Abstract
Background
Examining responders and non-responders to behavioral lifestyle interventions among overweight/obese adults with additional comorbidities may aid in refining and tailoring obesity treatment.
Purpose
The purpose of this study is to demonstrate the use of latent class analysis to identify patterns of response to behavioral lifestyle interventions based on adherence to diet and exercise recommendations.
Method
Repeated measures latent class analysis was applied to two clinical trial datasets, combination of two active interventions in the PREMIER Trial (n=501) and phase 1 of the Weight Loss Maintenance Trial (WLM; n=1685), to identify patterns of response to behavioral lifestyle interventions. Treatment response was based on adherence to daily recommendations for fruit/vegetable, fat, saturated fat, sodium, and exercise at baseline and 6 months.
Results
In PREMIER, three distinct latent classes emerged: responders (45.9 %), non-responders (23.6 %), and early adherers (30.5 %). Responders and Early Adherers had greater weight loss at 6 and 18 months and were more likely to meet behavioral recommendations at 18 months than Non-responders. For WLM, there were four latent classes: partial responders (16 %), non-responders (40 %), early adherers (2 %), and fruit/veggie only responders (41 %). Non-responders in WLM had significantly less weight loss at 6 months compared to that of the other three latent classes.
Conclusion
Latent class analysis is a useful method to apply to clinical trial data to identify distinct patterns of response to behavioral interventions. Overweight/ obese participants who respond to behavioral lifestyle treatment (i.e., meet behavioral recommendations) have significantly greater weight loss than that of participants who do not make behavioral changes.
Keywords: Lifestyle intervention, Treatment response, Behavior change, Latent class analysis
Introduction
Behavioral lifestyle interventions are generally effective treatments for obesity with mean losses of 8–10 % of initial weight in clinical trials [1, 2]. However, when considering translation and dissemination of these lifestyle interventions into clinical practice, it is important to understand not only if the intervention is efficacious at the group level, but also for whom it is most effective. Examining who responds versus does not respond to current lifestyle interventions may aid in the refining and tailoring of obesity treatment to individual needs.
Effectiveness of a lifestyle intervention is often determined by a specific criterion for the clinical outcome of interest. In obesity treatment, individuals who lose 5 % or greater of their initial weight either during active intervention or by the end of the intervention are generally considered responders to treatment [3, 4]. Individuals who do not complete the intervention or who lose <5 % of their initial weight are described as non-responders [4]. However, defining response to a behavioral lifestyle intervention only in terms of weight outcomes may not provide a complete description of intervention efficacy. The direct outcome of any successful behavioral lifestyle intervention is behavior change (e.g., consuming a healthier diet and increasing physical activity), and improvements in clinical outcomes are a result of these behavioral changes. Thus, whether or not an individual meets the behavioral goals (e.g., diet and exercise recommendations) specified by the lifestyle intervention program should also be considered an indicator of treatment response.
There are typically multiple behavioral recommendations for participants to meet over the course of a behavioral life-style intervention. Thus, classifying participants as responders or non-responders becomes more complex because treatment response is defined by multiple behaviors. Latent class analysis (LCA) is a person-centered, model-based approach that can be used to examine unique clusters of individuals that have a similar response pattern across multiple characteristics [5, 6] Traditional analytic approaches (e.g., factor analysis) focus on relationships among variables. In contrast, the focus in LCA is on the relationship among persons within the sample. Individuals are classified based on the probability of belonging to a certain latent class [5].
In this secondary data analysis, LCA was applied to two multi-center randomized clinical trial datasets (PREMIER [7, 8] and Weight Loss Maintenance [9]) to determine if we could identify distinct subgroups of overweight/ obese participants based on their patterns of behavioral response to a behavioral lifestyle intervention. Only participants with body mass index ≥25 kg/m2 in each trial were included in the secondary analyses. Response to treatment was based on adherence to daily diet and exercise recommendations specified in each trial over 6 months. In addition to identifying distinct subgroups based on behavioral response, we compared these groups on weight outcomes. We applied LCA because we wanted to examine response to behavioral life-style intervention based on multiple indicators of treatment response. An advantage to using LCA is that multiple characteristics that classify individuals into subgroups can be examined simultaneously instead of examining each characteristic separately, which may increase the chance for type 1 error [6]. LCA provides the ability to examine the effect of meeting multiple behavioral recommendations, but does not limit the ability to identify which specific behavioral recommendations participants were able to achieve.
Methods
We conducted secondary data analysis using PREMIER and phase 1 of the Weight Loss Maintenance Trial (WLM) because the behavioral interventions implemented in these two trials are considered traditional behavioral lifestyle interventions as they provide nutrition education, emphasize increase in physical activity, and teach participants behavioral strategies including goal setting, self-monitoring, and problem solving [10].
PREMIER Trial (Study 1)
Study design, participants, and procedures for PREMIER have been described previously [7, 11]. In summary, PREMIER was a four-center, randomized clinical trial designed to test the effects of lifestyle modification on blood pressure, weight, and diet among adults ages 25 and older with either prehypertension or stage 1 hypertension. Participants were randomly assigned to one of three conditions: 1) an “advice only” condition (not included in our analyses); 2) a lifestyle intervention referred to as “Established,” that included weight loss, physical activity, and sodium reduction lifestyle recommendations; or 3) “Established plus DASH,” a lifestyle intervention that consisted of the established intervention plus promotion of the Dietary Approaches to Stop Hypertension (DASH) diet [12, 13]. The Established and Established plus DASH diet interventions occurred over 18 months. Both lifestyle interventions consisted of 18 face-to-face sessions (14 groups and 4 individuals) over the first 6 months and 15 face-to-face sessions (12 groups and 3 individuals) for the remaining 12 months. Sessions were held weekly in the first 3 months, biweekly for the next 3 months, and monthly through 18 months.
