Abstract
Delafloxacin is a broad-spectrum anionic fluoroquinolone under development for the treatment of bacterial pneumonia. The goal of the study was to determine the pharmacokinetic/pharmacodynamic (PK/PD) targets in the murine lung infection model for Staphylococcus aureus, Streptococcus pneumoniae, and Klebsiella pneumoniae. Four isolates of each species were utilized for in vivo studies: for S. aureus, one methicillin-susceptible and three methicillin-resistant isolates; S. pneumoniae, two penicillin-susceptible and two penicillin-resistant isolates; K. pneumoniae, one wild-type and three extended-spectrum beta-lactamase-producing isolates. MICs were determined using CLSI methods. A neutropenic murine lung infection model was utilized for all treatment studies, and drug dosing was by the subcutaneous route. Single-dose plasma pharmacokinetics was determined in the mouse model after administration of 2.5, 10, 40, and 160 mg/kg. For in vivo studies, 4-fold-increasing doses of delafloxacin (range, 0.03 to 160 mg/kg) were administered every 6 h (q6h) to infected mice. Treatment outcome was measured by determining organism burden in the lung (CFU counts) at the end of each experiment (24 h). The Hill equation for maximum effect (Emax) was used to model the dose-response data. The magnitude of the PK/PD index, the area under the concentration-time curve over 24 h in the steady state divided by the MIC (AUC/MIC), associated with net stasis and 1-log kill endpoints was determined in the lung model for all isolates. MICs ranged from 0.004 to 1 mg/liter. Single-dose PK parameter ranges include the following: for maximum concentration of drug in serum (Cmax), 2 to 70.7 mg/liter; AUC from 0 h to infinity (AUC0–∞), 2.8 to 152 mg · h/liter; half-life (t1/2), 0.7 to 1 h. At the start of therapy mice had 6.3 ± 0.09 log10 CFU/lung. In control mice the organism burden increased 2.1 ± 0.44 log10 CFU/lung over the study period. There was a relatively steep dose-response relationship observed with escalating doses of delafloxacin. Maximal organism reductions ranged from 2 log10 to more than 4 log10. The median free-drug AUC/MIC magnitude associated with net stasis for each species group was 1.45, 0.56, and 40.3 for S. aureus, S. pneumoniae, and K. pneumoniae, respectively. AUC/MIC targets for the 1-log kill endpoint were 2- to 5-fold higher. Delafloxacin demonstrated in vitro and in vivo potency against a diverse group of pathogens, including those with phenotypic drug resistance to other classes. These results have potential relevance for clinical dose selection and evaluation of susceptibility breakpoints for delafloxacin for the treatment of lower respiratory tract infections involving these pathogens.
INTRODUCTION
Delafloxacin (RX-3341, ABT-492, and WQ-3034) is a novel fluoroquinolone antibiotic in development for the treatment of respiratory tract infections. Oral (p.o.) and intravenous (i.v.) formulations have been developed with promising pharmacokinetic (PK) and efficacy results (1, 2). Delafloxacin has a broad spectrum of activity that includes drug-resistant Staphylococcus aureus, Streptococcus pneumoniae, and Klebsiella pneumoniae (3–7). Previous clinical studies in patients with acute bacterial skin and skin structure infections (ABSSIs) have demonstrated potency and efficacy, especially with respect to S. aureus (8, 9).
Pneumonia is one of the most common infectious diseases encountered worldwide and remains a significant cause of morbidity and mortality (10). The major pathogen of community-acquired pneumonia (CAP) continues to be S. pneumoniae despite major advances in vaccination development and administration to at-risk populations. In the hospital setting, S. aureus and Gram-negative bacteria are more commonly encountered and are frequently drug resistant (11).
Staphylococcus aureus is particularly challenging due to its inherent pathogenicity and increased prevalence of drug-resistant phenotypes (i.e., methicillin-resistant S. aureus [MRSA]) contributing to serious infections. It is the leading bacterial cause of life-threatening infection due to these attributes (12–14). For example, in the United States, S. aureus is the most common cause of nosocomial infection and leads to more than 80,000 illnesses and 11,000 deaths yearly (12). Unfortunately, there is a paucity of novel agents to treat MRSA pulmonary infections and even fewer that have oral and i.v. formulation options.
The objectives of our experiments were to characterize the in vivo efficacy of delafloxacin using a neutropenic murine lung infection model for three common respiratory tract pathogen groups, including S. aureus, S. pneumoniae, and K. pneumoniae. Specifically, the pharmacokinetic/pharmacodynamic (PK/PD) targets of delafloxacin were examined to provide a framework for further development of drug-dosing regimens to optimize delafloxacin therapy for respiratory infections. The integration of these targets and pharmacokinetics from human studies will also be useful in setting preliminary susceptibility breakpoints for delafloxacin.
MATERIALS AND METHODS
Organisms, media, and antibiotic.
