Abstract
A 41-year-old woman presented 8 years after a left total hip arthroplasty. She complained of progressive groin pain for several months. Radiographs demonstrated a hard-on-hard bearing surface combination and radiolucent lines surrounding the acetabular shell. Laboratory analysis revealed a mild leukocytosis, a normal erythrocyte sedimentation rate, and a mildly elevated C-reactive protein. Serum cobalt and chromium levels were markedly elevated. Aspiration of the hip joint was negative for infection. Magnetic resonance imaging failed to demonstrate a pseudotumor. Revision total hip arthroplasty was performed, and a ceramic-on-metal bearing surface combination was explanted. Significant intraoperative findings included dark gray synovial fluid, metal transfer onto the ceramic femoral head, and a grossly loose acetabular shell pivoting about a single well-fixed screw. The explanted components otherwise appeared normal macroscopically. Histologic analysis of the capsular tissue demonstrated aseptic lymphocyte-dominated vasculitis-associated lesion and inclusion bodies consistent with third-body wear. Revision arthroplasty to a ceramic-on-polyethylene bearing surface combination was performed with a good clinical result and laboratory normalization at 9-month follow-up.
Keywords: Adverse reaction to metal debris, Ceramic-on-metal, Metal-on-metal, Total hip arthroplasty
Introduction
As the number of young and active patients undergoing total hip arthroplasty (THA) increases [1], the search for the ideal bearing surface combination that has minimal wear and permits durable long-term results is ongoing. There are multiple alternatives for bearing surfaces, and each has unique characteristics that must be considered before utilization in the operative theater. Currently available acetabular liners include polyethylene, cobalt-chrome, and ceramic options. Femoral head options include cobalt-chrome, ceramicized metal, and ceramic designs. Although the metal-on-polyethylene (MoP) bearing surface combination—in which a cobalt-chrome femoral head articulates with a polyethylene acetabular liner—has a proven track record and excellent long-term results [2], hard-on-hard bearing surface combinations using pairings of the available metal and ceramic components have remained an attractive alternative because of in vitro studies reporting decreased volumetric wear [3].
Recently, the metal-on-metal (MoM) bearing surface combination has fallen out of favor because of complications associated with metal debris particles. The American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, the Hip Society, and multiple other authors have published guidelines on monitoring and management of patients with MoM hips 4, 5. Although technology for ceramic componentry is evolving, early-generation ceramic-on-ceramic hips were fraught with complications that included squeaking and component fracture 6, 7. Therefore, the ceramic-on-metal (CoM) and metal-on-ceramic (MoC) bearing surface options were introduced with the theoretical advantage of minimizing the complications associated with ceramic-on-ceramic hips and MoM hips [8].
Initial enthusiasm for CoM and MoC hips originated from industry-sponsored hip simulator analyses 9, 10, 11 and a limited number of in vivo clinical trials with short-term follow-up 11, 12, 13. Despite previous reports of CoM and MoC bearing surfaces possessing good functional outcomes at short-term follow up, elevations in cobalt and chromium levels were observed that often paralleled levels seen in patients with MoM hips 11, 12, 13. The significance of elevated metal ion levels was underappreciated at the time, and it is estimated that the CoM bearing surface combination alone was used in >10,000 THAs [14]. As the body of evidence regarding adverse reactions to metal debris in MoM and MoP hips continues to evolve 8, 15, reports of this situation in CoM and MoC hips are distinctively lacking in the literature. To our knowledge, only 2 case reports exist which describe metal debris–associated complications in patients with the MoC bearing surface combination 16, 17, with no reports describing these same complications in patients having previously undergone CoM THA.
Therefore, we report the case of a patient who came to our clinic with a painful CoM THA and describe the clinical presentation, workup, and management of this scenario.
Case history
A 41-year-old woman with no significant medical history underwent uncemented left THA at an outside facility for degenerative osteoarthritis. Outside records were obtained and reported that she had undergone CoM THA as a participant in a multicenter clinical study. Implanted components included Pinnacle Gription titanium acetabular shell (52 mm), with a single titanium screw for additional fixation, cobalt-chrome acetabular liner (52 × 36 mm), Biolox (CeramTech, Plochingen, Germany) Delta ceramic femoral head (36 + 5 mm), and Summit Porocoat titanium femoral stem with high offset neck (size 12) (Johnson and Johnson-DePuy Orthopaedics, Inc., Warsaw, IN, USA).
