Abstract
A better understanding of the consequences of spine surgery complications is warranted to optimize patient-reported outcomes and contain the rising health care costs associated with the management of adult spinal deformity (ASD). We systematically searched PubMed and Scopus databases using keywords “adult spinal deformity surgery,” “complications,” and “cost” for published studies on costs of complications associated with spinal surgery, with a particular emphasis on ASD and scoliosis. In the 17 articles reviewed, we identified 355,354 patients with 11,148 reported complications. Infection was the most commonly reported complication, with an average treatment cost ranging from $15,817 to $38,701. Hospital costs for patients with deep venous thrombosis, pulmonary thromboembolism, and surgical site infection were 2.3 to 3.1 times greater than for patients without those complications. An effort to collect and characterize data on cost of complications is encouraged, which may help health care providers to identify potential resources to limit complications and overall costs.
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-016-9352-9) contains supplementary material, which is available to authorized users.
Keywords: Adult spinal deformity, Complications, Cost analysis, Outcomes, Scoliosis, Spine surgery
Introduction
Approaches to clinical management of patients with adult spinal deformity (ASD) can be broadly categorized into nonoperative and operative care. Nonoperative care includes treatment approaches such as yoga, physical therapy (aerobic conditioning and core strengthening), stretching, chiropractic manipulation, acupuncture, use of pharmacologic agents, and use of spinal bracing. Excluding the use of pharmacologic agents, nonoperative care is typically associated with no major complications and is often considered the first line of treatment in asymptomatic patients or patients of poor general health with comorbidities contraindicated for surgery [1, 2]. Despite being associated with fewer complications, nonoperative care lacks scientific evidence supporting its efficacy. Patients receiving nonoperative care have reported no significant improvement in back and leg pain, self-image, mental health, health-related quality-of-life (HRQoL) measures, and overall satisfaction with their treatment compared to patients receiving operative care [3–5].
The surgical modalities included in operative care may vary from decompression procedures to anterior-only, posterior-only, or combined anterior-posterior fusion in conjunction with decompression of neural elements to osteotomies [1, 2]. There is strong evidence that surgical treatment of ASD is significantly associated with improvements in patients’ clinical outcomes and quality-of-life measures [5–8]. The downside, however, of operative care is high complication rates, both major and minor. Some of the reported complications in the literature are hemorrhage, pseudoarthrosis, cerebrospinal fluid leaks, infection, neurological deficits, implant failure, thromboembolic events, ischemic optic neuropathy, cardiopulmonary complications, systemic complications, and death [1, 2, 8, 9].
Nasser et al., in a systematic review of 105 studies on complications in spine surgery containing data on 79,471 patients with 13,067 complications, reported an overall complication incidence of 16.4 % [10]. Other studies have reported an estimated 40 to 86 % complication rate occurring in adult patients undergoing scoliosis surgery [11, 12]. Studies report that complication rates tend to be significantly higher in older patients than in younger patients. Yet, older patients undergoing spine surgery for spinal deformities have demonstrated greater improvements in standardized measures of disability, pain, and HRQoL measures than younger patients [7, 13]. Scheufler et al. reviewed clinical outcomes and complications in 30 adult scoliotic patients and found that patients were satisfied with the surgical intervention at 1-year follow-up, despite the majority of patients having high major complication rates [14].
Regardless of the complication rates associated with surgical treatment of ASD, there appears to be an increasing trend in the number of spine deformity surgeries and the costs associated with the treatment. For instance, the total number of spine deformity surgeries between 2000 to 2010 in Medicare patients increased by fourfold, average charge per inpatient stay increased more than 230 %, and total charges for spine deformity surgery increased by 16-fold from $56 million to more than $958 million [15]. Health economic research on ASD surgery has exploded in the past decade, providing tremendous insights on cost indices related to ASD surgery including index cost, direct cost, indirect cost, total cost after an extended period of follow-up, quality-adjusted life-years, or incremental cost/utility ratio [16–19]. However, the cost of spine surgery complications and its impact on overall health care costs related to ASD surgery have received relatively little attention.
