Abstract
Introduction
Although the incidence of cancer cervix has reduced in India during the last two decades, still most of the patients presenting in tertiary care centers are in advanced stages.
Material and Methods
At this center, we see 6% of cancer cervix cases every year, and most of these cases are in stage III and IVa. All these patients have squamous cell carcinoma and were treated with a combination of external and intracavitary radiotherapy along with concurrent cisplatin given once weekly. Eighty-nine point nine % patients had achieved a complete response.
Results
Local recurrence was seen in 17.9% at a median duration of 10.5 months, and 8.17% developed distant metastasis involving lung, liver, bone, and supraclavicular lymph nodes. Three patients developed metastasis at unusual sites involving breast, paraspinal muscles, and duodenum which are very rarely involved. These patients were treated with chemotherapy using carboplatin and Paclitaxel combination but succumbed within 8–10 months of development of metastasis.
Conclusion
The cause of involvement of these unusual sites is not clear, but it may be hematological spread, and we want to share these reports such that these sites are seen during follow-up of patients of cancer cervix.
Keywords: Cancer cervix, Metastasis, Unusual sites
Introduction
Cervical cancer is the fifth most common cancer worldwide and ranks second among all female cancers and is also the most common cause of cancer deaths in the developing countries. Five lakh, ten thousand new cases are seen annually with 2,88,000 deaths worldwide [1]. Sexually transmitted human papilloma virus (HPV) infection is the most important risk factor for cervical intraepithelial neoplasia and invasive cervical cancer [2]. Other factors include early age of marriage, low socioeconomic status, multiple sexual partners, intercourse with uncircumcised men, and multiple child bearing. In India, the incidence is around 19–44 per 100,000 women. Unlike many other cancers, cervical cancer occurs early and strikes at the productive period of a woman’s life. The incidence rises in 30–34 years of age and peaks at 55–65 years, with a median age of 38 years (age range, 21–67 years). The usual treatment of cancer cervix is concurrent chemotherapy and radiotherapy in locally advanced cases, and the results with this treatment are very good with minimal side effects with the advent of newer techniques in radiotherapy. The pattern of failure has been studied extensively and recurrences in pelvis, nodes, and distant sites have been seen. We studied the patterns of failure at our center and found some very unusual sites of metastasis which are being shared. A good review including all unusual sites was not seen in the literature. Only case reports have been discussed. We have tried to discuss the unusual sites of metastasis from cancer cervix with their probable routes of metastasis and prognosis in this article.
Materials and Methods
Six thousand, one hundred and ninety-nine patients were registered between January 2010 and December 2014 of whom patients with gynecological malignancy were 496, and those with carcinoma cervix were 306. The incidence of gynecological malignancies was 8 % and that of cervical cancer was 6 % at this center. Histologically, 92.5 % were Squamous cell carcinoma (SCC), and 7.5 % were Adenocarcinoma. 67 % patients presented in FIGO stage IIIB, 11.1 % in stage IVA, 9.8 % in stage IIB, 8.5 % in IIA, and 3.5 % in stage IB. Most of the patients presented in an advanced local stage and were treated mainly with concurrent chemotherapy using once weekly cisplatin 30 mg/m2 along with external radiotherapy on linear accelerator 50 Gy in 25 fractions in 5 weeks and three sittings of intracavitary radiotherapy of 7 Gy each covering 90 % of clinical target volume. 10 Gy in 5 fractions in 2 weeks boost to pelvis was given by external radiotherapy to patients who were unfit for brachytherapy.
All the post-op patients were given external beam radiotherapy (EBRT) at a dose of 50 Gy in 5 weeks followed by three sittings of intravaginal brachytherapy of 5 Gy each prescribed to the surface.
Results
All the patients were given similar treatment and were regularly followed up. Complete response after treatment was achieved in 89.9 % including all stages, and residual disease was seen in 10.1 % of patients. 17.9 % of patients developed recurrent local disease within 6–15 months with a median time of 10.5 months. 8.17 % patients developed distant metastasis involving Lung (n = 12) in 48 %, Liver (n = 7) in 28 %, Supraclavicular node (n = 2) in 8 %, Bone (n = 1) in 4 %, and unusual sites (n = 3) in 12 %. The unusual sites included breast, paraspinal muscles (Fig. 1), and the Duodenum (Fig. 2). The distant metastasis occurred within 8–18 months.
Fig. 1.
