Abstract
Traumatic occipitocervical dissociation (OCD) results from ligamentous injury to the craniocervical junction and is associated with a high rate of mortality and significant neurologic morbidity. The diagnosis is frequently missed on initial lateral cervical spinal radiographs mainly due to inadequate visualization of radiological landmarks and low degree of suspicion. Widespread availability of multidetector computed tomography (MDCT) of the spine and development of better diagnostic radiological criteria has allowed timely diagnosis and good clinical outcome following posterior occipitocervical fusion and instrumentation for a pathology that was once considered uniformly fatal. The present paper reviews the clinical features, diagnosis, and management of OCD in light of most recent literature.
Keywords: Atlanto-occipital dislocation, Occipito cervical dislocation, Cervical spine, Craniocervical junction, Occipitocervical fusion, Trauma
Introduction
The occipitocervical junction (OCJ) consists of structurally important osseous and ligamentous complexes that stabilize the skull base to the spine. Compromise of either the bony or ligamentous complex jeopardize the integrity of the occipitocervical junction. Occipitocervical dissociation (OCD) or atlantooccipital dislocation (AOD) was first described by Blackwood in 1908 and was considered quite rare as compared to other cervical spine injuries [1]. This may be secondary to the amount of force required to disrupt the occipitoatlantal junction that often proves fatal to the victim of this type of injury due to lack of in field advanced prehospital care and resuscitation accounting for the rarity of OCD in trauma victims presenting to the emergency department (ED); being reported in only about 1 % of patients presenting with cervical trauma [2, 3]. On the other hand, various studies have shown that in patients whose deaths are directly related to cervical spine injuries, 20 to 30 % are the result of OCD [2–4]. The often quoted low incidence of OCD (<1 %) is based on older prospective study and may be an underestimate in the current era [2]. The advent of specialized emergency response systems and the evolution of emergency medicine as a specialty coupled with advances in radiological imaging with better recognition of the diagnosis of OCD have served to alter the epidemiology of this injury over the last couple of decades [5–8, 9•]. Improvements in field resuscitation, cervical immobilization, and rapid transport have resulted in more survivors of OCD being evaluated by clinicians in the emergency department. This is evident from a number of case reports and individual case series documenting survival after OCD with reports of successful management and good neurologic recovery emphasizing the importance of prompt diagnosis and management [3, 7, 10, 11•, 12, 13]. The challenge now lies in having a high index of suspicion and appropriate recognition of this injury as it may manifest with subtle bony radiographic and computed tomography findings that has high potential to go unnoticed if not carefully looked for, especially in a patient with no neurological deficits which is not uncommon in patients with OCD who present to the emergency department [10].
Anatomy and biomechanics
A number of ligaments plays a vital role in maintaining the stability of occipitocervical junction and can be divided into two separate groups. The first group consists of the articular capsule ligaments, the anterior and posterior atlanto-occipital ligaments, and two lateral atlanto-occipital ligaments that attach the cranium to the atlas (C1) (Fig. 1) [14–16]. The anterior atlanto-occipital ligament is a continuation of the anterior longitudinal ligament, and the posterior atlanto-occipital ligament spans between the posterior border of the foramen magnum and the posterior atlantal arch. The cruciate ligament also contributes to the stability of this articulation.
Fig. 1.
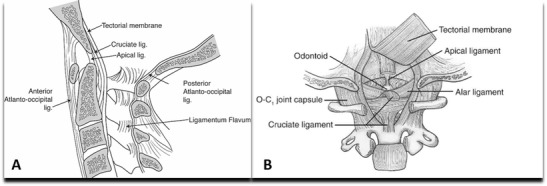
Artistic illustration of lateral (a) and posterior (b) views of the craniovertebral junction and the stabilizing ligaments. Note that the cruciate ligament is composed of horizontal fibers (i.e., transverse ligament) and vertical fibers. b The tectorial membrane, the rostral extent of the posterior longitudinal ligament, has been reflected in (b) to allow for visualization of more ventral structures
The second groups of ligaments are responsible for stability across the craniocervical junction and include the apical dental ligament, the alar ligaments, the tectorial membrane, and the ligamentum nuchae (Fig. 1) [14–16]. The alar ligaments are paired structures, each of which has two components: the atlanto alar and the occipital alar. These ligaments connect the tip of the odontoid to the occipital condyles and the lateral masses of the atlas, respectively, and are the main restraints for axial rotation, with each ligament specifically restricting contralateral axial rotation (Fig. 1). The apical dental ligament and the ligamentum nuchae contribute only slightly to the stability of the craniovertebral junction. The tectorial membrane is a continuation of the posterior longitudinal ligament and runs from the dorsal surface of the odontoid to insert on the ventral surface of the foramen magnum and resists hyperextension [14–16].