Given the increasing demographic shift towards an older population in the USA, an estimated 68 % prevalence of ASD in the elderly [20] and increases in both the number of ASD surgeries and their associated costs [15], it is vital to understand the economic and clinical consequences of complications. Despite the fact that complications are nearly unavoidable in spine surgery and that complications will further increase health care costs, there is a conspicuous gap in the literature on the specific costs of spine surgery complications and the impact of such complications on health care resource utilization and overall costs. With the advent of the “never event” ruling from the Centers for Medicare and Medicaid Services (CMS), which states that certain hospital-acquired adverse events should never occur following spinal surgery, it is essential to examine the cost of spine surgery complications associated with ASD surgery [21]. Understanding the impact of such complications may enable optimization of clinical outcomes and offer new insights in controlling overall cost of care from hospital, patient, and societal perspectives. We therefore carried out a systematic review of the spine surgery literature to ascertain the costs of complications associated with spine surgery and weigh their impact on the overall cost of ASD surgery.
Methods
Inclusion criteria
For this systematic review, we considered clinical articles on surgical correction of spinal deformity in adult (>18 years) patients. We placed no restriction on the type of surgical procedure (anterior, posterior, combined, etc.), location of the surgery (thoracic, lumbar, or cervical), or when the complication occurred (intraoperative vs. postoperative). Studies needed to mention the type and number of complications associated with the surgical procedure. In addition, only the studies reporting costs of specific complications or additional increases in overall treatment costs (direct or indirect) due to complications were included in the review. We excluded cadaveric studies, case reports, and editorials.
Search strategy
The electronic reference databases PubMed and Scopus were queried using the key words “adult spinal deformity surgery,” “complications,” and “costs.” The primary limits applied to our search strategy were “Humans” and “English language articles.” There were no restrictions imposed on publication status or publication date. No attempt was made to solicit unpublished data. From our initial query, we identified 18 articles in PubMed and 40 in Scopus. The abstract and title of each article were reviewed based on our inclusion/exclusion criteria and the full-text article was retrieved if the content was considered relevant to our study goals. This systematic screening resulted in 6 relevant articles. To ensure complete review, we checked the references of each of the 6 included articles and selected those cross-referenced articles that we deemed satisfactory based on our inclusion/exclusion criteria. A schematic representation of the search strategy is presented in Fig. 1.
Fig. 1.
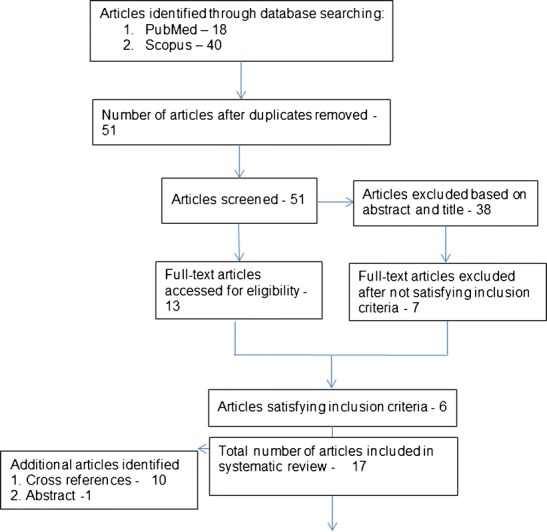
Flow diagram of the article selection process for relevant studies
Results
From our search, we identified 17 articles that met our inclusion criteria. Table S1 provides a detailed description of the reviewed articles by authors, year of study, reported diagnoses or type of surgical procedure, number of patients in each study, number of reported complications, duration of study to measure the intended outcomes, type of cost metric measured, cost of specific complications, and overall costs associated with the treatment.