For the current analyses, we combined participants randomized to the Established or Established + DASH conditions into one group and only included participants with a body mass index (BMI) ≥25 kg/m2 (n = 501). In both active intervention conditions, participants were provided with the same educational materials on weight loss, physical activity, and sodium. Also, both interventions emphasized self-monitoring of diet and exercise as well as goal setting with action plans, problem solving, relapse prevention, and social support through group interactions. The Established plus DASH intervention differed in terms of dietary education (specific to DASH diet recommendations) and food groups that were self-monitored. Participants from both interventions monitored total calories, sodium, and physical activity minutes, whereas the Established plus DASH also monitored fruit and vegetable servings and total fat intake. Table 1 presents the specific dietary and exercise recommendations for the Established and Established plus DASH intervention conditions.
Table 1.
Diet and exercise goals for PREMIER lifestyle interventions
| Established | Established + DASH Goals used in RMLCA for WLM |
Goals used in RMLCA for PREMIERa |
|
|---|---|---|---|
| Sodium intake | ≤2300 mg/day | ≤2300 mg/day | ≤2300 mg/day |
| Fat intake | ≤30 % of total energy | ≤25 % of total energy | ≤30 % of total energy |
| Saturated fat intake | – | ≤7 % of total energy | ≤10 % of total energy |
| Fruit/vegetable intake | – | 9–12 servings/day | ≤5 servings/day |
| Physical activity | 180 min/week of moderate intensity | 180 min/week of moderate intensity | 180 min/week of moderate intensity |
WLM Weight Loss Maintenance
For the repeated measures latent class analysis (RMLCA) for PREMIER, participants from both intervention conditions were combined; therefore, the goals were modified to be more modest, but consistent with national recommendations
Participants who were randomized to the Established or Established + DASH conditions had significantly greater weight loss, blood pressure reduction, and improvement in dietary intake compared to that of participants in the advice-only condition at 6- and 18-month follow-up [7, 8]. Despite intervention differences between the Established and Established + DASH, there was no significant difference in the amount of weight loss between the two intervention conditions at 6 [7] or 18 months [8].
Weight Loss Maintenance Trial (Study 2)
The Weight Loss Maintenance Trial (WLM) [9] was also a multi-center trial designed to compare two active strategies (interactive technology and personal contact) to a self-directed approach for weight loss maintenance among overweight/obese adults who were also taking medications for hypertension, dyslipidemia, or both. In phase 1 of WLM, 1685 participants were enrolled in a 6-month intensive behavioral lifestyle intervention [14]. The intensive behavioral lifestyle intervention consisted of 20-weekly, 2-h group sessions over the course of 6 months. Group sessions were supplemented with occasional individual contacts by phone or in person to assist participants with specific behavioral changes. Session content was similar to the material used in the Established + DASH intervention in PREMIER (study 1) and focused on goal setting, nutrition and physical activity education, problem solving, and social support. Participants were asked to follow the DASH diet [12, 13] and self-monitor dietary intake and minutes of physical activity daily.
Participants who lost ≥4 kg at the end of phase1 were then randomized to one of three maintenance strategies in phase 2 (n=1032): 1) self-directed, 2) interactive technology, or 3) personal contact [9]. Although there was weight regain over 30 months across the three conditions, findings suggested that brief, monthly personal contacts provided some benefit for sustaining weight loss long term [9]. For the current analysis, we were interested in behavioral response to intensive behavioral lifestyle weight loss interventions; therefore, we only used data from phase 1 of WLM (n=1685).
Measures
PREMIER (Study 1)
Clinic weight measurements were collected at baseline, 6, and 18 months and were used to calculate 6- and 18-month percent change in weight. Data from the 6- and 18-month assessments was also used to calculate 12- month (i.e., between 6 and 18 months) percent change in weight. Two unannounced 24-h dietary recalls were administered via telephone by a trained staff at baseline, 6-, and 18- month follow-up visits to assess dietary intake [7]. A 7-day physical activity recall was administered at each clinic visit and used to calculate minutes in moderate-to-vigorous activity [15, 16]. Participants in the Established and Established plus DASH interventions were asked to record food and beverage intake and minutes of physical activity in a food and fitness diary at least 3 days each week. Frequency of self-monitoring was equal to the number of days in which participants kept food records and recorded minutes of exercise since their last intervention session summed over 6 months.
WLM (Study 2)
Clinic weight measurements during Phase 1 of WLM (study 2) were collected at baseline and 6 months. The Block Food Frequency Questionnaire [17] and accelerometry were used to assess usual dietary intake and minutes of physical activity, respectively, at baseline and 6- month follow-up. For the accelerometry, participants were asked to wear the accelerometer for at least 10 h per day for at least 4 days including 1 weekend day. Participants were also asked to keep a daily record of food intake and minutes of physical activity. Adherence to self-monitoring was based on the number of food and activity diaries participants turned in over the 20-week intervention.
Statistical Analysis
We used repeated measures LCA (RMLCA) [5] to identify distinct subgroups of participants based on their behavioral response to the PREMIER (study 1) or WLM (study 2) behavioral lifestyle interventions during the intensive phase of the interventions (initial 6 months). Behavioral response to treatment over 6 months was examined because that is the time period in which the most weight loss occurred in both trials. In the current analysis, the behaviors of interest (i.e., characteristics) consisted of four specific dietary and one physical activity recommendation. Because participants from the two active intervention conditions in PREMIER (study 1) were combined for these analyses, we modified the recommendations to be more modest to account for differences in dietary education and targets between the two interventions (see Table 1). Specifically, the fruit/vegetable intake recommendation was set at five or more servings per day to be consistent with the original food guide pyramid recommendations [18] and the recommendations for energy from total fat (≤30 % per day) and saturated fat (≤10 % per day) were based on the Established condition targets and were also consistent with national recommendations [18]. However, for WLM (study 2), because the DASH diet was emphasized, DASH-specific recommendations for fruit/vegetable (9–12 servings), fat (≤25 % energy from fat), and saturated fat (≤7 % energy from saturated fat) consumption were used in the analyses (see Table 1).