OCD occurs following complete or near complete disruption of the ligamentous structures between the occiput and the upper cervical spine. Extreme forces in hyperextension, hyperflexion, and lateral flexion alone or in combination can result in this injury [17]. The prominent force responsible for producing OCD is often hyperextension that results in rupture of the tectorial membrane [13, 18, 19]. Incompetence of the alar ligaments and tectorial membrane allows for anterior dislocation of the cranium with respect to the upper cervical spine [20]. Some authors have suggested that hyperflexion forces may also be involved in some cases of AOD based on the observation that the posterior elements of C1 and C2 are commonly separated in the setting of AOD [17].
Clinical presentation
High-speed motor vehicle accidents and striking of pedestrians by motor vehicles remain the most common causes of craniocervical dissociation [17, 21]. OCD is more common among children and young adults. In fact, the injury is three times more common in children than in adults [2]. A relatively horizontal articular surfaces and more laxity of the ligamentous structures, combined with the presence of a relatively large head and a higher effective fulcrum in the pediatric cervical spine may account for these differences. The considerable force required to cause OAD explains the presence of often concurrent head, spinal cord, or multisystem traumatic injuries in patients with OCD. Neurological injury from AOD can be devastating and may often lead to sudden death secondary to brainstem injury [22]. Neural injury may be direct, as a result of traction or compression mechanisms, or indirect, secondary to cerebrovascular injury leading to ischemia [7, 10, 11•, 23]. Patients with vertebral artery insufficiency at this level may exhibit Wallenberg syndrome, consisting of ipsilateral defects of cranial nerves V, IX, X, and XI; ipsilateral Horner syndrome; dysphagia; and cerebellar dysfunction [7, 10, 11•, 23]. Due to respiratory compromise resulting from brainstem compression, mechanical ventilation if often needed and can make definitive neurologic assessment difficult. Survivors of OCD often have neurological impairment including lower cranial nerve deficits and spinal cord injury that may manifest as unilateral or bilateral sensory and motor deficits, cruciate paralysis, or even quadriplegia [7, 10, 11•, 23]. Reflex examination should be interpreted cautiously, given the possibility of spinal shock. Concomitant traumatic injuries to the brain, chest, abdomen, and extremities can also masquerade the underlying clinical exam and associated deficits. Autonomic dysregulation, including neurogenic shock, may also be a presenting symptom and should be appropriately recognized and managed to ensure hemodynamic stability. Despite the significant nature of the injury, up to 20 % of patients with AOD may have normal neurological examination at presentation with severe neck pain the only symptom in such patients [7, 10, 11•, 23]. It is in this group of patients with no deficits that the potential to miss an underlying OCD is of paramount importance and hence any patient involved in high-energy trauma should be suspected of having OCD, irrespective of clinical findings, and appropriate precautionary measures should be taken until the diagnosis is ruled out.
Classification
Traynelis et al. [17] classified occipitocervical dissociation patterns into three types according to the direction of dislocation of the occiput relative to the cervical spine. Type I occipitocervical dislocation consists of anterior displacement of the occiput with respect to C1; type II is primarily a longitudinal distraction with separation of the occiput from the atlas; and type III occipitoatlantal dislocation exists when the occiput is posteriorly dislocated from C1. The extreme instability of these injuries renders the position of the head relative to the neck completely arbitrary and more dependent on external forces than on any internal injury characteristic reducing the overall significance of the classification. Furthermore, this injury classification can miss the spontaneously repositioned injuries or rotatory injuries such as unilateral alar ligament disruptions.