Four S. aureus (one methicillin-susceptible [MSSA] and three methicillin-resistant), four S. pneumoniae (one penicillin-susceptible and three penicillin-resistant), and four K. pneumoniae (one wild-type and three extended-spectrum beta-lactamase-positive [ESBL]) strains were used for these studies (Table 1). S. aureus and K. pneumoniae organisms were grown, subcultured, and quantified using Mueller-Hinton broth (MHB) and agar (Difco Laboratories, Detroit, MI). S. pneumoniae isolates were grown, subcultured, and quantified using sheep blood agar (Remel, Milwaukee, WI). Delafloxacin for in vitro and in vivo studies was supplied by the study sponsor (Melinta Therapeutics, Inc., Lincolnshire, IL). Compound was prepared by reconstitution and subsequent dilution in sterile water.
TABLE 1.
In vitro activity of delafloxacin and levofloxacin against study organisms
| Organism | Descriptiona | Delafloxacin MIC (mg/liter) | Levofloxacin MIC (mg/liter) |
|---|---|---|---|
| S. aureus strains | |||
| ATCC 29213 | MSSA | 0.008 | 0.25 |
| ATCC 33591 | MRSA (USA200) | 0.008 | 0.25 |
| MW2 | MRSA (USA400) | 0.004 | 0.25 |
| R2527 | MRSA (USA300) | 0.004 | 0.125 |
| S. pneumoniae strains | |||
| ATCC 10813 | Pens | 0.03 | 1 |
| ATCC 49619 | Penr | 0.125 | 1 |
| 145 | Penr | 0.016 | 0.5 |
| 1329 | Penr | 0.016 | 0.5 |
| K. pneumoniae strains | |||
| ATCC 43816 | Wild type | 0.06 | 0.06 |
| 4105 | TEM-26, SHV-4 | 1 | 1 |
| 4110 | TEM-11, SHV-1 | 0.5 | 1 |
| 81-1260A | CTX-M, AmpC | 0.06 | 0.06 |
Pen, penicillin.
In vitro susceptibility testing.
The MICs of each compound for the various isolates were determined using Clinical and Laboratory Standards Institute (CLSI) microdilution methods (15). All MIC assays were performed in duplicate on three separate occasions. The median MIC of replicate assays is reported and utilized in PK/PD analyses.
Drug pharmacokinetics.
Single-dose plasma pharmacokinetics of delafloxacin were performed in neutropenic mice. Animals were administered single subcutaneous doses (0.2 ml/dose) of delafloxacin at dose levels of 2.5, 10, 40, and 160 mg/kg. Groups of three mice were sampled at each time point (seven time points, consisting of 1, 2, 4, 6, 8, 12, and 24 h) and dose level.
Plasma concentrations were determined using liquid chromatography-tandem mass spectrometry (LC-MS/MS) by the sponsor. Briefly, a stock calibration standard of delafloxacin meglumine salt (RX-3341-83-008) was prepared in dimethyl sulfoxide (DMSO) at a concentration of 1,000 μg/ml (corrected for salt form) to prepare working calibration standards and quality controls (QCs). Working calibration standards were prepared by serial dilution of working stock solution with methanol-water (50:50, vol/vol) over a range of 100 ng/ml to 500,000 ng/ml. Working QCs were prepared in methanol-water (50:50, vol/vol) at three concentration levels: high (300,000 ng/ml), middle (15,000 ng/ml), and low (300 ng/ml). Twenty microliters of each working QC was added to 180 μl of blank mouse plasma, vortex mixed, and run in duplicate. Standards in matrix were prepared with 5 μl of working calibration standard added to 45 μl of control blank mouse plasma in a 96-well collection plate. Fifty microliters of unknown mouse plasma or QC was added to the plate. For blanks and blanks with an internal standard, 50 μl of control blank mouse plasma was added. Twenty microliters of working internal standard (WIS) (1,000 ng/ml RX-4039, a closely related analog, in methanol-water [50:50, vol/vol]) was added to standards, unknowns, and control blanks. Twenty microliters of methanol-water was added to blanks without WIS. Samples were extracted by adding 300 μl of acetonitrile (ACN) to all samples in a 96-well collection plate and vortex mixed for 4 min. Samples were centrifuged for 10 min at 3,200 × g at 4°C. Fifty microliters of supernatant was transferred to 450 μl of ACN-water (50:50, vol/vol) in a 96-well autosampler plate and mixed with a multichannel pipette. Samples were analyzed for delafloxacin using LC-MS/MS. The assay lower limit of quantification was 10 ng/ml. The assay coefficient of variation was less than 10%.
Pharmacokinetic parameters (means ± standard deviations), including elimination half-life (t1/2), area under the concentration-time curve from 0 h to infinity (AUC0–∞), and maximum concentration in serum (Cmax), were calculated using a noncompartmental model. The half-life was determined by linear least-squares regression. The AUC was calculated from the mean concentrations using the trapezoidal rule. Pharmacokinetic estimates for dose levels that were not directly measured were calculated using linear interpolation for dose levels between those with measured kinetics (e.g., between 40 and 160 mg/kg) and linear extrapolation for dose levels above or below the highest and lowest dose levels with kinetic measurements. Murine protein binding of 97.6% (Melinta Therapeutics, Inc.; data on file) was used to determine free-drug concentrations.