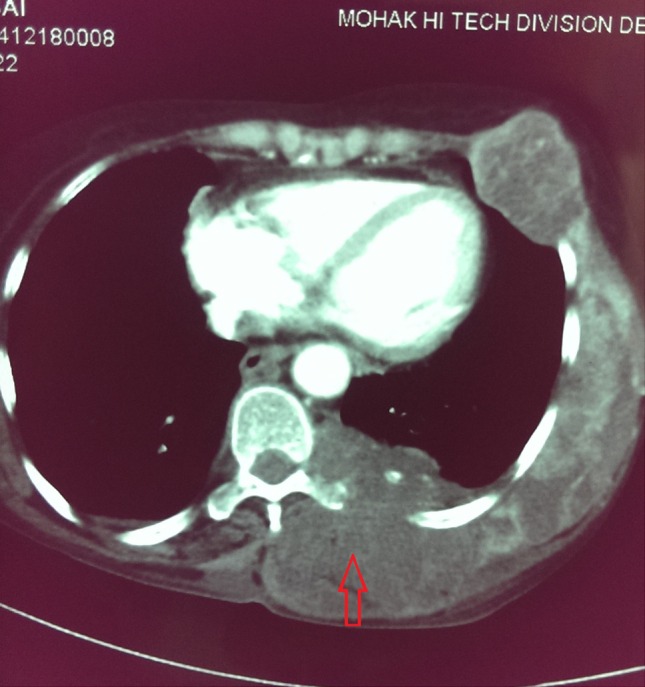
CT-scan showing paraspinal muscle metastasis (red arrow)
Fig. 2.
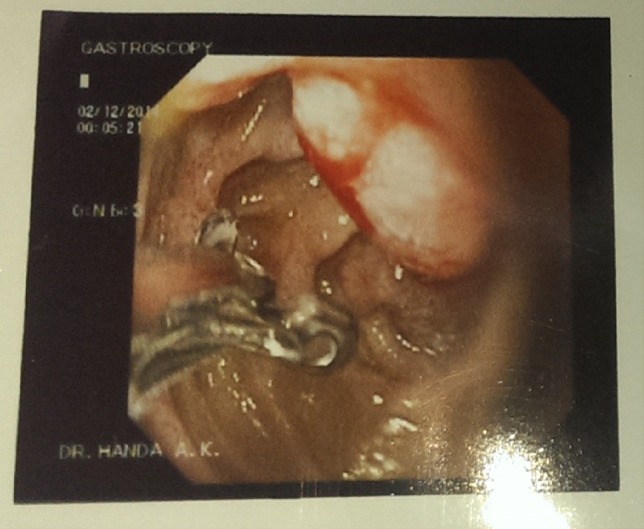
Upper gastroendoscopy showing an ulcer in the D2 region of the duodenum
All the three patients with rare site of metastasis had the same histology of metastatic squamous cell carcinoma (Figs. 3, 4). FIGO stage at diagnosis for paraspinal muscle metastasis and breast metastasis was stage IIIB, and for duodenal metastasis it was IIA, i.e., had locally advanced disease, and all the patients had developed complete local control after concurrent chemotherapy and radiotherapy. The duration of development of metastasis was 12 months after treatment for paraspinal muscle metastasis, 15 months for breast metastasis, and 17 months for duodenal metastasis (Table 1).
Fig. 3.
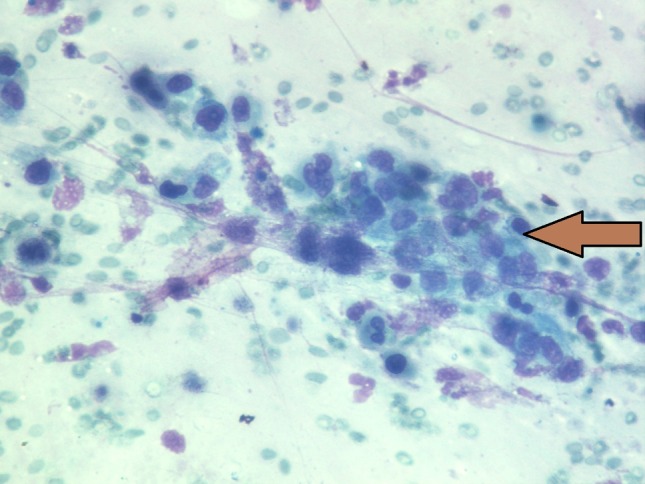
FNAC from skeletal muscle mass showing nests of pleomorphic squamous cells (bold arrow head)
Fig. 4.