For both datasets, we created 10 binary variables (yes or no) to indicate for each participant whether he or she met the five diet and physical activity recommendations at baseline and at 6 months. Response to treatment was defined based on the pattern of responses (yes or no) across the five recommendations and across time (at baseline and at 6 months), rather than the change in number of recommendations met from baseline to 6 months. This definition allowed classification of individuals based on adherence to multiple health behaviors, while not sacrificing the ability to identify which specific behavioral recommendation(s), participants were able to achieve. The RMLCA models were run using Mplus version 7. With 10 indicators (5 behaviors at each time point), each with 2 response options (yes or no), there were 2^10=1024 different possible response patterns or latent classes. An advantage of using RMLCA is that it provides a parsimonious summary of a large contingency table such as this and outputs only the most common response patterns within the sample [5].
In RMLCA, there are two estimated parameters using maximum likelihood, latent class prevalence and item-response probability [5]. Latent class prevalence indicates the proportion of individuals who share a similar response pattern across the five behaviors and across time (i.e., belong to the same latent class). Item-response probability is the probability of meeting a behavioral recommendation given the response pattern or latent class membership. For the current analysis, item-response probabilities <0.5 indicated that the given class had a low probability of meeting the specified behavioral recommendation at that time point; item-response probabilities ≥0.5 indicated that the class had a high probability of meeting the behavioral recommendation. RMLCA models with one to five latent classes (i.e., response patterns) were estimated. Fit indices were examined to aid in selection of the optimal model for the data. Specifically, better model fit was suggested by a lower Akaike information criterion (AIC) [19]; a lower Bayesian information criterion (BIC) [20]; a significant Lo-Mendell-Rubin likelihood ratio test, suggesting the more complex model (i.e., model with more patterns) fits the data better than the model with fewer patterns [21]; entropy, the estimate of certainty of classification (ranging from 0 to 1); and meaningfulness or interpretability of the response patterns.
To further distinguish the subgroups that emerged from the RMLCA, in PREMIER (study 1), we compared them on 6- and 18-month percent change in weight as well as proportion meeting the five diet and exercise recommendations at 18 months. For WLM (study 2), we compared the subgroups on 6-month percent change in weight.
Results
PREMIER (Study 1)
Among the 501 participants included in the analysis of PREMIER (study 1) data, 61 % were female, 35 % self-reported Black/African American, 1.8 % self-reported White Hispanic (remaining participants self-reported White/ Caucasian as their race/ethnicity), 32 % with BMI 25–29.9 kg/m2, and 68 % with BMI ≥30 kg/m2. Mean (SD) age was 50 (8.7) years. Participants, on average, attended 12 of the 18 intervention sessions (67 %) during the initial 6 months and 10 of the 15 intervention sessions (67 %) over the next 12 months. Across the behaviors, there was a 22–35 % increase in number of participants meeting the recommendations from baseline to 6 months, with the largest increase occurring in the number of participants meeting recommendations to reduce sodium intake to <2300 mg and limit energy from total fat to ≤30 % of energy (both had a 35 % increase). The lowest overall percent increase was for the number meeting the physical activity recommendation of 180 minutes of moderate activity per week.
RMLCA—Model Selection
After examining a series of latent class models and comparing them on the fit indices and meaningfulness (see Table 2), a three-class model was selected and interpreted. The classes represent behavioral adherence patterns across the five behaviors over the initial 6 months of the intervention and correspond to common response to treatment patterns within the sample. In RMLCA, a posterior probability is estimated for each participant, which indicates the probability that the individual belongs to a certain class. The average posterior probability for each of the three classes was ≥0.85, suggesting that on average, participants were appropriately classified in each class [5].
Table 2.
Repeated measures latent class analysis model estimation fit indices for PREMIER
| Pattern | AIC ↓ | BIC ↓ | LMRT (p<.05) | Entropy (0–1) |
|---|---|---|---|---|
| 1 | 5964.82 | 6006.98 | – | – |
| 2 | 5677.27 | 5765.81 | p<.001 | .79 |
| 3 | 5513.30 | 5648.23 | p=.22 | .78 |
| 4 | 5481.90 | 5663.211 | p=.01 | .79 |
| 5 | 5465.86 | 5693.55 | p=.81 | .79 |
Data in italics indicates the best fitting model relative to the other models tested
LMRT Lo-Mendell-Rubin Test
Nearly half of the participants (n=230; 45.9 %) are classified as “Responders” as they did not meet any of the behavioral recommendations at baseline (item-response probabilities <0.5), but had a high probability of meeting all the recommendations at 6-month follow-up (see Table 3). Thirty percent of the participants (n=153) were already meeting three dietary recommendations (i.e., fruit/vegetable intake, energy from total fat, and energy from saturated fat) at baseline and continued to do so at 6 months, but did not meet the sodium intake and physical activity recommendations until the 6-month follow-up. This subgroup of participants is referred to as the “Early Adherers” given that they were already meeting three of the recommendations at baseline and continued to meet these along with two additional recommendations at 6 months. Finally, the third class of participants (n=118;23.6 %) are described as “Non-Responders” as they had a low probability of meeting any of the behavioral recommendations at baseline and at 6 months. Table 4 presents similar data to Table 3, but provides further details on the mean amount of each macronutrient or food group consumed and minutes of moderate intensity physical activity for each class at baseline and 6 months based on the 24-h dietary and 7-day physical activity recalls administered.