Murine lung infection model.
Animals were maintained in accordance with the American Association for Accreditation of Laboratory Animal Care (AAALAC) criteria (16). All animal studies were approved by the Animal Research Committees of the William S. Middleton Memorial VA Hospital and the University of Wisconsin. Six-week-old, specific-pathogen-free, female ICR/Swiss mice weighing 24 to 27 g were used for all studies (Harlan Sprague-Dawley, Indianapolis, IN). Mice were rendered neutropenic (neutrophils of <100/mm3) by injecting cyclophosphamide (Mead Johnson Pharmaceuticals, Evansville, IN) intraperitoneally 4 days (150 mg/kg) and 1 day (100 mg/kg) before lung infection. Broth cultures of freshly plated S. aureus and K. pneumoniae were grown to logarithmic phase overnight to an absorbance of 0.3 at 580 nm using a Spectronic 88 spectrophotometer (Bausch and Lomb, Rochester, NY). S. pneumoniae isolates were grown overnight on sheep blood agar. A sterile loop was then used to transfer organisms to sterile saline, and absorbance was adjusted as described above. After a 1:10 dilution, bacterial counts of the inoculum ranged from 108.1 to 108.2 CFU/ml, 108.1 to 108.4 CFU/ml, and 108.0 to 108.3 CFU/ml for S. aureus, S. pneumoniae, and K. pneumoniae, respectively. Lung infections with each of the strains were produced by administration of 50 μl of inoculum into the nares of isoflurane-anesthetized mice. Mice were then held upright to allow for aspiration into the lungs. Therapy with delafloxacin was initiated 2 h after induction of infection.
Pharmacodynamic target associated with treatment efficacy.
In vivo treatment studies were performed in the murine lung model for each isolate. Seven (S. aureus and S. pneumoniae) and five (K. pneumoniae) 4-fold-increasing dosing regimens of delafloxacin were administered to groups of three neutropenic infected mice per dose level. The total daily doses of delafloxacin varied from 0.156 to 640 mg/kg/24 h. Zero-hour and untreated control animals were included for each strain. Drug was fractionated for an administration schedule of every 6 h and given by the subcutaneous route. Therapy was initiated 2 h after infection. Animals were euthanized at 24 h after infection, and the lungs were aseptically removed for CFU count determination.
The correlation between efficacy and the PK/PD parameter calculated as the ratio of the AUC over 24 h in the steady state to the MIC (AUC/MIC) was determined by nonlinear least-squares multivariate regression (SigmaPlot, version 12.3; Systat Software, San Jose, CA). The AUC/MIC was chosen as the predictive pharmacodynamic as previous studies have demonstrated this index to be predictive for fluoroquinolones (17–24). The mathematical model used was derived from the Hill equation: E = (Emax × DN)/(ED50N − DN), where E is the effector, in this case, the log change in CFU per lung between treated mice and untreated controls after the 24-h period of study, Emax is the maximum effect, D is the 24-h total dose, ED50 is the dose required to achieve 50% of the Emax, and N is the slope of the dose-effect curve. The values for the indices Emax, ED50, and N were calculated using nonlinear least-squares regression. The coefficient of determination (R2) was used to estimate the variance that might be due to regression with the PK/PD parameter AUC/MIC. The doses required to produce a net static effect (static dose) and a 1-log10 kill (1-log-kill dose) compared to the start of therapy were calculated for each drug-organism combination. The associated 24-h total- and free-drug AUC/MIC targets were calculated.
RESULTS
In vitro susceptibility testing.
The median MICs of delafloxacin for the strains used in the studies are shown in Table 1. Numerically, the lowest MICs were observed for S. aureus (range, 0.004 to 0.008 mg/liter). Methicillin resistance did not impact the in vitro potency of delafloxacin in this select group of organisms. The in vitro potency against S. pneumoniae and K. pneumoniae strains was more varied (range, 0.016 to 0.125 mg/liter and 0.06 to 1 mg/liter, respectively). An elevated levofloxacin MIC did correlate with an increased delafloxacin MIC for the latter two organism groups.
Drug pharmacokinetics.
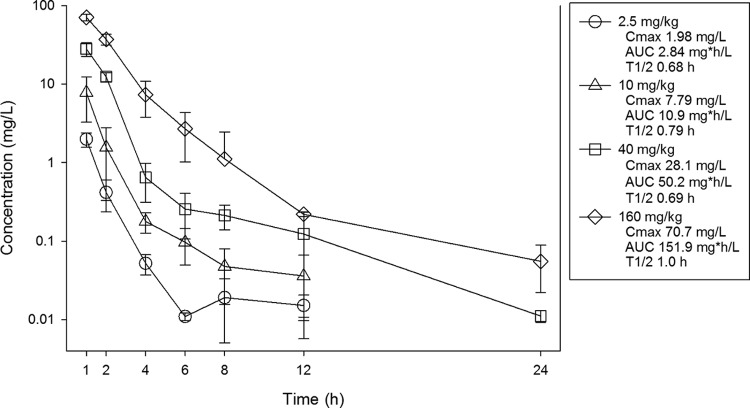
Single-dose pharmacokinetics of delafloxacin are shown in Fig. 1. At the doses studied, exposure to delafloxacin increased in a dose-dependent manner across the dose range. Cmax concentrations ranged from 2 to 71 mg/liter. AUC0–∞ values ranged from 2.8 to 152 mg · h/liter and were linear across the 2.5- to 160-mg dosing range (R2 of 0.99). The elimination half-life ranged from 0.7 to 1 h.
