Abstract
Many studies have demonstrated the beneficial effects that pharmacist-provided patient care services can have on patient health outcomes. However, the effectiveness of patient care services delivered by pharmacists in community pharmacy settings, where organizational barriers may affect service implementation or limit effectiveness, remains unclear. The authors systematically reviewed the literature on the effectiveness of pharmacist-delivered patient care services in community pharmacy settings in the United States. Of the 749 articles retrieved, 21 were eligible for inclusion in the review. Information concerning 134 outcomes was extracted from the included articles. Of these, 50 (37.3%) demonstrated statistically significant, beneficial intervention effects. The percentage of studies reporting favorable findings ranged from 50% for blood pressure to 0% for lipids, safety outcomes, and quality of life. Our findings suggest that evidence supporting the effectiveness of pharmacist-provided direct patient care services delivered in the community pharmacy setting is more limited than in other settings.
Keywords: pharmacists, direct patient care, systematic review, community pharmacies
Introduction
Medications play a major role in the management of most chronic illnesses. Recent data from the Centers for Disease Control and Prevention indicate that nearly 50% of all people in the United States report using at least one prescription drug during the past month and more than 10% report using five or more prescription drugs during that time frame (National Center for Health Statistics, 2012). Used appropriately, medications can reduce morbidity and mortality. Unfortunately, medications are not always used appropriately. Several prominent organizations have recognized that medication-related problems plague the U.S. health care system (Institute of Medicine, 2003; Kohn, Corrigan, & Donaldson, 2000; McGlynn et al., 2003). Inappropriate medication use can cause serious harm, including death, and increased health care expenditures (Ernst & Grizzle, 2001; Gurwitz & Rochon, 2002; Hohl et al., 2011; Weingart et al., 2009). Medication nonadherence is also a problem (DiMatteo, Giordani, Lepper, & Croghan, 2002; Krueger, Berger, & Felkey, 2005; Osterberg & Blaschke, 2005). In a review of studies that examined adherence to medications across diverse conditions, DiMatteo (2004) estimated that 21% of patients do not take their medications as prescribed. Rates of nonadherence to medications used to treat asymptomatic conditions, such as hypertension, tend to be even higher (Krueger et al., 2005; Osterberg & Blaschke, 2005). In an attempt to improve the quality of medication use and reduce the risk of adverse events, medication therapy management programs were included as a key benefit when Medicare was expanded in 2003 to include an outpatient prescription drug benefit (S. R. Smith & Clancy, 2006).
Within the health care system, pharmacists are uniquely trained to assist patients and other health care providers deal with issues involving medication management. Over the past 40 years, the role of pharmacists has expanded considerably, moving beyond solely dispensing medications to also include the provision of comprehensive clinical services (Cipolle, Strand, & Morley, 1998). In many settings, interdisciplinary health care teams now include pharmacists who provide expertise concerning medication management issues. Chisholm-Burns et al. (2010) recently conducted a systematic review evaluating the effects that clinical services delivered by pharmacists can have on patient health outcomes. This review identified a total of 298 publications from studies conducted in the United States that evaluated the effects of pharmacist-provided direct patient care services. The reviewed studies provided substantial evidence that pharmacist involvement in direct patient care can have beneficial effects on patient health outcomes. However, only 29 studies reviewed were conducted exclusively in community pharmacy settings, where most patients obtain their prescription medications. Moreover, in the Chisholm-Burns et al. review, studies that were conducted in community pharmacy settings were combined with those conducted in outpatient and ambulatory care settings for all analyses. Therefore, the effectiveness of patient care services delivered by pharmacists in community pharmacy settings remains unclear.
New Contribution
Much of the early work to expand pharmacists’ clinical role has occurred in inpatient and ambulatory care settings within teaching-focused health systems. However, many of the factors that facilitate pharmacist provision of effective direct patient care services in inpatient and ambulatory care settings are rarely present in community pharmacy settings. The dispensing process (i.e., filling prescriptions) drives the workflow in most community pharmacies (Weinberger et al., 2002a). Successfully incorporating high-quality clinical services into the dispensing process is challenging. In addition, community pharmacists usually have access to little clinical information about their patients other than the medications that have been dispensed for them (Cooksey, Knapp, Walton, & Cultice, 2002). Furthermore, although community pharmacists regularly communicate with prescribers, this is usually accomplished by telephone or fax, mediated through support personnel, and often concerns nonclinically oriented tasks such as obtaining refill authorizations. Given the barriers to delivery of direct patient care services in the community pharmacy setting described above, it is reasonable to suspect that the effectiveness of interventions delivered in this setting may differ from those delivered in outpatient and ambulatory care settings. Thus, the objective of this article is to systematically review the literature on the effectiveness of direct patient care services provided by pharmacists in community pharmacy settings in the United States.
Conceptual Framework
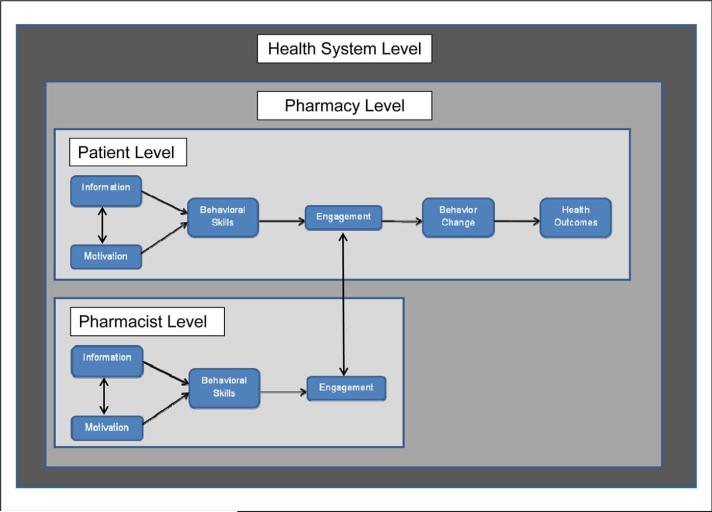
We use an ecological framework based on the information–motivation–behavioral skills (IMB) model to guide this review (Fisher, Fisher, Williams, & Malloy, 1994). Ecological models propose that patient behavior and health outcomes are influenced by both intrapersonal factors and factors operating at multiple levels of the physical and sociocultural environment (e.g., provider characteristics, availability and accessibility of services; Blalock, 2011; Glanz & Bishop, 2010). When evaluating the effectiveness of direct patient care services provided by pharmacists in community pharmacy settings, four levels of the ecological framework are most relevant: the patient level, the pharmacist level, the pharmacy level, and the health system level, including factors that influence either the delivery of services or patient access to care.
