Abstract
Three-dimensional (3-D) cell cultures are beneficial models for mimicking the complexities of in vivo tissues, especially in tumour studies where transport limitations can complicate response to cancer drugs. 3-D optical microscopy techniques are less involved than traditional embedding and sectioning, but are impeded by optical scattering properties of the tissues. Confocal and even two-photon microscopy limit sample imaging to approximately 100–200 μm depth, which is insufficient to image hypoxic spheroid cores. Optical clearing methods have permitted high-depth imaging of tissues without physical sectioning, but they are difficult to implement for smaller 3-D cultures due to sample loss in solution exchange. In this work, we demonstrate a microfluidic platform for high-throughput on-chip optical clearing of breast cancer spheroids using the SeeDB, ClearT2, and ScaleSQ clearing methods. Although all three methods are able to effectively clear the spheroids, we find that SeeDB and ScaleSQ more effectively clear the sample than ClearT2; however, SeeDB induces green autofluorescence while ScaleS causes sample expansion. Our unique on-chip implementation permits clearing arrays of 3-D cultures using perfusion while monitoring the 3-D cultures throughout the process, enabling visualization of the clearing endpoint as well as monitoring of transient changes that could induce image artefacts. Our microfluidic device is compatible with on-chip 3-D cell culture, permitting the use of on-chip clearing at the endpoint after monitoring the same spheroids during their culture. This on-chip method has the potential to improve readout from 3-D cultures, facilitating their use in cell-based assays for high-content drug screening and other applications.
I. INTRODUCTION
Three-dimensional (3-D) cell cultures and micro-tissues have emerged as a better in vitro model of live tissues by allowing the cells to maintain cell-cell and cell-matrix interactions that control cellular development, differentiation, and signalling.1–3 Owing to their better mimicry of live tissues, 3-D cell cultures have been used as a model for cancer drug screening, where drug transport in tissue can be a bottleneck in drug effectiveness, thus making drug screening using traditional two-dimensional (2-D) cell cultures less relevant.4,5 Multicellular tumour spheroids have been employed as a model for avascular tumour nodules, early metastases, and intravascular regions of solid tumours in cancers of the liver, brain, and breast.6–8 In addition to the limited drug delivery, these tumour sites are prone to nutrient and oxygen limitations. Starvation can upregulate cellular autophagic activity,9 which in turn can change the response to cancer drugs.10,11 Hypoxia has also been found to result in cells with more aggressive phenotype, thereby increasing tumour malignancy.12 In addition to tumour spheroids, micro-dissected tumour tissues have also been recently demonstrated to survive in culture within a microfluidic system, and present another type of micro-tissue with a potential for wide utility as an in vitro tissue model.13
Studying the heterogeneous conditions that can exist within 3-D cultures and micro-tissues requires data acquisition from the cells deep within the culture, which can be challenging. Traditional methods such as resin embedding and sectioning are laborious and time-consuming, while the slice deformation caused by sectioning can make 3-D reconstruction difficult.14 Alternatively, advanced microscopy techniques can image 3-D structures by optical sectioning. Light-sheet microscopy is very effective for transparent samples such as zebrafish15 and has also been employed for imaging spheroids;16 however, it requires special sample preparation techniques and imaging chambers optically accessible from two perpendicular planes, and so cannot be performed easily on every experimental setup. Two-photon (2-P) microscopy has also been used for imaging 3-D cell cultures,17 due to its higher penetration depth into the tissue, effective single-point excitation, and reduced photo-damage to the cells by its long-wavelength excitation.18,19 However, despite these improved abilities of 2-P microscopy in comparison with standard (single photon) confocal microscopy,20 it also faces some limitations. The scattering properties of 3-D cell cultures can still result in the non-uniform image intensity through a Z-stack,21,22 and in the case of spherical 3-D cultures, can lead to the sections with darkened interiors due to the longer optical path through the centre of the spherical structures. Much of the scattering induced by 3-D tissues such as tumour spheroids occurs in the lipid-aqueous interface,23 and is due to the refractive index (RI) mismatch between the tissue and the imaging medium that results in blurred images and shallow imaging depth due to the loss of signal photons.24,25 In order to address the issue of decreasing signal strength with increasing confocal imaging depth, le Roux et al. have used depth-dependent laser output modulation26 in confocal imaging. By using a linear laser output modulation from 1% to 10%, they were able to improve the image quality at larger imaging depths.
We have found that even 2-P imaging depths tend to be limited to ∼100–200 μm for our cell spheroid samples. A comparison of two-photon and standard single-photon confocal images at various imaging depths is presented in Figure S1 of the supplementary material50 and shows that although two-photon improves image brightness, clarity, and background fluorescence deep in the 3-D culture, usable imaging depth is still limited. Because there is evidence that biologically relevant phenomena such as necrotic cores can begin to form tumour spheroids in larger (400–600 μm) diameter,27 the ability to image deep into tumour spheroid samples (∼300 μm, to visualize the centres of 600 μm spheroids) would be highly valuable. Building upon the work by le Roux et al., we have also previously demonstrated the modulation of the excitation laser intensity with depth into the sample in two-photon microsopy.28 While this process increases the usable imaging depths, optical scattering still results in blurred slice images deep into the Z-stack, with nuclei in the centre of the spheroid much less well resolved in slices deeper into the spheroid.
Researchers have proposed various techniques to modify the optical properties of the tissues to facilitate 3-D tissue imaging. This can be achieved by removal of lipids from the tissue, or matching the RI of the tissue with the surrounding medium.29 CLARITY is a tissue clearing method that removes lipids from tissues using electrophoresis, while supporting the tissue with a 3-D hydrophilic polymer network.25 Alternatively, many methods have been proposed based on matching the RI of the tissue and its surrounding environment. A hydrophobic mixture of benzyl alcohol and benzyl benzoate (BABB) has been used to clear brain tissues;30 however, it quenches many fluorescent proteins31 and can reduce the signal from immunofluorescent labelling and lipophilic carbocyanine dyes.32 Hama et al.51 have developed Scale, a urea based clearing agent that preserves the fluorescent proteins. Scale requires long incubation times and swells the tissue, while a sorbitol-based variation (ScaleS) has been demonstrated to alleviate these issues through the use of a solution combining sorbitol and urea.35 ScaleSQ, a variant of ScaleS designed for faster clearing in a single-step process, uses a high concentration of urea along with sorbitol to clear 1–2 mm thick brain slices. Ke et al. have demonstrated SeeDB, a hydrophilic fructose-based clearing agent to match the RI of tissue lipids and the media, without quenching the fluorophores, shorter incubation time (days) than the urea-based methods (weeks to months), and size preservation in brain samples.33 Much faster clearing results (hours) with preservation of morphological features have been achieved by the ClearT and ClearT2 methods, containing formamide and formamide/polyethylene glycol (PEG) solutions, respectively.32 Although ClearT has a superior clearing capability compared to ClearT2, the latter can preserve fluorescent proteins and immunohistochemical labels.32 Other clearing techniques have combined elements of previously mentioned methods to achieve effective tissue clearing. For example, CUBIC relies on chemical lipid removal followed by RI matching,29 while FRUIT has combined the use of fructose and urea for reduced solution viscosity and easier clearing of brain samples.34 Among all the aforementioned clearing techniques, SeeDB,33 ClearT2,32 and ScaleS35 are the only ones demonstrated to be compatible with visualizing both intrinsically expressed fluorescent proteins and lipophilic dyes,36 two types of fluorophores with wide applicability in phenotypic drug screening research.
