Abstract
Background
The data on the prevalence of recurrent spontaneous miscarriage (RSM) in India are scarce. This study aimed to determine the prevalence of RSM in Indian females.
Methods
Female patients aged between 18 and 45 years with history of at least one spontaneous miscarriage were enrolled in the study. The probability of a subsequent miscarriage after the first, second, and third miscarriage was determined. The prevalence of RSM (defined as loss of ≥3 pregnancies of ≤20 weeks gestation each) between different age groups was compared using χ2 test. Binary logistic regression analysis was applied to determine any association between RSM and the presence of risk factors.
Results
Of the 2398 patients screened for eligibility, 767 (32 %) had a history of at least one spontaneous miscarriage. The prevalence of RSM among the 753 enrolled patients who satisfied the eligibility criteria in the study was 7.46 %. RSM was mostly recorded in the age group of ≥33 years (14.68 %, n = 32). In patients with RSM, the second and third miscarriages were more prevalent during 7th week to end of 11th week of gestation. The probability of having a subsequent miscarriage after the first, second, and third miscarriage was 0.25, 0.34, and 0.22, respectively. There was a significant association (p < 0.05) between RSM and clotting disorders, immunological factors, infections, and genetic disorders.
Conclusion
The study revealed a higher prevalence of RSM among the Indian women as compared to western data. Age, clotting disorders, immunological factors, infections, and genetic disorders were the significant risk factors associated with RSM.
Keywords: Recurrent spontaneous miscarriage, Prevalence, India
Introduction
Miscarriage is defined as spontaneous abortion without medical or mechanical means to terminate a pregnancy before the fetus is sufficiently developed to survive. In other words, miscarriage is early pregnancy loss before 20th week of gestation, or 139 days, counting from the first day of the last normal menses [1]. Approximately 15 % of all clinically recognized pregnancies result in spontaneous loss and many pregnancies are lost before a woman realizes that she is pregnant.
Recurrent spontaneous miscarriage (RSM) is defined as three or more clinically recognized pregnancy losses prior to 20 weeks of gestation from the last menstrual period. It affects 1–2 % of women [2]. The reported possible etiology of RSM includes genetic factors, uterine anatomical defects, infection, endocrine, and immunological factors. Maternal age and the number of prior spontaneous miscarriages are also associated with recurrent miscarriages [3]. The risk of subsequent miscarriage after the first two and three pregnancy losses is 30 and 33 %, respectively, in women without a history of live birth [2].
The current data on the prevalence of recurrent miscarriages in Indian women are scarce. Hence, this study was undertaken to determine the prevalence of RSM of ≤20 weeks of gestation among the Indian females.
Methods
Study Participants
Female patients aged between 18 and 45 years with a history of at least one spontaneous miscarriage of ≤20 weeks of gestation and willing to sign the patient authorization form were included in the study.
Study Sites
Outpatient gynecology and obstetrics clinics were selected from five major cities (Bengaluru, Delhi, Ahmedabad, Kolkata, and Mumbai) across India. Each study site obtained approval from their respective Institutional Ethics Committee before study initiation.
Study Design
This was a cross-sectional, multicenter, and outpatient clinic-based epidemiological study. The patients visiting the clinic for a routine clinical visit were screened to obtain information on eligibility and availability of data. The investigator discussed the study with eligible patients and recruited those willing to sign the patient authorization form. Each enrolled patient was identified by a unique patient identification number to maintain patient confidentiality. The information regarding patient demography; systolic and diastolic measurements; medical history; associated risk factors or conditions that may affect the outcome of pregnancy; menstrual, gynecological and obstetric history; and observations of gynecological examination was recorded. No follow-up visit or any interventions were undertaken in this study.
Outcome Measures
Primary study outcome was the prevalence (%) of female patients with RSM (defined as ≥3 consecutive pregnancy losses of ≤20 weeks of gestation each) among the enrolled patients. Secondary study outcome included comparison of age-specific miscarriages in patients with <3 and ≥3 spontaneous miscarriages of ≤20 weeks of gestation; probability of a subsequent miscarriage after the first miscarriage; and the association between RSM and known risk factors.