Most work on the IMB model has focused on patient-level factors that affect patient engagement in care and the processes through which patient engagement results in recommended behavioral changes and improved health outcomes (Fisher et al., 1994; Kelly, Melnyk, & Belyea, 2012; Osborn & Egede, 2010; Rivet Amico, 2011; Shell, Newman, Perry, & Folsom, 2011; L. R. Smith, Fisher, Cunningham, & Amico, 2012; Zarani, Besharat, Sadeghian, & Sarami, 2010). According to the model, patients are more likely to engage in care when they (a) have adequate information about the services available, (b) are motivated to engage in care, and (c) have the skills required to access the services available. Engagement in care then leads to the adoption and maintenance of recommended behaviors and, ultimately, improved health outcomes.
As shown in Figure 1, we have extended this model by incorporating it into an ecological framework that includes the four levels specified above (i.e., patient, pharmacist, pharmacy, health system). Borrowing from the IMB model, this framework postulates that pharmacists are more likely to engage in the delivery of clinical services when they have the requisite information, motivation, and behavioral skills. Changes in patient health behavior and health outcomes are then influenced by the transaction that occurs when patients seek clinical services from a pharmacist as well as the quality of the services the pharmacist delivers.
Figure 1.
Conceptual model.
Roberts, Benrimoj, Chen, Williams, and Aslani (2008) have identified seven factors that community pharmacists in Australia believe facilitate the successful implementation of clinical services in community pharmacy settings. These include one patient-level factor (i.e., patient receptivity), two pharmacist-level factors (i.e., having a good working relationship with local physicians, and good communication among pharmacy staff), two pharmacy-level factors (i.e., having an appropriate pharmacy layout, and adequate manpower), and two health system factors (i.e., external support to assist with program implementation, and reimbursement for clinical services provided).
At the patient level, little research has been conducted to examine factors that predict patient receptivity to receiving clinical services in the community pharmacy setting. However, in a cross-sectional study involving patients enrolled in a community pharmacy–based diabetes care program, self-reported intention to continue participating in the program was associated with patient beliefs concerning (a) perceived susceptibility to diabetes complications and (b) the extent to which program participation reduced their risk of developing these complications (Pinto, Lively, Siganga, Holiday-Goodman, & Kamm, 2006). Within the IMB model, these types of beliefs are conceptualized as motivating factors. In addition, as described above, other research suggests that patients have limited knowledge of the clinical services that can be provided by community pharmacists (Truong, Layson-Wolf, de Bittner, Owen, & Haupt, 2009). Thus, many patients may lack the information required to access services.
The two pharmacist-level factors identified by Roberts et al. (2008)—that is, having a good working relationship with local physicians and good communication among pharmacy staff—underscore the importance of pharmacists’ communication skills. Finally, the pharmacy and health system–level factors highlight the impact that environmental factors may have on service delivery, even when both the patient and the pharmacist have the information, motivation, and skills required to engage in the care delivery process.
Method
Literature Searches
We used a combination of strategies to identify relevant studies. First, we identified 194 articles that were included in the Chisholm-Burns et al. (2010) systematic review that were classified as having been conducted in the “outpatient/ambulatory care/retail/community setting.” We reviewed each of these articles to identify those that had been conducted exclusively in community pharmacy settings. Second, because the Chisholm-Burns et al. review was limited to studies published prior to February 2009, we performed an updated search to identify articles with publication dates between January 1, 2009 and December 31, 2011. We modeled the updated search after the one used by Chisholm-Burns et al. (2010) but included terms to limit retrieved studies to those that were conducted in community pharmacy settings. The following search terms were used in PubMed/Medline: (community pharmacy OR community pharmacy services [MeSH] OR independent pharmacy OR independent pharmacies OR retail pharmacy OR retail pharmacies OR chain pharmacy OR chain pharmacies) AND (pharmacy OR pharmacist OR pharmacotherapy OR pharmaceutical) AND (cost OR medication OR satisfaction OR outcome OR patient OR safety OR quality of life OR intervention OR economic OR adherence). The search excluded editorials, letters to the editor, and review articles and was limited to articles written in English, and involving human participants. This search yielded a total of 511 articles. Finally, after consultation with a health science librarian, we searched other databases for additional articles. Specifically, we hand-searched the Web of Science (ISI) using articles from the PubMed search as our seed articles and searched Google Scholar using “pharmacist*,” “community practice intervention*,” and “retail pharmacy*” as key words. We also searched the International Pharmaceutical Abstracts using the following search strategy: (pharmacist OR pharmacists AND disease management OR patient compliance OR patient satisfaction OR disease outcome OR quality of life). These additional literature searches yielded 44 articles. Thus, a total of 749 articles were retrieved via the three strategies described above.
Study Selection
At least two members of the research team reviewed the abstract of all articles retrieved to assess eligibility for the full-text review. Three members of the research team (AWR, JCL, SKO) had PharmD degrees, one (SJB) had BS in pharmacy and PhD degrees, and one (TT) was a third-year pharmacy student. To be eligible for inclusion, articles had to (a) report the results of an empirical study; (b) assess an intervention that included pharmacist or pharmacy student involvement in direct patient care; (c) be conducted entirely in a community pharmacy setting, assess services delivered entirely by community pharmacists in another setting (e.g., patient's workplace), or present results in a manner that allowed the effect of community pharmacist involvement to be isolated from other intervention effects; (d) include either a comparison group or a pre-intervention assessment of study outcomes; (e) report at least one patient outcome (e.g., therapeutic outcome, medication adherence, satisfaction); and (f) be conducted in the United States. Articles were excluded during the abstract review process only if both reviewers agreed that the article did not meet these eligibility criteria. When doubt regarding eligibility for inclusion remained after reviewing the abstract, the full text of the article was reviewed. A total of 684 articles were excluded based on review of abstracts and 27 additional articles were excluded based on review of the full-text articles. Average interrater agreement for study exclusion decisions was 93%.
Data Extraction
Data from studies that met our inclusion criteria were extracted from each article by two members of the research team. Each member of the research team extracted data from an approximately equal number of articles. Each reviewer worked independently to extract information from their assigned articles into forms that were part of a Microsoft Access database (Microsoft Inc. 2010, Redmond, WA). Each pair of reviewers then met to resolve discrepancies. Studies were excluded during this stage if both reviewers agreed that they did not meet study inclusion criteria on full-text review.
The following information was extracted from each article: disease/condition targeted, study design, intended length of follow-up, number of individuals enrolled and number who completed planned follow-ups, narrative description of all study groups, demographic characteristics of study participants (e.g., mean age, race, ethnicity, gender), mode of intervention delivery (e.g., face-to-face, telephone), duration of the intervention, number of planned intervention sessions, total planned contact time, and all patient-level outcomes reported with the exception of economic outcomes. We also assessed factors that affect the risk of bias at the study level using criteria recommended by the Agency for Healthcare Research and Quality (e.g., adequacy of randomization; appropriateness of comparison groups; attrition rate; adequacy of statistical analyses, including the use of intention-to-treat principles; statistical power; Viswanathan et al., 2012). We made a global assessment of the risk of bias—high, medium, or low—for each study, rating studies as having “high” risk of bias if we judged that the biases identified were so serious that they invalidated the results of the study (Viswanathan et al., 2012). All members of the research team discussed all studies initially categorized as having a “high” risk of bias to confirm the appropriateness of this rating. We piloted extraction procedures using four articles. Throughout the extraction process, we relied entirely on data reported in the published articles.
