Abstract
The atlas is subject to fracture under axial load, often due to traumatic injuries such as shallow dives and automobile accidents. These fractures account for 2–13 % of injuries to the cervical spine [Marcon RM et al. Clinics (Sao Paulo) 68(11):1455-61, 2013]. Fractures of the C1 vertebra are often difficult to diagnose, as there is often no neurological deficit or easily identifiable findings on radiographs. However, injuries to the atlas can be associated with vertebral artery injury and atlantoaxial or atlanto-occipital instability, making prompt and accurate diagnosis imperative. A detailed understanding of the anatomy, inherent stability, and common injury patterns is essential for any surgeon treating spinal trauma. This chapter explores the diagnosis and management of C1 fractures, as well as outcomes after treatment.
Keywords: C1, Jefferson fracture, Atlas fracture, Atlantoaxial instability, Transverse odontoid ligament, Upper cervical spine
Introduction
Atlas fractures account for 2–13 % of acute injuries of the cervical spine and 1–2 % of all spinal injuries [1, 2••]. Atlas injuries occur due to a traumatic axial load and are typically associated with other damage to the upper cervical spine. In addition, violent rotational forces on the head and neck may infrequently cause atlas fractures. Classically, patients presenting with fractures of the atlas have sustained an injury due to diving into shallow water, falling, or a motor vehicle accident [3]. There appears to be a male preponderance, with men accounting for 57–69 % of all cases [2••]. This imbalance is reversed in the elderly where 52 % of patients are female, while in younger patients males account for upwards of 70 % of cases [2••]. Pediatric patients with C1 fractures are rare, although the mortality rate among infants with this injury is approximately 16 % [2••]. Overall, a bimodal distribution is seen, with individuals aged in their mid-twenties and between 80–84 most at-risk for C1 fractures; however, the mean age of diagnosis is 64 years and nearly three-quarters of cases occur in patients over 50 years of age [2••, 3].
Relevant anatomy
The atlas, or C1 vertebra, sits just inferior to the occiput and through its articulations with C2 and the occipital condyles joins the skull to the spine. This allows for lateral and vertical mobility of the head and upper spine. C1 lacks a vertebral body, consisting instead of a posterior and anterior arch that encircles the spinal cord, mostly posterior to the dens [4]. The atlas has two lateral masses with concavities that match the condyles of the occiput, forming the occipito-cervical articulations and allowing for movement of the skull.
The C1-2 joint is highly mobile, with the dens of the axis secured to the anterior arch of the atlas by the transverse odontoid ligament. At the anterior aspect of the ring, the joint is secured by the anterior atlantoaxial ligament. Posteriorly, the ring of the atlas is connected to the C2 by the posterior atlantoaxial ligament. The dens articulates with the atlas via a facet on the posterior aspect of the anterior ring of the atlas, retained by the transverse ligament, providing the head with approximately 50 % of its lateral rotation.
The vertebral arteries pass through the transverse foramina of the atlas. They are subject to blunt vertebral arterial injury (BVAI) in cases of traumatic subluxation or fractures of the C1/C2 foramina. Most cases of BVAI remain asymptomatic and are often overlooked. Nevertheless, occlusion of bilateral or dominant vertebral arteries can be devastating and the mortality rate in patients with BVAI without a neurological event is around 7 %. The traditional diagnostic tool for vertebral injury is digital subtraction angiography; however, CT angiography has also been demonstrated as a viable means of identifying symptomatic BVAI in the upper cervical spine [5]. If there is concern for vertebral artery injury, it is the authors’ practice to obtain CT angiogram and treatment is based on patient comorbidities with neurosurgery follow-up. Typically, these cases are managed with 3 months of acetylsalicylic acid. Heparin and antiplatelet agents have been used for patients with asymptomatic BVAI as well. While these therapies appear to be effective, many trauma patients have multiple organ system injuries and anticoagulation would increase the risk of hemorrhagic complications. Therefore, aspirin is preferred at our institution. No monitoring is required unless indicated based on the injury pattern and comorbidities.