Table 3.
Latent classes of behavioral response to PREMIER lifestyle interventions: behavioral response patterns
| Responders (n=230, 45.9 %) |
Early adherers (n=153, 30.5 %) |
Non-responders (n=118, 23.6 %) |
||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Baseline | 6 months | Baseline | 6 months | |
| Sodium ≤2300 mg/day | No (p=.19) | Yes (ρ=.64) | No (p=.38) | Yes (ρ=.72) | No (p=.15) | No (p=.37) |
| Fat ≤30 % of total energy | No (p=.05) | Yes (ρ=.98) | Yes (ρ=.89) | Yes (ρ=.81) | No (p=.06) | No (p=.00) |
| Saturated fat ≤10 % of total energy | No (p=.19) | Yes (ρ=.93) | Yes (ρ=.91) | Yes (ρ=.78) | No (p=.13) | No (p=.22) |
| ≥5 servings of fruit and vegetables/day | No (p=.31) | Yes (ρ=.72) | Yes (ρ=.52) | Yes (ρ=.75) | No (p=.30) | No (p=.35) |
| 180 min/week of moderate physical activity | No (p=.36) | Yes (ρ=.61) | No (p=.46) | Yes (ρ=.71) | No (p=.37) | No (p=.49) |
Rho (ρ) is the item-response probability (i.e., probability that recommendation is met at given time point for the given latent class). Rho (ρ)>0.5 indicates high probability of meeting recommendations (<0.5 indicates low probability of meeting recommendations). No covariates were included in this repeated measures latent class model
Table 4.
Means (SE) of behavioral indicators at baseline and 6 months by latent class for PREMIER
| Responders |
Early adherers |
Non-responders |
||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | Baseline | 6 months | Baseline | 6 months | |
| Sodium (mg/day) | 3285.14 (89.28) | 2147.56 (71.26) | 2701.72 (93.39) | 2005.36 (81.42) | 3531.23 (124.98) | 2802.90 (108.04) |
| Percent energy from total fat | 36.82 (.43) | 22.57 (.47) | 25.50 (.47) | 23.23 (.79) | 37.64 (.57) | 37.00 (.46) |
| Percent energy from saturated fat | 12.26 (.19) | 7.13 (.17) | 8.03 (.17) | 7.30 (.31) | 12.50 (.23) | 12.27 (.26) |
| Servings of fruit and vegetables/day | 4.21 (.16) | 7.06 (.26) | 5.34 (.22) | 7.15 (.28) | 4.05 (.20) | 4.45 (.21) |
| Minutes/week of moderate physical activity |
212.15 (27.91) | 267.62 (21.62) | 232.31 (22.41) | 316.65 (26.35) | 215.44 (34.44) | 214.82 (23.59) |
No covariates were included in this repeated measures latent class model
We also conducted equality tests of means across the classes using the auxiliary e function within Mplus [22] to better characterize the three classes on number of sessions attended in the first 6 months and number of days of self-monitoring diet and exercise over the first 6 months. The overall test comparing mean session attendance across the classes was significant (χ2 = 14.67, p = .001); Early Adherers and Responders attended, on average, significantly more sessions compared to that of Non-responders (13 versus 11 sessions, respectively; p<.001). In terms of dietary self-monitoring, Early Adherers and Responders (both 74 days on average) monitored food and beverage intake on significantly more days over 6 months compared to that of Non-responders (54 days on average), overall p < .001. Early Adherers (66 days on average) and Responders (64 days on average) also self-monitored minutes of physical activity on significantly more days than that of Non-responders (48 days on average), overall p<.01.
Comparison of Latent Classes on Weight and Behavioral Outcomes
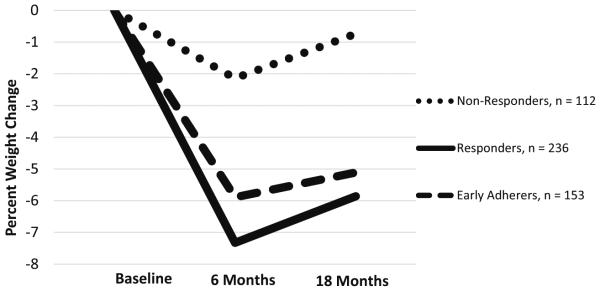
The three latent classes were compared on percent weight change from baseline to 6 months, 6 to 18 months, baseline to 18 months, and the proportion within each class meeting the five diet and exercise recommendations at 18- month follow-up. Figure 1 displays the mean percent weight change over 18 months for each latent class. Non-responders had a mean 6-month percent weight loss of −2.1 % (M=−3.92 kg, SE=.52), which was significantly lower than the weight loss for Early Adherers (M = −5.9 %, SE = .58; −5.24 kg, SE=.47, p<.001) and Responders (M=−7.3 %, SE=.50; −6.34 kg, SE=.43, p<.001). There was no significant difference in 6-month percent weight loss between Early Adherers and Responders. Participants, on average, across each latent class gained weight over the remaining 12 months of the intervention with Early Adherers gaining 0.78 %, Non-responders gaining 1.4 %, and Responders gaining 1.5 %; however, there was no significant difference among the classes in percent weight gain between 6- and 18-month follow-up. Over the entire 18 months of the intervention, Responders (M=−5.81 %, SE=.65, p<.001) and Early Adherers (M= −4.60 %, SE=.79, p=.005) had significantly greater weight loss compared to that of Non-responders (M = −1.88 %, SE=.49).
Fig. 1.