Data Synthesis
To minimize the risk of bias, we excluded studies rated as having a high risk of bias. In addition, at the outcome level, we excluded outcomes based on patient self-report measures unless a citation was provided indicating that the measure had been used in previous research. We also excluded the results of redundant analyses that yielded similar results and subgroup analyses unless they were supported by formal tests for interaction effects. Finally, we excluded before–after comparisons when the study included an independent comparison group. In these instances, to avoid inflation of Type I error, we only extracted information pertaining to the between-group differences.
We provide a qualitative synthesis of study findings. We also used a chi-square test to assess whether studies that used a randomized controlled trial (RCT) design were less likely to demonstrate beneficial intervention effects compared with studies that used other designs. We ruled out the possibility of conducting a meta-analysis due to the limited number of studies identified and the heterogeneity among studies in terms of design issues and outcome measures.
Finally, we compared our findings with those reported by Chisholm-Burns et al. (2010) in their review of pharmacist-provided direct patient care services across multiple health care settings. To perform this comparison, we classified the results of outcomes observed in the studies included in our review using the same classification system used in the previous review. These categories are
Favorable: Defined as statistically significant beneficial effects associated with pharmacist-provided care on all measures of the outcome
Not favorable: Defined as statistically significant beneficial effects associated with nonpharmacist-provided care on all measures of the outcome
Mixed: Defined as statistically significant beneficial effects associated with pharmacist-provided care on some, but not all, measures of the outcome
No effect: Defined as no statistically significant differences observed
Unclear: Used when insufficient information was available to classify intervention effectiveness
Results
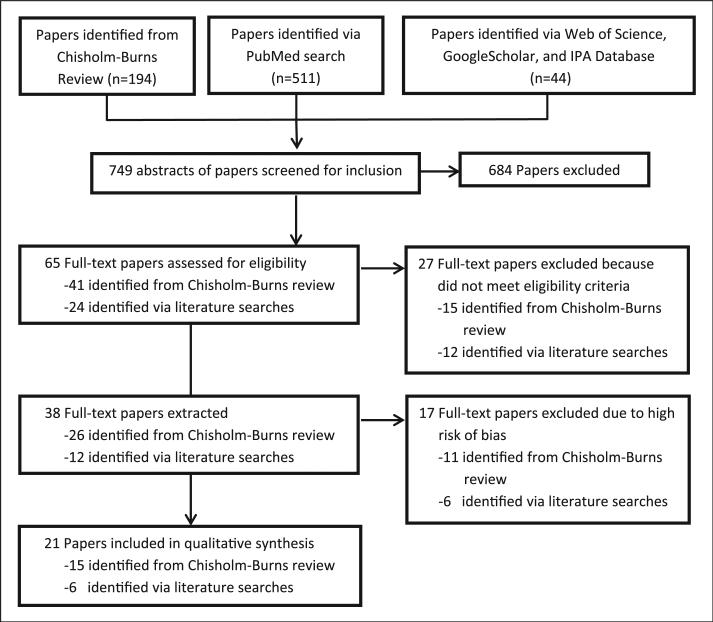
As shown in Figure 2, 684 of the 749 articles identified were excluded during the abstract review. Of the 65 articles included in the full-text review, 27 were excluded because review of the full-text articles revealed that they failed to meet the study inclusion criteria. Fifteen of the studies that we excluded based on the full-text review were included in the Chisholm-Burns review. We excluded 12 of these studies because they were not conducted exclusively in community pharmacy settings. Of the remaining three studies, one reported only process measures, one provided no information concerning the statistical significance of the findings reported, and one was not conducted in the United States.
Figure 2.
Selection of studies for inclusion in review.
We abstracted data from the remaining 38 articles. However, 17 studies were excluded following data abstraction because they were rated as having a high risk of bias. Thus, a total of 21 articles were included in the qualitative synthesis.
The included studies were published between 1973 and 2011 (Table 1). Twelve of the studies used RCT designs, four used before–after designs, four used cohort designs, and one used a nonrandomized comparison group design. The most common health conditions targeted by the interventions evaluated were diabetes (n = 4) and hypertension (n = 4). Three studies targeted multiple health conditions. Most of the interventions involved disease or medication management, three involved refill reminders, and one involved pharmacist administration of influenza vaccinations. The median sample size was 130 and the median length of planned follow-up was 9 months.
Table 1.
Study Characteristics.
| Characteristic | Number of Studies (%) |
|---|---|
| Condition studied | |
| Diabetes | 4 (19.0) |
| Hypertension | 4 (19.0) |
| Multiple chronic conditions | 3 (14.3) |
| Other (includes cardiovascular disease, HIV/AIDS, pulmonary disease, falls, hyperlipidemia, influenza, stroke) | 10 (47.6) |
| Study design | |
| Randomized controlled trial | 12 (57.1) |
| Cohort | 4 (19.0) |
| Before-after | 4 (19.0) |
| Nonrandomized controlled trial | 1 (4.8) |
| Nature of intervention | |
| Disease or medication management | 17 (81.0) |
| Refill reminders | 3 (14.3) |
| Pharmacist administration of influenza immunization | 1 (4.8) |
| Sample sizea | |
| ≤ 100 | 8 (40.0) |
| 101-300 | 5 (25.0) |
| >300 | 7 (35.0) |
| Planned length of follow-up | |
| <12 months | 12 (57.1) |
| ≥12 months | 9 (42.9) |
Number of study participants was not reported in one study. Prescriptions for ticlopidine was the unit of analysis in this study.
Information concerning a total of 134 outcomes was extracted from the 21 articles included in the review (Table 2). Of these 134 outcomes, the articles reported a total of 53 statistically significant differences at p < .05. Fifty of the 53 statistically significant differences favored the intervention group, indicating beneficial intervention effects. The remaining three statistically significant differences involved measures of health service utilization. Studies that used an RCT design were less likely to demonstrate a beneficial intervention effect compared with studies that used other designs (20.0% vs. 59.3%, respectively, χ2 = 21.8, p < .0001). In the next section, we discuss the findings reported, stratified by the type of outcome examined.
Table 2.