Injury patterns
Atlas fractures can involve various and multiple structures and follow a number of patterns. Burst, lateral mass, and laminar fractures are all recognized injuries. Single fractures involving the ring are highly unlikely, and a ring disruption typically accompanies any fracture [6, 7]. Atlanto-occipital dislocations (AOD), commonly called internal decapitations, are another fracture pattern with C1 involvement [8]. The Jefferson burst fracture, named after British neurosurgeon Sir Geoffrey Jefferson, was first reported in 1920 and typically presents as four bony fractures of the anterior and posterior arches of C1 following hyperextension or excessive axial loading of the atlas [6]. This type of fracture is not usually associated with neurological deficits due to the tendency of the fragments to spread out away from the spinal canal.
Atlas fractures may often involve trauma to the axis as well. C2 fractures can be categorized using either the Anderson and D’Alonzo classification or the Roy-Camille classification. Anderson and D’Alonzo recognized three types of odontoid fractures. Type I odontoid fractures involve the dens superior to the cruciform ligament and are considered to be stable. Type II is the most prevalent odontoid fracture pattern, identifiable by a break at the base of the dens, below the cruciform ligament. Type II fractures have a greater risk of nonunion and are unstable. Type III fractures move through the base of the odontoid and into the lateral masses of the axis. Due to a more extensive blood supply and larger surface area, these fractures are the most likely to heal. Moreover, they are stable when not significantly displaced. The Roy-Camille system offers an alternative classification with three types based on the direction of the fracture line. Types I and II are categorized by oblique fractures which slope anteriorly and posteriorly, respectively. The third type includes horizontal fracture lines with displacement of the dens either anteriorly or posteriorly.
Diagnosis
Atlas fractures can pose numerous difficulties for diagnosis. Classically, patients with C1 fractures present with pain in the upper neck and a history of trauma to the top of the head such as diving into shallow water or automobile collision [7]. While lower cervical injuries are more easily identified radiologically and likely to present with neurologic compromise, isolated C1 fractures can be harder to see on plain film radiographs and less likely to cause neurological deficits.
Definitive diagnosis of an isolated fracture often requires computed tomography (CT) scans, while ligamentous injury is most readily identified with magnetic resonance imaging (MRI) [9]. Ligamentous instability can be recognized on open-mouth view radiographs displaying lateral mass displacement of 7 mm or greater. The atlanto-dens interval (ADI), defined as the distance between the atlas and the dens, can also be used as a marker for ligamentous instability. The normal ADI is less than 3 mm, and a larger distance indicates a higher degree of ligamentous injury [10]. The use of CT and MRI allow for more complete assessment of the bony injury and more accurate assessment of the ligamentous structures associated with the atlas [3, 7, 9]. Identifying fractures is even more difficult in pediatric patients, because the C1 body may not be visualized radiographically until patients reach 1 year of age and does not fuse until 4 years of age [11]. Diagnosis is further stymied by congenital abnormalities that present with similar radiographic findings but do not cause cervical instability [12, 13]. It is therefore vital to exclude atlantoaxial and atlanto-occipital instability using radiographic imaging for accurate diagnosis and treatment.
Once identified, atlas fractures can be classified by the fracture pattern (Table 1). Type I fractures are isolated to the anterior or posterior arch, a rare injury with intact transverse ligament. Type II injuries, also known as Jefferson fractures, are burst fractures with bilateral fractures of the anterior and posterior arch of C1. Type III fractures involve the lateral mass. Jefferson fractures and lateral mass fractures may be in isolation or may be associated with significant ligamentous disruption.
Table 1.