FIG 1.
Single-dose plasma pharmacokinetics of delafloxacin in neutropenic mice. Four doses of delafloxacin that varied by 4-fold concentrations on a milligram/kilogram basis were administered by the subcutaneous route. Groups of three mice were sampled for each time point. Samples were collected every 1 to 24 h over a 24-h period. Each symbol represents the mean value from three animals. The error bars represent the standard deviations. Pharmacokinetic parameters listed in the box include maximum drug concentrations (Cmax), the AUC from 0 h to infinity (AUC), and the elimination half-life (t1/2) for each dose.
Pharmacodynamic target associated with treatment efficacy.
The bacterial burden at the start of therapy and growth in untreated controls are shown in Table 2. Growth increased from 1.5 to 3.3 log10 CFU in the lungs of untreated animals over a 24-h period. The dose-response curves for delafloxacin against each organism group based on the organism burden at the start of therapy (zero hour) is shown in Fig. 2A to C. Delafloxacin was highly effective against S. aureus (Fig. 2A). Against all four strains we observed a decrease of 1.5 to 2.2 log10 CFU in organism burden from untreated controls at even the lowest dose studied, and for two strains (MW2 and R2527) there was net bactericidal activity at the lowest dose. At the maximal doses studied, there was a >4-log10 kill from initial burden for all S. aureus strains.
TABLE 2.
In vivo activity and PK/PD analysis of delafloxacin against study organisms
| Organism | Bacterial burden at start of therapy (log10 CFU/lung) | Growth in controls at 24 h (Δlog10 CFU/lung) | Stasis |
1-log kill |
||||
|---|---|---|---|---|---|---|---|---|
| Dose (mg/kg/24 h) | 24-h AUC/MIC |
Dose (mg/kg/24 h) | 24-h AUC/MIC |
|||||
| Total drug | Free drug | Total drug | Free drug | |||||
| S. aureus strains | ||||||||
| 29213 | 6.35 | 1.99 | 0.93 | 130 | 3.12 | 3.22 | 451 | 10.8 |
| 33591 | 6.26 | 2.06 | 0.53 | 74.6 | 1.79 | 2.25 | 315 | 7.57 |
| MW2 | 6.33 | 1.53 | <0.16a | <43.8a | <1.05a | 0.98 | 276 | 6.61 |
| R2527 | 6.29 | 1.47 | <0.16a | <43.8a | <1.05a | 1.23 | 345 | 8.28 |
| Median | 0.34 | 59.2 | 1.42 | 1.74 | 330 | 7.92 | ||
| S. pneumoniae strains | ||||||||
| 10813 | 6.53 | 2.23 | 0.93 | 34.8 | 0.84 | 3.83 | 143 | 3.43 |
| 49619 | 6.48 | 1.8 | 1.36 | 12.2 | 0.29 | 15.5 | 137 | 3.29 |
| 145 | 6.27 | 2.07 | <0.16a | <10.9a | <0.26a | 0.23 | 16.5 | 0.39 |
| 1329 | 6.22 | 1.5 | 1.36 | 95.1 | 2.28 | 6.11 | 428 | 10.3 |
| Median | 1.14 | 23.5 | 0.56 | 4.97 | 140 | 3.36 | ||
| K. pneumoniae strains | ||||||||
| 43816 | 6.30 | 2.86 | 304 | 5287 | 127 | |||
| 4105 | 6.30 | 3.33 | 106 | 128 | 3.08 | 196 | 228 | 5.47 |
| 4110 | 6.32 | 2.82 | NAb | NA | NA | NA | NA | NA |
| 81-1260A | 6.28 | 2.83 | 84.8 | 1681 | 40.3 | 238 | 4369 | 105 |
| Median | 106 | 1681 | 40.3 | 217 | 2298 | 55.2 | ||
Dose and drug exposure (AUC/MIC) were set to the lowest values studied for organisms in which only bactericidal activity was observed.
NA, endpoint not achieved.
FIG 2.