Mean percent weight change over 18 months for each latent class. Both Responders and Early Adherers had significantly greater weight loss than that of Non-responders at 6 and 18 months (p<.01)
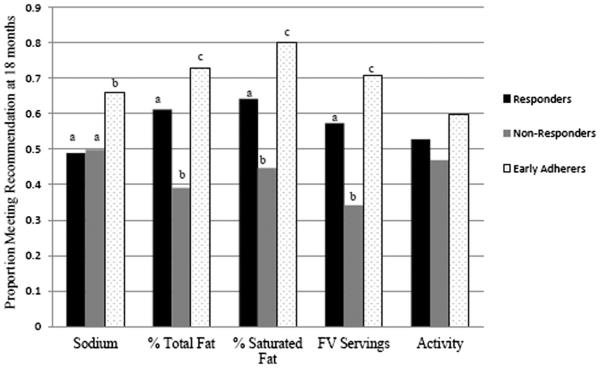
Figure 2 presents the proportion of participants within each latent class meeting the diet and physical activity recommendations at 18 months. Across all behaviors, Early Adherers had a higher proportion still meeting the recommendations at 18 months. Specifically, a significantly higher proportion of Early Adherers compared to Non-responders and Responders met the fruit/vegetable, percent energy from total fat, percent energy from saturated fat, and the sodium intake recommendations at 18 months. A significantly higher proportion of Responders met the percent energy from total fat, saturated fat, and fruit/vegetable intake recommendations compared to that of Non-responders. There was no significant difference among the classes on proportion meeting the moderate intensity physical activity recommendation of 180 minutes per week, which all fell approximately at or below 60 % of participants.
Fig. 2.
Proportion in each latent class meeting diet and exercise goals at 18 months in PREMIER. Different letters for same goal represent significant difference in proportions at p<.05 level. FV fruit/vegetable
WLM (Study 2)
In phase 1 of WLM (n=1685), 67 % of the participants were female, 44 % self-reported Black/African American race/ethnicity (remaining participants self-reported White/ Caucasian as race/ethnicity), and 79 % had a BMI ≥30 kg/ m2 [13]. Mean (SD) age was 54.8 (9.1) years. Participants, on average, attended 14 of the 20 intervention sessions (72 %). There was a 17–40 % increase in number of participants meeting the recommendations from baseline to 6 months, with the largest increase occurring in the number of participants consuming 9–12 servings of fruits and vegetables. The lowest overall percent increase was for the sodium intake recommendation of <2300 mg per day and the physical activity recommendation of 180 minutes of moderate activity per week.
RMLCA—Model Selection
After examining a series of latent class models and comparing them on the fit indices and meaningfulness (see Table 5), a four-class model was selected and interpreted for WLM (study 2). The average posterior probability for each of the four classes was ≥0.74. Approximately 16 % (n=272) of the participants are considered “Partial Responders” because they only met the sodium recommendation at baseline, but had a high probability of meeting the fruit/vegetable, total fat, saturated fat, and sodium intake recommendations at the 6-month follow-up (Table 6). Similar to PREMIER (study 1), phase 1 of WLM (study 2) also had a small number of participants considered Early Adherers (2 %, n=40) who were already meeting the total fat, saturated fat, and the sodium intake recommendations at baseline and met all of the recommendations except for physical activity at 6 months. Forty percent (n=677) of the participants were considered Non-responders because they did not meet any of the behavioral recommendations at baseline or 6 months with the exception of meeting the sodium intake recommendation at both baseline and 6 months. There was also another large subgroup that emerged among phase 1 WLM (study 2) participants described as “Fruit/Vegetable Only Responders” (41 %, n=696). These participants only met the fruit/vegetable recommendation at 6 months, but no other behavioral recommendations at either baseline or 6 months.tgroup1
Table 5.
Repeated measures latent class analysis model estimation fit indices for Weight Loss Maintenance Trial
| Pattern | AIC ↓ | BIC ↓ | LMRT (p<.05) | Entropy (0–1) |
|---|---|---|---|---|
| 1 | 12,707.83 | 12,762.13 | – | – |
| 2 | 12,118.26 | 12,232.28 | p<.001 | .60 |
| 3 | 11,901.07 | 12,074.81 | p<.001 | .52 |
| 4 | 11,805.72 | 12,039.19 | p=.04 | .60 |
| 5 | 11,747.88 | 12,041.08 | p>.05 | .64 |
Data in italics indicates the best fitting model relative to the other models tested
LMRT Lo-Mendell-Rubin Test
Table 6.