Types of Jefferson burst fractures
| Classification of fracture | Mechanism of injury | Diagnostic findings |
|---|---|---|
| Type I | Axial load and flexion or extension | Isolated fracture of the anterior or posterior arch |
| Type II | Axial load | Bilateral fractures of anterior and posterior arch |
| Type III | Axial load and rotation | Lateral mass fracture |
| Atlanto-occipital dislocation (AOD) | Distraction and hyperextension or hyperflexion of atlanto-occipital joint | Severe disruption of ligaments between base of skull and atlas |
Principles of treatment
The treatment of atlas fractures remains controversial, in part due to the frequent occurrence of other cervical injuries in association with these injuries. No standards or guidelines for treatment of C1 fractures alone or in combination with other cervical spine injuries have been developed [3, 14]. Instead, treatment recommendations for isolated C1 fractures and combined C1–C2 fractures are typically based on a group of case series [3]. Depending on the extent of trauma, nonoperative treatment consisting of external orthoses is often effective if the fracture is stable. Most isolated C1 fractures and stable C1–C2 fractures are managed with use of a rigid collar, a halo-thoracic brace, or sterno-occipitomandibular immobilization [3]. External immobilization is recommended for combined C1–C2 fractures unless instability is evident on upright and supine radiographs while the patient is wearing a brace [3]. Surgery is typically reserved for more complex cases, such as AODs, or when instability or neurologic compromise is present. Stability of the atlantoaxial joint is determined largely by the presence or absence of an intact transverse ligament, and the degree of anterior arch fracture displacement [11]. An intact ligament may be managed with the use of a soft or hard collar, while a ruptured ligament without a bony avulsion component may require a combination of traction, a halo vest, or surgery if refractory to nonoperative treatment. In the majority of cases, a hard collar is adequate treatment. Some clinicians prefer a halo vest or Minerva body jacket in order to prevent further trauma to the injured vertebra by limiting cervical mobility [7, 11].
Operative intervention for C1 fractures is rarely needed but may be required in cases of significant instability in the upper cervical spine. Surgical fixation typically involves instrumentation of C1 and C2 and may extend to the occiput [7]. For more extensive injuries of the cervical spine or those that include lower cervical vertebrae as well, the fusion can be extended. For combined C1–C2 fractures, operative intervention consisting of instrumentation and fusion should be considered for type III hangman’s fractures and the concurrent presence of a type II odontoid fracture in an elderly patient [3, 7, 11].
Surgical indications
Surgical treatment for isolated axis fractures is rarely indicated, as collar immobilization is typically adequate. The primary consideration for surgery is instability, typically assessed using mobility on flexion-extension films. Using the Anderson and D’Alonzo classification, type I and III odontoid process fractures are typically considered stable while type II, the most common variant, is unstable. Another objective surgical indication includes a confirmed (i.e., using MRI) midsubstance transverse ligament disruption and the presence of atlanto-occipital instability. A relative indication for surgery that is not universally accepted is the presence of bilateral displacement of the lateral masses adding up to greater than 6.9 mm on open-mouth radiographs [9, 12]. An offset of this magnitude suggests rupture of the transverse ligament of the atlas and associated instability. An offset of both lateral masses of the atlas over the axis ranging from 3 to 9 mm may also be indicative of a Jefferson burst fracture [15]. While these injuries may be initially treated with rigid immobilization, patients should be followed for continued pain and instability. Flexion-extension views can be obtained 3 months after injury to assess for any remaining pathologic motion indicative of persistent instability. If radiographic evidence of instability persists, internal fixation of C1–2 may be performed to mitigate neck pain and risk of serious injury to the brainstem and spinal cord (Fig. 1) (Fig. 2).
Fig. 1.
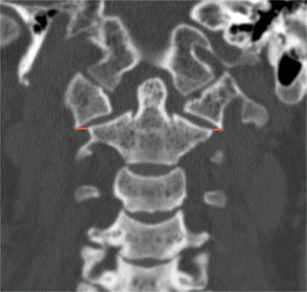
Coronal CT image demonstrating measurement technique for lateral mass displacement. Reprinted with permission from Radcliff et al. [9]
Fig. 2.

Case example demonstrating preoperative CT images (top) as well as intraoperative and postoperative radiographs (bottom)
Atlanto-occipital displacement injuries are some of the more unstable injury patterns associated with C1 fractures. These are caused by traumatic hyperflexion or extension of the neck, which severs the posterior longitudinal ligament as well as the bilateral alar ligaments. The capsular and accessory ligaments can also be disrupted [16]. The instability caused by dislocation or subluxation of the atlanto-occipital joint may result in severe damage to the spinal cord and often death. Upwards of 30 % of traffic collision deaths are due to AODs [8, 16]. An atlanto-occipital displacement with a concomitant C1 fracture may be diagnosed on CT scans, which show a basion-dens interval (BDI), the distance between the basion and the tip of the dens, exceeding 10–12 mm. Atlanto-occipital dissociation injuries may also be diagnosed when the occipital condyle-C1 interval (CCI) exceeds 4 mm [8, 15]. Pang et al. reviewed the CCI and other radiographic landmarks and found that, for the evaluation and diagnosis of AOD, the CCI is the most direct tool to measure displacement in AOD and is especially useful in pediatric injuries [17]. An AOD requires emergent surgical fixation to minimize the risks of progressive neurologic injury and even mortality. Additionally, presurgical external fixation with a halo vest is recommended to minimize other complications. Axial traction and rigid cervical collars are contraindicated because of potential to distract the injured joint further [8]. Patients suffering an AOD often present with concomitant injuries to the lower cervical spine and should undergo a thorough clinical evaluation. In the event of trauma to the occiput or other vertebra, internal fixation is required and should extend to the most inferior affected vertebra [18].