Bellabarba et al. [10] recently published a three-stage classification also known as Harborview classification system with attempt to reflect injury severity and quantify the stability of the occipitocervical junction and associated therapeutic implications (Table 1). Stage I injury is defined as a stable minimally or nondisplaced craniocervical injury in which there is sufficient preservation of ligamentous integrity to allow for nonoperative treatment. Examples of such injuries may include unilateral alar ligament avulsion or a partial ligamentous injury (or sprain), any of which would be documented on magnetic resonance imaging (MRI) as per the authors [10]. A stage 2 injury represents partially or completely spontaneously reduced bilateral craniocervical dissociation (CCD) involving minimal displacement (Harris lines within ≤2 mm beyond the upper limit of normal) [10]. A stage 3 injury denotes a highly unstable injury defined by gross craniocervical malalignment (Harris lines >2 mm beyond acceptable limits), requiring internal fixation [10]. Patients in both stage I and II have minimally displaced occipitocervical injuries per this classification and may have less easily recognized unstable occipitocervical dissociative injuries. The authors recommended dividing these patients into stage I and II based on use of a manual traction test with surgery reserved for patients in group II [10]. The major drawback of this classification is the reliance on plain radiographs and use of dynamic radiography to determine spinal stability in questionable cases [7]. Furthermore, in the author’s series, no lesions were reported that corresponded to a stage I injury, and thus no direct evaluation of this classification scheme is available [7]. These again highlight the point that all these injuries should be considered highly unstable until proven otherwise and if presents often mandates surgical fixation as the stage I injury may not have true OCD based on sensitive CT criteria for diagnosis of OCD [9•]. Also use of manual traction has fallen out of favor at most of the centers and is uncommonly performed for diagnosing unstable injuries. In fact, axial traction should be avoided in cases of OCD especially Traynelis type II OCD because it reproduces the distractive mechanism of injury and can be associated with a possible risk of damaging the spinal cord, medulla, or vertebral arteries and risk of causing neurologic deterioration [17].
Table 1.
Harborview classification for craniocervical injuries [10]
| Stage | Description of injury |
|---|---|
| 1 | Magnetic resonance imaging (MRI) evidence of injury to craniocervical osseoligamentous stabilizers; craniocervical alignment within 2 mm of normal; distraction of ≤2 mm on provocative traction radiography |
| 2 | MRI evidence of injury to craniocervical osseoligamentous stabilizers; craniocervical alignment within 2 mm of normal; distraction of >2 mm on provocative traction radiography |
| 3 | Craniocervical malalignment of >2 mm on static radiography |
Horn et al. [7] proposed another grading scale based on MRI and computed tomography (CT) evidence (Table 2). Grade I injuries are indicated by normal CT findings in relation to established methods of diagnosis (the Power ratio, BDI, BAI–BDI, and X-line) but have moderately abnormal MR imaging findings (high posterior ligaments or occipitoatlantal signal) [7]. These can often be managed conservatively as there is no evidence of a true OCD on CT. In grade II injuries, there is a minimum of one abnormal finding on CT based on established diagnostic criteria or there are grossly abnormal MR imaging findings in the occipitoatlantal joints, tectorial membrane, alar ligaments, or cruciate ligaments often necessitating surgical intervention [7].
Table 2.
Grading scale for occipitoatlantal injuries [7]
| Grade | Definition |
|---|---|
| I | Normal findings on CT based on established methods of diagnosis with moderately abnormal findings on MRI (high signal in posterior ligaments or occipitoatlantal joints) |
| II | ≥1 abnormal finding on CT based on established diagnostic criteria or grossly abnormal MRI findings in occipitoatlantal joints, tectorial membrane, alar ligaments, or cruciate ligaments |
Diagnosis
Even though plain films of the cervical spine are often the first imaging ordered in patients with cervical trauma, inadequate evaluation of the complete cervical spine and various other shortcomings along with wider availability of multi detector computed tomography (MDCT) has changed this algorithm. Injuries to the upper cervical spine are notoriously difficult to detect with plain radiographs, for several reasons such as the parallax effect at the occipitocervical junction and obscuration due to mastoid air cells [12]. These points should be kept in mind when evaluating lateral cervical spine X-rays in patients with spine trauma.