Latent classes of behavioral response to phase 1 Weight Loss Maintenance Trial behavioral lifestyle intervention
| Responders (n=272, 16 %) |
Early adherers (n=40, 2 %) |
Non-responders (n=677, 40 %) |
Fruit/vegetable-only responders (n=696, 41 %) |
|||||
|---|---|---|---|---|---|---|---|---|
| Baseline ρ M (SE) |
6 months ρ M (SE) |
Baseline ρ M (SE) |
6 months ρ M (SE) |
Baseline ρ M (SE) |
6 months ρ M (SE) |
Baseline ρ M (SE) |
6 months ρ M (SE) |
|
| Sodium ≤2300 mg/ day |
Yes (ρ=.60) 2332.68 (72.23) |
Yes (ρ=.83) 1739.96 (47.59) |
Yes (ρ=.84) 1781.71 (123.45) |
Yes (ρ=.86) 1832.18 (103.12) |
Yes (ρ=.70) 2131.90 (47.74) |
Yes (ρ=.93) 1640.26 (32.51) |
No (ρ=.15) 3382.52 (67.35) |
No (ρ=.26) 2788.38 (56.42) |
| Fat ≤25 % of total energy |
No (ρ=.00) 37.74 (.40) |
Yes (ρ=.79) 22.41 (.32) |
Yes (ρ=.79) 23.98 (1.00) |
Yes (ρ=.69) 23.49 (.78) |
No (ρ=.01) 39.26 (.32) |
No (ρ=.09) 32.35 (.37) |
No (ρ=.00) 40.47 (.31) |
No (ρ=.02) 33.51 (.32) |
| Saturated fat ≤7 % of total energy |
No (ρ=.05) 10.61 (.15) |
Yes (ρ=.87) 6.10 (.08) |
Yes (ρ=.80) 6.53 (.26) |
Yes (ρ=.72) 6.24 (.23) |
No (ρ=.02) 11.08 (.11) |
No (ρ=.04) 9.09 (.10) |
No (ρ=.00) 11.42 (.10) |
No (ρ=.08) 9.13 (.10) |
| 9–12 servings fruit/ veggies/day |
No (ρ=.09) 5.05 (.17) |
Yes (ρ=.73) 10.88 (.27) |
No (ρ=.28) 7.29 (.65) |
Yes (ρ=.64) 10.21 (.63) |
No (ρ=.02) 4.15 (.10) |
No (ρ=.21) 6.69 (.19) |
No (ρ=.15) 5.67 (.14) |
Yes (ρ=.60) 9.76 (.22) |
| 180 min/week moderate activity |
No (ρ=.17) 111.67 (7.18) |
No (ρ=.37) 169.62 (11.08) |
No (ρ=.17) 108.93 (15.78) |
No (ρ=.41) 183.26 (27.82) |
No (ρ=.18) 110.50 (4.93) |
No (ρ=.35) 168.36 (9.91) |
No (ρ=.23) 128.43 (5.71) |
No (ρ=.40) 169.64 (7.82) |
Rho (ρ) is the item-response probability (i.e., probability that recommendation is met at given time point for the given latent class). Rho (ρ)>0.5 indicates high probability of meeting recommendations (<0.5 indicates low probability of meeting recommendations). No covariates were included in this repeated measures latent class model
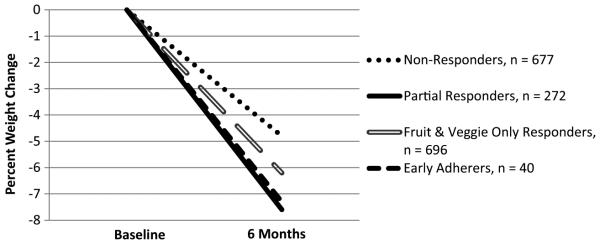
The overall test comparing mean session attendance across the classes was not significant (χ2 =4.84, p = .18). Non-responders and Fruit/Vegetable Responders attended, on average, 14 sessions, Partial Responders attended 15 sessions, and Early Adherers attended 16 of the 20 sessions. There was a significant overall difference in the number of food and physical activity diaries turned in over the 20 weeks (χ2 = 10.01, p=.02). Specifically, Early Adherers turned in significantly more diaries over 20 weeks (14 on average) than that of Non-responders (11 on average); otherwise, there were no other significant differences among the classes. Partial Responders completed 12 diaries on average and Fruit/ Vegetable Responders completed 11. Partial Responders (M = −7.6 %, SE = .85, p = .01; −6.52 kg, SE = .37), Early Adherers (M=−7.3 %, SE=.72, p<.01; −6.09 kg, SE=.73), and Fruit/Vegetable-Only Responders (M=−6.2 %, SE=.32, p<.01; −5.90 kg, SE=.25) all had significantly greater weight loss at 6 months compared to that of Non-responders (M= −4.8 %, SE=.36; −5.18 kg, SE=.23). There was no significant difference in weight loss among Partial Responders, Early Adherers, and Fruit/Vegetable-Only Responders (see Fig. 3).
Fig. 3.
Mean percent weight change over 6 months for each latent class in phase 1 of Weight Loss Maintenance Trial. Partial Responders, Early Adherers, and Fruit/Vegetable-Only Responders had significantly greater weight loss than that of Non-responders at 6 months (p<.01)
Discussion
Using RMLCA, we identified three distinct subgroups among participants who were randomized to either the Established or Established + DASH behavioral lifestyle interventions, which were combined into one group for the analysis, in PREMIER (study 1): Responders, Early Adherers, and Non-responders. Furthermore, four subgroups emerged among participants in phase 1 of WLM (study 2): Partial Responders, Early Adherers, Fruit/Vegetable-Only Responders, and Non-responders. Early behavioral response to treatment in PREMIER (study 1) was associated with a greater than 5 % weight loss, on average, in the short term (i.e., initial 6 months of treatment) and the long term (i.e., over 18 months). A modest weight loss of 5–10 % of initial weight has been considered a clinically significant weight loss [23–25]. Also, a high proportion of participants (≥50 %) within the Responders and Early Adherers maintained adherence to the behavioral recommendations at 18 months. For WLM (study 2), a variation of responders emerged (i.e., partial responders and fruit/vegetable-only responders) who achieved clinically significant weight loss (≥5 % of initial weight), on average, by the end of the intensive behavioral intervention phase.
Although the behavioral lifestyle interventions implemented in PREMIER (study 1) and phase 1 of WLM (study 2) were very similar, the number and specific characteristics of the behavioral response patterns (i.e., latent classes) that emerged were not quite comparable between the two trials. However, this is not a limitation of LCA, but rather a reflection of the differences in the specific behavioral recommendations used to create the classes as well as differences in the measures used to assess diet and physical activity. The subgroups or latent classes that emerged in PREMIER (study 1) could be considered to have good separation, i.e., the degree to which the classes can be clearly distinguished from each other [5]. Responders were participants who did not meet any of the behavioral recommendations at baseline, but all of them at 6 months, whereas Non-responders did not meet any of the behavioral recommendations at baseline or 6 months. However, in WLM (study 2), Partial Responders, Early Adherers, and Non-responders were all meeting the sodium intake recommendation at both baseline and 6 months and none of the four subgroups met the physical activity recommendation at either time point. There is some evidence that food frequency questionnaires as used in WLM (study 2) can underestimate sodium consumption as compared to 24-h dietary recalls as used in PREMIER (study 1) [26]. Furthermore, accelerometry, used in WLM (study 2) is considered a more objective measure of physical activity and thus less susceptible to bias (e.g., recall bias) like the 7-day physical activity recall used in PREMIER (study 1) [27].
