A paper by Nuno Bernardes et al.1 entitled “Modulation of membrane properties of lung cancer cells by azurin enhances the sensitivity to EGFR-targeted therapy and decreased β1 integrin mediated adhesion” in this volume of Cell Cycle aims to gain a better understanding about the mechanism of action of azurin as a therapeutic protein for cancer treatment. Prior to this publication, Dr. Fialho's group reported that azurin targets P-cadherin overexpression in a subset of breast cancer, antagonizing its pro-invasive effects. They found that azurin decreases the hyper-phosphorylation of FAK and Src non-receptor tyrosine kinases associated to P-cadherin overexpression. They also performed a microarray analysis of azurin treated cells observing a decrease in the expression of several genes coding for membrane receptors associated to cell signaling, particularly receptor tyrosine kinases and chemokine receptors.2
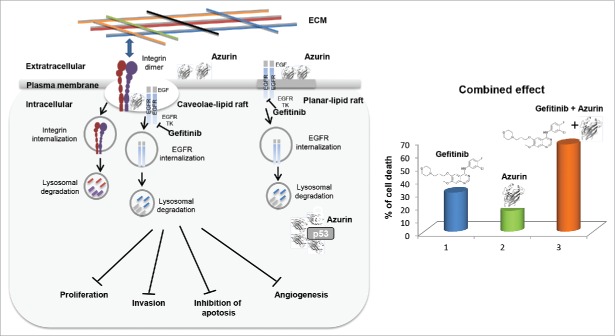
In this Cell Cycle paper, Bernardes et al. have evaluated the effects of azurin on Non-small cell lung cancer (NSCLC) cells with regard to their gene expression profile. Altogether this paper provides new evidence supporting the anticancer effects of this bacterial protein across several cancer cell lines. They show that azurin modulates the levels and localization of integrin beta1, affecting the downstream signaling cascade and the invasiveness of NSCLC A549 cells. Moreover they present evidence that combined treatments of azurin with gefitinib and erlotinib (tyrosine kinase inhibitors targeting the Epidermal Growth Factor Receptor EGFR) enhance the sensitivity of lung cancer cells to these molecules. Finally, by using Atomic Force Microscopy (AFM), the authors analyzed the cancer cell surface following treatments with azurin and/or gefitinib, measuring the changes on morphological and mechanical properties of the cells. These changes included increases in cell mass, height, volume and elasticity. The overall changes in the membrane properties seem to revert the carcinogenic phenotype, allowing cancer cells to adopt a more “epithelial-like” behavior, becoming less invasive (Fig. 1, left). Taken together these findings have significant relevance and may pave the way of using azurin as an adjuvant to improve the efficacy of chemotherapeutic drugs (Fig. 1, right).
Figure 1.
[Left] Gefitinib binds to the intracellular enzyme (tyrosine kinase) of the EGFR ultimately inducing anti-proliferative effects. Azurin binds to cancer cells through binding to lipid raft components and cell-surface receptors. Upon entry, azurin interferes in cancer cell growth by multiple mechanisms including complex formation with p53. [Right] A dual therapy has demonstrated that azurin enhances the sensitivity of the anticancer drug Gefitinib.
It is important in this context to realize that azurin had previously been shown not only to reduce the invasiveness of breast and the proliferation of lung cancer cells as mentioned above, but in xeno-transplanted mice harboring melanoma and breast tumors, intravenous injections of azurin led to significant tumor regression in vivo in such mice through complex formation and stabilization of the tumor suppressor protein p53.3 In addition, azurin not only demonstrates anticancer activity, but also has strong activity against viruses such as the HIV/AIDS virus HIV-1 and parasites such as the malarial parasite Plasmodium falciparum4 and the opportunistic parasite Toxoplasma gondii.5 A 28-amino acid fragment of azurin, termed p28, in a phase I clinical trial in the United States has not only demonstrated no toxicity but significant tumor regressing effects in 15 stage IV cancer patients with refractory solid tumors, substantially prolonging the lives of some patients and allowing both partial and complete regression of these refractory tumors in such patients.6 In a second phase I trial in a number of hospitals, p28 has shown similar lack of toxicity but significant efficacy in pediatric patients with brain tumors (http://clinicaltrials.gov/ct2/show/NCT01975116), allowing the USFDA to approve the designation of p28 as an orphan drug for the treatment of glioma. Azurin is known to have other domains (azurin 88–113) besides the p28 domain (azurin 50–77) with strong anticancer activity through binding with the cell surface EphB2 receptors and interfering in their cancer growth promotion.7 Will azurin be a better and more effective drug in cancer therapy if its lack of toxicity but significant efficacy in clinical trials in cancer patients can be demonstrated? This paper by Bernardes et al.1 in this issue of Cell Cycle is a significant step toward this direction.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- [1].Bernardes N., et al.. Cell Cycle 2016; 15(11):1415-24; PMID: 27096894; http://dx.doi.org/ 10.1080/15384101.2016.1172147) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bernardes N. et al.. Int J Biochem Cell Biol 2014; 50:1-9; PMID:24509127; http://dx.doi.org/ 10.1016/j.biocel.2014.01.023 [DOI] [PubMed] [Google Scholar]
- [3].Yamada T., et al.. Proc Natl Acad Sci 2004; 101:4770-5; PMID:15044691; http://dx.doi.org/ 10.1073/pnas.0400899101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chaudhari A., et al.. Cell Cycle 2006; 5:1642-8; PMID:16861897; http://dx.doi.org/ 10.4161/cc.5.15.2992 [DOI] [PubMed] [Google Scholar]
- [5].Naguleswaran A., et al.. Antimicrob Agents Chemotherap 2008; 52:402-8; PMID:18070964; http://dx.doi.org/ 10.1128/AAC.01005-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Warso MA, et al.. Brit J Cancer 2013; 108:1061-70; PMID:23449360; http://dx.doi.org/ 10.1038/bjc.2013.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chaudhari A, et al.. Biochemistry 2007; 46:1799-1810; PMID:17249693; http://dx.doi.org/ 10.1021/bi061661x [DOI] [PubMed] [Google Scholar]