Lateral cervical X-rays when performed should be evaluated to determine traditional measures of instability such as Powers’ ratio, X-line method, condylar gap method, basion-dens interval (BDI), and basion-axial interval (BAI) [8, 24] (Fig. 2). Although the radiographic findings in patients with OCD can quite dramatic, they may be subtle or even absent on initial films [25–28]. When alignment of the bony structures of the CVJ appears normal, careful evaluation of surrogate markers of OCD such as abnormally prominent prevertebral soft tissues, retropharyngeal emphysema, or an increase in the interval between the posterior elements of C1 and C2 may be useful [2, 17]. Powers’ ratio compares measurements relating the skull base to C1 and is demonstrated in Fig. 2. Normal values are typically <0.9 and when it exceeds 1, OCD should be suspected [8, 9•, 24, 29, 30]. Normal values are Powers’ ratio was originally described to detect anterior dislocation injuries and, as such, is less sensitive to distraction or posterior dislocation injuries. BAI when combined with the BDI is known as the Harris method [8, 29, 31, 32] (Fig. 2). The basion-dens interval or BDI is abnormal in the presence of a displacement between the basion and the dens of more than 10 mm in adults or more than 12 mm in pediatric patients. Basion-axial interval or BAI is considered abnormal when there is anterior displacement of 12 mm or more or posterior displacement of 4 mm or more between the basion and posterior C2 line. Nevertheless, difficulty in visualizing all the relevant anatomic landmarks at the CVJ for application of these methods makes diagnosing OCD using plain lateral cervical X-rays [12]. Even when accurately calculated, the BAI-BDI method has a sensitivity of only 50.5 % and a large portion of patients will require additional confirmatory imaging [8, 9•]. Hence even though, the use of Harris lines on a plain X-rays is often recommended for diagnosis of OCD, in the event of a non-diagnostic film in the presence of signs that should raise concern for OCD such as enlargement of the predental space, high cervical spinal cord deficits, respiratory dysfunction or apnea, subarachnoid hemorrhage at the CCJ or cranial nerve deficits; performance of MDCT should be strongly considered [30]. Presence of MRI findings such as signal abnormalities affecting the tectorial membrane, alar and transverse ligaments, or occipitoatlantal joint capsule suspicious of OCD may also indicate towards presence of possible OCD and requires further evaluation with CT scan [7, 10, 29, 30].
Fig. 2.
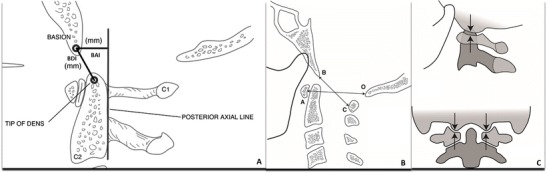
Schematic diagrams depicting the most common X-ray criteria developed to assess the CVJ and diagnosis of OCD. a Demonstrates the basion-dens interval (BDI) and Basion-axial interval (BAI) which together constitutes the Harris lines. The BDI is abnormal in the presence of a displacement between the basion and the dens of more than 10 mm in adults or more than 12 mm in pediatric patients. BAI is considered abnormal when there is anterior displacement of 12 mm or more or posterior displacement of 4 mm or more between the basion and posterior C2 line. b Demonstrates Power’s ratio which can be calculated by dividing the basion-posterior atlas arch (BC) to the opisthion-anterior arch (OA) and is abnormal at values greater than 1. Condyle to C1 interval or CCI (c) is the distance between the occipital condyle and the superior articular facet of the atlas
MDCT has replaced as the imaging modality of choice in an awake symptomatic patient, recommendation and is proven to be more sensitive and specific than cervical spine radiographs (CSR) in detecting spinal column injury [33]. While evaluation of X-rays may lead to suspicion of presence of OCD, MDCT of the spine is now commonly used as a routine screening test for cervical spine injury and allows for more accurate Harris line measurements as the relevant anatomy is visualized 99.75 % of the time with CT as compared to 39 to 84 % of the time with plain films [12], with the additional advantage of enabling the examiner to visualize the occipitocervical and atlantoaxial joints directly to assess for subluxation. Even the slightest asymmetry or distraction of the atlanto-occipital joints should be viewed with suspicion because these joints usually have a displacement tolerance of 2 mm or less [9•, 12, 34]. Dedicated studies using CT scanning to diagnose OCD have supported the use of the BDI (with 10 mm as the cutoff) and the condyle to C1 interval (CCI) as particularly sensitive imaging parameter for atlanto-occipital dislocation [12, 30]. Similar to pediatric population, direct assessment of CCI on a sagittal and coronal CT scan may be more reliable than other radiological measurements to diagnose OCD even in adults [9•, 12, 30, 34] (Fig. 2). While earlier studies suggested a cutoff of ≥2 mm [12] and 2.5 mm [34] as abnormal in adults, a recent retrospective study analyzing a control group and patients with OCD study be Martinez-del-Campo et al. [9•] proposed a cutoff for the CCI of 1.5 mm and condylar sum of 3.0 mm as more accurate with 100 % sensitivity and specificity and no false-negatives as compared to all other radiological parameters used to diagnosed OCD. In the same study, the cutoff of 2.0 and 2.5 mm had higher false-negative rates of 13.6 and 22.7 %, respectively. In children, the CCI determined on CT has the highest diagnostic sensitivity and specificity for AOD and should be performed in the event of any suspicion of OCD [30]. In the study by Pang et al. [30], a normal CCI was 1.28 ± 0.26 mm and proposed a CCI ≥4 mm as diagnostic for AOD with a sensitivity and specificity of 100 % compared with other standard diagnostic tests including the Powers ratio, Wholey method, Harris BAI-BDI, and Sun interspinous ratio.