The risk factors assessed for association with RSM were uterine anomalies (septate uterus, uni/bicornuate uterus, leiomyoma, cervical insufficiency); clotting disorders [Factor V Leiden, Plasminogen activator inhibitor-1, prothrombin gene mutation, antiphospholipid syndrome (APS), Von Willebrand disease, idiopathic thrombocytopenic purpura]; endocrine disorders [Cushing’s syndrome, polycystic ovarian disorder (PCOD), diabetes, thyroid]; infections (TORCH [toxoplasmosis, other {syphilis, varicella-zoster, parvovirus B19}, rubella, cytomegalovirus, and herpes infection], Listeria monocytogenes); immunological factors (antiphospholipid antibody, hemophilia); genetic disorders (chromosomal abnormality, Down’s syndrome); and other general risk factors (smoking, drugs, alcohol consumption, uterine injury).
Gynecological examination included observation of the vulva, vagina, cervix, uterus, and adnexa of uterus as conducted by the obstetrician or gynecologist.
Analysis
All data analysis was performed using SAS® for Windows (Version 9.2, SAS Institute, Cary, NC, USA). All continuous variables were summarized using number (N), mean, standard deviation (SD), minimum, maximum, and range (maximum–minimum) as applicable. Categorical variables were summarized using frequency and percentages. A two-sided statistical analysis was performed at 5 % level of significance (LOS), if not specified in particular. The prevalence of RSMs between age groups was compared using χ2 test. The binary logistic regression analysis model was applied to determine the association (if any) between recurrent miscarriages and the presence of an associated risk factor.
Results
Baseline Data
A total of 2398 females were screened for eligibility, of which 767 (32 %) patients had a history of at least one spontaneous miscarriage of less than and equal to 20 weeks of gestation. Of these, 755 patients meeting the inclusion criteria were selected. Two patients discontinued the study due to lack of time and 753 (31.40 %) patients were finally enrolled in the study. The demographic profile and baseline characteristics of enrolled patients are presented in Table 1.
Table 1.
Demography and baseline characteristics of enrolled patients
| Parameters | N | Mean (SD) | Range (min, max) |
|---|---|---|---|
| Age (years) | 753 | 29.76 (5.85) | (18, 45) |
| Weight (kg) | 751a | 60.28 (11.48) | (32.30, 122) |
| Height (cm) | 753 | 156.10 (6.58) | (128, 175) |
| Systolic blood pressure (mmHg) | 751a | 116.13 (11.39) | (80, 170) |
| Diastolic blood pressure (mmHg) | 750b | 75.15 (8.41) | (50, 140) |
| Duration of menstrual bleeding (days) | 742c | 4.37 (2.17) | (1, 42) |
| Duration of last menstrual cycle (days) | 738d | 30.91 (6.03) | (15, 90) |
aData were missing for two patients
bData were missing for three patients
cData were missing for 11 patients
dData were missing for 15 patients
Primary Outcome
Of the 753 enrolled patients who satisfied the eligibility criteria, 56 (7.46 %) patients had RSM. The 95 % confidence interval for the prevalence percentage of RSM was 5.58 and 9.34.
Secondary Outcomes
Relation with Age
The prevalence rates of spontaneous miscarriages (which may or may not be recurrent) as per the age of the patient are summarized in Table 2.
Table 2.
Prevalence rates of spontaneous miscarriage in different age groups
| Age subgroups | N | <3 Spontaneous miscarriages n (%) |
p value |
|---|---|---|---|
| 18–22 | 64 | 58 (90.63) | 0.0007 |
| 23–27 | 230 | 220 (95.65) | |
| 28–32 | 241 | 225 (93.36) | |
| 33 and above | 218 | 186 (85.32) | |
| Total | 689 | 753 |
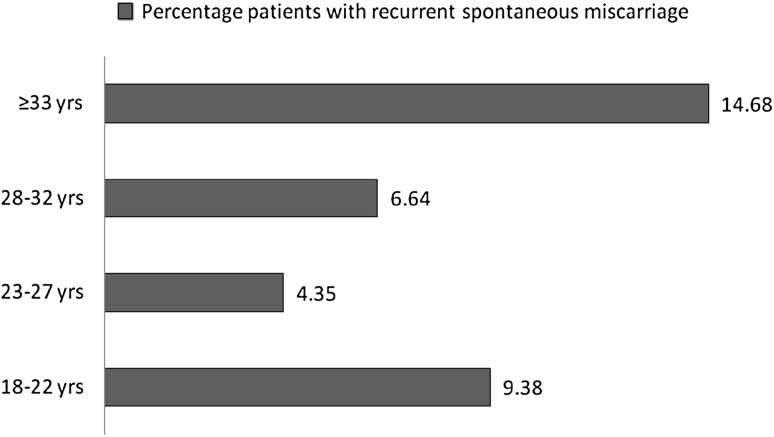
Among the enrolled patients, less than three spontaneous miscarriage (of ≤20 weeks of gestation) was mostly observed in the age group of 23–27 years (95.65 %, n = 220) and RSM was mostly recorded in the age group of ≥33 years (14.68 %, n = 32). The incidence of RSM in patients of different age groups is presented in Fig. 1.