Summary of Study Findings.
| Reference | Specific Measure Used | Time Assessed Following Baseline | Comparatora | Results |
|---|---|---|---|---|
| Medication adherence | ||||
| McKenney, Slining, Henderson, Devins, and Barr (1973) | Mean adherence percentage during study (pill count) | 5-month average | Control group | Intervention: 92%*** Comparator: 56% |
| McKenney et al. (1973) | Mean adherence percentage after study (pill count) | 6 months | Control group | NR |
| Ascione, Brown, and Kirking (1985) | Mean days late/refill (Rx records) | 4 months | Control group | NR |
| Ascione et al. (1985) | Mean days late/refill (Rx records) | 4 months | Baseline | Intervention: 6.6 days** Comparator: 19.15 days |
| Park, Kelly Carter, and Burgess (1996) | Mean adherence percentage (pill count) | 1 month | Control group | Intervention: 96.7%* Comparator: 86.0% |
| Park et al. (1996) | Mean adherence percentage (pill count) | 2 months | Control group | Intervention: 97.2%* Comparator: 86.7% |
| Park et al. (1996) | Mean adherence percentage (pill count) | 3 months | Control group | NS |
| Berringer et al. (1999) | Mean adherence percentage (Rx records) | 12 months | Baseline | NS |
| Fincham and Wallace (2000) | Mean days late for refill (Rx records) | 5 months | Baseline | Intervention: 2.37 days* Comparator: 10.5 days |
| Weinberger et al. (2002b) | Mean adherence (self-report) | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Mean adherence (self-report) | 12 months | Peak flow groupa | NS |
| Weinberger et al. (2002b) | Percentage nonadherent (self-report) | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Percentage nonadherent (self-report) | 12 months | Peak flow groupa | NS |
| Zillich, Sutherland, Kumbera, and Carter (2005) | Percentage nonadherent (self-report) | 3 months | Control group | NS |
| Planas, Crosby, Mitchell, and Farmer (2009) | Percentage adherent (Rx records) | 9 months | Control group | NS |
| Nietert et al. (2009; Phone PT)b | Days to refill prescription (Rx records) | 9 months | Control group | NS |
| Nietert et al. (2009; Fax MD)b | Days to refill prescription (Rx records) | 9 months | Control group | NS |
| Nietert et al. (2009; Phone PT)b | Percentage filled Rx for medication in same disease class within 30 days of index date (Rx records) | 30 days | Control group | NS |
| Nietert et al. (2009; Fax MD)b | Percentage filled Rx for medication in same disease class within 30 days of index date (Rx records) | 30 Days | Control group | NS |
| Nietert et al. (2009; Phone PT)b | Percentage filled Rx for medication in same disease class within 60 days of index date (Rx records) | 60 days | Control group | NS |
| Nietert et al. (2009; Fax MD)b | Percentage filled Rx for qualified medication in same disease class within 60 days of index date (Rx records) | 60 days | Control group | NS |
| Hirsch, Rosenquist, Best, Miller, and Gilmer (2009) | Percentage adherent, MPR 80% to 120% (Rx claims data) | 1 year | Comparison group | Intervention: 56.3%*** Comparator: 38.1 % |
| Hirsch, Rosenquist, et al. (2009) | Percentage excess prescription fills, MPR > 120% (Rx claims data) | 1 year | Comparison group | Intervention: 19.7%*** Comparator: 44.8% |
| Gazmararian, Jacobson, Pan, Schmotzer, and Kripalani (2010) | Change in cumulative medication gap (Rx records) | 6 months | Control group | NS |
| Hirsch et al. (2011) | Percentage adherent, MPR 80% to 120% (Rx claims data) | 1 year | Comparison group | Intervention: 65.8%*** Comparator: 43.0% |
| Hirsch et al. (2011) | Percentage adherent, MPR 80% to 120% (Rx claims data) | 2 years | Comparison group | Intervention: 71.8%*** Comparator: 44.8% |
| Hirsch et al. (2011) | Percentage adherent, MPR 80% to 120% (Rx claims data) | 3 years | Comparison group | Intervention: 69.4%*** Comparator: 47.3% |
| Hirsch et al. (2011) | Percentage excess prescription fills, MPR > 120% (Rx claims data) | 1 year | Comparison group | Intervention: 14.6%*** Comparator: 39.7% |
| Hirsch et al. (2011) | Percentage excess prescription fills, MPR > 120% (Rx claims data) | 2 years | Comparison group | Intervention: 12.5%*** Comparator: 36.9% |
| Hirsch et al. (2011) | Percentage excess prescription fills, MPR > 120% (Rx claims data) | 3 years | Comparison group | Intervention: 12.9%*** Comparator: 35.5% |
| Appropriate medication use | ||||
| Chrischilles et al. (2004) | Change in percentage of people aged 65+ using a Beers drug (Rx claims data) | 9 months | Comparison group | Intervention: −14.3%* Comparator: −2.8% |
| Chrischilles et al. (2004) | Percentage with at least one problem on Medication Appropriateness Index | 9 months | Baseline | Intervention: 89.1%** Comparator: 92.1% |
| Chrischilles et al. (2004) | Mean Medication Appropriateness Index | 9 months | Baseline | Intervention: 8.3 Comparator: 9.4 |
| Chrischilles et al. (2004) | Change in number of active drugs used (Rx claims data) | 9 months | Comparison group | NS |
| Nola et al. (2000) | Percentage of patients on lipid-lowering therapy (Rx records) | 6 months | Control group | NS |
| Hirsch, Rosenquist, et al. (2009) | Percentage using 1+ contraindicated ART regimen (Rx claims data) | 1 year | Comparison group | Intervention: 11.6%*** Comparator: 16.6% |
| Blalock et al. (2010) | Rate of filling prescriptions for high-risk medications/1,000 days (Rx records) | 1 year | Control group | NS |
| Hirsch et al. (2011) | Percentage using 1+ contraindicated ART regimen (Rx claims data) | 1 year | Comparison group | Intervention: 10.7%* Comparator: 14.8% |
| Hirsch et al. (2011) | Percentage using 1+ contraindicated ART regimen (Rx claims data) | 2 years | Comparison group | Intervention: 8.9%** Comparator: 13.7% |
| Hirsch et al. (2011) | Percentage using 1+ contraindicated ART regimen (Rx claims data) | 3 years | Comparison group | Intervention: 8.9%* Comparator: 12.2% |
| Immunization receipt | ||||
| Grabenstein, Guess, Hartzema, Koch, and Konrad (2001) | Percentage vaccinated in 1998, but not in 1997 | 1 year | Comparison group | Intervention: 34.7%** Comparator: 23.9% |
| Grabenstein et al. (2001) | Change in percentage vaccinated from 1997 to 1998 (65 years and older) | 1 year | Comparison group | NS |
| Grabenstein et al. (2001) | Change in percentage vaccinated from 1997 to 1998 (<65 years with chronic conditions) | 1 year | Comparison group | Intervention: 9.2%* Comparator: −1.4% |
| Self-care activities | ||||
| Doucette, Witry, Farris, and McDonough (2009) | Mean change in diet self-care activities (days/week) | 12 months | Control group | Intervention: 0.7 days/week*** Comparator: −0.55 days/week |