Characteristics of studies included in systematic review
Of the 17 studies included in the review [18, 22–34, 37–39], two studies were prospective in design and the rest were retrospective studies. Only one study was conducted in Canada [22]. These articles were published between 1999 and 2016 and included a total of 355,344 subjects, with the number of subjects in each study ranging from 42 to 278,866. The lowest and the highest mean ages of the patients reported by the studies were 42.3 and 62.4 years. Average follow-up of the studies ranged from 30 days to 68 months. Eight studies reported only complications, six studies reported complications and revision surgeries, one study reported complications and adverse events, and two studies reported either adverse events or revision surgeries. The number of complications in each study ranged from 5 to 5402 with a total of 11,168 reported complications. The proportion of complications in each study ranged from 1.3 to 57.0 %, yielding an overall complication incidence of 3.13 %. Number of adverse events reported was 3367 and number of revision surgeries reported was 504. Direct costs (costs related to hospital care—payers’ perspective) of spine surgery complications were reported in all the studies, while two studies additionally reported indirect costs (costs related to patient—societal perspective) of complications [23, 24••].
Cost analysis—complications
Ten of the 17 reviewed articles reported costs related to medical or surgical complications occurring during either intraoperative or postoperative period. The most frequently reported complication was infection, specifically surgical site infections (SSIs). The average direct cost to treat a patient with an “infection or SSI” complication ranged from $15,817 to $38,701. McGirt et al. reported the average direct cost to treat one SSI case as $15,817, which translates to a total direct cost of $4.6 million dollars in treating 292 SSIs [25]. Whitmore et al. reported an additional increase in treatment cost of $4067 to treat a wound infection [26], while Godil et al. estimated infection-related costs per 100 spinal fusion to be $438,165 [27]. Three studies reported cost of complications by comparing treatment costs between infection and non-infection/control cohorts [24••, 27, 28]. In general, the additional increase in direct cost to treat a patient in the infection cohort was $6719 to $12,619 more than the direct cost to treat a patient in the control cohort. The advantage of such a comparison, in the context of using an intervention measure among treatment cohorts, is predicting the impact of complications on the overall costs. For instance, Godil et al. estimated that use of topical vancomycin powder to treat SSIs will result in a cost savings of $433,765 per 100 posterior spinal fusions [27]. Similarly, Theologis et al. demonstrated a cost savings of $244,402 per 100 thoracolumbar adult deformity procedures [28]. In contrast to infection versus non-infection comparisons, Patil et al. reported the effect of number of complications on the mean total hospital charges. The mean total hospital charges for an adult patient with 0, 1, 2, and 3 complications were $51,622, $68,100, $1.03 million, and $1.18 million, respectively [29].
The average total costs of several other complications reported in the literature are as follows: (a) pseudoarthrosis—$76,695, (b) instrument failure—$66,838, (c) junctional failure—$42,766, (d) neurological/radiculopathy—$29,561, (e) medical complications—$26,622, and (f) pain complication—$20,947 [30]. The median inpatient charges reported for patients with deep venous thrombosis (DVT) was $607,952 more compared to patients without DVT (3.1 times greater), while the median inpatient charges for patients with pulmonary embolism (PE) was $386,479 more compared to patients without PE (2.3 times greater) [31••]. Whitmore et al. reported an average increase in direct cost of $7233, $6968, and $4537 for pulmonary complication, instrument malposition, and new neurological deficit, respectively. Likewise, Nandyala et al. reported that the additional increase in mean total hospital costs to treat a patient with cervical durotomy or lumbar durotomy complication was $7638 and $2412, respectively [32].
Cost analysis—revision surgeries
Five studies reported cost due to revision surgeries. Revision surgeries were due to symptomatic lumbar disc herniation or recurrent stenosis. One study did not report the reason for revision surgery. The average direct cost of revision surgeries ranged from $26,593 to $86,673. Ambrossi et al. reported the estimated cost of recurrent disc herniation per 100 cases of first-lumbar discectomy to be approximately $289,797 [33].
Cost analysis—adverse events
Hellsten et al. reported the incremental dollar cost to treat a patient based on the severity grade of adverse events (AEs). The severity grades were defined as follows: grade 1—requires no/minimal treatment, grade 2—requires treatment and is not likely to cause long-term (>6 months) sequelae, grade 3—requires treatment and is most likely to cause long-term sequel, and grade 4—death. The mean cost per discharge for cases with AEs was 50 % more than discharge costs of cases without AEs. The incremental dollar cost to treat a patient with AE severity grade 1 to grade 3 increased from $4224 to $147,285. This exponential increase translates to a 6.5 times total increment in dollar cost of $0.66 million for AE severity grade 1 to $4.27 million for AE severity grade 3 over a 4-year period [22].