Based on level III evidence, the most recent guidelines from the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee recommend applying the BDI-BAI (Harris lines) method on a plain lateral cervical X-ray in adults [35•]. If this is non-diagnostic and there is high clinical suspicion or significant prevertebral soft tissue swelling, CT and/or MRI are recommended. In children, the CCI determined on CT has the highest diagnostic sensitivity and specificity for AOD and should be considered the investigation of choice for diagnosing OCD [30].
With the recent studies, showing the superiority of CCI even in adults, use of CT with assessment of CCI may become the standard criteria for diagnosing OCD in the future [9•]. MRI generally demonstrates increased T2-weighted signal intensity within the occiput-C1 and C1-C2 articulations [7, 10, 30]. Definitive evidence of disruption of the alar and tectorial ligaments can sometimes be seen, although making this determination may be difficult. Evaluation of the spinal cord and brainstem parenchyma may reveal injuries ranging from mild edema and increased T2-weighted signal intensity to the presence of intraspinal hematoma or even transection. Epidural fluid collections representing hematoma or cerebrospinal fluid are commonly seen, as is the presence of subdural hematoma. Extensive soft tissue swelling extending to the occipitocervical finding is a universal finding and is easily identified on MRI.
While controversial, manual traction views under specific, controlled conditions have been advocated by some investigators for a selected group of patients in whom the diagnosis of occipitocervical dissociation is uncertain [10]. Use of newer criteria with very high sensitivity and specificity may obviate the utility of this test. If performed, it should be done in the operating room by using live fluoroscopic evaluation with electro diagnostic monitoring. It is recommended to use manual traction rather than weights as it provides important proprioceptive feedback. With a negative test result, a firm end point is felt almost immediately by the surgeon performing the distraction.
Treatment and outcomes
Improvement in maintenance of hemodynamic and respiratory instability at the scene and inline stabilization of the neck and cervical spine injury precautions, including the proper application of a rigid cervical collar at the trauma scene and during transfer to the hospital, had led to an increasing number of these patients survive this injury that was once considered fatal [2, 7, 9•, 10]. This is important as recent modern series have reported mortality rates as low as 0 % in patients who were diagnosed on initial evaluation and appropriately treated, mostly with surgery [11•]. This is in contrast to studies where if the diagnosis of OCD was delayed by a mean of 2 days (range 1–15 days), almost 40 % of these patients suffering profound neurological deterioration before AOD was clinically recognized exemplifying the extreme unstable nature of this injury [10].
Once the diagnosis has been confirmed, continued provisional stabilization should be maintained until definitive surgical intervention can be performed. The use of traction in treatment of patients with OCD is controversial with contradictory opinions in various studies and has been associated with a 10 % risk of neurological deterioration [27, 35•, 36–38]. While not routinely recommended, the goal of traction, if used, is mainly to decompress the neural elements by realigning the bony structures and should be best reserved for instances of type I (anterior), type III (posterior), and lateral AOD in patients with neurological deficit [17]. Similarly, the most appropriate form of provisional stabilization is controversial and depends on many factors, including the timing of surgery, the degree of initial displacement, and the patient’s neurologic status, body habitus, and associated injuries. Possible options include rigid cervical collar immobilization, use of halo immobilization, and various other options such as taping of the head to sandbags on both sides or use of Trendelenburg positioning, if tolerated, to minimize distraction [35•]. External immobilization has a high failure rate. Use of nonoperative measures alone can result in worsening in up to 50 % of patients and should be avoided as OCD as ligamentous injury is the main mode of failure in OCD and is unlikely to heal over time despite prolonged external in a patient who has a true OCD [35•].