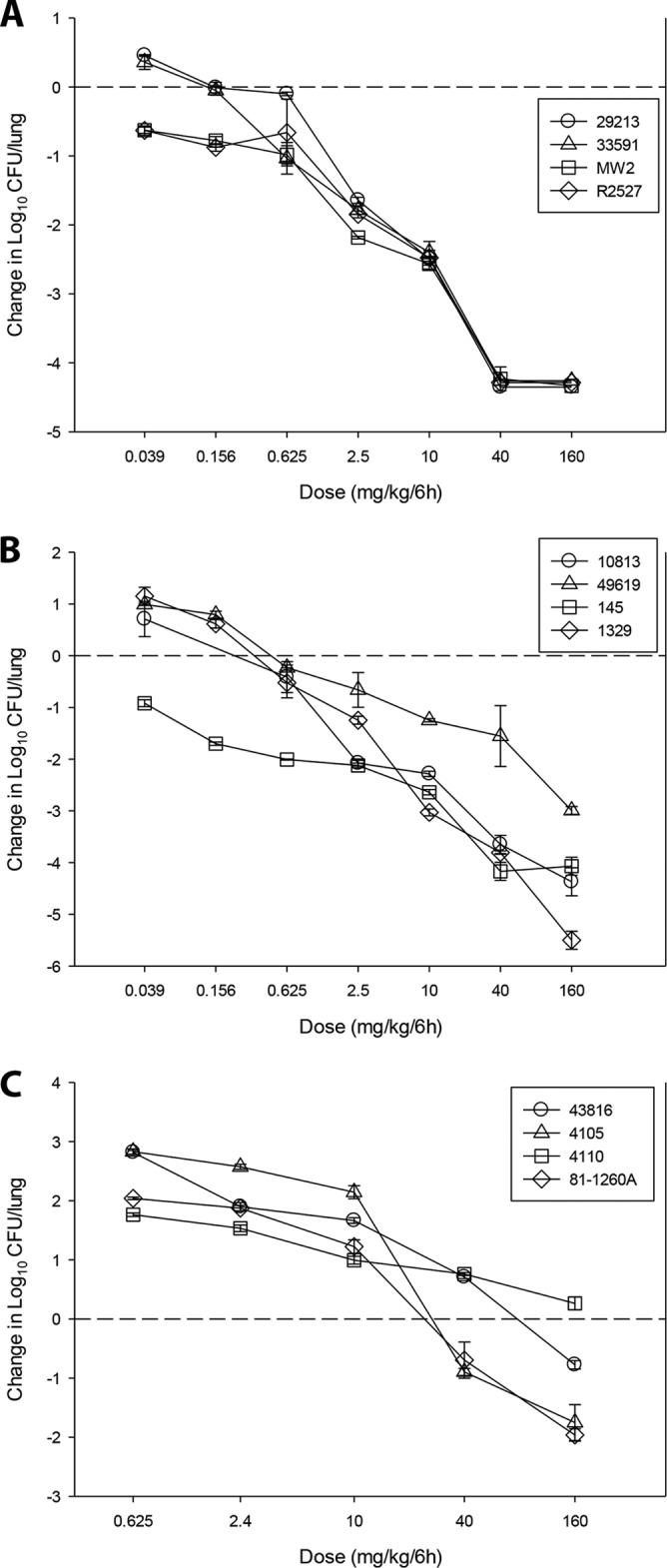
In vivo dose-response curves for delafloxacin against four S. aureus (A), four S. pneumoniae (B), and four K. pneumoniae (C) strains using a neutropenic murine lung infection model. Each symbol represents the mean and standard deviation from three mice. Four-fold-increasing dose levels were fractionated for a regimen of dosing every 6 h. The burden of organisms was measured at the start and end of therapy. The study period was 24 h. The horizontal dashed line at 0 represents the burden of organisms in the lungs of mice at the start of therapy. Data points below the line represent killing, and points above the line represent growth.
Likewise, delafloxacin was very potent against S. pneumoniae (Fig. 2B). The lowest dose for this group resulted in a decline of 1.2 to 3.0 log10 CFU compared to levels in untreated controls. Once again, we observed net bactericidal activity at the lowest dose studied for one of the strains (S. pneumoniae 145). The maximal effect from the start of therapy for this group was also a >4-log10 kill for three of four strains, the exception being 49619, for which the delafloxacin MIC was significantly higher than that for the other three isolates.
The dose-response effects against K. pneumoniae (Fig. 2C) strains were in keeping with the group's increased MICs relative to those of the other organism groups. Maximal effect varied from near stasis to almost a 2-log10 kill compared to the initial burden.
The dose-response data for each organism group was modeled to examine the impact of the PK/PD index AUC/MIC on treatment effect, and results are shown in Fig. 3A to C. The AUC/MIC was a strong predictor of treatment outcome based on regression analysis for S. aureus and S. pneumoniae (R2 values of 0.89 and 0.70, respectively). The data fit for K. pneumoniae was less strong (R2 of 0.49). Total daily doses necessary to achieve net stasis and a 1-log kill for strains that achieved these endpoints are shown in Table 2. The median static dose was 0.34 mg/kg/24 h for S. aureus, 1.14 mg/kg/24 h for S. pneumoniae, and 84.8 mg/kg/24 h for K. pneumoniae. The 1-log-kill dose was similarly lowest for S. aureus at 1.74 mg/kg/24 h, followed by 4.97 mg/kg/24 h for S. pneumoniae, and 217 mg/kg/24 h for K. pneumoniae. The associated total- and free-drug AUC/MIC values for the static dose and 1-log-kill dose are also shown in Table 2. The median free-drug 24-h AUC/MIC targets for stasis were 1.42, 0.56, and 40.3 for S. aureus, S. pneumoniae, and K. pneumoniae, respectively. The free-drug 24-h AUC/MIC targets for a 1-log kill were 7.92, 3.36, and 55.2 for S. aureus, S. pneumoniae, and K. pneumoniae, respectively.