| Doucette et al. (2009) | Mean change in diabetes self-care activities (days/week) | 12 months | Control group | Intervention: 0.79 days/week* Comparator: 0.06 days/week |
| Doucette et al. (2009) | Mean change in exercise self-care activities (days/week) | 12 months | Control group | NS |
| Blood pressure | ||||
| McKenney et al. (1973) | Percentage normotensive (DBP < 90 mmHg) during study | 5-month average | Control group | NR |
| McKenney et al. (1973) | Percentage normotensive (DBP < 90 mmHg) after study | 6 months | Control group | NR |
| Park et al. (1996) | Percentage normotensive (BP < 140/90 mmHg) | 3 months | Baseline | Intervention: 52.2%* Comparator: 17.4% |
| Park et al. (1996) | Mean DBP (mmHg) | 3 months | Baseline | Intervention: 83.2 mmHg* Comparator: 87.8 mmHg |
| Park et al. (1996) | Mean SBP (mmHg) | 3 months | Baseline | Intervention: 143.2 mmHg* Comparator: 155.5 mmHg |
| Zillich et al. (2005) | Mean SBP (mmHg) | 3 months | Control group | NS |
| Zillich et al. (2005) | Mean change in DBP (mmHg) | 3 months | Control group | Intervention: −8.8 mmHg Comparator: −5.6 mmHg |
| Zillich et al. (2005) | Percentage achieving blood pressure control | 3 months | Control group | NS |
| John et al. (2006) | Mean SBP (mmHg) | NR | Baseline | Intervention: 120.4 mmHg* Comparator: 124.1 mmHg |
| John et al. (2006) | Mean DBP (mmHg) | NR | Baseline | Intervention: 77.4 mmHg* Comparator: 80.4 mmHg |
| Doucette et al. (2009) | Change in SBP | 12 months | Control group | NS |
| Doucette et al. (2009) | Change in DBP | 12 months | Control group | NS |
| Planas et al. (2009) | Mean change in SBP (mmHg) | 9 months | Control group | Intervention: −17.3 mmHg** Comparator: 2.7 mmHg |
| Planas et al. (2009) | Odds of achieving blood pressure goal | 9 months | Control group | Odds ratio: 12.92* (95% CI = 1.47, 113.77) |
| Planas et al. (2009) | Percentage at goal blood pressure (< 130/80) | 9 months | Control group | Intervention: 48.0%** Comparator: 6.7% |
| Blood glucose | ||||
| Berringer et al. (1999) | Blood glucose (home monitoring) | 6 months | Baseline | NS |
| Berringer et al. (1999) | Blood glucose (home monitoring) | 12 months | Baseline | Intervention: 149.7 mg/dl* Comparator: 179.0 mg/dl |
| HBA1C | ||||
| Cranor and Christensen (2003) | HbA1c % | 9 months | Comparison group | Intervention: 6.9%* Comparator: 7.7% |
| Cranor, Bunting, and Christensen (2003) | HbA1c % | 6 months | Baseline | Intervention: 6.8%**** Comparator: 7.9% |
| Cranor et al. (2003) | HbA1c% | 12 months | Baseline | Intervention: 6.7%**** Comparator: 7.7% |
| Cranor et al. (2003) | Percentage of patients with optimal HbA1c | 6 months | Baseline | Intervention: 62.5%**** Comparator: 38.2% |
| Cranor et al. (2003) | Percentage of patients with optimal HbA1c | 12 months | Baseline | Intervention: 66.7%**** Comparator: 39.5% |
| Doucette et al.(2009) | Change in HbA1c | 12 months | Control group | NS |
| Lipids | ||||
| Cranor et al. (2003) | LDL-C (mg/dl) | 6 months | Baseline | NS |
| Cranor et al. (2003) | LDL-C (mg/dl) | 12 months | Baseline | NS |
| Cranor et al. (2003) | Percentage of patients with optimal LDL | 6 months | Baseline | NS |
| Cranor et al. (2003) | Percentage of patients with optimal LDL | 12 months | Baseline | NS |
| Cranor et al. (2003) | HDL-C (mg/dl) | 6 months | Baseline | Intervention:47.1 mg/dl* Comparator: 46.0 mg/dl |
| Cranor et al. (2003) | HDL-C (mg/dl) | 12 months | Baseline | NS |
| Cranor et al. (2003) | Percentage of patients with optimal HDL-C | 6 months | Baseline | NS |
| Cranor et al. (2003) | Percentage of patients with optimal HDL-C | 12 months | Baseline | NS |
| Doucette et al. (2009) | Change in LDL-C | 12 months | Control group | NS |
| Nola et al. (2000) | Triglycerides (mg/dl) | 6 months | Control group | NS |
| Nola et al. (2000) | Total cholesterol (mg/dl) | 6 months | Control group | NS |
| Nola et al. (2000) | HDL-C (mg/dl; SD) | 6 months | Control group | NS |
| Nola et al. (2000) | LDL-C (mg/dl; SD) | 6 months | Control group | NS |
| Nola et al. (2000) | Percentage reaching cholesterol goal | 6 months | Control group | NS |
| Pulmonary disease control | ||||
| Weinberger et al. (2002b) | Mean peak flow rate, percentage predicted | 12 months | Control groupa | Intervention: 63.7%* Comparator: 61.8% |
| Weinberger et al. (2002b) | Mean peak flow rate, percentage predicted | 12 months | Peak flow groupa | NS |
| Safety outcomes | ||||
| Nola et al. (2000) | AHA; Risk Factor prediction score | 6 months | Control group | NS |
| Hirsch, Rosenquist, et al. (2009) | Percentage with 1+ opportunistic infection (Claims data) | 1 year | Comparison group | NS |
| Blalock et al. (2010) | Rate of recurrent falls/1,000 days | 1 year | Control group | NS |
| Blalock et al. (2010) | Rate of injurious falls/1,000 days | 1 year | Control group | NS |
| Hirsch et al. (2011) | Percentage with 1+ opportunistic infection (Claims data) | 1 year | Comparison group | NS |
| Hirsch et al. (2011) | Percentage with 1+ opportunistic infection (Claims data) | 2 years | Comparison group | NS |
| Hirsch et al. (2011) | Percentage with 1+ opportunistic infection (Claims data) | 3 years | Comparison group | NS |
| Quality of life | ||||
| Park et al. (1996) | Mean general health perception: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean physical functioning: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean physical health: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean emotional problems: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean social functioning: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean mental health: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean bodily pain: Health Status Questionnaire | 3 months | Control group | NS |
| Park et al. (1996) | Mean energy/fatigue: Health Status Questionnaire | 3 months | Control group | Intervention: 67.6* Comparator: 56.5 |
| Weinberger et al. (2002b) | Mean disease-specific HRQOL (COPD patients) | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Mean disease-specific HRQOL (COPD patients) | 12 months | Peak flow groupa | NS |
| Weinberger et al. (2002b) | Mean disease-specific HRQOL (asthma patients) | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Mean disease-specific HRQOL (asthma patients) | 12 months | Peak flow groupa | NS |
| Cranor and Christensen (2003) | Physical health | 9 months | Baseline | NS |
| Cranor and Christensen (2003) | Mental health | 9 months | Baseline | NS |
| Patient satisfaction | ||||
| Kradjan et al. (1999) | Mean general satisfaction | 3 months | Control group | NS |
| Kradjan et al. (1999) | Mean satisfaction with clinical competence | 3 months | Control group | NS |