Most of the aforementioned tissue clearing protocols have been developed to clear neurological tissues and mouse brains; however, different tissue types may have different clearing results and optimal protocols. For example, Boutin and Hoffman-Kim recently compared ClearT2, Scale, and SeeDB on tissue-engineered neural sphere samples.37 Although the original demonstration of SeeDB on murine neonatal brain and adult hemi-brain samples showed minimal sample volume change, Boutin and Hoffman-Kim found significant shrinkage in their SeeDB-treated neural sphere samples. It is thus crucial to test different clearing protocols on the tissue of interest, while monitoring the sample during the process could give greater insight as to the effects of each protocol.
Das et al. have investigated the use of a commercial clearing agent optimized for pancreatic tissue, FocusClear®, on porcine pancreas tissue cores.38 They fabricated a millimetre-scale custom chamber from glass microscope slides in order to clear a 40–600 μm thick section of tissue with millimetre-scale area. Clearing in the device yielded greatly improved light transmittance and allowed the authors to image pancreatic islet structures in the tissue; however, only one tissue section could be cleared at a time.
We are able to produce large numbers of multicellular tumour spheroids containing a hydrogel, collagen, and Matrigel® based scaffold to resemble the tumour extracellular matrix (ECM).39 Although Boutin et al. have studied optical clearing in neural stem cell spheroids and glioma,37 to the best of our knowledge, no study has been performed on optical clearing of ECM-containing tumour spheroids. Most of the clearing protocols were developed for millimetre-scale tissue samples and require successive incubations in different solutions; this can be difficult to implement, requiring centrifugation for solution exchange around tumour spheroid samples. Centrifugation can damage the spheroid structure, and for some protocols such as SeeDB can actually be impossible to implement due to solution density matching to that of micro-tissue, resulting in the loss of spheroid samples during the clearing process. Additionally, it is difficult to compare the same spheroid samples before and after clearing, or to image samples that had been monitored during microfluidic on-chip cell culture.
In this work, we propose a rapid and high-throughput platform for on-chip optical clearing of arrays of tumour spheroids. We have adapted the SeeDB, ClearT2, and ScaleSQ tissue clearing techniques for application in a microfluidic environment (hereafter called μSeeDB, μClearT2, and μScaleSQ, respectively). We use two-photon microscopy to assess the methods' clearing efficacy in multicellular tumour spheroids of fluorescent protein expressing human cancer cells, owing to its better image quality, higher laser penetration depth, and reduced photobleaching damage. This work is a step towards establishing a tumour-on-a-chip platform for image-based cancer drug screening.
II. EXPERIMENTAL
A. Cell culture and spheroid preparation
1. Cancer cell culture
MCF-7 breast cancer cells were transfected with FUCCI growth cycle indicator40 using Lypofectamine 3000 (Invitrogen, Carlsbad, CA) reagent, following the product guidelines. The transfected cells express mKO2 (ex/em:551/565 nm) during the G1 phase, while expressing mAG1 (ex/em:492/505 nm) during the S/G2/M phases. The cells will express both fluorophores during their transition from G1 to S, while no fluorophore is expressed during the transition from M to G1.40 The cells were cultured in DMEM/F12 (Sigma-Aldrich, St. Louis, USA) supplied with 5% foetal bovine serum (Invitrogen, Carlsbad, USA), 2.5 mM L-glutamine and 0.05 mg/mL Gentamycin sulphate (Bio Basic, Markham, Canada) at 37 °C and 5% CO2. Cells were detached using 0.25% Trypsin/EDTA (Invitrogen) and spun down to be resuspended to the desired concentration.
2. Tumour spheroid formation
MCF-7 breast cancer tumour spheroids were formed within hydrogel beads with the culture of cell-laden hydrogel beads formed using a microfluidic flow-focusing method.39 The spheroids were kept in hydrophobic cell culture flasks (Sarstedt, Nümbrecht, Germany) with other culture conditions similar to the previously described adherent cell culture. The average diameter of the spheroids at the point of imaging was 370 ± 90 μm.
3. Spheroid fixation
The alginate shell around the spheroids was removed by suspending them in Ca2+/Mg2+-free phosphate buffered saline (PBS; Invitrogen). Subsequently, the spheroids were fixed using 2% formaldehyde (Ted Pella, Redding, USA) in PBS at room temperature overnight.
B. Clearing solution preparation
1. SeeDB tissue clearing
As described by Ke et al.,33 solutions of 20%, 40%, 60%, 80%, 100%, and 115% wt./vol. fructose (Bio Basic, Markham, ON) were dissolved in ultrapure H2O at room temperature, except the latter two at 65 °C. α-thioglycerol was added after cooling to reach a final concentration of 0.5%.
2. ClearT2 tissue clearing
As described by Kuwajima et al.,32 a 40% polyethylene glycol (PEG) solution in ultrapure H2O was prepared by dissolving PEG 8000 (Bio Basic) in warm water. A 50% formamide/20% PEG solution was made by mixing formamide with 40% PEG/H2O in equal amounts. A 25% formamide/10% PEG solution was prepared by the dilution of the 50% formamide/20% PEG solution in an equal amount of ultrapure H2O.
3. ScaleSQ(0) tissue clearing
As described by Hama et al.,35 a solution of 9.1M urea and 22.5% (w/v) sorbitol in ultrapure H2O was prepared by dissolving urea (Anachemia, Richmond, BC) and sorbitol (Bio Basic) in warm water. The ScaleSQ(0) solution was chosen for our clearing experiments due to its rapid clearing and absence of detergents. As suggested by Hama et al.,35 the solution was kept warm (>30 °C) at all times by incubating at 37 °C in an incubator before use, and by using portable hot packs as well as a lens-warmer setup to warm the solution during the on-chip clearing experiment. We did not observe urea precipitation during our experiments under these conditions.