As a general rule, purely bony injuries to the atlas can be successfully treated with immobilization. Reserving surgical stabilization for patients who have clear ligamentous injuries with obvious instability in addition to bony injury appears to be an effective and safe treatment strategy [18, 19•].
Management techniques
Nonoperative management
Nonoperative management remains the mainstay of treatment for C1 fractures. Isolated atlas fractures can be effectively managed with 8 to 12 weeks of external immobilization of the craniocervical junction [3]. Collar immobilization or cervical traction for this period of time is usually sufficient to allow for proper healing; however, the type of orthosis required varies [3, 20]. Nonoperative treatment typically consists of external immobilization through use of a rigid collar, halo vest, or Minerva jacket [20]. Soft collars are inadequate for immobilization and often result in worsening pain to the patient with neck motion as well as further fracture displacement. Following immobilization, dynamic imaging studies such as flexion-extension films should be ordered to rule out late instability [3].
In the absence of significant displacement, C1 fractures can often be treated with a period of rigid collar immobilization. In cases with more significant fracture displacement, more rigid immobilization with the halo vest or Minerva jacket may be required. The halo vest is more rigid than the Minerva jacket, providing greater restriction of the C1–2 joint. Flexion and extension of the upper cervical spine is diminished by as much as 75 % when a halo vest is employed. The greater rigidity of the halo orthosis also restricts more lateral movement of the atlantoaxial joint when compared with the Minerva jacket [21]. For this reason, the halo vest is the preferred option for upper cervical injuries [22]. With injuries extending to the mid and lower cervical spine, thermoplastic Minerva jackets offer greater comfort to patients, fewer complications, and can provide effective stabilization [22].
Despite its superiority over the Minerva jacket, the halo orthosis has significant potential complications. Halo ring slippage, loosening, infection, and irritation and discomfort are common [7, 20]. Halo vest immobilization (HVI) failure rates reported in the literature reach as high as 85 % [23]. Pediatric patients in particular are subject to complications with use of halo vests [7].
Such orthoses may not be appropriate for patients who are morbidly obese, or who lack the necessary neurological function to avoid the formation of decubitus ulcers [7]. Instead, cranial traction or rigid collars should be supplemented in these cases with vigilant nursing care [24]. Rigid collars avoid many of the potential complications of more restrictive orthoses at the cost of stability. Thus, patients must be simultaneously assessed for their ability to comply with various immobilization methods as well as their required degree of stabilization. Occasionally, orthotic stabilization will result in nonunion or continued instability, in which case surgical intervention is necessary. Stability is assessed after an appropriate course of immobilization, with flexion-extension radiographs. Greater than a 5 mm increase in the atlanto-dens interval is often considered unstable and may require surgical intervention.
Operative techniques
While there is no consensus on a single best operative technique, there are numerous options for surgical stabilization reported in the literature. Depending on the case, plain radiography, intraoperative fluoroscopy, CT imaging, or 3D navigation may aid in the proper placement of instrumentation [25]. Currently, the choice of surgical approach and instrumentation is determined largely by the presence of associated injuries to the cervical spine. The degree of associated trauma will therefore determine the appropriate course of treatment.
The incidence rate of C2 fractures concurrent with C1 fractures is approximately 41–44 % [7]. Upper cervical fractures with isolated C1–C2 instability can be effectively treated with C1–C2 fusion. However, if the C1 injury is a burst fracture, fixation should attempt to bring together the C1 lateral masses followed by fixation to C2. Alternatively, instrumentation can span from the occiput to C2 [7]. While odontoid fractures associated with C1 fractures typically may be managed with external immobilization alone, type II odontoid fractures, especially in the elderly, often are optimally managed with surgical intervention [7, 26, 27].