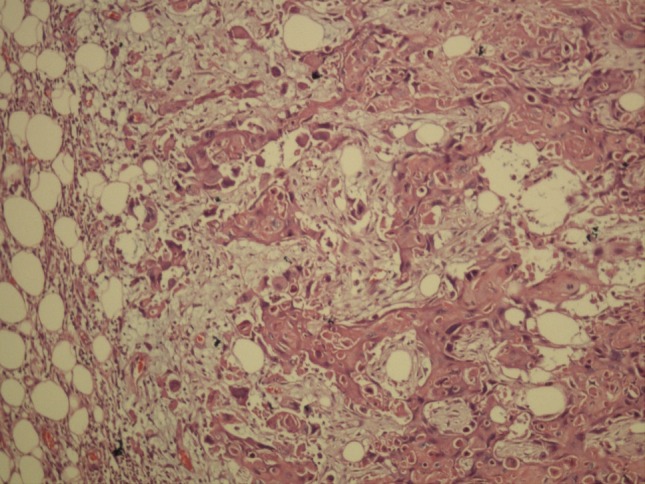
Histopathology specimen of excision of breast lump showing squamous cell metastasis
Table 1.
The characteristics of the patients with unusual metastasis
| Case no. |
Unusual site of metastasis |
Histology | FIGO stage | Duration (months) |
|---|---|---|---|---|
| 1. | Para-spinal muscle | Metastatic SCC | IIIB | 12 |
| 2. | Breast | Metastatic SCC | IIIB | 15 |
| 3. | Duodenum | Metastatic SCC | IIA | 17 |
SCC squamous cell carcinoma
Discussion
Cervical cancer is the second most common cancer in women worldwide, and the most common cancer cause of death in women in the developing countries. Carcinoma cervix is the most prevalent malignancy in Indian women with incidence of about 19–44 per 100,000 women [3]. The standard treatment for cancer cervix is a combination once weekly cisplatinum along with external and Intracavitary radiotherapy and gives a good control. Metastasis to distant sites is very unusual. Metastasis in carcinoma cervix can occur via lymphatic spread or hematogenous spread. Hematogenous spread in carcinoma cervix is more common in advanced stage and mostly occurs through venous plexus or the paracervical veins. The common site of distant metastasis includes lung, liver, bones, and supraclavicular nodes. The rare sites include heart, brain, muscles, and very occasionally other sites.
Patients with cervical cancer can develop pelvic recurrence, distant metastasis, or combination of both. A 10–20 % recurrence rate has been reported following primary surgery or radiotherapy in women with stage IB–IIA cervical tumors with no evidence of lymph node involvement, while up to 70 % of patients with nodal metastases and/or more locally advanced tumors will suffer relapse [4–7]. As the bulk of a pelvic tumor increases, the proportion of patients with disease recurrent or persistent in the pelvis as the only site of failure is greater than the proportion developing distant metastases. Perez et al. reported a total pelvic failure rate of 10 % in stage IB, 17 % in stage IIA, 23 % in stage IIB, 42 % in stage III, and 74 % in stage IVA after radiotherapy alone [8]. Hematogenous spread in carcinoma cervix is more common in advanced stage and mostly occurs through venous plexus or the paracervical veins. The 10-year actuarial incidence of distant metastases was 3 % in stage IA, 16 % in stage IB, 31 % in stage IIA, 26 % in stage IIB, 39 % in stage III, and 75 % in stage IVA [9]. In patients who develop distant metastases, the most frequently observed metastatic sites were lung (21 %), para-aortic nodes (11 %), abdominal cavity (8 %), and supraclavicular nodes (7 %). Bone metastases occurred in 16 % of patients, predominantly involving the lumbar and thoracic spine. Patients who relapsed in lymph nodes had a median survival of 24 weeks, while those who relapsed in other organs had a median survival of only 12 weeks [10]. The majority of recurrences occur within 2 years of diagnosis, and the prognosis is poor, with most patients dying as a result of uncontrolled disease.
Skeletal muscles and small intestine are highly resistant to primary and metastatic cancers both due to the high contractile activity; good oxygenation and blood flow in the muscles [11, 12] and high mobility; rapid transit time of food leading to reduced contact time for carcinogens; and high immune protection due to more lymphocytes in the intestine, which protects them from malignancies [13, 14].