C. Microfluidic chip design and experimental setup
The experimental setup during tissue clearing is depicted in Figure 1(a). The tumour spheroids, trapped inside the microfluidic device, were imaged through a #1.5 (0.17 mm thick) glass coverslip (Fisher Scientific, Pittsburgh, USA). The microfluidic device was fabricated by poly(dimethylsiloxane) (PDMS) soft lithography using Sylgard 184 (Paisley Products of Canada, Scarborough, Canada) and an SU-8 3050 (Microchem, Westborough, USA) on silicon master with a 300 μm photoresist thickness. After curing, the PDMS devices were demolded and inlet/outlet holes punched using a 0.5 mm coring tool (Harris Uni-Core through Ted Pella, no longer available). The PDMS was bonded to the glass coverslips using a 75 second exposure to air plasma and subsequent contact of the glass and PDMS surfaces. After bonding, the devices were left in a 70 °C oven overnight before flushing the channels with ethanol and water and degassing the chips in water under vacuum for >30 minutes to ensure no bubbles were trapped in the traps. During imaging, the device was loaded upside-down into the upright microscope so that it could be imaged through the cover glass. The microscope was located in a dark enclosure; the chip output tubing was connected to a waste tube inside this enclosure, and the chip input was routed outside the enclosure to permit fluid supply during imaging.
FIG. 1.
Experimental setup during on-chip tissue clearing. (a) Clearing setup on the stage of the two-photon microscope used to monitor the clearing process. Inset shows the schematic of the microfluidic trapping chip, including the small flap structures used to help make the traps more resilient to small amounts of backflow. (b) Phase contrast microscope image of the trapping chip with immobilized hydrogel beads containing dispersed cells.
The design of the microfluidic device is shown in the inset of Figure 1(a). The device consists of a large channel (1.35 mm × 7 mm) containing 12 C-shaped hydrodynamic trapping structures to immobilize 3-D cell cultures. Each of these trapping structures is 300 μm in diameter and contains a small flap at the inlet to help retain the cultures under small amounts of backflow. The flap extends approximately halfway down the channel height, and additional flaps are also integrated into the other pathways of the device to improve trap yield (ensuring that the cultures need to pass by flaps whether they enter the traps or continue down the channel). A phase contrast microscope image of the microfluidic device is shown in Figure 1(b).
D. Tissue clearing setup and procedure
After fixation, spheroids in PBS were loaded into the microfluidic trapping devices using a syringe under positive manual pressure. A 3 mL plastic syringe (BD, Mississauga, Canada) outfitted with a 22G blunt needle tip (Nordson EFD, East Providence, USA) was connected to the microfluidic device friction-fit with another 22G blunt needle via Tygon microbore tubing (“0.020” internal diameter, Cole-Parmer, Montreal, Canada). Tubing pinch-clamps (Cole-Parmer, Montreal, Canada) were used to stop the flow while the syringe was changed to a PBS-containing syringe to prevent bubble introduction into the channel. After rinsing un-trapped spheroids away using PBS, the tubing was clamped and syringe was disconnected. A long tube, pre-filled with clearing solution and connected to a syringe filled with the final clearing solution was then connected to the device input for all clearing methods. Care was taken during tube filling and connection to ensure that bubbles were not introduced to the tubing.
1. SeeDB tissue clearing
We developed an accelerated SeeDB process to expose the spheroids to the increasing concentrations of fructose more rapidly than perfusing each solution sequentially through the long tube. The long tube was pre-loaded with 10 cm lengths of 20%, 40%, 60%, 80%, 100%, and 115% fructose in water (Figure S350). The beads were imaged prior to clearing. The tubing was then un-clamped and the solutions were slowly perfused into the device at a rate of approximately 20 μL/min by applying positive pressure to the syringe using a syringe pump. As the purpose of these different solutions is to gradually expose the micro-tissues to the clearing solution, any mixing of the solutions within the tube due to diffusion or solution flow was not deemed problematic. The solution was continuously perfused during clearing, and the tubing was re-clamped after the spheroid was judged to be sufficiently cleared (which took approximately 20 minutes for the imaged samples).
2. ClearT2 tissue clearing
The long tube was pre-loaded with a 10 cm length of PBS, 40 cm length of 25% formamide and 10% PEG (ClearT2–1), and a 10 cm length of 50% formamide and 20% PEG (ClearT2–2), with the syringe of ClearT2–2 left attached to the inlet. The clearing procedure was the same as the SeeDB tissue clearing methods described above. Again, the solution was continuously perfused during the clearing process and the tubing was re-clamped after the monitored spheroid was judged to be sufficiently cleared.
3. ScaleSQ(0) tissue clearing
The long tube was pre-loaded with a 20 cm length of PBS and 40 cm length of ScaleSQ(0) solution, with the syringe of ScaleSQ(0) left attached to the inlet. The clearing procedure was the same as the SeeDB and ClearT2 tissue clearing methods described above.
E. Imaging
This work utilized a high-NA objective lens (gives diffraction-limited x-y and z-resolutions of 0.19 μm and 0.6 μm, respectively), which would also permit the resolution of small intracellular features or of collagen fibres by simultaneous second harmonic generation imaging.41 If this high resolution is not required, imaging depth could be further improved by using a lower-NA objective lens, which would likely be less susceptible to scattering,42 or by using longer-wavelength excitation43 if it is compatible with the fluorescent labels and microscope system. The orange and green FUCCI expression of the tumour spheroids was imaged both before and after clearing using 2-P microscopy to assess the clearing performance. All imaging was performed using an Olympus FV1000 MPE upright microscope excited with a SpectraPhysics MaiTai DeepSee Ti:Sapphire pulsed laser providing two-photon excitation at 880 nm. A 25X water dipping objective lens optimized for 2-P (XLPLN25XWMP) with an NA of 1.05 and a working distance of 2 mm was used for all imaging. The green and orange FUCCI fluorescence passed through 495–540 nm (green) and 576–630 nm (red) filters before reaching the PMT detectors. Additionally, the microscope permitted the acquisition of an image representing the transmitted laser intensity using the microscope's condenser setup below the microfluidic device. This transmitted laser intensity yielded a differential interference contrast (DIC)-like image of the scanned area.
A two-photon Z-stack of each spheroid (with red, green, and transmitted light colour channels) was acquired before and after clearing with a 5 μm slice spacing. Additionally, a time series of one spheroid per chip, at a Z-depth where light attenuation was present, was acquired during the clearing to monitor the process. This time series was used to discern the endpoint of our clearing process (the point at which the spheroid was judged to be sufficiently cleared and tubing re-clamped).
F. Demonstration of compatibility with on-chip cell culture
The microfluidic devices used for our implementation of on-chip clearing may also be used for on-chip cell culture. We have demonstrated the on-chip culture of arrays of tumour spheroids in such a device, using two-photon imaging to monitor the spheroids' proliferation in 3-D while maintaining good spheroid viability.44 For this work, a custom chamber was designed to keep the microfluidic device immersed in Dulbecco's PBS to maintain channel osmolality while also permitting flipping the device upside-down to be observed with the upright microscope. The enclosed chamber permitted monitoring with both an inverted brightfield microscope and the upright 2-P.