FIG 3.
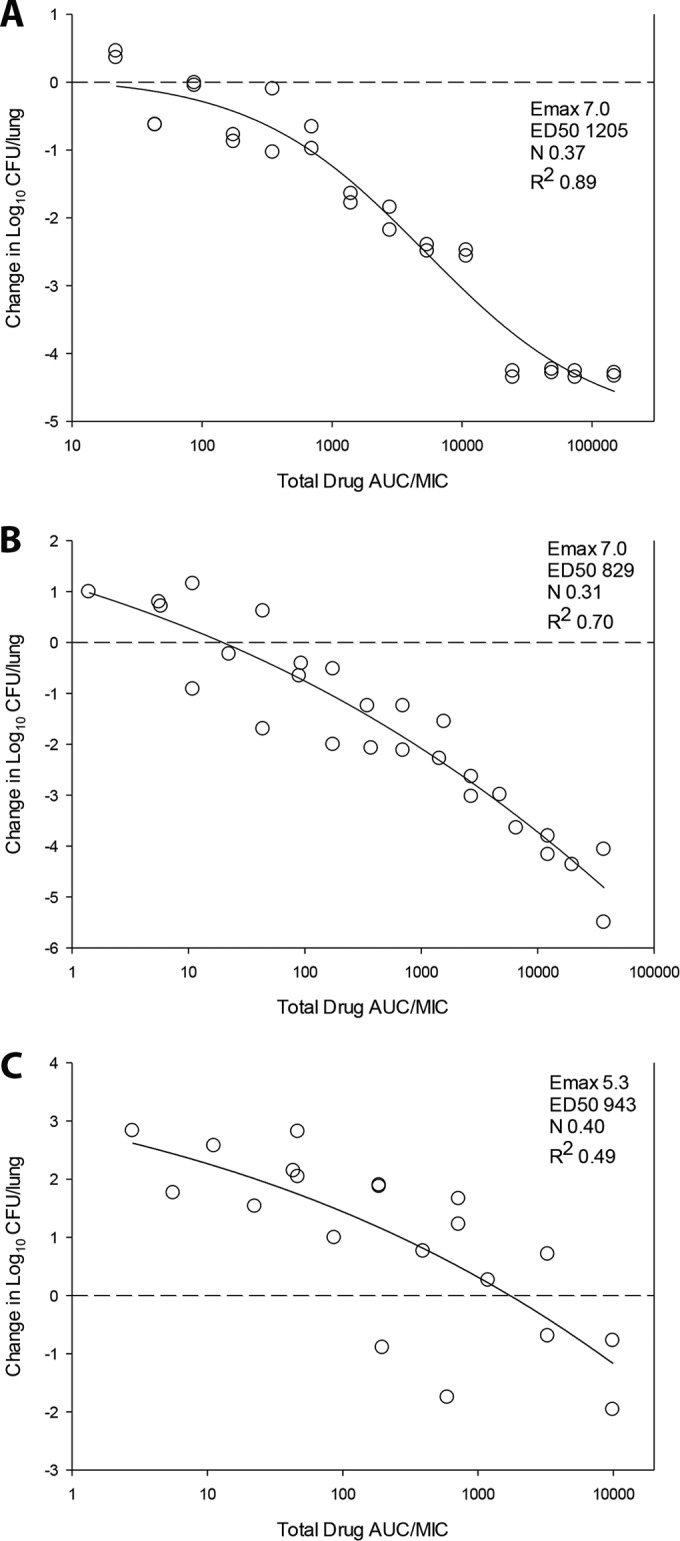
Relationship between the PK/PD index total-drug AUC/MIC ratio and treatment efficacy of delafloxacin against four S. aureus (A), four S. pneumoniae (B), and four K. pneumoniae (C) strains using a neutropenic murine lung infection model. Each symbol represents the mean from three mice. Four-fold-increasing dose levels were fractionated for a regimen of dosing every 6 h. The study period was 24 h. The delafloxacin exposure is expressed as the total-drug 24-h AUC/MIC. The burden of organisms was measured at the start and end of therapy. The horizontal line at 0 represents the burden of organisms in the lungs of mice at the start of therapy. Data points below the line represent killing, and points above the line represent growth. The R2 value represents the coefficient of determination. The ED50 represents the AUC/MIC associated with 50% of the maximal effect (Emax), and N is the slope of the relationship, or the Hill coefficient. The line drawn through the data points is the best-fit line based upon the sigmoid Emax formula.