After index THA, the patient was made weight bearing as tolerated and actively participated in formal physical therapy. Her postoperative course was unremarkable, and the patient quickly returned to her preoperative functional level with no pain or limitations. Approximately 8 years postoperatively, the patient presented to our clinic reporting several months of progressively worsening left groin pain which was causing her to miss days at work. She had not experienced any recent trauma and denied systemic symptoms such as fever or chills.
Physical examination revealed an antalgic gait and painful decreased left hip range of motion. She did not have a Trendelenburg sign. The surgical site was appropriately healed, and the overlying skin was benign. There was no palpable soft tissue mass over the greater trochanter. The patient's weight, height, and body mass index were 84 kg, 165 cm, and 31 kg/m2, respectively.
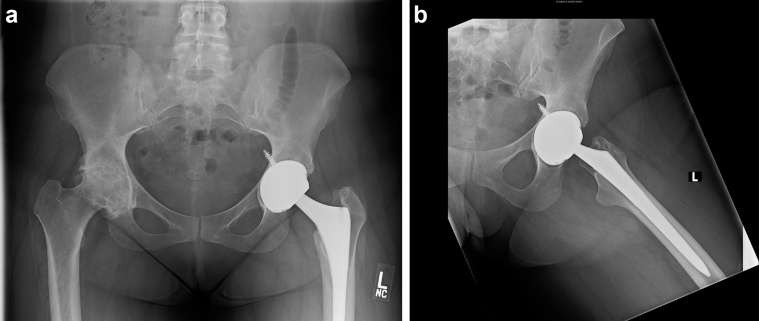
Radiographs of the left hip demonstrated THA with a hard-on-hard bearing surface combination. There was no radiographic evidence of catastrophic hardware failure. There was a complete radiolucent line surrounding the acetabular shell which was concerning for acetabular loosening. Acetabular inclination was 59°. The femoral stem appeared to be well fixed (Fig. 1). Laboratory analysis revealed a mild leukocytosis of 10.9 × 103 white blood cells/μL (normal: 4.6–10.2 × 103 white blood cells/μL). The erythrocyte sedimentation rate was within normal limits at 16 mm/h (normal: 0–20 mm/h), and the C-reactive protein was mildly elevated at 1.5 mg/dL (normal: <1.0 mg/dL). Serum cobalt and chromium levels were markedly elevated at 18.0 ppb and 13.4 ppb, respectively. Aspiration of the left hip joint was performed which revealed a white blood count of 1850 cells/mL with 87% segmented neutrophils on the differential. Bacterial cultures of the synovial fluid were negative for growth at 72 hours for aerobic, anaerobic, and acid-fast species.
Figure 1.
AP pelvis radiograph (a) and lateral view (b) of a 41-year-old woman with a hard-on-hard bearing surface combination demonstrating a complete radiolucent line surrounding the acetabular shell. The femoral stem appears to be well fixed.
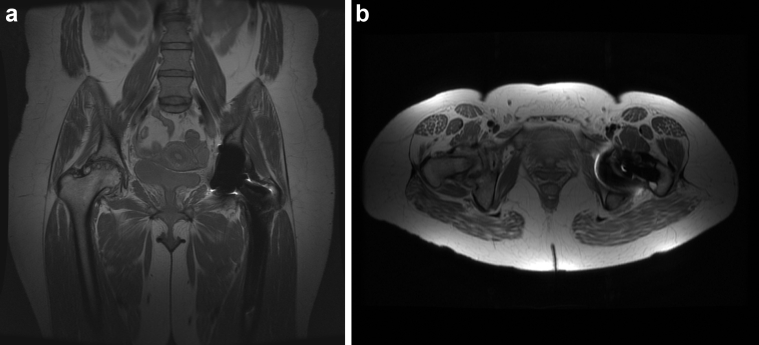
The patient subsequently underwent metal artifact reduction sequence (MARS) magnetic resonance imaging (MRI) of the left hip which demonstrated intact hip abductor tendons on the greater trochanter and no evidence of pseudotumor (Fig. 2).
Figure 2.