Cost analysis—indirect costs
The impact of complications was also reported in terms of indirect costs. Kuhns et al. reported that infection following dorsal cervical fusion surgery was associated with an additional increase in indirect costs of $3739 compared to patients without infection. In the same study, the authors reported that presence of infection was associated with an additional 23 days of lost wok [24••]. Adogwa et al. reported revision surgery in 42 patients was associated with a median 6.5 months of loss of work and mean 2-year indirect costs of $18,623 ± 909 [34]. Tosteson et al. reported the mean indirect cost of 63 repeat surgeries as $28,019 [23].
Discussion
The purpose of this systematic review was to identify the cost of complications occurring during the surgical treatment of ASD or scoliosis from the spine surgery literature. We also sought to determine the extent to which the cost of these complications impacts overall costs, including direct or indirect costs.
Although surgical correction of ASD is cost-effective and improves quality-of-life and clinical outcomes compared to nonoperative treatment, it is nonetheless associated with complications. In the setting of increasing health care resource utilization associated with the surgical correction of ASD, it is essential to identify, characterize, and quantify cost of complications to improve the safety and cost-effectiveness of patient care. Results from our review highlight the degree to which occurrence of complications or revision surgeries increase the overall costs associated with the management of ASD. While this literature review is by no means a comprehensive assessment of cost of spine surgery complications and its impact on the overall costs associated with ASD surgery, our intention was to present a broad overview on the effect that complications can have on the overall costs in the surgical treatment of ASD.
This systematic review has limitations. First, we did not have a strict operative definition of our keyword “complication” and as a result included articles that reported cost metrics due to complications, AEs, or revision surgeries. Unfortunately, there is no consistent definition of “complication” in the spine literature. The term complication is usually defined in the context of undesirable or unexpected events that occur intraoperatively or following surgery. In contrast, complication is also used to define reoperation that may occur weeks to months following the primary surgery. Dekutoski et al., in a systematic review of 22 articles on spine surgery, defined complication as “an unintended and undesirable diagnostic or therapeutic event that may impact the patients’ care” [35]. A standardized definition of complication that takes into consideration a patient’s comorbidities and the severity of the complication need to be adopted across institutions for an unbiased estimation and comparison. Second, the majority of the studies included in our review were retrospective, relying on data obtained from administrative databases. Due to the inherent lack of systematic and methodological rigor behind construction of administrative databases [36], it is challenging to use them in epidemiologic and health services research and consequently draw valid and reliable conclusions. Third, because of wide discrepancy in how each study reported complications costs, we could not determine a pooled estimate of a specific complication cost.