Fig. 1.
Incidence of recurrent spontaneous miscarriage among patients in different age groups
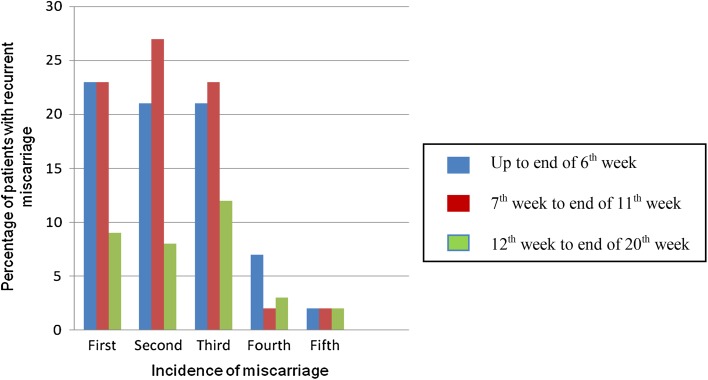
The mean age of patients experiencing first, second, and third miscarriage was 25.52 (±4.31), 26.39 (±4.48), and 27.92 (±5.09) years, respectively. In patients with RSMs, the first miscarriage was equally prevalent up to the end of 6th week (3.05 %, n = 23) versus 7th to the end of 11th week of gestation (3.05 %, n = 23), whereas the second and third miscarriages were more prevalent in 7th week to the end of 11th week of gestation (3.59 %, n = 27; 3.05 %, n = 23, respectively). The incidence of spontaneous miscarriage in patients with recurrent miscarriage as per the week of gestation is presented in Fig. 2.
Fig. 2.
Incidence of spontaneous miscarriage (week of gestation) in patients with recurrent spontaneous miscarriages
Probability of a Subsequent Miscarriage
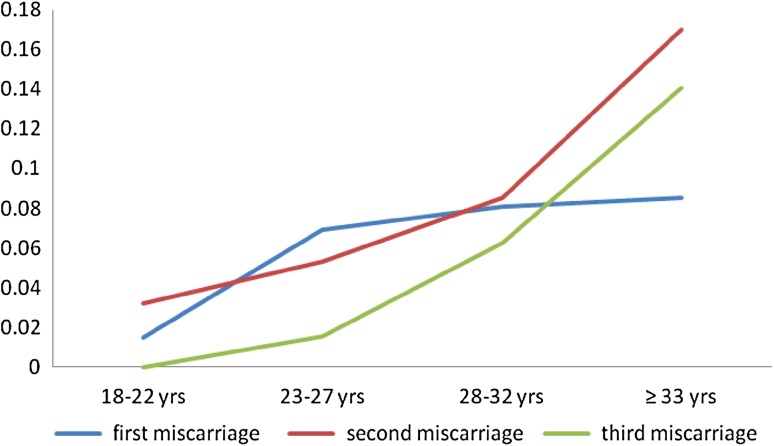
The percentage of patients having a subsequent miscarriage after the first, second, and third miscarriage was 24.97, 34.04, and 21.88 %, respectively. The probability of a subsequent miscarriage after the first, second, and third miscarriage was 0.2497, 0.3404, and 0.2188, respectively, in enrolled patients. Among all the age groups, patients aged ≥33 years had the highest probability of subsequent miscarriage after the first (0.0850), second (0.1702), and third (0.1406) miscarriage as presented in Fig. 3.
Fig. 3.