| Kradjan et al. (1999) | Mean satisfaction with explanation | 3 months | Control group | Intervention: 3.6* Comparator: 3.4 |
| Kradjan et al. (1999) | Mean satisfaction with access | 3 months | Control group | NS |
| Kradjan et al. (1999) | Mean satisfaction with pharmacist-MD relationship | 3 months | Control group | NS |
| Kradjan et al. (1999) | Mean satisfaction with consideration | 3 months | Control group | NS |
| Weinberger et al. (2002b) | Mean satisfaction with pharmacist | 12 months | Control groupa | Intervention:Values not reported* Comparator:Values not reported |
| Weinberger et al. (2002b) | Mean satisfaction with pharmacist | 12 months | Peak flow groupa | Intervention:Values not reported*** Comparator:Values not reported |
| Weinberger et al. (2002b) | Mean satisfaction with health care | 6 months | Control groupa | Intervention:Values not reported** Comparator:Values not reported |
| Weinberger et al. (2002b) | Mean satisfaction with health care | 6 months | Peak flowa monitoring | NS |
| Weinberger et al. (2002b) | Mean satisfaction with health care | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Mean satisfaction with health care | 12 months | Peak flow groupa | NS |
| Cranor and Christensen (2003) | Mean satisfaction with technical aspects | 9 months | Baseline | Intervention: 82.7** Comparator: 64.4 |
| Cranor and Christensen (2003) | Mean satisfaction with consideration | 9 months | Baseline | Intervention: 78.5** Comparator: 64.1 |
| Cranor and Christensen (2003) | Mean satisfaction with explanation | 9 months | Baseline | Intervention: 82.8** Comparator: 71.1 |
| Cranor and Christensen (2003) | Mean general satisfaction | 9 months | Baseline | Intervention: 79.8** Comparator: 69.4 |
| Patient knowledge | ||||
| Nola et al. (2000) | Mean score on hyperlipidemia—patient knowledge evaluation | 6 months | Control group | NS |
| Health care utilization | ||||
| Weinberger et al. (2002b) | Percentage with a breathing-related ED visit or hospitalization (COPD) | 12 months | Control groupa | NS |
| Weinberger et al. (2002b) | Percentage with a breathing-related ED visit or hospitalization (COPD) | 12 months | Peak flow groupa | NS |
| Weinberger et al. (2002b) | Percentage with a breathing-related ED visit or hospitalization (asthma) | 12 months | Control groupa | Intervention: 15.7%*** Comparator: 7.3% |
| Weinberger et al. (2002b) | Percentage with a breathing-related ED visit or hospitalization (asthma) | 12 months | Peak flow groupa | NS |
| Cranor and Christensen (2003) | Outpatient and inpatient claims with diabetes diagnosis, mean | 9 months | Baseline | Intervention: 2.8** Comparator: 1.5 |
| Cranor and Christensen (2003) | Outpatient and inpatient claims with diagnosis other than diabetes, mean | 9 months | Baseline | NS |
| Cranor and Christensen (2003) | Outpatient and inpatient claims with any diagnosis, mean | 9 months | Baseline | Intervention: 7.4** Comparator: 5.2 |
| Chrischilles et al. (2004) | Claims for medical services | 9 months | Comparison group | NS |
| Chrischilles et al. (2004) | Outpatient facility claims | 9 months | Comparison group | NS |
| Chrischilles et al. (2004) | Inpatient institutional claims | 9 months | Comparison group | NS |
| Chrischilles et al. (2004) | Emergency department claims | 9 months | Comparison group | NS |
Note: NR = Statistical significance of observed differences not reported; NS = observed differences not statistically significant; CI = confidence interval; Rx = pharmacy; ED = emergency department; MPR = medication possession ratio; ART = antiretroviral therapy; SBP = systolic blood pressure; DBP = diastolic blood pressure; HbA1c = glycated hemoglobin; LDL-C = low-density lipoprotein cholesterol; HDL-C = high-density lipoprotein cholesterol; AHA = American Heart Association; HRQOL = health-related quality of life; COPD = chronic obstructive pulmonary disease.
The study by Weinberger et al. (2002b) had two control groups, a usual care group and a peak flow monitoring group.
The study by Nietert et al. (2009) evaluated two different refill reminder interventions, “phone the patient” and “fax the physician.”
p < .05.
p < .01.
p < .001.
p < .0001.
Qualitative Synthesis of the Outcomes Reported
Behavior and Behavior Change Outcomes
The articles reviewed examined effects of the interventions on four types of behaviors: medication adherence, appropriate medication use, receipt of immunizations, and participation in self-care activities. The articles examined a total of 46 behavioral outcomes. Of these, 24 (52.2%) were statistically significant at p < .05.
Medication adherence
Twelve studies evaluated the effects of interventions on medication adherence. Six of these studies found no statistically significant effects (Berringer et al., 1999; Gazmararian, Jacobson, Pan, Schmotzer, & Kripalani, 2010; Nietert et al., 2009; Planas, Crosby, Mitchell, & Farmer, 2009; Weinberger et al., 2002b; Zillich, Sutherland, Kumbera, & Carter, 2005). These included four studies that evaluated the effects of disease management programs and two that evaluated the effects of refill reminders. A total of 30 adherence outcomes were reported across the 12 studies. Of these, 13 were statistically significant at p < .05, with all significant differences favoring the intervention group. Eight of these statistically significant outcomes were from two articles by Hirsch and colleagues. In these articles, the investigators used a retrospective cohort design to examine the effects of an HIV/AIDS pharmacy medication management compensation pilot program targeting California Medicaid beneficiaries. The intervention group included individuals with HIV/AIDS who filled at least 50% of their antiretroviral therapy prescriptions at pilot pharmacies that provided a wide range of medication management services. The comparison group included individuals with HIV/AIDS who primarily used nonpilot pharmacies (Hirsch et al., 2011; Hirsch, Rosenquist, Best, Miller, & Gilmer, 2009). This study found consistent between-group differences in the percentage of patients classified as adherent of approximately 20% over the 3 years of the study. Of the remaining four studies that reported one or more statistically significant adherence outcomes, three had mixed findings and were based on relatively small samples, ranging from 49 to 102 (Ascione, Brown, & Kirking, 1985; McKenney, Slining, Henderson, Devins, & Barr, 1973; Park, Kelly, Carter, & Burgess, 1996) and the remaining study did not report sample size. In this final study, data were analyzed using prescription refills as the unit of analysis (Fincham & Wallace, 2000).