Atlantoaxial stabilization can be achieved via the use of the Goel-Harms technique, using polyaxial screw fixation of the lateral masses of C1 and pedicle screw or pars fixation of C2 [28•]. The procedure begins with a midline incision descending from below the inion to just superior to the sub-axial cervical spine. Next, a retractor is used to separate the muscles of the splenius capitis and dissection continues until the posterior arch of C1 and the lamina of C2 are visible. Following adequate exposure of the bony landmarks, the central and medial sections of the lateral mass are skeletonized in order to identify the C1 lateral mass entry point, taking care to avoid the vertebral artery. During this step, the venous plexus is subjected to cauterization, tamponade, and application of hemostatic agents. The C2 nerve root can be retracted caudally. The entry point is made 3–4 mm lateral to the medial aspect of the C1 lateral mass employing a matchstick or awl bit. Next, the lateral mass is cannulated with a drill aimed approximately 20° rostral with a minimal medial trajectory. A partially threaded screw is placed with only the smooth portion of the instrument abutting the C2 nerve root. Screws are then placed in the C2 pars or pedicle, with the entry point of the pars screw a few millimeters rostral to the C2/C3 joint and a slightly rostral and lateral entry point to that of the pars screw for a C2 pedicle screw. Once the screws are securely placed, their alignment is assessed via lateral and AP fluoroscopy. Upon confirmation of the proper placement, rods are cut and affixed to the screw tulip heads using set screws. To help achieve arthrodesis, the posterior C1 arch, the C2 lamina, and the C1/C2 joint space are decorticated and a bone graft is placed [27]. This approach has been reported with a fusion rate as high as 100 % and with few postoperative complications [28•, 29, 30].
An alternative method of stabilizing the C2–C1 articulation is the Magerl technique. This technique often requires a separate percutaneous placement of the drill and screw in order to achieve a shallower trajectory towards the C1–2 joint. As with the Harms technique, a separate midline incision is made and the C2 lateral mass and pars are exposed. This allows orientation of the C2 pars which allows drill guidance using lateral fluoroscopy across the C2, C1 joint. After drilling, screws are inserted bilaterally crossing the facet joint of C1–2 [31, 32].
Complications
Complications in the management of C1 fractures range from minor discomfort to death. The primary concern with C1 fractures is establishing and maintaining cervical stability. Atlanto-occipital and atlantoaxial instability threatens the brainstem and spinal cord, potentially causing myelopathy and even mortality. Additional issues may arise depending on the management techniques used to address the injuries.
Conservative management with external immobilization is predominantly associated with cervical discomfort. Patients may also experience fracture nonunion, contact ulcers, and infection depending on the orthosis used and patient-specific factors. The halo vest in particular is associated with discomfort and the potential for pin site infections [20, 33]. Elderly patients especially do poorly with halo vest immobilization. The Minerva jacket and rigid collars, while less likely to result in such complications, are also less rigid and may not provide sufficient stability in all cases [7].
Surgical complications from the procedures outlined above are, for the most part, nonspecific to C1 fractures. Infection of the surgical site is always a serious concern. Dislodged or misplaced hardware can lead to pain, instability, and neurological deficits. Furthermore, the misplacement or migration of instrumentation may result in vertebral arterial injury [34]. Intraoperative imaging such as fluoroscopy is useful in order to avoid misplacement of screws and avoid damage to the vertebral artery [25, 30]. Reduced bone density and osteoporosis are also potential sources of hardware failure in the upper cervical spine.
A complication unique to the atlantoaxial joint is the cock-robin deformity resulting from a sagittal split fractures involving the lateral mass. In this situation, the C1 lateral mass subluxes laterally, allowing the occipital condyle to settle onto the lateral mass of C2. This is often a complication of nonoperative care and requires occipito-cervical reconstructive surgery [35]. This deformity increases the difficulty of corrective surgery due to the close proximity of the vertebral artery [36]. Loss of mobility is another concern. Patients who have undergone fixation from C1–2 have rotational mobility at the joint reduced by half. Occiput to C2 fixation will also produce a 50 % diminished range flexion and extension [36].