The incidence of skeletal muscle metastasis in carcinoma cervix is reported to be <1 % [15–17], breast is involved as metastatic site in only 1.2 % [18], whereas small bowel accounts for only 0.4 % [13] of all cancer metastases. Isolated metastasis to small bowel is extremely rare from cancer cervix and is mainly through para-aortic or mesenteric nodes and less commonly by hematogenous spread or is due to peritoneal seedlings [19, 20]. In the remaining all sites, it usually spreads by hematogenous route. Till now, only 10 cases of metastasis in skeletal muscle, 6 cases in small bowel, and very few in breasts from cancer cervix have been reported in the world literature.
The most common muscles involved in metastasis from cancer cervix are the Psoas muscle [15]. In breast upper outer quadrant and in small bowel ileum, duodenum and jejunum, respectively, are usually involved. The median duration from treatment of primary to the development of metastasis ranges from 2 to 13 years [14]. We also show metastasis in the whole length of paraspinal muscles, upper outer quadrant of breast, and the duodenum, and all these sites are very rare to be involved.
The prognosis of patients after development of metastasis is usually poor. The treatment options include all the modalities of cancer treatment. Surgery followed by palliative chemotherapy and local radiotherapy are the usual treatments offered to the patients. The overall survival is less. We could not find median survival being reported in the literature for these metastatic cases.
Out of 306 patients of carcinoma cervix, only 25 developed distant metastasis. These patients had an advanced local disease, and three of them developed metastasis in muscles, breast, and duodenum respectively. These are very rare sites to be involved, and only very few cases have been described in the literature. The exact route of metastasis to these sites cannot be ascertained, but it may probably be due to hematogenous route in locally advanced disease. The median duration of development of the metastasis in this series is around 10.5 months, which also correlates with the other studies found in the literature. All the three patients with unusual metastasis were advised for palliative chemotherapy, and none of them survived longer and succumbed to the disease within 6 months of development of metastasis, which is almost the same as seen in other series.
Conclusion
Metastasis in carcinoma cervix can occur at some unusual sites, which should always be kept in mind during the follow-up of stage III and IV patients, and any unusual symptom should be thoroughly investigated. The prognosis in these cases is poor, and survival is short; hence, active treatment with radiotherapy or chemotherapy is indicated. The unusual sites should always be seen during the follow-up or a whole body PET CT Scan should be done at least once after 1 year of treatment to diagnose metastasis early.
Acknowledgments
Compliance with Ethical Requirements and Conflict of Interest
There are no ethical issues related to this topics and there is no conflict of interest between the authors. There are no financial or any other issues related to this topic also.
Virendra Bhandari
on completion of MD in Radiation Oncology worked as a Senior Registrar at Tata Memorial Hospital Mumbai and then as a Consultant Oncologist at Allahabad and Aurangabad, where he was involved in treatment of solid and hematological malignancies with chemotherapy and radiotherapy. He has received the UICC Fellowship twice for his project in Brachytherapy and underwent training at Christie Hospital Manchester (UK) and Utrecht Hospital, the Netherlands. He has also received the Fellowship in Hyperthermia at D D Hoed Cancer Hospital, Rotterdam, the Netherlands, and another Fellowship in Image Guided Radiotherapy planning at Henry ford hospital, Detroit (USA). Presently, he is working as a Professor at Sri Aurobindo Medical College and P G Institute, Indore and working on Linear accelerator with IGRT facility and HDR Brachytherapy. He has more than 25 Publications in various National and International Indexed journals and many presentations to his credit.
Footnotes
Mehlam Kausar is a Registrar in the Department of Radiotherapy, Sri Aurobindo institute of Medical Science; Ayush Naik is a Registrar in the Department of Radiotherapy, Sri Aurobindo institute of Medical Science; Manika Batra is a Registrar in the Department of Radiotherapy, Sri Aurobindo institute of Medical Science; Virendra Bhandari is a Professor in the Roentgen-SAIMS Radiation Oncology Centre, Sri Aurobindo institute of Medical Science.