Probability of subsequent miscarriage as per age groups
The probability of subsequent miscarriage after the third miscarriage was 0.2143 and was highest in the age group of more than or equal to 33 years (0.1250) among the patients with RSM.
Association Between Recurrent Spontaneous Miscarriages and Risk Factors
The occurrence of RSMs was found to be associated with clotting disorders, immunological factors, infections, and genetic disorders. The detailed results are presented in Table 3.
Table 3.
Associated risk factors and incidence of recurrent spontaneous miscarriage
| Enrolled (N = 753)a
risk factors |
Recurrent spontaneous miscarriage | p value | |||
|---|---|---|---|---|---|
| Yes n (%) |
No n (%) |
Total n (%) |
|||
| Uterine anomalies | Present | 4 (14.29) | 24 (85.71) | 28 (3.73) | 0.1305 |
| Absent | 40 (8.10) | 454 (91.90) | 494 (65.78) | ||
| Unknown | 12 (5.24) | 217 (94.76) | 229 (30.49) | ||
| Clotting disorders | Present | 3 (50.00) | 3 (50.00) | 6 (0.80) | 0.0015 |
| Absent | 38 (8.60) | 404 (91.40) | 442 (58.85) | ||
| Unknown | 15 (4.95) | 288 (95.05) | 303 (40.35) | ||
| Endocrine disorders | Present | 13 (10.32) | 113 (89.68) | 126 (16.78) | 0.3137 |
| Absent | 30 (7.44) | 373 (92.56) | 403 (53.66) | ||
| Unknown | 13 (5.86) | 209 (94.14) | 222 (29.56) | ||
| Infections | Present | 6 (22.22) | 21 (77.78) | 27 (3.60) | 0.0052 |
| Absent | 37 (7.82) | 436 (92.18) | 473 (62.98) | ||
| Unknown | 13 (5.18) | 238 (94.82) | 251 (33.42) | ||
| Immunological factors | Present | 5 (33.33) | 10 (66.67) | 15 (2.00) | |
| Absent | 37 (8.98) | 375 (91.02) | 412 (54.86) | ||
| Unknown | 14 (4.32) | 310 (95.68) | 324 (43.14) | ||
| Genetic disorders | Present | 1 (25.00) | 3 (75.00) | 4 (0.53) | 0.0494 |
| Absent | 38 (9.07) | 381 (90.93) | 419 (55.79) | ||
| Unknown | 17 (5.18) | 311 (94.82) | 328 (43.68) | ||
| General risk factors | Present | 1 (6.67) | 14 (93.33) | 15 (2.00) | 1.00 |
| Absent | 54 (7.52) | 664 (92.48) | 718 (95.61) | ||
| Unknown | 1 (5.56) | 17 (94.44) | 18 (2.40) | ||
aData was missing for two patients
As shown in Table 3, the association between RSMs and risk factors such as clotting disorders, immunological factors, infections, and genetic disorders was statistically significant at 5 % LOS. RSM was highly prevalent in patients diagnosed with APS (n = 4, 0.53 %), among clotting disorders; TORCH (n = 22, 2.93 %), among infections; antiphospholipid antibody (n = 8, 1.07 %), among immunological factors; and Down’s syndrome (n = 2, 0.27 %), among genetic disorders. The association between RSM and other risk factors such as uterine anomalies, endocrine disorders, and general risk factors was not statistically significant.
The medical, gynecological history, and abnormal findings in gynecological examination had no significant association with the occurrence of RSM.
Discussion
The prevalence of SM (also known as sporadic miscarriage) is more as compared to RSM [4]. The data on the prevalence of recurrent miscarriage in Indian patients are scarce. The current study examined the prevalence of RSM in Indian women.
It is estimated that 10–15 % of clinically recognized pregnancies worldwide end in a miscarriage. However, the actual rates of miscarriage might be higher as many women have very early miscarriages without ever realizing that they are pregnant [2]. The occurrence of spontaneous miscarriage in India has been reported to be around 10 % [5]. However, our study observed a much higher prevalence of spontaneous miscarriage in the Indian women (32 %).
Compared to spontaneous miscarriages, the prevalence of recurrent miscarriages is much lower [2]. The prevalence of recurrent pregnancy losses including only clinical miscarriages occurring before 21 weeks of gestation (where clinical evidence of pregnancy existed) is 0.8–1.4 %. However, the prevalence of RSM is high if biochemical losses [as indicated by a positive urinary human chorionic gonadotropin (hCG) or a raised serum β-hCG within 6 weeks of gestation] are also included, and is estimated to be as high as 2–3 % [4]. In this study, the prevalence of clinically evident RSM was as high as 7.46 % among the Indian women.