Cranio-cervical fixation is the treatment of choice in most cases of traumatic OCD as has been recommended in the most recent guidelines from the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee [35•]. Posterior occipitocervical fusion is the procedure of choice which can be done using a variety of techniques including posterior wiring and structural grafting, Ransford loop fixation with wiring or plate/rod and screw fixation with structural grafting [39, 40] (Fig. 3). We recommend the use of electro diagnostic monitoring with prepositioning baselines and continued provisional stabilization for turning patients with this highly unstable injury into the prone position. The development of rigid fixation has led to increasingly successful outcomes and a concomitant decrease in the need for postoperative immobilization [39–41]. Wire or cable fixed rods or loops represented an advance over prior techniques, but such constructs only provided semi rigid fixation. Modern segmental screw-based constructs enable rigid short-segment fixation and provide adequate stability to achieve successful fusion in over 90 % of patients [39, 41]. The details of surgical technique and other nuances are beyond the scope of this paper.
Fig. 3.

Lateral cross table X-ray (a) of the cervical spine demonstrating distraction across the CVJ suggestive of OCD. CT scan performed confirmed the diagnosis by clearly demonstrating increased CCI interval of more than 2 mm (arrow in b) and an abnormal powers ration of >1 (c). An occipitocervical plating and fusion was performed (d)
Treatment outcomes in survivors of occipitocervical dissociation depend on the type and severity of associated injuries (particularly intracranial injuries and cerebrovascular injury), the severity of neurologic deficits, and the timeliness with which the diagnosis of craniocervical dissociation is recognized [7, 10, 11•]. Missed diagnosis of OCD is the most important factor associated with negative outcome in patients sustaining this injury and is higher in patients with other associated significant injuries and reliance on X-rays along for initial diagnosis of OCD [1, 10, 11•, 12]. While preserved or less dramatic neurological findings can result in good overall long-term outcome in patients with OCD diagnosed at the time of injury, the degree of suspicion for OCD in this group of patients may be low with potential to miss the diagnosis and hence should be kept in mind [10, 11•].
Conclusion
OCD is a devastating injury and is more prevalent than was originally considered with a significant morbidity and mortality if left unrecognized. Availability of high resolution CT has facilitated the diagnosis due to better visualization of the craniocervical junction. Recognition of newer diagnostic criteria for OCD, especially abnormal condylar separation on a high resolution MDCT, has the potential to allow easier recognition and reduce the incidence of missed diagnosis with its untoward sequel. A high index of suspicion following high impact trauma with early recognition and prompt surgical fixation can lead to good clinical outcome. Posterior occipitocervical fusion and instrumentation remains the surgical treatment of choice.
Compliance with ethical standards
Conflict of interest
Manish K. Kasliwal declares that he has no conflict of interest.
Ricardo B. Fontes reports personal fees from Stryker, outside the submitted work.
Vincent C. Traynelis reports personal fees from Medtronic, during the conduct of study. He has received grants in the form of Institutional Fellowship Support from both Globus and AO, outside of the submitted work. In addition, Dr. Traynelis has a patent for Posterior cervical instrumentation with royalties paid.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding
No funding was received in support of this study.