To fabricate the device used for on-chip culture and subsequent tissue clearing, the microfluidic chip was bonded to a 50 mm × 75 mm #1.5 (0.17 mm thick) glass coverslip (Schott Nexterion, Tempe, USA); a rectangular ring of PDMS with an outer size of 50 mm × 75 mm, a height of approximately 10 mm, and a wall thickness of 8 mm was also bonded to the same coverslip to define the chamber. This rectangular PDMS ring was cored with the same 0.5 mm coring tool as the microfluidic chip to access the chamber and route the fluidic inlets and outlets. A 50 mm × 75 mm × 1 mm glass slide was bonded to the top of the PDMS ring to enclose the system, and the chamber was filled with Dulbecco's PBS before use.
After degassing the chip and sterilizing the channel by flowing 70% ethanol, water, PBS, and cell culture media sequentially through channels, the hydrogel bead-based cell cultures containing small MCF-7 tumour spheroids were loaded into the chip 8 days after bead formation. The chamber was filled with Dulbecco's PBS to prevent any evaporation or changes in channel osmolarity caused by water evaporation through the PDMS, and the channel was perfused with cell culture media at a rate of 1 μL/min. The spheroids were cultured on-chip for 9 days and then fixed on-chip using 4% paraformaldehyde in PBS. After fixation, the spheroids were rinsed with PBS and cleared using a single-step SeeDB-like process,45 in which the channel was immediately perfused with the 115% fructose in water solution while monitoring using two-photon microscopy. The single-step process was chosen for this proof-of-concept experiment due to its rapid clearing and simple experimental process. Reduced sample shrinkage (Table S150) as well as moderate autofluorescence (Figure S450) would be expected using the accelerated multistep microfluidic clearing process described in Section II D.
G. Image processing
Images were histogram-adjusted in ImageJ (NIH, http://imagej.nih.gov/ij/) to ensure visibility in print. For the purpose of comparing images, the same histogram adjustment was made to each image. Maximum intensity 3-D renderings were created from the Z-stack data using BioView3D (from the Center for Bio-Image Informatics, UCSB) and Icy (from the Quantitative Image Analysis Unit, Institut Pasteur, Paris, France). Again, each Z-stack and rendering was made using the same process for the purposes of comparison. Image measurements were made either manually in ImageJ or using custom scripts written using MATLAB® (Mathworks, Natick, USA) where indicated.
For calculations of spheroid size change after treatment as well as transmitted light intensity change, the spheroid transmitted light images were analysed. The area change was calculated as Apost/Apre, where Apost and Apre are the spheroid areas after and before treatment, respectively. These areas were calculated by manually segmenting the transmitted laser intensity image of the Z-stack frame which was observed to have best focus of the outside edge of the spheroid. This same segmentation was used to calculate the average transmitted light intensity change after clearing. The transmitted light intensity before and after clearing (Tpre and Tpost, respectively) was quantified by dividing the average transmitted light intensity in the segmented spheroid region by the maximum image value (4095 for the 12-bit images used). As all images were acquired using the same imaging parameters, the transmitted light intensities for the different clearing processes can be compared.
In order to quantify the effects of tissue clearing on image quality, we analyzed spheroid fluorescence intensity in the red channel as a function of objective Z-step depth into the sample, before and after treatment, for three spheroids cleared with μSeeDB, three spheroids cleared with μClearT2, and three spheroids cleared with μScaleSQ(0). We chose to analyze both the average intensity within the spheroid region as well as the standard deviation of the intensity. The average intensity quantifies the overall brightness of the fluorescence, while the standard deviation gives a measure of the range of fluorescent intensities detected within the spheroid region (with a wider range of intensities indicative of less blurriness and higher contrast).
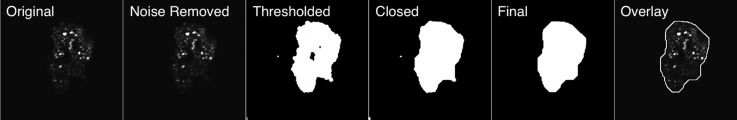
The fluorescent regions in a denoised red channel two photon fluorescence image at each depth were first segmented using a custom MATLAB script using a low intensity threshold of 0.003 a.u. (chosen to accurately discern the spheroid area and held constant for all image stacks analyzed). This threshold was selected by running the segmentation using several thresholds and comparing the segmentations' ability to separate the cell-containing spheroid region from the background. Otsu's method of choosing the segmentation threshold46 was also attempted; however, it was not found to be more effective (potentially due to the large variance in nucleus intensities present within the spheroid regions). These segmented regions were then dilated and eroded (morphological close operation), and subsequently eroded and then dilated (morphological open operation) using a disk-shaped structuring element with 50 pixel radius to fill in the spheroid regions and remove segmented non-spheroid regions. Holes in the segmented regions were filled and isolated segmented regions of size less than 300 pixels were removed. The segmentation process was run on each Z-slice within each image stack in order to quantify its intensity information. The steps of the segmentation process are illustrated in Figure 2.
FIG. 2.
Results of segmentation process used for analyzing spheroid fluorescence intensity with depth. The original image, noise removed image, thresholded segmentation, closed thresholded segmentation, and final segmentation are shown, and the final segmentation is shown overlaid upon the original image. The area inside the segmentation was used for the calculation of the mean intensity and the standard deviation of the intensity.
The intensities of the final segmented regions in the original (not denoised) fluorescence image were then averaged, and the standard deviation of these pixel intensities was also calculated as a measure of image contrast in the spheroid-containing region. Slices deep in the uncleared spheroids tend to exhibit blurriness of the fluorescent nuclei due to scattering effects, which reduces image contrast in this region. The results from 3 to 5 spheroids were quantified for each clearing type, and the mean and standard error of the 3–5 measurements were plotted. Both the average intensity and the standard deviation of the intensity within the segmented region were plotted versus objective Z-step depth into the spheroid, and the plots from before and after clearing were plotted on the same axes.
III. RESULTS
A. Clearing increases fluorescence imaging penetration depth
Figure 3 presents a comparison of images acquired before and after clearing obtained with 2-P microscopy using the μSeeDB, μClearT2, and μScaleSQ(0) clearing methods. Figures 3(a) and 3(b) show the images of a spheroid prior to (a) and after (b) clearing with μSeeDB, while Figures 3(c) and 3(d) show the images of a spheroid prior to (c) and after (d) clearing with μClearT2. Figures 3(e) and 3(f) show the images of a spheroid prior to (c) and after (d) clearing with μScaleSQ(0).
FIG. 3.
Results of on-chip tissue clearing of tumour spheroid cultures obtained with 2-P microscopy using μSeeDB (a) and (b), μClearT2 (c) and (d), and μScaleSQ(0) (e) and (f) solutions. Images depict the FUCCI fluorescent protein fluorescence of the tumour spheroid cultures. Cross-sectional image slices at various objective Z-step depths into the spheroids, histogram adjusted version of the deepest cross-sections shown, maximum Z-intensity projection images, and 3-D renderings reconstructed from the two-photon Z-stack are presented for each clearing type before (left—(a), (c), and (e)) and after (right—(b), (d), and (f)) the clearing process. All three clearing processes appear to improve imaging quality deep into the spheroid, with enhanced light penetration and sharper images visible after clearing. The μSeeDB process induces green autofluorescence, while the μClearT2 and μScaleSQ(0) processes also appear to induce a shift in the colour of the orange fluorescent nuclei (fluorescent nuclei become more yellow). The ClearT2 process offers a more moderate improvement in brightness than the other two processes. All scale bars represent 100 μm.