Maternal age is known to be an independent risk factor for miscarriage [6]. Indian women whose age at first birth was 31–49 years were more vulnerable for spontaneous miscarriage than those whose age at first birth was less [5]. The incidence of miscarriage is reported to be 10 % in women aged 20–24 years and 51 % in women aged 40–44 years [4]. A statistically significant association was found between age and spontaneous miscarriage in this study as well. As the age of the patients increased, the occurrence of more than or equal to three spontaneous miscarriages and probability of a subsequent miscarriage after the first, second, and third miscarriage was also increased.
The percentage of patients who had a subsequent miscarriage after the first, second, and third miscarriage in this study was 24.97, 34.04, and 21.88 %, respectively. These findings are well supported by some earlier studies, wherein the risk of a subsequent miscarriage after one spontaneous miscarriage was approximately 22–25 %; after two spontaneous miscarriages, the risk of another was 25 %; and after three spontaneous miscarriages, this risk was further increased to 30 % [7].
Miscarriage can be caused by environmental, genetic, anatomical, endocrine, thrombophilia, and infectious diseases [6]. Among the patients with RSM, the existence of uterine anomalies was comparatively higher (12.6 % [range from 1.8 to 37.6 %]) [8]. Our study shows that 14.29 % of Indian females with uterine anomalies had RSM (non-significant).
The range of patients with RSM tested positive for antiphospholipid antibodies varies from 8 to 42 % [8]. In our study, the APS was the major immunological risk factor associated with RSM.
The previous studies have found that in patients with recurrent miscarriage, viral infections such as cytomegalovirus, herpes virus, and parvoviruses are predominant. Bacterial infections such as Chlamydia trachomatis, Ureaplasma urealyticum, and Mycoplasma hominis, followed by bacterial vaginosis, are also associated risk factors causing recurrent miscarriage [9]. In our study, TORCH infection was found to be a significant risk factor causing RSM.
Chromosomal abnormalities contribute to 50 % of spontaneous miscarriages [10]. However, in this study, the chromosomal abnormality recorded was comparatively low which can be attributed to the absence of any diagnostic test on enrolled patients.
Thyroid disease (9.45 %), PCOD (7.72 %), and TORCH (2.93 %) were the major risk factors identified in the enrolled patients. Uterine septum (0.67 %), bicornuate uterus (0.67 %), leiomyoma (1.07 %), cervical insufficiency (1.20 %), APS (0.53 %), diabetes (0.93 %), hemophilia, and chromosomal abnormality (0.13 %) were identified in minor number of patients.
In conclusion, this study revealed a higher prevalence of RSM among the Indian women as compared to western data and this was due to the fact that only patients with a history of at least one spontaneous miscarriage of less than or equal to 20 weeks of gestation were included in the study and did not represent the general population. Increase in maternal age was associated with significant increase in spontaneous miscarriages. The first, second, and third miscarriages were more prevalent during 7th week to end of 11th week of gestation in patients with RSM. Significant association was found between RSMs and risk factors like clotting disorders, immunological factors, infections, and genetic disorders.
Thus, the finding of this epidemiological study has furnished important information regarding the prevalence of RSMs and the associated risk factors in the Indian women.
Acknowledgments
The financial support for this study was provided by Abbott India Limited, Mumbai, India. The authors acknowledge the support of clinical investigators who participated in the study (listed in alphabetical order): Dr. Appu Ghai, Dr Badal Dhali, Dr. Bharti Seth, Dr. Bipasa Sen, Dr. Chandrika, Dr. Chitra Rammurthy, Dr. Gayatri Despande, Dr. Indrani Lodh, Dr. Nagarathna, Dr. Naresh Goyal, Dr. Nikunj Shah, Dr. Nimmi Mahajan, Dr. Nirmala Pipara, Dr. Nupur Gupta, Dr. Mohan Raut, Dr. Pradeep Gohel, Dr. Pooja Gupta, Dr. Poornima Ramakrishna, Dr. Priti Vyas, Dr. Purvi Rathi, Dr. Rajendra Prasad Ganguly, Dr. Rajesh Punjabi, Dr. Rajesh Somani, Dr. Ratnabali Chakravorty, Dr. Ruchi Malhotra, Dr. Rupa Iyengar, Dr. S. Sreelatha, Dr. Suman Bijlani, Dr. Sunil Patel, and Dr. Veena G. Shinde.