References
- 1.Sankaranarayanan R, Ferlay J. Worldwide burden of gynecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006;20:207–225. doi: 10.1016/j.bpobgyn.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Schiffman M, Castle PE, Jeronim J, et al. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi: 10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal U, Dahiya P, Chauhan A, et al. Scalp metastasis in carcinoma of the uterine cervix—a rare entity. Gynecol Oncol. 2002;87:310–312. doi: 10.1006/gyno.2002.6829. [DOI] [PubMed] [Google Scholar]
- 4.Delgado G, Bundy B, Zaino R, et al. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990;38:352–357. doi: 10.1016/0090-8258(90)90072-S. [DOI] [PubMed] [Google Scholar]
- 5.Zaino RJ, Ward S, Delgado E, et al. Histopathologic predictors of the behavior of surgically treated stage IB squamous cell carcinoma of the cervix. A Gynecologic Oncology Group study. Cancer. 1992;69:1750–1758. doi: 10.1002/1097-0142(19920401)69:7<1750::AID-CNCR2820690717>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 6.Burghardt E, Baltzer J, Tulusan AH, et al. Results of surgical treatment of 1028 cervical cancers studied with volumetry. Cancer. 1992;70:648–655. doi: 10.1002/1097-0142(19920801)70:3<648::AID-CNCR2820700318>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 7.Stehman FB, Bundy BN, DiSaia PJ, et al. Carcinoma of the cervix treated with radiation therapy. I. A multi-variate analysis of prognostic variables in the Gynecologic Oncology Group. Cancer. 1991;67:2776–2785. doi: 10.1002/1097-0142(19910601)67:11<2776::AID-CNCR2820671111>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 8.Perez CA, Grigsby PW, Camel HM, et al. Irradiation alone or combined with surgery in stage IB, IIA, and IIB carcinoma of the uterine cervix: update of a nonrandomized comparison. Int J Radiat Oncol Biol Phys. 1995;31:703–716. doi: 10.1016/0360-3016(94)00523-0. [DOI] [PubMed] [Google Scholar]
- 9.Fagundes H, Perez CA, Grigsby PW, et al. Distant metastases after irradiation alone in carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 1992;24:197–204. doi: 10.1016/0360-3016(92)90671-4. [DOI] [PubMed] [Google Scholar]
- 10.Van Nagell Jr JR, Rayburn W, Donaldson ES, et al. Therapeutic implications of patterns of recurrence in cancer of the uterine cervix. Cancer. 1979;44:2354–2361. doi: 10.1002/1097-0142(197912)44:6<2354::AID-CNCR2820440653>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 11.Acinas Garcia O, Fernandez FA, Satue EG, et al. Metastasis of malignant neoplasms to skeletal muscle. Rev Esp Oncol. 1984;31:57–67. [PubMed] [Google Scholar]
- 12.Weiss L. Biomechanical destruction of cancer cells in skeletal muscle: a rate-regulator for hematogenous metastasis. Clin Exp Metastasis. 1989;7:483–491. doi: 10.1007/BF01753809. [DOI] [PubMed] [Google Scholar]
- 13.Schottenfeld D, Beebe-Dimmer JL, Vigneau FD. The epidemiology and pathogenesis of neoplasia in the small intestine. AEP. 2009;19(1):58–69. doi: 10.1016/j.annepidem.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gurian L, Ireland K, Petty W, et al. Carcinoma of the cervix involving the duodenum: case report and review of the literature. J Clin Gastroenterol. 1981;3:291–294. doi: 10.1097/00004836-198109000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Ferrandina G, Salutari V, Testa A, et al. Recurrence in skeletal muscle from squamous cell carcinoma of the uterine cervix: a case report and review of the literature. BMC Cancer. 2006;6:169. doi: 10.1186/1471-2407-6-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Padhi S, Banerjee S, Das S, et al. Carcinoma cervix with atypical presentation of metastatic lesion as a cyst in the right deltoid muscle. Indian J Pathol Microbiol. 2008;51:450–451. doi: 10.4103/0377-4929.42527. [DOI] [PubMed] [Google Scholar]
- 17.Mariya Y, Watanabe S, Yokoyama Y, et al. Metastasis of uterine cervical cancer to the biceps muscle of right upper arm; report of a case. Rinsho Hoshasen. 1990;35:1447–1450. [PubMed] [Google Scholar]
- 18.Hajdu SI, Urban JA. Cancers metastatic to the breast. Cancer. 1972;29:1691–1696. doi: 10.1002/1097-0142(197206)29:6<1691::AID-CNCR2820290637>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 19.Misonou J, Natori T, Aizawa M, et al. Stage (Ia) cervical cancer recurring 13 years after hysterectomy and causing small intestinal perforation: a case report with a review of the literature. Acta Pathol Jpn. 1988;38(2):225–234. doi: 10.1111/j.1440-1827.1988.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 20.Mathur SK, Pandya GP. Solitary metastatic malignant stricture of the ileum: a rare cause of small bowel obstruction (a case report) J Postgrad Med. 1984;30:186. [PubMed] [Google Scholar]