Appropriate medication use
Five studies evaluated the effects of interventions on appropriate medication use. Two of these studies, both using RCT designs, found no statistically significant effects (Blalock et al., 2010; Nola et al., 2000). Of the 10 outcomes reported across all 5 studies, 7 were statistically significant at p < .05, with all significant differences favoring the intervention group. Four of these were from the two articles by Hirsch and colleagues described above (Hirsch et al., 2011; Hirsch, Rosenquist, et al., 2009). Relative to individuals in the comparison group, these articles found that patients in the intervention group were approximately 30% less likely to use one or more contraindicated antiretroviral medication regimen. The remaining three statistically significant findings were from a study by Chrischilles et al. (2004) that used a prospective cohort design to evaluate the effect of the Iowa Medicaid Pharmaceutical Case Management program. This program was targeted toward patients identified as being at high risk of experiencing medication-related adverse effects. In this study, the percentage of patients aged 65 years and older who were using a drug on the Beers list decreased by 14.3% from baseline to follow-up in the intervention group compared with 2.8% in the comparison group. The Beers list identifies medications that are potentially inappropriate for older adults (American Geriatrics Society 2012 Beers Criteria Update Expert Panel, 2012). In addition, the Medication Appropriateness Index (Samsa et al., 1994) revealed significant improvements from baseline to follow-up.
Immunization
One study evaluated the effect of a statewide policy change allowing pharmacist administration of immunization vaccines (Grabenstein, Guess, Hartzema, Koch, & Konrad, 2001). An adjacent state that did not allow pharmacist administration of these vaccines served as a comparison group. Among individuals who had not been vaccinated in the previous year, 34.7% were vaccinated the following year in the state that enacted the policy change compared with 23.9% in the comparison state (p < .01). In addition, in the state that enacted the policy change, there was an increase of 9.2% in the percentage of people younger than 65 years who were vaccinated the following year compared with a decrease of 1.4% in the comparison state (p < .05).
Self-care activities
One study found that a diabetes disease management program had positive effects on diet and diabetes self-care activities (Doucette, Witry, Farris, & McDonough, 2009). On average, individuals in the intervention group participated in diet and diabetes self-care activities about 1 day/week more often than individuals in the control group. However, the program had no effect on exercise.
Health Outcomes
The articles reviewed examined effects of the interventions on six types of health outcomes: blood pressure, blood glucose and HbA1c, lipids, pulmonary disease control, safety outcomes, and quality of life. The articles examined a total of 60 health outcomes. Of these, 18 (30.0%) were statistically significant at p < .05.
Blood pressure
Six studies evaluated the effects of interventions on blood pressure. Two of these studies, both using RCT designs, found no statistically significant effects (Doucette et al., 2009; McKenney et al., 1973). Of the 15 outcomes reported, 9 were statistically significant at p < .05 and favored the intervention group. Seven of the statistically significant effects were observed in three studies that used RCT designs. However, three of these outcomes were observed in a study that did not report the statistical significance of between-group comparisons involving blood pressure outcomes (Park et al., 1996). Instead, the study assessed changes in blood pressure control within the intervention group over time. In one of the RCTs, 48.0% of patients in the intervention group were classified as having blood pressure at goal compared with 6.7% of patients in the control group (Planas et al., 2009). Statistically significant differences reported in other studies were more modest, with differences in diastolic blood pressure ranging from 3.2 to 4.6 mmHg and differences in systolic blood pressure ranging from 3.7 to 12.3 mmHg.
Blood glucose and HbA1c
Four studies evaluated the effects of interventions on either blood glucose or HbA1c. Of the eight outcomes reported, six were statistically significant at p < .05 and favored the intervention group. However, all of the statistically significant differences were observed in studies that used relatively weak research designs, either a before–after design (Berringer et al., 1999; Cranor, Bunting, & Christensen, 2003) or a nonrandomized comparison group (Cranor & Christensen, 2003). On average, HbA1c declined approximately 1% over time in these studies. One of these studies found that the percentage of patients with optimal HbA1c improved from less than 40% at baseline to more than 60% at follow-up. However, the only study that used an RCT design found no differences in HbA1c outcomes between groups (Doucette et al., 2009).
Lipids
Three studies evaluated the effects of interventions on lipid levels, two using RCT designs (Cranor et al., 2003; Doucette et al., 2009; Nola et al., 2000). Of the 14 outcomes reported, one was statistically significant at p < .05. The significant finding was observed in a study using a before–after research design (Cranor et al., 2003). It showed an average increase in high-density lipoprotein cholesterol from 46.0 mg/dl at baseline to 47.1 mg/dl at follow-up.
Pulmonary disease control
One study, using an RCT design, evaluated the effect of disease management on peak flow rate in patients with asthma and chronic obstructive pulmonary disease (Weinberger et al., 2002b). This study found an improvement in peak flow rate among patients in the intervention group compared with a usual care control group (mean = 63.7% vs. 61.8%, respectively, p < .02). However, peak flow rate did not differ between patients in the intervention group and patients in a second control group that received basic instruction concerning peak flow monitoring.
Safety outcomes
Four studies evaluated the effects of interventions on safety outcomes, including American Heart Association Risk Factor prediction score (Nola et al., 2000), occurrence of opportunistic infections (Hirsch et al., 2011; Hirsch, Rosenquist et al., 2009), and rate of falls and injurious falls (Blalock et al., 2010). None of the seven safety outcomes examined were statistically significant at p < .05.
Quality of life
Three studies evaluated the effects of interventions on quality of life (Cranor & Christensen, 2003; Park et al., 1996; Weinberger et al., 2002b). Cranor and Christensen (2003) used the SF-12 (Ware, Kosinski, & Keller, 2000). Park et al. (1996) used the Health Status Questionnaire developed by Flack and Grimm (1993). Finally, Weinberger et al. (2002b) used a disease-specific measure developed by Juniper et al. (1992). Of the 14 outcomes reported, one was statistically significant at p < .05. The significant finding was observed in a study using an RCT research design (Park et al., 1996).
Other Outcome Measures
In addition to the behavioral and health outcomes described above, some studies evaluated effects of interventions on patient satisfaction, knowledge, and health care utilization. Findings for these outcomes are discussed below.
Patient satisfaction
Three studies assessed patient satisfaction (Cranor & Christensen, 2003; Kradjan et al., 1999; Weinberger et al., 2002b). Cranor and Christensen (2003) and Kradjan et al. (1999) used a measure of satisfaction with pharmacy services developed by MacKeigan and Larson (1989). Weinberger et al. (2002b) used measures assessing satisfaction with the pharmacist (Tierney et al., 1999) and satisfaction with health care in general (Ware, Snyder, Wright, & Davies, 1983). Two of the three studies used RCT designs (Kradjan et al., 1999; Weinberger et al., 2002b). Of the 12 satisfaction outcomes reported in these studies, 4 were statistically significant at p < .05. Although the third study had an independent comparison group, the four satisfaction outcomes reported were based on before–after comparisons (Cranor & Christensen, 2003). All four of these outcomes showed statistically significant increases in satisfaction over time at p < .05.