Conclusions
Complications related to ASD surgery affect both clinical outcomes and health care costs. In addition to being associated with poorer clinical outcomes, complications can increase hospital and societal costs. Increased hospital costs are a result of additional diagnoses, treatments, and length of stay, while, increases in societal cost may be reflected in loss of productivity, out-of-pocket expenses, and outpatient visits. Needless to say, our results demonstrate that complications impose a substantial clinical and financial burden on health care delivery. It is crucial to quantify the cost of specific complications associated with ASD surgery so that health care providers can optimize patient outcomes and control escalating health care costs associated with management of ASD.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 26.8 kb)
Compliance with ethical standards
Conflict of interest
Samrat Yeramaneni and Chessie Robinson declare that they have no conflict of interest. Richard Hostin reports personal fees from DePuy Synthes and grants from DePuy Synthes, NuVasive, Seeger, DJO, and K2M, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Complications in Spine Surgery
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Good CR, et al. Adult spine deformity. Curr Rev Musculoskelet Med. 2011;4(4):159–67. doi: 10.1007/s12178-011-9101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Youssef JA, et al. Current status of adult spinal deformity. Glob Spine J. 2013;3(1):51–62. doi: 10.1055/s-0032-1326950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith JS, et al. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65(1):86–93. doi: 10.1227/01.NEU.0000347005.35282.6C. [DOI] [PubMed] [Google Scholar]
- 4.Li G, et al. Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine (Phila Pa 1976) 2009;34(20):2165–70. doi: 10.1097/BRS.0b013e3181b3ff0c. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis a prospective multicenter evidence-based medicine study. Spine. 2009;34(20):2171–8. doi: 10.1097/BRS.0b013e3181a8fdc8. [DOI] [PubMed] [Google Scholar]
- 6.Yadla S, et al. Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus. 2010;28(3):E3. doi: 10.3171/2009.12.FOCUS09254. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976) 2011;36(10):817–24. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 8.Glassman SD, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32(24):2764–70. doi: 10.1097/BRS.0b013e31815a7644. [DOI] [PubMed] [Google Scholar]
- 9.Baron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine. 2006;31(19):S106–18. doi: 10.1097/01.brs.0000232713.69342.df. [DOI] [PubMed] [Google Scholar]
- 10.Nasser R, et al. Complications in spine surgery. J Neurosurg Spine. 2010;13(2):144–57. doi: 10.3171/2010.3.SPINE09369. [DOI] [PubMed] [Google Scholar]
- 11.Ganocy T., M. Ohtomo, and O. Boachie-Adjei. Complication rates for combined anterior-posterior adult deformity surgery. in SRS Meeting. 2003.
- 12.Lapp MA, et al. Long-term complications in adult spinal deformity patients having combined surgery: a comparison of primary to revision patients. Spine. 2001;26(8):973–83. doi: 10.1097/00007632-200104150-00025. [DOI] [PubMed] [Google Scholar]
- 13.Daubs MD, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32(20):2238–44. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 14.Scheufler K-M, et al. Less invasive surgical correction of adult degenerative scoliosis. Part II: complications and clinical outcome. Neurosurgery. 2010;67(6):1609–21. doi: 10.1227/NEU.0b013e3181f918cf. [DOI] [PubMed] [Google Scholar]
- 15.McCarthy I, et al. Health economic analysis of adult deformity surgery. Neurosurg Clin N Am. 2013;24(2):293. doi: 10.1016/j.nec.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Kamerlink JR, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am. 2010;92(5):1097–104. doi: 10.2106/JBJS.I.00879. [DOI] [PubMed] [Google Scholar]
- 17.McCarthy IM, et al. Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J. 2014;14(10):2326–33. doi: 10.1016/j.spinee.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy IM, et al. Analysis of the direct cost of surgery for four diagnostic categories of adult spinal deformity. Spine J. 2013;13(12):1843–8. doi: 10.1016/j.spinee.2013.06.048. [DOI] [PubMed] [Google Scholar]
- 19.Kim S, et al. Cost-utility of lumbar decompression with or without fusion for patients with symptomatic degenerative lumbar spondylolisthesis. Spine J. 2012;12(1):44–54. doi: 10.1016/j.spinee.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Schwab F, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30(9):1082–5. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 21.Mattie AS, Webster BL. Centers for Medicare and Medicaid Services’ “ never events”: an analysis and recommendations to hospitals. Health Care Manag. 2008;27(4):338–49. doi: 10.1097/HCM.0b013e31818c8037. [DOI] [PubMed] [Google Scholar]