Future directions
The optimal treatment for C1 fractures remains ambiguous, and the orthoses prescribed for C1 fractures also differ based on surgeon and patient preference. Indications for surgery are often debated, and the approaches and instrumentation vary from practice to practice. This variation in methodology for surgical and conservative management is quite common and unfortunately impedes systematic analyses and consensus agreements. Further research is recommended to establish standards and guidelines for treatment [3].
Conclusions
C1 fractures are a complex group of upper cervical injuries, and diagnosis and treatment thereof requires a holistic approach. The context of any concurrent spinal trauma in addition to patients’ overall health (e.g., obesity, myelopathy, ability to comply with treatment, osteoporosis) will dictate treatment methods. While the majority of these injuries can be treated with nonoperative immobilization, certain fracture characteristics will require surgical fixation or fusion. The surgeon must be aware of the fracture patterns that require more extensive stabilization and follow patients closely for signs of instability and deformity after nonoperative management.
Case example
A 72-year-old female presents to the trauma bay after losing her balancing and falling from standing down a flight of stairs. On CT of the head and cervical spine, a C1 ring fracture is visible (top left). MRI angiography of the neck similarly demonstrates a fracture of the anterior and posterior arches of C1 on the left side with mild displacement. The patient is treated with physical therapy and fitted for a Miami J collar. Five months later, the patient is diagnosed with spinal stenosis and incomplete healing of fracture (top right). She then undergoes posterior occiput to C4 fusion (bottom left and bottom right).
Compliance with ethical standards
Conflict of interest
Loren B. Mead II and Jonathan Krystal declare that they have no conflict of interest. Paul W. Millhouse reports financial relations with Globus Medical, outside the submitted work. Alexander R. Vaccaro reports other from Replication Medica, personal fees from DePuy, personal fees from Medtronics, personal fees from Stryker Spine, personal fees and other from Globus, other from Paradigm Spine, personal fees and other from Stout Medical, other from Progressive Spinal Technologies, other from Advanced Spinal Intellectual Properties, personal fees from Aesculap, other from Spine Medica, other from Computational Biodynamics, other from Spinology, other from In Vivo, other from Flagship Surgical, other from Cytonics, other from Bonovo Orthopaedics, other from Electrocore, other from Gamma Spine, other from Location Based Intelligence, other from FlowPharma, personal fees from Gerson Lehrman Group, personal fees from Guidepoint Global, personal fees from Medacorp, other from Rothman Institute and Related Properties, other from AO Spine, personal fees and other from Innovative Surgical Design, other from Association of Collaborative Spine Research, personal fees from Orthobullets, personal fees from Thieme, personal fees from Jaypee, personal fees from Elsevier, personal fees from Taylor Francis/Hodder and Stoughton, personal fees from Expert Testimony, personal fees from Ellipse, other from Vertiflex, other from Avaz Surgical, other from Clinical Spine Surgery, other from Spine Journal, other from Prime Surgeons, outside the submitted work.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Cervical Injuries and Treatment
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Marcon RM, Cristante AF, Teixeira WJ, Narasaki DK, Oliveira RP, De barros filho TE. Fractures of the cervical spine. Clinics (Sao Paulo) 2013;68(11):1455–1461. doi: 10.6061/clinics/2013(11)12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.••.Matthiessen C, Yohan R. Epidemiology of atlas fractures—a national registry-based cohort study of 1,537 cases. Spine J. 2015;15(11):2332–2337. doi: 10.1016/j.spinee.2015.06.052. [DOI] [PubMed] [Google Scholar]