Footnotes
This article is part of the Topical Collection on Cervical Injuries and Treatment
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Blackwood NJ., III Atlo-occipital dislocation: a case of fracture of the atlas and axis, and forward dislocation of the occiput on the spinal column, life being maintained for thirty-four hours and forty minutes by artificial respiration, during which a laminectomy was performed upon the third cervical vertebra. Ann Surg. 1908;47:654–8. doi: 10.1097/00000658-190805000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bucholz RW, Burkhead WZ. The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg Am. 1979;61:248–50. [PubMed] [Google Scholar]
- 3.Powers B, Miller MD, Kramer RS, Martinez S, Gehweiler JA., Jr Traumatic anterior atlanto-occipital dislocation. Neurosurgery. 1979;4:12–7. doi: 10.1227/00006123-197901000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Ehlinger M, Charles YP, Adam P, et al. Survivor of a traumatic atlanto-occipital dislocation. Orthop Traumatol Surg Res : OTSR. 2011;97:335–40. doi: 10.1016/j.otsr.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Chan RN, Ainscow D, Sikorski JM. Diagnostic failures in the multiple injured. J Trauma. 1980;20:684–7. doi: 10.1097/00005373-198008000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma. 1993;34:342–6. doi: 10.1097/00005373-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine. 2007;6:113–20. doi: 10.3171/spi.2007.6.2.113. [DOI] [PubMed] [Google Scholar]
- 8.Lee C, Woodring JH, Goldstein SJ, Daniel TL, Young AB, Tibbs PA. Evaluation of traumatic atlantooccipital dislocations. AJNR Am J Neuroradiol. 1987;8:19–26. [PMC free article] [PubMed] [Google Scholar]
- 9.•.Martinez-Del-Campo E, Kalb S, Soriano-Baron H, et al. Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine. 2016;24(4):535–45. This study defines rigorous computed tomography criteria for the occipital condyle–C1 interval that has higher sensitivity and specificity to allow radiological diagnsois of occipitocervical dissociatio in adults. [DOI] [PubMed]
- 10.Bellabarba C, Mirza SK, West GA, et al. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine. 2006;4:429–40. doi: 10.3171/spi.2006.4.6.429. [DOI] [PubMed] [Google Scholar]
- 11.•.Mendenhall SK, Sivaganesan A, Mistry A, Sivasubramaniam P, McGirt MJ, Devin CJ. Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J : Off J N Am Spine Soc. 2015;15:2385–95. This is one of the largest retrospective series of traumatic adult atlantooccipital dislocation that identifies various factors affecting outcome of patients with AOD and demonstrates that if timely diagnosed, these patients have good quality of life following surgical treatment.
- 12.Dziurzynski K, Anderson PA, Bean DB, et al. A blinded assessment of radiographic criteria for atlanto-occipital dislocation. Spine. 2005;30:1427–32. doi: 10.1097/01.brs.0000166524.88394.b3. [DOI] [PubMed] [Google Scholar]
- 13.Page CP, Story JL, Wissinger JP, Branch CL. Traumatic atlantooccipital dislocation. Case report. J Neurosurg. 1973;39:394–7. doi: 10.3171/jns.1973.39.3.0394. [DOI] [PubMed] [Google Scholar]
- 14.Martin MD, Bruner HJ, Maiman DJ. Anatomic and biomechanical considerations of the craniovertebral junction. Neurosurgery. 2010;66:2–6. doi: 10.1227/01.NEU.0000365830.10052.87. [DOI] [PubMed] [Google Scholar]
- 15.Tubbs RS, Hallock JD, Radcliff V, et al. Ligaments of the craniocervical junction. J Neurosurg Spine. 2011;14:697–709. doi: 10.3171/2011.1.SPINE10612. [DOI] [PubMed] [Google Scholar]
- 16.Yuksel M, Heiserman JE, Sonntag VK. Magnetic resonance imaging of the craniocervical junction at 3-T: observation of the accessory atlantoaxial ligaments. Neurosurgery. 2006;59:888–92. [DOI] [PubMed]
- 17.Traynelis VC, Marano GD, Dunker RO, Kaufman HH. Traumatic atlanto-occipital dislocation. Case report. J Neurosurg. 1986;65:863–70. doi: 10.3171/jns.1986.65.6.0863. [DOI] [PubMed] [Google Scholar]
- 18.Fruin AH, Pirotte TP. Traumatic atlantooccipital dislocation. Case report. J Neurosurg. 1977;46:663–6. doi: 10.3171/jns.1977.46.5.0663. [DOI] [PubMed] [Google Scholar]
- 19.Zampella EJ, Duvall ER, Langford KH. Computed tomography and magnetic resonance imaging in traumatic locked-in syndrome. Neurosurgery. 1988;22:591–3. doi: 10.1227/00006123-198803000-00027. [DOI] [PubMed] [Google Scholar]