Figures 3(a)–3(f) show 2-P slice images at four objective Z-step depths (with images of the same spheroid matched to best show approximately the same spheroid position), as well as a maximum Z-intensity projection image and a maximum intensity projection 3-D rendering of the spheroid. The histogram-adjusted image at the deepest Z-step location is also depicted, with the same histogram adjustment made to each of the 6 images (the minimum level remained at 0, while the maximum level was reduced from 255 to 127).
Figures 3(a)–3(b) show that the μSeeDB process appears to induce green autofluorescence in the sample, which has the potential to confound imaging of the green channel. Figures 3(c)–3(f) show that the μClearT2 and μScaleSQ(0) processes also appear to change the fluorescence characteristics of the sample. Although the green fluorescent nuclei do not appear to significantly change, the orange fluorescent nuclei appear to shift from a more reddish colour to a more yellowish colour (perhaps indicative of a blue-shift of the fluorescence emission characteristics, or perhaps induction of autofluorescence only within the orange nuclei).
It is evident that all three clearing methods improve visibility of deeper parts of the spheroid, increasing light penetration as well as reducing blurring of the nuclei deep in the sample. The area and transmittance changes induced by each clearing process are presented in Table I. For our spheroid samples, we find that the μSeeDB and μClearT2 methods induce minimal sample volume changes at the endpoint; however, we did find that for the μSeeDB process the sample shrinkage is dependent on flow rate in the microfluidic channel (Figure S250), with higher flow rates leading to higher shrinkage. This effect is described and quantified in the supplementary material.50 We find that μScaleSQ induces sample swelling, likely due to the hyperhydration caused by the urea.47 All three processes significantly increase the average transmitted light intensity through the sample, with μSeeDB and μScaleSQ offering a greater increase in the transmitted intensity than μClearT2.
TABLE I.
Comparison of spheroid areas (A) and transmittances (T) before (Apre, Tpre) and after (Apost, Tpost) on-chip clearing.
| Clearing type | μSeeDB (N = 4) | μClearT2 (N = 3) | μScaleSQ (N = 4) |
|---|---|---|---|
| (μm2 ) | (121 ± 55) × 103 | (93 ± 50) × 103 | (107 ± 65) × 103 |
| (%) | 102 ± 8 | 108 ± 5 | 117 ± 2 |
| (%) | 46.0 ± 3.4 | 45.2 ± 0.5 | 43.2 ± 2.0 |
| (%) | 51.5 ± 2.0 | 49.2 ± 2.2 | 50.7 ± 2.4 |
As another measure of clearing efficacy, we quantified spheroid fluorescence intensity in the red channel as a function of objective Z-step depth into the sample, before and after treatment, for five spheroids cleared with μSeeDB, five spheroids cleared with μClearT2, and three spheroids cleared with μScaleSQ(0). The analysis process is described in the Image Processing section of the Methods. The results of this process are plotted in Figure 4. Figures 4(a)–4(c) present these results, plotting the mean and standard error of the beads studied after μSeeDB (a), μClearT2 (b), and μScaleSQ(0) (c). For each clearing type, we plot the average red channel fluorescence intensity in the segmented region, as well as the standard deviation of the intensities in the segmented region as a measure of image blur and contrast.
FIG. 4.
Analysis of average red channel fluorescence intensity in the spheroid regions before (black) and after (red) clearing, for three clearing types. The average spheroid fluorescence intensity and standard deviation of the intensities within the spheroid region were calculated and the mean and standard errors of the results from 3 to 5 spheroids are plotted. μSeeDB (a) results in a marked improvement in intensity and intensity standard deviation with depth. μClearT2 (b) results in a moderate improvement in intensity and a larger improvement in standard deviation with depth into the sample. μScaleSQ(0) results in a marked improvement in intensity and standard deviation with depth, significantly increasing the depth into which the sample could be imaged. Error bars depict the standard error of N = 3–5 measurements (indicated with the clearing type), and are primarily due to different spheroid morphologies.
Both the average intensity and intensity standard deviation at depths greater than 100 μm increase after clearing for all three clearing types, consistent with the qualitative improvement shown in Figure 3. Both μSeeDB and μScaleSQ(0) significantly increased the measured intensities deep in the spheroid, and also significantly increased the depths to which the spheroid could be imaged. Although μClearT2 resulted in a more modest improvement in the intensity characteristics, this still resulted in an improvement in the image quality as shown in Figure 3.
B. On-chip clearing is compatible with microfluidic devices used for on-chip culture and monitoring
The results of our on-chip culture and clearing within the same microfluidic device are presented in Figure 5. All images depict the same spheroid at different points in the experiment. We have previously demonstrated excellent spheroid viability (89 ± 5% viability after 9 days of on-chip culture, not significantly different from the 93 ± 2% viability of spheroids grown in a standard cell culture flask) and similar spheroid proliferation within the microfluidic environment as in standard cell culture flasks;44 An example viability staining image and plot of spheroid proliferation are shown in Figures 5(a)–5(c). Figures 5(d) and 5(e) present maximum Z-intensity projection images of the spheroid 13 days (d) and 17 days (e) after hydrogel bead formation, showing the increase in spheroid size (indicative of spheroid proliferation) between these two imaging points.
FIG. 5.
Demonstration of the compatibility of a single-step on-chip SeeDB-based clearing process with microfluidic devices used for on-chip cell culture. FUCCI-expressing MCF-7 cell nuclei were imaged with two-photon microscopy, appearing green when dividing and orange when in the interphase stages of their cell cycle. (a) and (b) 2-P slice images with (a) and without (b) transmitted light overlay showing FUCCI-expressing nuclei (orange, green) and fixable viability staining using eFluor 450®, which labels dead nuclei blue. Live spheroids show holes in the blue stain for live nuclei, while dead cells exhibit blue nuclei. (c) Mean spheroid diameter over time in culture, for spheroids both in the flask and in the microfluidic chip. Similar spheroid proliferation is observed on and off-chip. (d) and (e) Maximum Z-intensity projection images of the spheroid 13 days (d) and 17 days (e) after hydrogel bead formation, showing the increase in spheroid size between these two imaging points. (f)–(h) Two-photon fluorescence Z-slice images of the same spheroid at different points during the clearing process. (f) Prior to fixation, during imaging at day 17. A slice approximately 175 μm into the spheroid is shown. (g) After on-chip fixation in 4% paraformaldehyde, conducted immediately after imaging at day 17. (h) After a single-step μSeeDB process, in which the spheroid was immediately perfused with the 115% fructose solution while monitoring with two-photon microscopy. Both fixation and clearing were performed in the same chip as the spheroid culture. (a)–(e) Reproduced with permission from Grist et al., in The 19th International Conference on Miniaturized Systems for Chemistry and Life Sciences (MicroTAS 2015), Gyeongju, Korea (2015), pp. 594–596. Copyright 2004 Chemical and Biological Microsystems Society, CBMS.44 All scale bars represent 100 μm.