DISCUSSION
Our studies demonstrated delafloxacin to be highly active against S. aureus, including against isolates with methicillin resistance. This potent activity has been observed in previous in vitro studies (3–6). Additionally, we observed in vitro potency against beta-lactam-susceptible and -resistant S. pneumoniae and K. pneumoniae strains comparable to that of previous reports (3–7, 25). Similar to findings of earlier studies, elevated MICs of other fluoroquinolones correlated with an increased delafloxacin MIC for wild-type strains although the delafloxacin MICs for these less susceptible strains remained relatively low (≤1 mg/liter).
In vivo pharmacodynamic evaluation of antimicrobial activity requires the integration of the aforementioned in vitro potency (MIC), drug pharmacokinetics, and antimicrobial activity over time (21). Previous studies with fluoroquinolones have consistently shown concentration-dependent activity with prolonged postantibiotic effects (17–24). The PK/PD index associated with the efficacy of antibiotics characterized by this pattern of activity is the AUC/MIC. The present study demonstrated a strong correlation with this PK/PD index and the outcome in each bacterial species.
The pharmacodynamic target associated with net stasis in previous fluoroquinolone studies has been a 24-h free-drug AUC/MIC of 25 to 50 for S. pneumoniae and values 2- to 4-fold higher (≥100) for S. aureus and Gram-negative pathogens (17, 18, 20, 21, 24). In the present study with delafloxacin, we found PD targets that were lower for each of the pathogen groups. This difference was most profound for S. pneumoniae and S. aureus. The 24-h free-drug AUC/MIC required for stasis for S. pneumoniae was 0.56. Likewise, the 24-h free-drug AUC/MIC target for stasis for S. aureus was 1.42. These endpoints are approximately 50- to 100-fold lower than those of comparative fluoroquinolone pharmacodynamic studies. The notable PK/PD efficacy against S. aureus and specifically MRSA strains is particularly exciting, given limited options for the treatment of respiratory tract infections due to S. aureus. Against K. pneumoniae, our identified targets were modestly lower than those of other fluoroquinolones, with a 24-h free-drug AUC/MIC target for stasis of 40.
Recently, pharmacokinetic analyses of oral and intravenous delafloxacin in humans have been published (1, 2). The current doses being studied in clinical trials include 450 mg orally (p.o.) and 300 mg i.v. twice daily (1). These doses correspond to a 24-h total-drug AUC of approximately 61.6 mg · h/liter and 46.8 mg · h/liter, respectively. After accounting for protein binding, which is 84% in humans (1, 2), the corresponding free-drug AUC/MIC values would be 9.9 and 7.5, respectively. Using the PK/PD targets for stasis identified in this study, the twice-daily doses of either 450 mg p.o. or 300 mg i.v. would achieve free-drug exposures that would be adequate to exceed the MIC90 of S. aureus, including MRSA isolates, and S. pneumoniae, including penicillin- and fluoroquinolone-resistant isolates (3–7, 25). The drug exposures would also be predicted to achieve AUC/MIC exposures in excess of the stasis targets identified in this study for K. pneumoniae isolates with a delafloxacin MIC of ≤0.1 mg/liter. This would include all K. pneumoniae isolates that are susceptible to other fluoroquinolones and a subset of those that are resistant to other fluoroquinolones, where it has been noted that the delafloxacin MIC90 has been as high as 4 to 8 mg/liter (3–5). Pharmacodynamic study of delafloxacin against organisms resistant to other fluoroquinolones and/or with elevated delafloxacin MICs will be an important area for future study.
In conclusion, delafloxacin exhibited potent in vitro and in vivo efficacy against three important respiratory pathogen groups, including S. aureus (MSSA and MRSA), S. pneumoniae, and K. pneumoniae. Efficacy against the former two pathogen groups was particularly robust compared to that of other fluoroquinolones. At maximal drug exposures, a >4-log10 kill was observed against these groups, and free-drug AUC/MIC targets were <10 whether one examined stasis or bactericidal endpoints. When combined with human PK results, these studies suggest that the current twice-daily dosing regimens in development should achieve drug exposures that exceed the stasis targets identified in this study for each of the pathogen groups and, perhaps most importantly, against MRSA. The data presented will be useful for delafloxacin dosing regimen optimization for the treatment of respiratory tract infections and for setting the preliminary breakpoints.
ACKNOWLEDGMENT
This study was funded by Melinta Therapeutics, Inc.