- 20.Werne S. Studies in spontaneous atlas dislocation. Acta Orthop Scand Suppl. 1957;23:1–150. [PubMed] [Google Scholar]
- 21.Dickman CA, Papadopoulos SM, Sonntag VK, Spetzler RF, Rekate HL, Drabier J. Traumatic occipitoatlantal dislocations. J Spinal Disord. 1993;6:300–13. doi: 10.1097/00002517-199306040-00004. [DOI] [PubMed] [Google Scholar]
- 22.Fisher CG, Sun JC, Dvorak M. Recognition and management of atlanto-occipital dislocation: improving survival from an often fatal condition. Can J Surg J Can de Chir. 2001;44:412–20. [PMC free article] [PubMed] [Google Scholar]
- 23.Sweet J, Ammerman J, Deshmukh V, White J. Cruciate paralysis secondary to traumatic atlantooccipital dislocation. J Neurosurg Spine. 2010;12:19–21. doi: 10.3171/2009.8.SPINE08496. [DOI] [PubMed] [Google Scholar]
- 24.Rojas CA, Bertozzi JC, Martinez CR, Whitlow J. Reassessment of the craniocervical junction: normal values on CT. AJNR Am J Neuroradiol. 2007;28:1819–23. doi: 10.3174/ajnr.A0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eismont FJ, Bohlman HH. Posterior atlanto-occipital dislocation with fractures of the atlas and odontoid process. J Bone Joint Surg Am. 1978;60:397–9. [PubMed] [Google Scholar]
- 26.Gabrielsen TO, Maxwell JA. Traumatic atlanto-occipital dislocation; with case report of a patient who survived. Am J Roentgenol Radium Therapy, Nucl Med. 1966;97:624–9. doi: 10.2214/ajr.97.3.624. [DOI] [PubMed] [Google Scholar]
- 27.Pang D, Wilberger JE., Jr Traumatic atlanto-occipital dislocation with survival: case report and review. Neurosurgery. 1980;7:503–8. doi: 10.1227/00006123-198011000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Woodring JH, Selke AC, Jr, Duff DE. Traumatic atlantooccipital dislocation with survival. AJR Am J Roentgenol. 1981;137:21–4. doi: 10.2214/ajr.137.1.21. [DOI] [PubMed] [Google Scholar]
- 29.Garrett M, Consiglieri G, Kakarla UK, Chang SW, Dickman CA. Occipitoatlantal dislocation. Neurosurgery. 2010;66:48–55. doi: 10.1227/01.NEU.0000365802.02410.C5. [DOI] [PubMed] [Google Scholar]
- 30.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation—part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery. 2007;61:995–1015. [DOI] [PubMed]
- 31.Harris JH, Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162:881–6. doi: 10.2214/ajr.162.4.8141012. [DOI] [PubMed] [Google Scholar]
- 32.Harris JH, Jr, Carson GC, Wagner LK, Kerr N. Radiologic diagnosis of traumatic occipitovertebral dissociation: 2. Comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162:887–92. doi: 10.2214/ajr.162.4.8141013. [DOI] [PubMed] [Google Scholar]
- 33.Ryken TC, Hadley MN, Walters BC, et al. Radiographic assessment. Neurosurgery. 2013;72(Suppl 2):54–72. doi: 10.1227/NEU.0b013e318276edee. [DOI] [PubMed] [Google Scholar]
- 34.Gire JD, Roberto RF, Bobinski M, Klineberg EO, Durbin-Johnson B. The utility and accuracy of computed tomography in the diagnosis of occipitocervical dissociation. Spine J : Off J N Am Spine Soc. 2013;13:510–9. doi: 10.1016/j.spinee.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 35.•.Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery. 2013;72 Suppl 2:114–26. Describes the most recent guidelines from the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint Guidelines Committee for diagnosis and management of traumatic atlantooccipital dislocation. [DOI] [PubMed]
- 36.Evarts CM. Traumatic occipito-atlantal dislocation. J Bone Joint Surg Am. 1970;52:1653–60. [PubMed] [Google Scholar]
- 37.Levine AM, Edwards CC. Traumatic lesions of the occipitoatthop Relat Res. 1989;(239):53–68. [PubMed]
- 38.Watridge CB, Orrison WW, Arnold H, Woods GA. Lateral atlantooccipital dislocation: case report. Neurosurgery. 1985;17:345–7. doi: 10.1227/00006123-198508000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Garrido BJ, Puschak TJ, Anderson PA, Sasso RC. Occipitocervical fusion using contoured rods and medial offset connectors: description of a new technique. Orthopedics. 2009;32. doi:10.3928/01477447-20090818-11. [DOI] [PubMed]
- 40.Lu DC, Roeser AC, Mummaneni VP, Mummaneni PV. Nuances of occipitocervical fixation. Neurosurgery. 2010;66:141–6. doi: 10.1227/01.NEU.0000365744.54102.B9. [DOI] [PubMed] [Google Scholar]
- 41.Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24:1425–34. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]