- 22.Hellsten EK, et al. An economic evaluation of perioperative adverse events associated with spinal surgery. Spine J. 2013;13(1):44–53. doi: 10.1016/j.spinee.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Tosteson AN, et al. The cost effectiveness of surgical versus non-operative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33(19):2108. doi: 10.1097/BRS.0b013e318182e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.••.Kuhns BD, et al. Cost and quality of life outcome analysis of postoperative infections after subaxial dorsal cervical fusions. J Neurosurg Spine. 2015;22(4):381–6. doi: 10.3171/2014.10.SPINE14228. [DOI] [PubMed] [Google Scholar]
- 25.McGirt MJ, et al. Comparative analysis of perioperative surgical site infection after minimally invasive versus open posterior/transforaminal lumbar interbody fusion: analysis of hospital billing and discharge data from 5170 patients: clinical article. J Neurosurg Spine. 2011;14(6):771–8. doi: 10.3171/2011.1.SPINE10571. [DOI] [PubMed] [Google Scholar]
- 26.Whitmore RG, et al. Patient comorbidities and complications after spinal surgery: a societal-based cost analysis. Spine (Phila Pa 1976) 2012;37(12):1065–71. doi: 10.1097/BRS.0b013e31823da22d. [DOI] [PubMed] [Google Scholar]
- 27.Godil SS, et al. Comparative effectiveness and cost-benefit analysis of local application of vancomycin powder in posterior spinal fusion for spine trauma: clinical article. J Neurosurg Spine. 2013;19(3):331–5. doi: 10.3171/2013.6.SPINE121105. [DOI] [PubMed] [Google Scholar]
- 28.Theologis AA, et al. Local intrawound vancomycin powder decreases the risk of surgical site infections in complex adult deformity reconstruction: a cost analysis. Spine (Phila Pa 1976) 2014;39(22):1875–80. doi: 10.1097/BRS.0000000000000533. [DOI] [PubMed] [Google Scholar]
- 29.Patil CG, et al. Inpatient complications, mortality, and discharge disposition after surgical correction of idiopathic scoliosis: a national perspective. Spine J. 2008;8(6):904–10. doi: 10.1016/j.spinee.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Hostin RA, et al. What is the most expensive cause for readmission following adult spinal deformity surgery? Spine J. 2015;15(10):S193. [Google Scholar]
- 31.••.Daniels AH, et al. Hospital charges associated with “never events”: comparison of anterior cervical discectomy and fusion, posterior lumbar interbody fusion, and lumbar laminectomy to total joint arthroplasty. J Neurosurg Spine. 2016;1–5. A retrospective analysis of larger inpartient database estimating the cost of ‘never events’ associated with spine, knee, and hip surgery using the ICD9-CM codes. Despite the low incidence rate of complications (DVT, PE, and SSI), costs for patients with complications increased by a factor of 1.8 t o 4.3.
- 32.Nandyala SV, et al. Cost analysis of incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2014;39(17):E1042–51. doi: 10.1097/BRS.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 33.Ambrossi GLG, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery. 2009;65(3):574–8. doi: 10.1227/01.NEU.0000350224.36213.F9. [DOI] [PubMed] [Google Scholar]
- 34.Adogwa O, et al. Cost per quality-adjusted life year gained of revision neural decompression and instrumented fusion for same-level recurrent lumbar stenosis: defining the value of surgical intervention: clinical article. J Neurosurg Spine. 2012;16(2):135–40. doi: 10.3171/2011.9.SPINE11308. [DOI] [PubMed] [Google Scholar]
- 35.Dekutoski MB, et al. Surgeon perceptions and reported complications in spine surgery. Spine. 2010;35(9S):S9–21. doi: 10.1097/BRS.0b013e3181d830de. [DOI] [PubMed] [Google Scholar]
- 36.Cowper DC, et al. Using administrative databases for outcomes research: select examples from VA Health Services Research and Development. J Med Syst. 1999;23(3):249–59. doi: 10.1023/A:1020579806511. [DOI] [PubMed] [Google Scholar]
- 37.Linville DA, et al. Complications in the adult spinal deformity patient having combined surgery: does revision increase the risk? Spine. 1999;24(4):355–63. doi: 10.1097/00007632-199902150-00012. [DOI] [PubMed] [Google Scholar]
- 38.Parker SL, et al. Post-operative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): literature review and cost analysis. Minim Invasive Neurosurg. 2011;54(1):33–7. doi: 10.1055/s-0030-1269904. [DOI] [PubMed] [Google Scholar]
- 39.Parker SL, et al. Factors influencing 2-year health care costs in patients undergoing revision lumbar fusion procedures: clinical article. J Neurosurg Spine. 2012;16(4):323–8. doi: 10.3171/2011.12.SPINE11750. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 26.8 kb)