Coronal (a) and axial (b) MARS MRI demonstrating no evidence of pseudotumor or abductor insuffiency.
Revision left THA was performed. Intraoperatively, there was no apparent discoloration of the extracapsular soft tissues and no evidence of pseudotumor formation with the initial dissection. After hip joint capsulotomy, copious dark gray synovial fluid was encountered. Capsular tissue was sent for culture and histologic analysis.
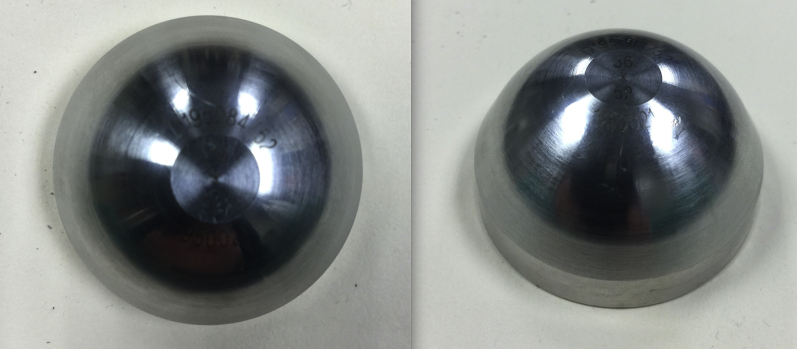
The femoral head was solidly engaged onto the femoral neck. After disimpaction, gross inspection of the explanted femoral head demonstrated evidence of metal transfer most pronounced on the posterior-superior aspect (Fig. 3). The femoral component appeared to be well fixed into the proximal femur on manual manipulation. Gross inspection of the trunnion demonstrated no evidence of fretting or discoloration. The acetabular liner demonstrated no evidence of edge loading, backside wear, fretting, or discoloration (Fig. 4), and it was noted to be appropriately engaged into the acetabular shell before explantation. The acetabular shell was found to be grossly loose on manual manipulation with a Kocher clamp, and it pivoted about a single well-fixed screw in the posterior-superior zone. The screw and acetabular shell (Fig. 5) were removed. The acetabular shell had minimal bony in-growth noted on inspection of the backside. No macroscopic evidence of fretting or discoloration was observed at the acetabular shell–screw interface.
Figure 3.
Photographs of explanted Biolox (CeramTech, Plochingen, Germany) Delta ceramic femoral head. There is evidence of metal transfer onto the ceramic femoral head.
Figure 4.
Photographs of explanted DePuy cobalt-chromium acetabular liner (Johnson and Johnson-DePuy Orthopaedics, Inc., Warsaw, IN).
Figure 5.
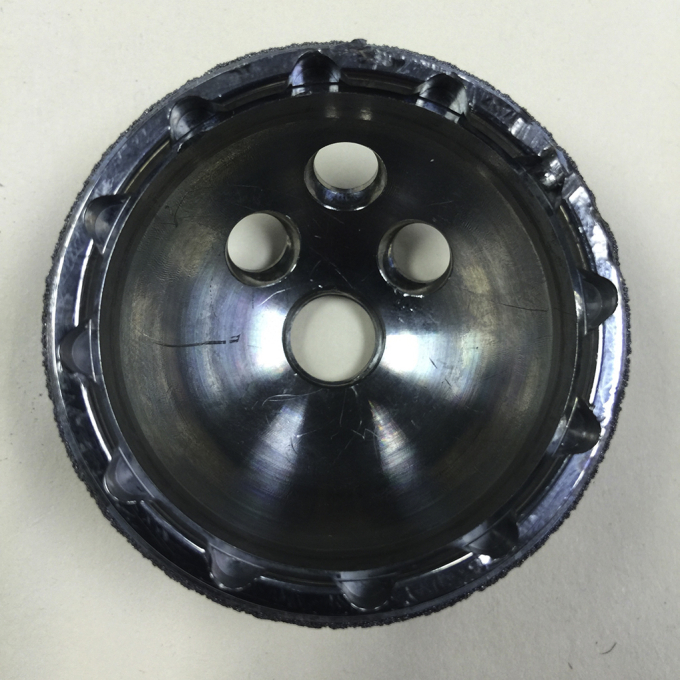
Photograph of explanted Pinnacle Gription titanium acetabular shell. (Johnson and Johnson-DePuy Orthopaedics, Inc., Warsaw, IN).