Figures 5(f)–5(h) present the images of this same spheroid at the study endpoint before and after clearing. Figure 5(f) presents a two-photon fluorescence Z-slice image at day 17 (a slice approximately 175 μm into the spheroid is shown). Figure 5(g) presents a two-photon fluorescence Z-slice image of the same spheroid after fixation in 4% paraformaldehyde, conducted immediately after imaging at day 17. We observed that both the transmitted light intensity (not shown) and the fluorescence intensity decreased after paraformaldehyde fixation, consistent with the findings reported in the previous work on SeeDB33 suggesting that fixation decreases the depth to which tissues can be imaged. Fixation also resulted in spheroid shrinkage and deformation into a curved shape, potentially due to the initial concave morphology of this spheroid combined with the osmotic pressure of the fixative. Finally, Figure 5(h) presents a two-photon fluorescence Z-slice image of the same spheroid after a single-step μSeeDB process, in which the spheroid was immediately perfused with the 115% fructose solution while monitoring with two-photon microscopy. Many more fluorescent nuclei are visible in the spheroid core after clearing in Figure 5(h) than in the un-cleared live in Figure 5(f) or fixed in Figure 5(g) spheroid images. Some green autofluorescence induced by the SeeDB process is visible, while both the orange and green nuclei in the spheroid centre are much more visible and better-resolved after clearing. Figures 5(f)–5(h) present the slice images taken at approximately the same position in the sample.
This work demonstrates the compatibility of the on-chip clearing implementation with microfluidic on-chip cell culture. Since the same microfluidic devices were used for all of our on-chip clearing studies (μSeeDB, μClearT2, and μScaleSQ(0)), it follows that all of the investigated clearing protocols could be applied directly after on-chip culture and fixation. This compatibility is highly beneficial because it permits tracking of the same 3-D cultures during their culture, during any test conditions such as drug treatment, as well as during staining, fixation, and clearing.
C. On-chip clearing is rapid and permits monitoring of 3-D cultures during clearing
All clearing experiments performed on-chip were conducted in less than 1 h, which is a significant improvement over the multi-day original SeeDB process. We believe that the combination of smaller diffusion distances and the constant supply of fresh clearing solution to the sample helps to expedite this rapid clearing.
Another advantage of the on-chip clearing method is that it permits monitoring of the clearing process. This monitoring is advantageous as it allows the endpoint of clearing to be more accurately discerned, permitting more expedient imaging: specifically, the prolonged exposure to SeeDB reagents can increase sample autofluorescence over time, and the formamide in ClearT2 is not suitable for long-term sample storage.32 Monitoring also allows us to visualize the same spheroid at different stages of the clearing process, facilitating the optimization of clearing protocols as it can permit the visualization of sample changes in response to the clearing assays that could induce artefacts. We have not observed visible bleaching of the FUCCI fluorescent proteins during the monitoring process. Examples of this in situ monitoring capability are presented in Figure 6.
FIG. 6.
Monitoring of spheroid size and transmitted light intensity during the accelerated multistep μSeeDB, two-step μClearT2, and one-step μScaleSQ clearing processes. (a), (c), and (e) Spheroid area is plotted vs. time during the μSeeDB (a), μClearT2 (c), and μScaleSQ (e) clearing processes. (b), (d), and (f) Measured fluorescence intensity in the red channel and transmitted light intensity of the spheroids are plotted vs. time during the μSeeDB (b), μClearT2 (d), and μScaleSQ (f) clearing processes. The depth of the optical slice at which the fluorescence intensities are obtained is approximately 125 μm, 190 μm, and 135 μm for μSeeDB (b), μClearT2 (d), and μScaleSQ (f), respectively.
We acquired both 2-P fluorescence and transmitted light intensity images at a single Z-plane during the processes, acquiring one frame every ∼11 s. We segmented the spheroid from the transmitted light intensity images and plotted the spheroid size in Figures 6(a), 6(c), and 6(e) and average transmitted light intensity in Figures 6(b), 6(d), and 6(f) during the accelerated multistep μSeeDB in Figures 6(a) and 6(b), two-step μClearT2 in Figures 6(c) and 6(d), and single-step μScaleSQ(0) processes in Figures 6(e) and 6(f). As a demonstration of the utility of this ability, we found that during the μClearT2 process, our spheroid samples first shrunk to approximately 80% of their original area, and then expanded back to close to their initial size (Figure 6(b) and inset images). μClearT2 was previously reported (with only endpoint analysis) to not cause a significant sample volume change.32,37 μScaleSQ(0) also first shrinks and then expands, as was described in its original demonstration.35 This shrinkage-expansion process for μClearT2 and μScaleSQ(0) is likely due to an initial osmotic shrinkage followed by swelling due to hyperhydration; formamide (which is similar to urea) may clear tissues by a similar hyperhydration mechanism.47 Awareness of responses like this could be important to the users of this clearing method as the shrinkage-expansion process has the potential to induce imaging artefacts. Our microfluidic implementation facilitates the monitoring required to discover these types of effects.
IV. CONCLUSIONS
We have demonstrated on-chip clearing of arrays of tumour spheroid cultures using the SeeDB fructose-based tissue clearing process, the ClearT2 formamide-PEG clearing process, and the ScaleSQ(0) clearing process based on urea and sorbitol. The on-chip tissue clearing protocol yields rapid (<1 h) clearing of arrays of 3-D cultures using all three methods. The unique microfluidic implementation reduces spheroid loss during clearing and allows 3-D cultures to be monitored during the clearing process. Additionally, the same spheroid can be easily imaged at different stages of clearing. The monitoring facilitated by our microfluidic process allowed us to observe a spheroid shrinkage-expansion process during ClearT2 treatment that, to our knowledge, had not been previously reported as previous work (finding minimal sample volume changes) used endpoint analysis alone. This type of shrinkage and expansion could lead to sample changes and imaging artefacts, so the awareness of these effects enabled by monitoring could be beneficial to researchers developing clearing assays.
Although we demonstrate the procedure using the SeeDB, ClearT2, and ScaleSQ(0) clearing solutions, the versatile on-chip implementation is also compatible with other clearing protocols. For example, FRUIT,34 CUBIC,48 or ClearT,32 could also be implemented in this on-chip manner and may offer improved results for different types of 3-D cultures while retaining the advantages offered by the microfluidic implementation. ScaleSQ(5), another ScaleSQ variant, could also be implemented as its 5% concentration of Triton X-100 has been found to result in improved clearing efficacy.35 Another interesting process that could be implemented on-chip is the SeeDB2 clearing protocol,52 which uses solutions of iohexol, refractive index-matched to objective immersion oil, to reduce both scattering and spherical aberrations and permit super-resolution microscopy. This increases the versatility of the clearing platform, as different types of 3-D cultures and micro-tissues could respond differently to different clearing protocols and the platform could aid in the protocol optimization for different tissue types.