Compliance with ethical requirements and Conflict of interest
Each study site (Bengaluru, Delhi, Ahmedabad, Kolkata, and Mumbai) across India obtained approval from their respective Institutional Ethics Committee before study initiation. The study was conducted in accordance with the protocol, applicable local regulatory guidelines, and ethical principles that have their origin in the Declaration of Helsinki. Dr. Ameet Patki declares that he has no conflict of interest. Dr. Naveen Chauhan declares that he is an employee of Abbott India Limited and has participated in the planning and writing of the manuscript. He has seen and approved the final version of manuscript.
Dr. Ameet Patki
is presently appointed as an Honorary Associate Professor in K.J. Somaiya Medical College, Hospital and Research Centre and Medical Director at Fertility Associates—Centre For Assisted Reproduction in Mumbai. He is a member of prestigious various organizations, including MOGS, India—Royal College of OBGYN London, ISAR. He is a chairperson of FOGSI Perinatology Committee; he has contributed to over 50 chapters and editorial contribution to textbooks. He has been invited as faculty and has delivered over 150 lectures, guest lectures orations, CMEs, and workshops at national and international levels. He has organized academic meetings and scientific sessions at national and international level. He has conducted over 50 Hands-on IUI Workshops in India and also an extensive 5-day Hands-On Workshop in Basic and Advanced IVF Training for the Gynecologists and Embryologist. He has two international patents to his credit for his work in Stem Cell Research and Infertility.

References
- 1.Li L, Leung PC, Chung TK, et al. Systematic review of Chinese medicine for miscarriage during early pregnancy. Evid Based Complement Altern Med. 2014;2014:753856. doi: 10.1155/2014/753856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford HB, Schust DJ. Recurrent pregnancy loss: etiology, diagnosis, and therapy. Rev Obstet Gynecol. 2009;2(2):76–83. [PMC free article] [PubMed] [Google Scholar]
- 3.Li TC, Makris M, Tomsu M, et al. Recurrent miscarriage: aetiology, management and prognosis. Hum Reprod Update. 2002;8(5):463–481. doi: 10.1093/humupd/8.5.463. [DOI] [PubMed] [Google Scholar]
- 4.Larsen EC, Christiansen OB, Kolte AM, et al. New insights into mechanisms behind miscarriage. BMC Med. 2013;11:154. doi: 10.1186/1741-7015-11-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maharana B. Correlates of spontaneous and induced abortion in India: an investigation using a nationwide large scale survey data, Population Association of America. In: 2011 Annual meeting program. http://paa2011.princeton.edu/abstracts/111333. Accessed 25 Feb 2015.
- 6.Royal College of Obstetricians and Gynaecologists. The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. Green-top Guideline No. 17. London: RCOG; 2011. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_17.pdf. Accessed 25 Feb 2015.
- 7.Simpson J, Carson S. Genetic and nongenetic causes of pregnancy loss. Global Library of Women’s Medicine; 2013. ISSN 1756-2228. doi:10.3843/GLOWM.10319.
- 8.Practice Committee of the American Society for Reproductive Medicine Evaluation and treatment of recurrent pregnancy loss: committee opinion. Fertil Steril. 2012;98(5):1103–1111. doi: 10.1016/j.fertnstert.2012.06.048. [DOI] [PubMed] [Google Scholar]
- 9.Nigro G, Mazzocco M, Mattia E, et al. Role of the infections in recurrent spontaneous abortion. J Matern Fetal Neonatal Med. 2011;24(8):983–989. doi: 10.3109/14767058.2010.547963. [DOI] [PubMed] [Google Scholar]
- 10.Gonçalves RO, Santos WV, Sarno M, et al. Chromosomal abnormalities in couples with recurrent first trimester abortions. Rev Bras Ginecol Obstet. 2014;36(3):113–117. doi: 10.1590/S0100-72032014000300004. [DOI] [PubMed] [Google Scholar]