Inspection of the acetabulum after removal of the shell demonstrated intact bony columns with no evidence of significant bony loss. The acetabulum was reamed and a Pinnacle Gription titanium acetabular shell (54 mm) (Johnson and Johnson-DePuy Orthopaedics, Inc., Warsaw, IN) was impacted with good press fit. Two titanium screws were placed into the posterior-superior zone of the acetabulum for additional fixation. An Altrx Altralink polyethylene liner (neutral 36 mm) (Johnson and Johnson-DePuy Orthopaedics, Inc., Warsaw, IN, USA) was engaged into the acetabular shell. Finally, a Biolox Delta ceramic femoral head (36+8.5 mm) Biolox (CeramTech, Plochingen, Germany) with revision titanium sleeve designed to fit the 12/14 taper of the existing femoral trunion was impacted.
Intraoperative bacterial cultures were negative for aerobic, anaerobic, and acid-fast species at 72 hours. Histologic analysis of the synovial tissue of the left hip was notable for pigment-laden macrophages consistent with inclusion bodies (Fig. 6) and perivascular lymphocytic infiltrates (Fig. 7).
Figure 6.
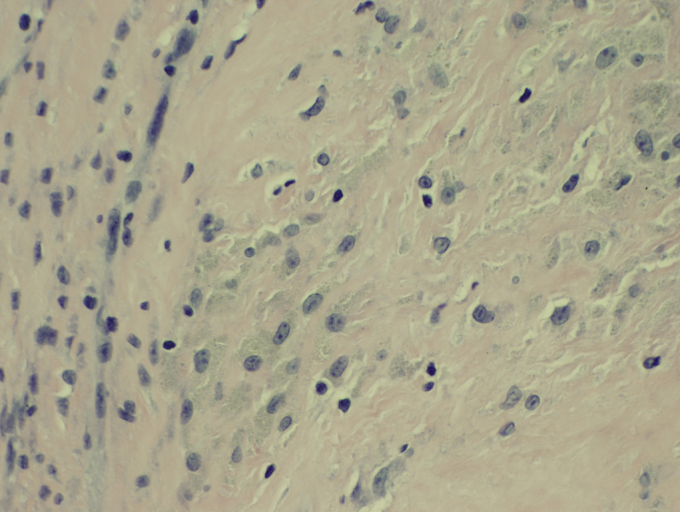
High-power histologic image of the left hip synovium. Chronic inflammation and pigment-laden macrophages are demonstrated.
Figure 7.
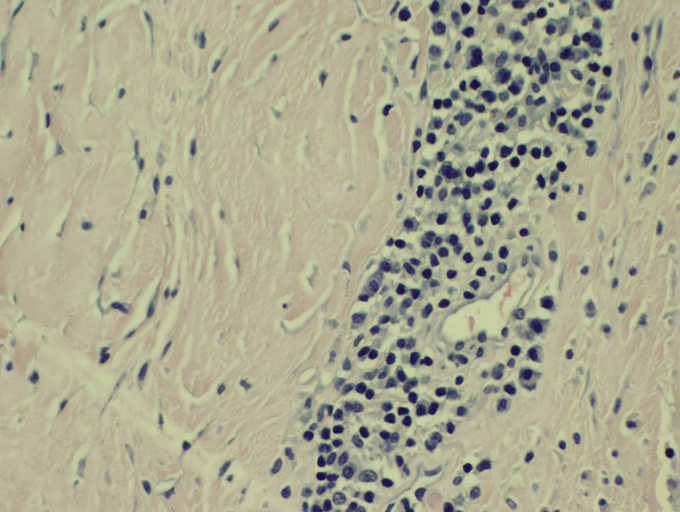
High-power histologic image of the left hip synovium. Perivascular lymphocytic infiltrates are demonstrated.