We also demonstrated a proof-of-concept on-chip study, in which tumour spheroids grown and monitored on-chip were fixed and cleared in the same microfluidic device, permitting monitoring of the same spheroids throughout the process. We anticipate that this capability will aid in the development of on-chip array-based drug screening assays, in which arrays of 3-D cell cultures can be monitored in 3-D throughout their culture, drug treatment, staining, fixation, and clearing. Additionally, the process will be compatible with microfluidic devices that we have developed for microenvironment control,49 further increasing the scope of these results. Future work could involve increasing the microfluidic array size to simultaneously clear larger arrays of tissues, optimizing the process for other types of micro-tissues, and applying this on-chip clearing implementation to drug screening or other 3-D culture assays.
ACKNOWLEDGMENTS
We thank Jonathan Schmok for contributions to image processing, Meng-Chi (Andy) Liu for assistance with device fabrication, Eric Cheng for assistance with confocal imaging, and Kevin Hodgson and Garnet Martens for assistance with imaging and fixation protocols. Also, we would like to thank Bruce Hou and Anika Meng for the help in image processing. We are grateful to the Canadian Breast Cancer Foundation—BC/Yukon Region, the Natural Sciences and Engineering Research Council of Canada (NSERC), the Canadian Institutes of Health Research (CIHR), and the Canadian Microelectronics Corporation (CMC) Microsystems for graduate and project funding. We also acknowledge The UBC Bioimaging Facility where the imaging and on-chip cell culture were conducted.
References
- 1. Young E. W. K., Integr. Biol. (9), 1096–1109 (2013). 10.1039/c3ib40076j [DOI] [PubMed] [Google Scholar]
- 2. Abbott A., Nature , 870–872 (2003). 10.1038/424870a [DOI] [PubMed] [Google Scholar]
- 3. Griffith L. G. and Swartz M. a., Nat. Rev. Mol. Cell Biol. , 211–224 (2006). 10.1038/nrm1858 [DOI] [PubMed] [Google Scholar]
- 4. Achilli T. M., McCalla S., Meyer J., Tripathi A., and Morgan J. R., Mol. Pharm. (7), 2071–2081 (2014). 10.1021/mp500002y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Minchinton A. I. and Tannock I. F., Nat. Rev. Cancer (8), 583–592 (2006). 10.1038/nrc1893 [DOI] [PubMed] [Google Scholar]
- 6. Friedrich J., Ebner R., and Kunz-Schughart L. A., Int. J. Radiat. Biol. (11–12), 849–871 (2007). 10.1080/09553000701727531 [DOI] [PubMed] [Google Scholar]
- 7. Desoize B., Crit. Rev. Oncol./Hematol. (2–3), 59–60 (2000). 10.1016/S1040-8428(00)00076-7 [DOI] [PubMed] [Google Scholar]
- 8. Kunz-Schughart L. a., Cell Biol. Int. (3), 157–161 (1999). 10.1006/cbir.1999.0384 [DOI] [PubMed] [Google Scholar]
- 9. Kundu M. and Thompson C. B., Annu. Rev. Pathol. , 427–455 (2008). 10.1146/annurev.pathmechdis.2.010506.091842 [DOI] [PubMed] [Google Scholar]
- 10. Sui X., Chen R., Wang Z., Huang Z., Kong N., Zhang M., Han W., Lou F., Yang J., Zhang Q., Wang X., He C., and Pan H., Cell Death Dis. , e838 (2013). 10.1038/cddis.2013.350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li X., Xu H.-l., Liu Y.-x., An N., Zhao S., and Bao J.-k., Acta Pharmacol. Sin. (5), 612–624 (2013). 10.1038/aps.2013.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vaupel P., Oncologist , 21–26 (2008). 10.1634/theoncologist.13-S3-21 [DOI] [PubMed] [Google Scholar]
- 13. Astolfi M., Peant B., Lateef M. A., Rousset N., Kendall-Dupont J., Carmona E., Monet F., Saad F., Provencher D., Mes-Masson A. M., and Gervais T., Lab Chip (2), 312–325 (2016). 10.1039/C5LC01108F [DOI] [PubMed] [Google Scholar]
- 14. Ju T., Warren J., Carson J., Bello M., Kakadiaris I., Chiu W., Thaller C., and Eichele G., J Neurosci. Methods (1–2), 84–100 (2006). 10.1016/j.jneumeth.2006.02.020 [DOI] [PubMed] [Google Scholar]
- 15. Keller P. J., Methods (3), 268–278 (2013). 10.1016/j.ymeth.2013.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pampaloni F., Ansari N., and Stelzer E. H. K., Cell Tissue Res. , 161–177 (2013). 10.1007/s00441-013-1589-7 [DOI] [PubMed] [Google Scholar]
- 17. Warden R., Saunders J., and Tsourkas A., Cancer Biol. Ther. (23), 2235–2236 (2009). 10.4161/cbt.8.23.10270 [DOI] [PubMed] [Google Scholar]
- 18. Gratton E., Barry N. P., Beretta S., and Celli A., Methods (1), 103–110 (2001). 10.1006/meth.2001.1219 [DOI] [PubMed] [Google Scholar]
- 19. Oheim M., Michael D. J., Geisbauer M., Madsen D., and Chow R. H., Adv. Drug Delivery Rev. (7), 788–808 (2006). 10.1016/j.addr.2006.07.005 [DOI] [PubMed] [Google Scholar]
- 20. Brown E. B., Campbell R. B., Tsuzuki Y., Xu L., Carmeliet P., Fukumura D., and Jain R. K., Nat. Med. (9), 1069–1069 (2001). 10.1038/nm0901-1069 [DOI] [PubMed] [Google Scholar]
- 21. Bullen A., Nat. Rev. Drug Discovery (1), 54–67 (2008). 10.1038/nrd2446 [DOI] [PubMed] [Google Scholar]
- 22. Ma H. L., Jiang Q., Han S., Wu Y., Cui Tomshine J., Wang D., Gan Y., Zou G., and Liang X. J., Mol. Imaging (6), 487–498 (2012). 10.2310/7290.2012.00012 [DOI] [PubMed] [Google Scholar]
- 23. Cheong W. F., Prahl S. A., and Welch A. J., IEEE J. Quantum Electron. (12), 2166–2185 (1990). 10.1109/3.64354 [DOI] [Google Scholar]
- 24. Marx V., Nat. Methods (12), 1209–1214 (2014). 10.1038/nmeth.3181 [DOI] [PubMed] [Google Scholar]