This study has several strengths and implications for future studies. Latent class analysis has been applied to other health-related observational studies and clinical data to identify subgroups based on behavioral and psychosocial characteristics [28–31]. However, to our knowledge, this is the first application of RMLCA to use randomized clinical trial data to identify responders and non-responders to a behavioral lifestyle intervention. We extended the literature on response to behavioral lifestyle interventions by examining behavioral outcomes as indicators of response, not just weight outcomes. Furthermore, LCA has several advantages over more conventional analytic approaches that can be used to classify individuals. Logistic regression assumes that the classes or subgroups are known and only involves establishing predictors of class membership. In contrast, in LCA, the classes are not known, thus they are latent, and are identified using a set of three or more characteristics (i.e., indicators) that are theoretically relevant to the construct of interest (e.g., behavior change). Also, LCA does not limit the number of possible classes/ subgroups like logistic regression, so there is an opportunity to model numerous patterns of behavioral change. Although cluster analysis has been used to classify individuals in health behavior change research [30], this approach is limited to use with cross-sectional data. LCA allows for repeated measures and uses data from each time point to classify the individual, therefore accounting for the inherent correlation between each repeated measure [32]. Principal components analysis has previously been used to examine different profiles, particularly, weight change trajectories within a large clinical trial [33, 34]. However, principal components analysis does not account for the uncertainty in classifying individuals when comparing the components/factors on distal outcomes. In LCA, the categorical latent variable structure is maintained, and any uncertainty or classification error in the classification of individuals is adjusted for when predicting class membership or when using the classes to predict an outcome such as weight change [32].
There are several limitations to address. First, measures of dietary intake (24-h dietary recall and Block FFQ) and physical activity (7-day physical activity recall in PREMIER only) were obtained by self-report and were therefore subject to bias. However, unannounced 24-h dietary recalls were performed by trained personnel who applied the multiple pass method to obtain the most accurate information during the PREMIER trial (study 1). Furthermore, a more objective measure, accelerometry, was used in WLM (study 2) to assess physical activity. Second, adherence to behavioral recommendations was based on a single assessment, which may not necessarily reflect adherence on a daily basis. Third, response to treatment was based on adhering to five prespecified recommendations or cut points; thus, absolute change in a specific behavior was not represented in the determination of treatment response. For instance, although not at the recommended target, non-responders across both trials, on average, reported a decline in fat intake as well as an increase in fruit/vegetable intake and physical activity over 6 months. Future studies may consider the use of latent profile analysis to maintain the continuous nature of the behavioral variables while identifying distinct subgroups of treatment response based on mean changes [35, 36].
Use of RMLCA to analyze future behavioral study data has implications for the development of more adaptive interventions in clinical settings [37,38]. Replication of this analytic approach in other behavioral lifestyle intervention studies is needed to start to identify common baseline and treatment-related characteristics across studies that distinguish treatment responders and non-responders. Furthermore, by examining patterns of adherence across behaviors during treatment, we can identify treatment responders and non-responders early on and revise or tailor the intervention based on the needs of the individual. For instance, in PREMIER (study 1), an adaptive intervention would consist of the original active lifestyle interventions as previously described and at 6 months, participants who are considered early adherers may be given the option to decrease intensity, responders would be encouraged to continue treatment as is for the remaining 12 months, and non-responders would perhaps be given the option of a more intense intervention or a totally different treatment approach.
In summary, in both PREMIER (study 1) and WLM (study 2), there were subgroups of behavioral responders and non-responders that emerged using LCA and were validated based on significant differences in weight loss outcomes. These findings are important in that they allow us to go beyond establishing efficacy of the intervention and begin to examine for whom treatment is most effective when considering an effectiveness trial or dissemination of the intervention into clinical settings.
Footnotes
Conflict of Interest Lawrence Appel, Janelle Coughlin, Arlene Dalcin, and Gerald Jerome have an institutional (Johns Hopkins University) conflict of interest with Healthways, Inc.
Contributor Information
Stephanie L. Fitzpatrick, Department of Preventive Medicine, Rush University Medical Center, 1700 W. Van Buren St., Room 478A, Chicago, IL 60607, USA
Janelle W. Coughlin, Department of Psychiatry & Behavioral Sciences, Johns Hopkins School of Medicine, Baltimore, MD, USA
Lawrence J. Appel, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA
Crystal Tyson, Department of Medicine, Duke University, Durham, NC, USA.
Victor J. Stevens, Center for Health Research, Kaiser Permanente Northwest, Portland, OR, USA
Gerald J. Jerome, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA
Arlene Dalcin, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA.
Phillip J. Brantley, Pennington Biomedical Research Center, Louisiana State University, Baton Rouge, LA, USA
Felicia Hill-Briggs, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA.