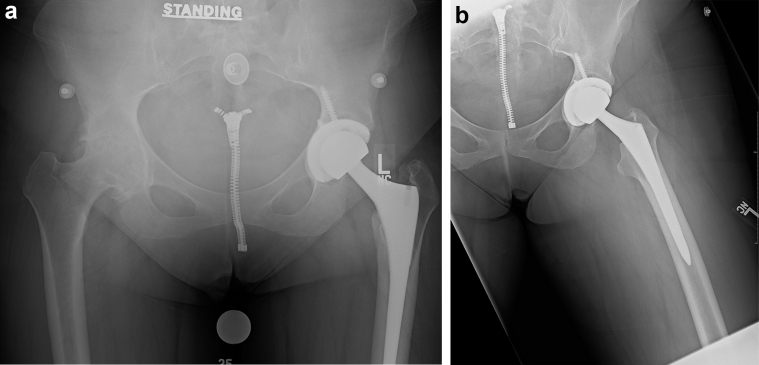
The acute postoperative course was uneventful, and the patient began working with a physical therapist on the day of surgery. At 6 weeks postoperatively, she was ambulating without any assistive devices. At the 12-week postoperative visit (Fig. 8), the patient had no pain in the left hip or groin and had returned to full-time employment. Because of her good outcome with revision left THA, she elected to undergo elective right THA at this time point as treatment for osteoarthritis which had not responded to nonoperative measures. At 9 months from revision left THA (and 6 months from primary right THA), the patient was pain free in the bilateral hips and groin and had again returned to full-time employment. She ambulated without a limp and was satisfied with her outcome. Repeat serum cobalt and chromium levels were 1.3 ppb and <1.0 ppb, respectively.
Figure 8.
AP pelvis radiograph (a) and lateral view (b) 12 weeks after revision of the left acetabular shell and exchange to a polyethylene acetabular liner and a ceramic femoral head.
Discussion
As the body of evidence for workup and management of a painful MoM THA continues to grow, clinical data to help guide decision making for patients with a painful THA and a metal and ceramic bearing surface combination are distinctively sparse [3]. Algorithms designed to help surgeons navigate clinical encounters with painful MoM hips may or may not be applicable to CoM and MoC hips 4, 5. Elevated serum metal ion levels after CoM THA has previously been reported and is associated with an increase in chromosomal breaks, aneuploidy in peripheral lymphocytes, and systemic symptoms including vision changes and hearing loss 12, 13, 16, 18.
The individual and synergistic contribution of component malposition, mechanically assisted crevice corrosion (MACC), and metal hypersensitivity observed with both MoC and CoM bearing combinations has yet to be defined [15]. Component malpositioning leading to failure of CoM THA was reported by Issac et al. who demonstrated that patients with significantly elevated (>10 μg/L) serum cobalt or chromium levels possessed a malpositioned acetabular component with inclination >50°, anteversion >25°, or both [12]. Subsequent studies by Schouten et al. [18] and Kazi et al. [13] however failed to demonstrate a statistical difference in serum cobalt and chromium levels in patients with increased acetabular inclination. Although the MoM hip literature has consistently reported that acetabular inclination >55 is associated with higher cobalt and chromium levels because of edge loading 19, 20, 21, it is currently unknown if the patient's acetabular inclination in this case was responsible for the need for revision. No evidence of edge loading was noted on gross inspection of the explanted acetabular shell.
MACC has been associated with failure of both MoP and hard-on-hard bearing surface combinations because of component modularity [15]. Modularity at both the head–neck and neck–body junctions has previously been associated with generation of metal ion debris secondary to fretting, destruction of the passivation layer, and ultimately increased corrosion 8, 15, 22, 23. The current patient underwent THA using a commercially available stem using head–neck modularity. Gross inspection of the trunnion of the femoral neck on explantation demonstrated no signs of fretting or discoloration typically described with MACC. It is unlikely that the use of modular components in the current case leads to failure of the patient's CoM THA.
Previous reports after failed MoM hip arthroplasties have described 3 distinct histologic responses to metal debris including a macrophage-dominated response, an aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL), or a mixed response containing elements of both a macrophage and lymphocytic-mediated process 24, 25. In a report of 29 patients with failed MoM hip arthroplasties (5 after THA and 24 after hip resurfacing), the mean time to revision surgery was 2.8 and 6.9 years for patients with histologic specimens consistent with ALVAL and a macrophage-dominated response, respectively. Intraoperative findings of metallosis, oil-colored synovial fluid, or thickened capsular tissue did not correlate with the final histologic diagnosis [24].
