org/10.1097/01.chi.0000046822.95464.14. [DOI] [PubMed] [Google Scholar]
- Seligman LD, Ollendick TH. Comorbidity of anxiety and depression in children and adolescents: an integrative review. Clinical Child and Family Psychology Review. 1998;1(2):125–1125. doi: 10.1023/a:1021887712873. http://dx.doi.org/10.1023/a:1021887712873. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Klein DN. Dimensional diagnosis of depression: adding the dimension of course to severity, and comparison to the DSM. Comprehensive Psychiatry. 2002;43(6):420–426. doi: 10.1053/comp.2002.35902. http://dx.doi.org/10.1053/comp.2002.35902. [DOI] [PubMed] [Google Scholar]
- Shear MK, Bjelland I, Beesdo K, Gloster AT, Wittchen HU. Supplementary dimensional assessment in anxiety disorders. International Journal of Methods in Psychiatric Research. 2007;16(S1):S52–S64. doi: 10.1002/mpr.215. http://dx.doi.org/10.1002/mpr.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Wells KB, Meredith LS, Jackson CA, Camp P. Comorbid anxiety disorder and the functioning and well-being of chronically ill patients of general medical providers. Archives of General Psychiatry. 1996;53(10):889. doi: 10.1001/archpsyc.1996.01830100035005. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Roelofs K, Hovens JGFM, Elzinga BM, van Oppen P, Zitman FG, et al. Personality, life events and the course of anxiety and depression. European Journal of Personality. 2011;25:443–452. [Google Scholar]
- Starr LR, Davila J. Temporal patterns of anxious and depressed mood in generalized anxiety disorder: a daily diary study. Behaviour Research and Therapy. 2012a;50:131–141. doi: 10.1016/j.brat.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Davila J. Cognitive and interpersonal moderators of daily co-occurrence of anxious and depressed moods in generalized anxiety disorder. Cognitive Therapy and Research. 2012b;36:655–669. doi: 10.1007/s10608-011-9434-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Beck AT. Beck Anxiety Inventory. San Antonio, TX: Pearson Education Inc; 1997. [Google Scholar]
- Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivariate Behavioral Research. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Sundel M, Sundel SS. Behavior change in the human services: behavioral and cognitive principles and applications. Thousand Oaks, CA: SAGE Publications, Incorporated; 2004. [Google Scholar]
- Swendsen JD. Anxiety, depression, and their comorbidity: an experience sampling test of the helplessness–hopelessness theory. Cognitive Therapy & Research. 1997;21(1):97–114. [Google Scholar]
- Swendsen JD. The helplessness–hopelessness theory and daily mood experience: an idiographic and cross-situational perspective. Journal of Personality and Social Psychology. 1998;74(5):1398–1408. http://dx.doi.org/10.1037/0022-3514.74.5.1398. [Google Scholar]
- Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. http://dx.doi.org/10.1002/jts.2490090305. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1985. [Google Scholar]
- Tryon WW. Possible mechanisms for why desensitization and exposure therapy work. Clinical Psychology Review. 2005;25(1):67–95. doi: 10.1016/j.cpr.2004.08.005. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. [Google Scholar]
- Walsemann KM, Bell BA, Goosby BJ. Effect of school racial composition on trajectories of depressive symptoms from adolescence through early adulthood. Race and Social Problems. 2011;3(3):131–145. http://dx.doi.org/10.1007/s12552-011-9053-3. [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. The Journal of Abnormal Psychology. 2005;114(4):522–536. doi: 10.1037/0021-843X.114.4.522. http://dx.doi.org/10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. The Journal of Abnormal Psychology. 1995;104(1):15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. The Journal of Abnormal Psychology. 1995;104(1):3–14. doi: 10.1037//0021-843x.104.1.3. http://dx.doi.org/10.1037/0021-843X.104.1.3. [DOI] [PubMed] [Google Scholar]
- Wax Y. Collinearity diagnosis for a relative risk regression analysis: an application to assessment of diet-cancer relationship in epidemiological studies. Statistics in Medicine. 1992;11(10):1273–1287. doi: 10.1002/sim.4780111003. http://dx.doi.org/10.1002/sim.4780111003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. American Journal of Epidemiology. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Wilson KA, Hayward C. A prospective evaluation of agoraphobia and depression symptoms following panic attacks in a community sample of adolescents. Journal of Anxiety Disorders. 2005;19(1):87–103. doi: 10.1016/j.janxdis.2003.11.001. http://dx.doi.org/10.1016/j.janxdis.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Becker E, Lieb R, Krause P. Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychological Medicine. 2002;32(1):119–132. doi: 10.1017/s0033291701004925. http://dx.doi.org/10.1017/S0033291701004925. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Kessler RC, Pfister H, Höfler M, Lieb R. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatrica Scandinavica. 2000;102:14–23. http://dx.doi.org/10.1111/j.0065-1591.2000.acp29-03.x. [PubMed] [Google Scholar]
- Wu AD, Zumbo BD. Understanding and using mediators and moderators. Social Indicators Research. 2008;87(3):367–392. http://dx.doi.org/10.2307/27734670. [Google Scholar]
- Youden W. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]