- 3.Kakarla UK, Chang SW, Theodore N, Sonntag VK. Atlas fractures. Neurosurgery. 2010;66(3 Suppl):60–67. doi: 10.1227/01.NEU.0000366108.02499.8F. [DOI] [PubMed] [Google Scholar]
- 4.Jefferson G. Fracture of the atlas vertebra: report of four cases, and a review of those previously recorded. Br J Surg. 1920;7(27):407–422. doi: 10.1002/bjs.1800072713. [DOI] [Google Scholar]
- 5.Payabvash S, McKinney AM, McKinney ZJ, Palmer CS, Truwit CL. Screening and detection of blunt vertebral artery injury in patients with upper cervical fractures: the role of cervical CT and CT angiography. Eur J Radiol. 2014;83(3):571–577. doi: 10.1016/j.ejrad.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 6.Hadley MN, Curtis DA, Browner CM, Sonntag VKH. Acute traumatic atlas fractures: management and long term outcome. Neurosurgery. 1988;23(1):31–35. doi: 10.1227/00006123-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Garrett M, Consiglieri G, Kakarla UK, Chang SW, Dickman CA. Occipitoatlantal dislocation. Neurosurgery. 2010;66(3):A48–A55. doi: 10.1227/01.NEU.0000365802.02410.C5. [DOI] [PubMed] [Google Scholar]
- 8.Gray H, Warren HL, Inc Bartleby.com . Anatomy of the human body. New York: Bartleby.com; 2000. [Google Scholar]
- 9.Radcliff KE, Sonagli MA, Rodrigues LM, Sidhu GS, Albert TJ, Vaccaro AR. Does C1 fracture displacement correlate with transverse ligament integrity? Orthop Surg. 2013;5(2):94–99. doi: 10.1111/os.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson RS, Banit DM, Rhyne AL, Darden BV. Upper cervical spine injuries. J Am Acad Orthop Surg. 2002;10(4):271–280. doi: 10.5435/00124635-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Lee C, Woodring JH. Unstable Jefferson variant atlas fractures: an unrecognized cervical injury. AJNR Am J Neuroradiol. 1991;12(6):1105–1110. [PMC free article] [PubMed] [Google Scholar]
- 12.Gehweiler J, Daffner RH, Roberts L. Malformations of the atlas vertebra simulating the Jefferson fracture. Am J Roentgenol. 1983;140(6):1083–1086. doi: 10.2214/ajr.140.6.1083. [DOI] [PubMed] [Google Scholar]
- 13.de Zoete A, Langeveld UA. A congenital anomaly of the atlas as a diagnostic dilemma: a case report. J Manipulative Physiol Ther. 2007;30(1):62–64. doi: 10.1016/j.jmpt.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Hadley MN. Isolated fractures of the atlas in adults. Neurosurg. 2002;50:S120–S124. doi: 10.1097/00006123-200203001-00020. [DOI] [PubMed] [Google Scholar]
- 15.Chaput CD, Walgama J, Torres E, Dominguez D, Hanson J, Song J, et al. Defining and detecting missed ligamentous injuries of the occipitocervical complex. Spine. 2011;36(9):709–714. doi: 10.1097/BRS.0b013e3181de4ec1. [DOI] [PubMed] [Google Scholar]
- 16.Deliganis AV, Mann FA, Grady MS. Rapid diagnosis and treatment of a traumatic atlantooccipital dissociation. Am J Roentgenol. 1998;171(4):986. doi: 10.2214/ajr.171.4.9762980. [DOI] [PubMed] [Google Scholar]
- 17.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation–part 2: the clinical use of (occipital) condyle-c1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery. 2007;61(5):995–1015. doi: 10.1227/01.neu.0000303196.87672.78. [DOI] [PubMed] [Google Scholar]
- 18.Joaquim AF, Ghizoni E, Tedeschi H, Lawrence B, Brodke DS, Vaccaro AR, et al. Upper cervical injuries—a rational approach to guide surgical management. J Spinal Cord Med. 2014;37(2):139–151. doi: 10.1179/2045772313Y.0000000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.•.Joaquim AF, Ghizon E, Tedeschi H, Yacoub ARD, Brodke DS, Vaccaro AR, et al. Upper cervical injuries: clinical results using a new treatment algorithm. J Craniovertebral Junction & Spine. 2015;6(1):16–20. doi: 10.4103/0974-8237.151585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee TT, Green BA, Petrin DR. Treatment of stable burst fracture of the atlas (Jefferson fracture) with rigid cervical collar. Spine. 1998;23(18):1963–1967. doi: 10.1097/00007632-199809150-00008. [DOI] [PubMed] [Google Scholar]