In our patient, the histologic presence of aggregates of perivascular lymphocytic infiltrates is consistent with at least some element of ALVAL; however, the presence of inclusion bodies in macrophages is suggestive of third-body wear. Thus, the histologic diagnosis is a mixed process. In the presence of a well-fixed screw and a loose acetabular shell, it is hypothesized that fretting between the acetabular shell–screw interface led to the formation of metal debris despite no macroscopic evidence on intraoperative inspection. It is currently unknown whether the single screw used during the index procedure provided sufficient stability to allow bony ingrowth to occur. To our knowledge, the titanium shell used at the index procedure has not been associated with a lack of bony in-growth. The debris generated from this articulation may have resulted in third-body wear and could be responsible for the metal transfer observed on the femoral head at the time of explantation and the macrophage inclusion bodies noted on histology. This could also explain the elevated serum cobalt and chromium levels reported in this patient preoperatively. Although previous literature has associated failure of hard-on-hard bearing surfaces to component malposition [21] and MACC [15], we believe that third-body wear must be considered in the management of a patient with a painful CoM THA.
To our knowledge, there are no previously reported cases of adverse reaction to metal debris after CoM THA. Our patient presented with severe groin pain, serum cobalt and chromium levels >10 μg/L, and acetabular shell loosening. At this point, prevalence of elevated metal ion levels after CoM THA is not well described and its usefulness for predicting the need for revision surgery is unknown. A larger evaluation of this patient population is needed to help guide clinical decision making for the patient presenting to clinic with a painful CoM THA.
Summary
We report the case of a 41-year-old woman who presented 8 years after CoM THA with groin pain and decreased level of function. Infection workup was negative, and cobalt and chromium levels were markedly elevated. At revision surgery, the acetabular shell was grossly loose and pivoted about a well-fixed screw. Revision THA was performed with implantation of a new acetabular shell and exchange to a CoP bearing surface. Clinical outcome was successful and laboratories normalized by 9 months postoperatively. To our knowledge, there has been no previous report of adverse reaction to metal debris in a CoM THA.
Footnotes
One or more of the authors of this article have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2015.07.002.
Appendix. Supplementary data
References
- 1.Kurtz S.M., Lau E., Ong K. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babovic N., Trousdale R.T. Total hip arthroplasty using highly cross-linked polyethylene in patients younger than 50 years with minimum 10-year follow-up. J Arthroplasty. 2013;28(5):815. doi: 10.1016/j.arth.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Greenwald A.S., Garino J.P., American Academy of Orthopaedic Surgeons. Committee on Biomedical Engineering, American Academy of Orthopaedic Surgeons. Committee on Hip and Knee Arthritis Alternative bearing surfaces: the good, the bad, and the ugly. J Bone Joint Surg Am. 2001;83-A(Suppl 2 Pt 2):68. doi: 10.2106/00004623-200100022-00002. [DOI] [PubMed] [Google Scholar]
- 4.Kwon Y.M., Jacobs J.J., MacDonald S.J. Evidence-based understanding of management perils for metal-on-metal hip arthroplasty patients. J Arthroplasty. 2012;27(8 Suppl):20. doi: 10.1016/j.arth.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 5.Lombardi A.V., Jr., Barrack R.L., Berend K.R. The Hip Society: algorithmic approach to diagnosis and management of metal-on-metal arthroplasty. J Bone Joint Surg Br. 2012;94(11 Suppl A):14. doi: 10.1302/0301-620X.94B11.30680. [DOI] [PubMed] [Google Scholar]
- 6.Ha Y.C., Koo K.H., Jeong S.T. Cementless alumina-on-alumina total hip arthroplasty in patients younger than 50 years: a 5-year minimum follow-up study. J Arthroplasty. 2007;22(2):184. doi: 10.1016/j.arth.2006.02.169. [DOI] [PubMed] [Google Scholar]