REFERENCES
- 1.Hoover R, Hunt T, Benedict M, Paulson SK, Lawrence L, Cammarata S, Sun E. 2016. Safety, tolerability, and pharmacokinetic properties of intravenous delafloxacin after single and multiple doses in healthy volunteers. Clin Ther 38:53–65. doi: 10.1016/j.clinthera.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Hoover R, Hunt T, Benedict M, Paulson SK, Lawrence L, Cammarata S, Sun E. 2016. Single and Multiple ascending-dose studies of oral delafloxacin: effects of food, sex, and age. Clin Ther 38:39–52. doi: 10.1016/j.clinthera.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 3.Almer LS, Hoffrage JB, Keller EL, Flamm RK, Shortridge VD. 2004. In vitro and bactericidal activities of ABT-492, a novel fluoroquinolone, against Gram-positive and Gram-negative organisms. Antimicrob Agents Chemother 48:2771–2777. doi: 10.1128/AAC.48.7.2771-2777.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harnett SJ, Fraise AP, Andrews JM, Jevons G, Brenwald NP, Wise R. 2004. Comparative study of the in vitro activity of a new fluoroquinolone, ABT-492. J Antimicrob Chemother 53:783–792. doi: 10.1093/jac/dkh180. [DOI] [PubMed] [Google Scholar]
- 5.Nilius AM, Shen LL, Hensey-Rudloff D, Almer LS, Beyer JM, Balli DJ, Cai Y, Flamm RK. 2003. In vitro antibacterial potency and spectrum of ABT-492, a new fluoroquinolone. Antimicrob Agents Chemother 47:3260–3269. doi: 10.1128/AAC.47.10.3260-3269.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Remy JM, Tow-Keogh CA, McConnell TS, Dalton JM, Devito JA. 2012. Activity of delafloxacin against methicillin-resistant Staphylococcus aureus: resistance selection and characterization. J Antimicrob Chemother 67:2814–2820. doi: 10.1093/jac/dks307. [DOI] [PubMed] [Google Scholar]
- 7.Zhanel GG, Palatnick L, Nichol KA, Bellyou T, Low DE, Hoban DJ. 2003. Antimicrobial resistance in respiratory tract Streptococcus pneumoniae isolates: results of the Canadian Respiratory Organism Susceptibility Study, 1997 to 2002. Antimicrob Agents Chemother 47:1867–1874. doi: 10.1128/AAC.47.6.1867-1874.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kingsley J, Mehra P, Lawrence LE, Henry E, Duffy E, Cammarata SK, Pullman J. 2016. A randomized, double-blind, phase 2 study to evaluate subjective and objective outcomes in patients with acute bacterial skin and skin structure infections treated with delafloxacin, linezolid or vancomycin. J Antimicrob Chemother 71:821–829. doi: 10.1093/jac/dkv411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O'Riordan W, Mehra P, Manos P, Kingsley J, Lawrence L, Cammarata S. 2015. A randomized phase 2 study comparing two doses of delafloxacin with tigecycline in adults with complicated skin and skin-structure infections. Int J Infect Dis 30:67–73. doi: 10.1016/j.ijid.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Mandell LA. 2015. Community-acquired pneumonia: an overview. Postgrad Med 127:607–615. doi: 10.1080/00325481.2015.1074030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. 2005. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest 128:3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. 2013. Antibiotic resistance threats in the United States, 2013. Centers for Disease Control and Prevention, Atlanta, GA: www.cdc.gov/drugresistance/threat-report-2013. [Google Scholar]
- 13.Moellering RC., Jr 2012. MRSA: the first half century. J Antimicrob Chemother 67:4–11. doi: 10.1093/jac/dkr437. [DOI] [PubMed] [Google Scholar]
- 14.Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. 2015. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 28:603–661. doi: 10.1128/CMR.00134-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute. 2012. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, 9th ed CLSI document M07-A9. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 16.National Research Council Committee. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC. [Google Scholar]
- 17.Andes D, Craig WA. 2002. Pharmacodynamics of the new fluoroquinolone gatifloxacin in murine thigh and lung infection models. Antimicrob Agents Chemother 46:1665–1670. doi: 10.1128/AAC.46.6.1665-1670.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andes D, Craig WA. 2003. Pharmacodynamics of the new des-F(6)-quinolone garenoxacin in a murine thigh infection model. Antimicrob Agents Chemother 47:3935–3941. doi: 10.1128/AAC.47.12.3935-3941.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andes DR, Craig WA. 1998. Pharmacodynamics of fluoroquinolones in experimental models of endocarditis. Clin Infect Dis 27:47–50. doi: 10.1086/514624. [DOI] [PubMed] [Google Scholar]
- 20.Craig W, Dalhoff A. 1998. Pharmacodynamics of fluoroquinolones in experimental animals. Handb Exp Pharmacol 127:208–232. [Google Scholar]
- 21.Craig WA. 1998. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 26:1–10. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 22.Drusano GL, Johnson DE, Rosen M, Standiford HC. 1993. Pharmacodynamics of a fluoroquinolone antimicrobial agent in a neutropenic rat model of Pseudomonas sepsis. Antimicrob Agents Chemother 37:483–490. doi: 10.1128/AAC.37.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dudley MN. 1991. Pharmacodynamics and pharmacokinetics of antibiotics with special reference to the fluoroquinolones. Am J Med 91:45S–50S. doi: 10.1016/0002-9343(91)90311-K. [DOI] [PubMed] [Google Scholar]
- 24.Forrest A, Nix DE, Ballow CH, Goss TF, Birmingham MC, Schentag JJ. 1993. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother 37:1073–1081. doi: 10.1128/AAC.37.5.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gunderson SM, Hayes RA, Quinn JP, Danziger LH. 2004. In vitro pharmacodynamic activities of ABT-492, a novel quinolone, compared to those of levofloxacin against Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Antimicrob Agents Chemother 48:203–208. doi: 10.1128/AAC.48.1.203-208.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]