- 21.Lauweryns P. Role of conservative treatment of cervical spine injuries. Eur Spine J. 2010;19(Suppl 1):23–26. doi: 10.1007/s00586-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benzel EC, Hadden TA, Saulsbery CM. A comparison of the Minerva and halo jackets for stabilization of the cervical spine. J Neurosurg. 1989;70(3):411–414. doi: 10.3171/jns.1989.70.3.0411. [DOI] [PubMed] [Google Scholar]
- 23.Shin JJ, Kim SJ, Kim TH, Shin HS, Hwang YS, Park SK. Optimal use of the halo-vest orthosis for upper cervical spine injuries. Yonsei Med J. 2010;51(5):648–652. doi: 10.3349/ymj.2010.51.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benzel EC, Larson SJ, Kerk JJ, Millington PJ, Novak SM, Falkner RH, et al. The thermoplastic Minerva body jacket: a clinical comparison with other cervical spine splinting techniques. J Spinal Disord. 1992;5(3):311–319. doi: 10.1097/00002517-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Costa F, Ortolina A, Attuati L, Cardia A, Tomei M, Riva M, et al. Management of C1–2 traumatic fractures using an intraoperative 3D imaging-based navigation system. J Neurosurg Spine. 2014;22(2):128–133. doi: 10.3171/2014.10.SPINE14122. [DOI] [PubMed] [Google Scholar]
- 26.Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9(1):56–59. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo Q, Deng Y, Wang J, Liang W, Lu X, Guo X, et al. Comparison of clinical outcomes of posterior C1-2 temporary fixation without fusion and C1-2 fusion for fresh odontoid fractures. Neurosurg. 2015;4:77–83. doi: 10.1227/NEU.0000000000001006. [DOI] [PubMed] [Google Scholar]
- 28.•.Sattarov K, Skoch J, Abbasifard S, Patel AS, Avila MJ, Walter CM, et al. Posterior atlantoaxial fixation: a cadaveric and fluoroscopic step-by-step technical guide. Surg Neurol Int. 2015;6(4):S244–S247. doi: 10.4103/2152-7806.156611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurg. 2002;51(6):1351–1357. [PubMed] [Google Scholar]
- 30.SV Patkar. “Sub-Facetal C2 body screw in posterior fixation (Goel-Harm’s technique) of the atlanto-axial joint avoiding the vertebral artery.” The Internet Journal of Neurosurgery 10, no. 1. Accessed September 20, 2015. http://print.ispub.com/api/0/ispub-article/14745.
- 31.Mummaneni PV, Haid RW. Atlantoaxial fixation: overview of all techniques. Neurol India. 2005;53(4):408–415. doi: 10.4103/0028-3886.22606. [DOI] [PubMed] [Google Scholar]
- 32.Floyd T, Grob D. Translaminar screws in the atlas. Spine. 2000;25(22):2913–2915. doi: 10.1097/00007632-200011150-00013. [DOI] [PubMed] [Google Scholar]
- 33.Koller H, Resch H, Tauber M, Zenner J, Augat P, Penzkofer R, et al. A biomechanical rationale for C1-ring osteosynthesis as treatment for displaced Jefferson burst fractures with incompetency of the transverse atlantal ligament. Eur Spine J. 2010;19(8):1288–1298. doi: 10.1007/s00586-010-1380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muratsu H, Doita M, Yanagi T, Sekiguchi K, Nishida K, Tomioka M, et al. Cerebellar infarction resulting from vertebral artery occlusion associated with a Jefferson fracture. J Spinal Disord Tech. 2005;18(3):293–296. [PubMed] [Google Scholar]
- 35.Bransford R, Chapman JR, Bellabarba C. Primary internal fixation of unilateral C1 lateral mass sagittal split fractures: a series of 3 cases. J Spinal Disord Tech. 2011;24(3):157–163. doi: 10.1097/BSD.0b013e3181e12419. [DOI] [PubMed] [Google Scholar]
- 36.Shatsky J, Bellabarba C, Nguyen Q, Bransford RJ. A retrospective review of fixation of C1 ring fractures—does the transverse atlantal ligament (TAL) really matter? Spine J. 2015 doi: 10.1016/j.spinee.2015.11.041. [DOI] [PubMed] [Google Scholar]