- 7.Park K.S., Seon J.K., Yoon T.R. The survival analysis in third-generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2015 doi: 10.1016/j.arth.2015.05.017. http://dx.doi.org/10.1016/j.arth.2015.05.017 [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Jacobs J.J., Skipor A.K., Patterson L.M. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80(10):1447. doi: 10.2106/00004623-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Firkins P.J., Tipper J.L., Ingham E. A novel low wearing differential hardness, ceramic-on-metal hip joint prosthesis. J Biomech. 2001;34(10):1291. doi: 10.1016/s0021-9290(01)00096-3. [DOI] [PubMed] [Google Scholar]
- 10.Ishida T., Clarke I.C., Donaldson T.K. Comparing ceramic-metal to metal-metal total hip replacements—a simulator study of metal wear and ion release in 32- and 38-mm bearings. J Biomed Mater Res B Appl Biomater. 2009;91(2):887. doi: 10.1002/jbm.b.31471. [DOI] [PubMed] [Google Scholar]
- 11.Williams S., Schepers A., Isaac G. The 2007 Otto Aufranc Award. Ceramic-on-metal hip arthroplasties: a comparative in vitro and in vivo study. Clin Orthop Relat Res. 2007;465:23. doi: 10.1097/BLO.0b013e31814da946. [DOI] [PubMed] [Google Scholar]
- 12.Isaac G.H., Brockett C., Breckon A. Ceramic-on-metal bearings in total hip replacement: whole blood metal ion levels and analysis of retrieved components. J Bone Joint Surg Br. 2009;91(9):1134. doi: 10.1302/0301-620X.91B9.22306. [DOI] [PubMed] [Google Scholar]
- 13.Kazi H.A., Perera J.R., Gillott E., Carroll F.A., Briggs T.W. A prospective study of a ceramic-on-metal bearing in total hip arthroplasty. Clinical results, metal ion levels and chromosome analysis at two years. Bone Joint J. 2013;95-B(8):1040. doi: 10.1302/0301-620X.95B8.31574. [DOI] [PubMed] [Google Scholar]
- 14.Cigada A., Cotogno G., Chiesa R. The ceramic-on-metal coupling in total hip replacements for young patients: a review study. J Appl Biomater Biomech. 2011;9(1):2. doi: 10.5301/JABB.2011.7730. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs J.J., Cooper H.J., Urban R.M., Wixson R.L., Della Valle C.J. What do we know about taper corrosion in total hip arthroplasty? J Arthroplasty. 2014;29(4):668. doi: 10.1016/j.arth.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Steens W., von Foerster G., Katzer A. Severe cobalt poisoning with loss of sight after ceramic-metal pairing in a hip—a case report. Acta Orthop. 2006;77(5):830. doi: 10.1080/17453670610013079. [DOI] [PubMed] [Google Scholar]
- 17.Valenti J.R., Del Rio J., Amillo S. Catastrophic wear in a metal-on-ceramic total hip arthroplasty. J Arthroplasty. 2007;22(6):920. doi: 10.1016/j.arth.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Schouten R., Malone A.A., Tiffen C., Frampton C.M., Hooper G. A prospective, randomised controlled trial comparing ceramic-on-metal and metal-on-metal bearing surfaces in total hip replacement. J Bone Joint Surg Br. 2012;94(11):1462. doi: 10.1302/0301-620X.94B11.29343. [DOI] [PubMed] [Google Scholar]
- 19.De Haan R., Pattyn C., Gill H.S. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90(10):1291. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]
- 20.Fox C.M., Bergin K.M., Kelly G.E. MRI findings following metal on metal hip arthroplasty and their relationship with metal ion levels and acetabular inclination angles. J Arthroplasty. 2014;29(8):1647. doi: 10.1016/j.arth.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 21.Nicolli A., Bisinella G., Padovani G. Predictivity and fate of metal ion release from metal-on-metal total hip prostheses. J Arthroplasty. 2014;29(9):1763. doi: 10.1016/j.arth.2014.04.041. [DOI] [PubMed] [Google Scholar]
- 22.Cooper H.J., Della Valle C.J., Berger R.A. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94(18):1655. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgs G.B., Hanzlik J.A., MacDonald D.W., Implant Research Center Writing Committee Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices?: a retrieval study. J Arthroplasty. 2013;28(8 Suppl):2. doi: 10.1016/j.arth.2013.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berstock J.R., Baker R.P., Bannister G.C., Case C.P. Histology of failed metal-on-metal hip arthroplasty; three distinct sub-types. Hip Int. 2014;24(3):243. doi: 10.5301/hipint.5000117. [DOI] [PubMed] [Google Scholar]
- 25.Willert H.G., Buchhorn G.H., Fayyazi A. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.