- 25. Chung K., Wallace J., Kim S. Y., Kalyanasundaram S., Andalman A. S., Davidson T. J., Mirzabekov J. J., Zalocusky K. A., Mattis J., Denisin A. K., Pak S., Bernstein H., Ramakrishnan C., Grosenick L., Gradinaru V., and Deisseroth K., Nature (7449), 332 (2013). 10.1038/nature12107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. le Roux L., Volgin A., Maxwell D., Ishihara K., Gelovani J., and Schellingerhout D., Mol. Imaging (5), 214–221 (2008). 10.2310/7290.2008.00023 [DOI] [PubMed] [Google Scholar]
- 27. Groebe K. and Mueller-Klieser W., Int. J. Radiat. Oncol., Biol., Phys. (2), 395–401 (1996). 10.1016/0360-3016(95)02065-9 [DOI] [PubMed] [Google Scholar]
- 28. Grist S. M., Cheng E., Yu L. F., and Cheung K. C., in The 18th International Conference on Miniaturized Systems for Chemistry and Life Sciences (MicroTAS 2014), San Antonio, Texas (2014), pp. 551–553. [Google Scholar]
- 29. Susaki E. A., Tainaka K., Perrin D., Kishino F., Tawara T., Watanabe T. M., Yokoyama C., Onoe H., Eguchi M., Yamaguchi S., Abe T., Kiyonari H., Shimizu Y., Miyawaki A., Yokota H., and Ueda H. R., Cell (3), 726–739 (2014). 10.1016/j.cell.2014.03.042 [DOI] [PubMed] [Google Scholar]
- 30. Dodt H. U., Leischner U., Schierloh A., Jahrling N., Mauch C. P., Deininger K., Deussing J. M., Eder M., Zieglgansberger W., and Becker K., Nat. Methods (4), 331–336 (2007). 10.1038/nmeth1036 [DOI] [PubMed] [Google Scholar]
- 31. Becker K., Jahrling N., Saghafi S., Weiler R., and Dodt H. U., Plos One (3), e33916 (2012). 10.1371/journal.pone.0033916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kuwajima T., Sitko A. a., Bhansali P., Jurgens C., Guido W., and Mason C., Development (6), 1364–1368 (2013). 10.1242/dev.091844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ke M.-T., Fujimoto S., and Imai T., Nat. Neurosci. (8), 1154–1161 (2013). 10.1038/nn.3447 [DOI] [PubMed] [Google Scholar]
- 34. Hou B., Zhang D., Zhao S., Wei M., Yang Z., Wang S., Wang J., Zhang X., Liu B., Fan L., Li Y., Qiu Z., Zhang C., and Jiang T., Front. Neuroanat. , 1–11 (2015). 10.3389/fnana.2015.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hama H., Hioki H., Namiki K., Hoshida T., Kurokawa H., Ishidate F., Kaneko T., Akagi T., Saito T., Saido T., and Miyawaki A., Nat. Neurosci. (10), 1518 (2015). 10.1038/nn.4107 [DOI] [PubMed] [Google Scholar]
- 36. Kim S. Y., Chung K., and Deisseroth K., Trends Cognit. Sci. (12), 596–599 (2013). 10.1016/j.tics.2013.10.005 [DOI] [PubMed] [Google Scholar]
- 37. Boutin M. E. and Hoffman-Kim D., Tissue Eng. Part C (3), 292–302 (2015). 10.1089/ten.tec.2014.0296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Das R., Agrawal A., Upton M. P., and Seibel E. J., SPIE , 89410N (2014). 10.1117/12.2041114 [DOI] [Google Scholar]
- 39. Yu L., Grist S. M., Nasseri S. S., Cheng E., Hwang Y. C. E., Ni C., and Cheung K. C., Biomicrofluidics (2), 024118 (2015). 10.1063/1.4918754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sakaue-Sawano A., Kurokawa H., Morimura T., Hanyu A., Hama H., Osawa H., Kashiwagi S., Fukami K., Miyata T., Miyoshi H., Imamura T., Ogawa M., Masai H., and Miyawaki A., Cell (3), 487–498 (2008). 10.1016/j.cell.2007.12.033 [DOI] [PubMed] [Google Scholar]
- 41. Cheng E., Song C., Yu L., and Cheung K. C., in 18th International Conference on Miniaturized Systems for Chemistry and Life Sciences (MicroTAS 2014) (Royal Society of Chemistry, San Antonio, Texas, USA, 2014), pp. 2514–2515. [Google Scholar]
- 42. Tung C. K., Sun Y., Lo W., Lin S. J., Jee S. H., and Dong C. Y., Microsc. Res. Tech. (6), 308–314 (2004). 10.1002/jemt.20116 [DOI] [PubMed] [Google Scholar]
- 43. Kobat D., Durst M. E., Nishimura N., Wong A. W., Schaffer C. B., and Xu C., Opt. Express (16), 13354–13364 (2009). 10.1364/OE.17.013354 [DOI] [PubMed] [Google Scholar]
- 44. Grist S. M., Nasseri S. S., Poon T., Liu M.-C., Roskelley C., and Cheung K. C., in The 19th International Conference on Miniaturized Systems for Chemistry and Life Sciences (MicroTAS 2015), Gyeongju, Korea (2015), pp. 594–596. [Google Scholar]
- 45. Grist S. M., Nasseri S. S., Ni C., Roskelley C., and Cheung K. C., in The 19th International Conference on Miniaturized Systems for Chemistry and Life Sciences (MicroTAS 2015), Gyeongju, Korea (2015), pp. 308–310. [Google Scholar]
- 46. Otsu N., IEEE Trans. Syst. Man Cybern. (1), 62–66 (1979). 10.1109/TSMC.1979.4310076 [DOI] [PubMed] [Google Scholar]
- 47. Richardson D. S. and Lichtman J. W., Cell (2), 246–257 (2015). 10.1016/j.cell.2015.06.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Susaki E. A., Tainaka K., Perrin D., Yukinaga H., Kuno A., and Ueda H. R., Nat. Protoc. (11), 1709–1727 (2015). 10.1038/nprot.2015.085 [DOI] [PubMed] [Google Scholar]
- 49. Grist S., Schmok J., Liu M.-C., Chrostowski L., and Cheung K., Sens.-Basel (8), 20030 (2015). 10.3390/s150820030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.See supplementary material at http://dx.doi.org/10.1063/1.4959031E-BIOMGB-10-009604 for a comparison of confocal and two-photon images of 3-D cultures as well as further analysis of sample shrinkage during clearing.
- 51. Hama H., Kurokawa H., Kawano H., Ando R., Shimogori T., Noda H., et al. , Nature Neurosci. , 1481–1488 (2011). 10.1038/nn.2928 [DOI] [PubMed] [Google Scholar]
- 52. Ke M. T., Nakai Y., Fujimoto S., Takayama R., Yoshida S., Kitajima T. S., et al. , Cell Rep. , 2718–2732 (2016). 10.1016/j.celrep.2016.02.057 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- See supplementary material at http://dx.doi.org/10.1063/1.4959031E-BIOMGB-10-009604 for a comparison of confocal and two-photon images of 3-D cultures as well as further analysis of sample shrinkage during clearing.