References
- 1.Butryn ML, Webb V. Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34(4):841–59. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wadden TA, Webb VL, Moran CH. Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125(9):1157–70. doi: 10.1161/CIRCULATIONAHA.111.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kong W, Langlois MF, Kamga-Ngande C, Gagnon C, Brown C, Baillargeon JP. Predictors of success to weight-loss intervention program in individuals at high risk for type 2 diabetes. Diabetes Res Clin Pract. 2010;90(2):147–53. doi: 10.1016/j.diabres.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, et al. Pretreatment predictors of attrition and successful weight management in women. Int J Obes Relat Metab Disord. 2004;28(9):1124–33. doi: 10.1038/sj.ijo.0802727. [DOI] [PubMed] [Google Scholar]
- 5.Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. Wiley; New Jersey: 2010. [Google Scholar]
- 6.Lanza ST, Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. 2013;14(2):157–68. doi: 10.1007/s11121-011-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 8.Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Rohm Young D, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144(7):485–95. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 9.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the Weight Loss Maintenance randomized controlled trial. JAMA. 2008;299(10):1139–48. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 10.Jones LR, Wilson CI, Wadden TA. Lifestyle modification in the treatment of obesity: an educational challenge and opportunity. Clin Pharmacol Ther. 2007;81(5):776–9. doi: 10.1038/sj.clpt.6100155. [DOI] [PubMed] [Google Scholar]
- 11.Funk KL, Elmer PJ, Stevens VJ, Harsha DW, Craddick SR, Lin PH, et al. PREMIER—a trial of lifestyle interventions for blood pressure control: intervention design and rationale. Health Promot Pract. 2008;9(3):271–80. doi: 10.1177/1524839906289035. [DOI] [PubMed] [Google Scholar]
- 12.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. N Engl J Med. 1997;336(16):1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 13.Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, et al. Descriptive characteristics of the dietary patterns used in the dietary approaches to stop hypertension trial. DASH collaborative research group. J Am Diet Assoc. 1999;99(8 Suppl):S19–27. doi: 10.1016/s0002-8223(99)00412-5. [DOI] [PubMed] [Google Scholar]
- 14.Hollis JF, Gullion CM, Stevens VJ, et al. Weight loss during the intensive intervention phase of the Weight Loss Maintenance Trial. Am J Prev Med. 2008;35(2):118–26. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blair SN, Haskell WL, Po H, Paffenbarger RS, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical activity methodology by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1986;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 16.Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, et al. Physical activity assessment methodology in the five-city project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 17.Harlan LC, Block G. Use of adjustment factors with a brief food frequency questionnaire to obtain nutrient values. Epidemiology. 1990;1(3):224–31. doi: 10.1097/00001648-199005000-00008. [DOI] [PubMed] [Google Scholar]
- 18.US Department of Agriculture . The food guide pyramid. Vol Home and Garden Bulletin No. 252. US Department of Agriculture; Washington, D.C.: 1992. [Google Scholar]
- 19.Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–32. [Google Scholar]
- 20.Sclove L. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–43. [Google Scholar]
- 21.Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model: Multidiscip J. 2007;14:535–69. [Google Scholar]
- 22.Wang C, Brown CH, Bandeen-Roche K. Residual diagnostics for growth mixture models: examining the impact of a preventive intervention on multiple trajectories of aggressive behavior. J Am Stat Assoc. 2005;100(3):1054–76. [Google Scholar]
- 23.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Look AHEAD Research Group. Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566–75. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization . Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity; Geneva: Jun, 1997. pp. 3–5. 1998; Publication No. WHO/NUT/NCD/98.1. [PubMed] [Google Scholar]
- 26.Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute Food Frequency Questionnaires. Am J Epidemiol. 2001;154(12):1089–99. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 27.Sloane R, Clutter Snyder D, Demark-Wahnefried W, Lobach D, Kraus WE. Comparing the 7-day PAR with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–40. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Vries H, Van’t Riet J, Spigt M, Metsemakers J, van den Akker M, Vermunt JK, et al. Clusters of lifestyle behaviors: results from the Dutch SMILE study. Prev Med. 2008;46(3):203–8. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 29.BeLue R, Lanza ST, Figaro MK. Lifestyle therapy changes and hypercholesterolemia: Identifying risk groups in a community sample of Blacks and Whites. Ethn Dis. 2009;19(2):142–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Ogden LG, Stroebele N, Wyatt HR, Catenacci VA, Peters JC, Stuht J, et al. Cluster analysis of the national weight control registry to identify distinct subgroups maintaining successful weight loss. Obesity (Silver Spring) 2012;20(10):2039–47. doi: 10.1038/oby.2012.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trivedi RB, Ayotte BJ, Thorpe CT, Edelman D, Bosworth HB. Is there a nonadherent subtype of hypertensive patient? A latent class analysis approach. Patient Prefer Adherence. 2010;4:255–62. doi: 10.2147/ppa.s11335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lanza ST, Collins LM. A mixture model of discontinuous development in heavy drinking from ages 18 to 30: the role of college enrollment. J Stud Alcohol. 2006;67(4):552–61. doi: 10.15288/jsa.2006.67.552. [DOI] [PubMed] [Google Scholar]
- 33.Espeland MA, Bray GA, Neiberg R, et al. Describing patterns of weight changes using principal components analysis: results from the action for health in diabetes (Look AHEAD) research group. Ann Epidemiol. 2009;19(10):701–10. doi: 10.1016/j.annepidem.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neiberg RH, Wing RR, Bray GA, et al. Patterns of weight change associated with long-term weight change and cardiovascular disease risk factors in the Look AHEAD study. Obesity (Silver Spring) 2012;20(10):2048–56. doi: 10.1038/oby.2012.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vermunt JK, Magidson J. Latent class cluster analysis. In: Hagenaars JA, McCutcheon AL, editors. Applied latent class analysis. Cambridge University Press; 2002. pp. 89–106. [Google Scholar]
- 36.Fitzpatrick SL, Lai BS, Brancati FL, Golden SH, Hill-Briggs F. Metabolic syndrome risk profiles among African American adolescents: National Health and Nutrition Examination Survey, 2003–2010. Diabetes Care. 2013;36(2):436–42. doi: 10.2337/dc12-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48. doi: 10.1146/annurev-clinpsy-032511-143152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA. Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Translational Behavioral Medicine. 2014 May 06; doi: 10.1007/s13142-014-0265-0. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]