Knowledge
One study evaluated the effect of a hyperlipidemia disease management program on knowledge using a measure that had been used in previous research (Nola et al., 2000). The program had no effect on this measure.
Health care utilization
Four studies evaluated the effects of interventions on health service utilization. Of the 11 outcomes reported, 3 were statistically significant at p < 0.05, with all revealing greater utilization of health services in the intervention group. In the study by Weinberger et al. (2002b), the percentage of asthma patients who had a breathing-related emergency department visit or hospitalization was higher in the intervention group compared with the usual care control group (15.7% vs. 7.3%, respectively, p < .001). The other significant findings were observed by Cranor et al. in a study involving diabetes disease management (Cranor & Christensen, 2003). From baseline to follow-up, this study found that (a) the average number of outpatient and inpatient claims with a diabetes diagnosis increased from 1.5 to 2.8 (p < .01) and (b) the average number of total outpatient and inpatient claims increased from 5.2 to 7.4 (p < .01).
Sensitivity Analyses
We performed two sensitivity analyses to determine if the outcomes reported in articles that we excluded due to high risk of bias were more likely to report beneficial intervention effects compared with included articles. The first analysis focused just on outcomes extracted from the 17 studies that were excluded due to a risk of bias. Of 86 outcomes abstracted from these 17 studies, 28 (32.6%) demonstrated beneficial effects, similar to our findings for the included studies.
The second analysis focused just on studies that were included in the Chisholm-Burns et al. review. This included a total of 26 studies, 15 that were included in our main review and 11 that were excluded following data extraction due to a high risk of bias. Of the 173 outcomes extracted from these studies, 58 (33.5%) demonstrated beneficial intervention effects. The 15 included and 11 excluded studies were similar with respect to the percentage of outcomes that demonstrated beneficial effects (32.0% vs. 35.7%, respectively).
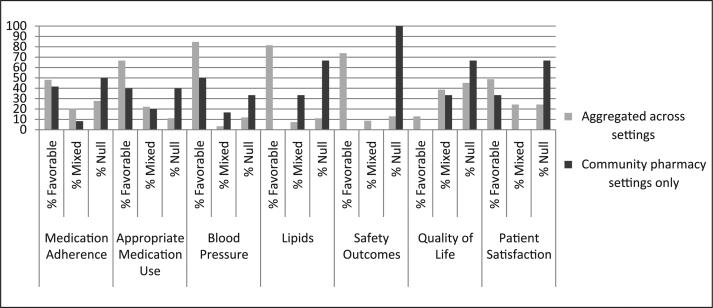
Comparison With Findings Aggregated Across Diverse Practice Sites
Figure 3 compares the outcomes reported in the 21 articles included in this review, which were limited to studies conducted in community pharmacy settings, with the outcomes reported by Chisholm-Burns et al. (2010) in their review of the effects of pharmacist-delivered patient care services aggregated across diverse practice settings (e.g., inpatient, outpatient). The figure is limited to seven outcomes that were reported both in the Chisholm-Burns et al. review and in at least three of the 21 articles included in our review. These outcomes are medication adherence, appropriate medication use, blood pressure, lipids, safety outcomes, quality of life, and patient satisfaction. As expected, the percentage of studies yielding favorable findings was lower in the community pharmacy–based studies than in the aggregated studies reported in the Chisholm-Burns et al. review. In the aggregated findings, the percentage of studies reporting favorable findings ranged from 84.7% for blood pressure to 12.9% for quality of life. In comparison, among the community pharmacy–based studies included in our review, the percentage of studies reporting favorable findings ranged from 50% for blood pressure to 0% for lipids, safety outcomes, and quality of life.
Figure 3.
Outcomes of studies evaluating the effects of pharmacist-delivered patient care services, aggregated across settings and limited to studies conducted in community pharmacy settings.
Note: Data shown for the aggregated findings are based on results reported by Chisholm-Burns et al. (2010). Data for the community pharmacy settings are based on results from the 21 articles included in the current review. Outcomes were classified using the following criteria: favorable = statistically significant beneficial effects associated with pharmacist care on all measures of the outcome; mixed = statistically significant beneficial effects associated with pharmacist-provided care on some, but not all measures of the outcome; null = no statistically significant differences observed.
Analysis of Hypothesized Facilitating Factors
In this section, we discuss findings from the articles reviewed in relation to the seven factors hypothesized to facilitate the successful implementation of clinical services in community pharmacy settings: patient receptivity, pharmacists’ relationship with local physicians, communication among pharmacy staff, pharmacy layout, manpower issues, availability of external support to assist with program implementation, and reimbursement for clinical services provided (Roberts et al., 2008).
Three of the articles reviewed discussed patient receptivity to the intervention directly. One study evaluating an asthma pharmaceutical care program found that patients did not expect community pharmacists to provide clinical services and did not perceive the value of these services (Kradjan et al., 1999). Two other studies evaluating refill reminder interventions reported that patients were sometimes confused or annoyed by the reminders (Ascione et al., 1985; Nietert et al., 2009). Participation rate may be another indicator of patient receptivity. Three of the studies reported that fewer than 25% of patients approached accepted invitations to participate in the study (Blalock et al., 2010; Gazmararian et al., 2010; Nola et al., 2000). Another study compared the outcomes of patients who primarily used community pharmacies that offered specialized services for HIV-positive patients (Hirsch et al., 2011; Hirsch, Rosenquist, et al., 2009). Because patients selected whether to use specialized versus traditional pharmacies, it is reasonable to speculate that those using the specialized pharmacies valued the services that they provided. Moreover, the percentage of patients using the specialized pharmacies increased from 5.9% in 2004 to 28.1% in 2007, suggesting that patient awareness and receptivity increased over time.
Several studies addressed issues related to the quality of the pharmacist–physician relationship. In most cases, this involved reporting the percentage of pharmacist recommendations that were accepted by the physician. Reported acceptance rates ranged from 28.6% (Doucette et al., 2009) to 86% (Zillich et al., 2005). Two articles (Blalock et al., 2010; Doucette et al., 2009) discussed difficulties that study pharmacists experienced when attempting to communicate with physicians. Finally, in a study involving refill reminders, 45% of the physicians contacted declined to participate (Nietert et al., 2009).
Only one study described the processes through which pharmacy staff communicated with one another to coordinate service delivery (Berringer et al., 1999). This study found a significant reduction in blood glucose among study participants at a 12-month follow-up.
The only article that discussed a pharmacy layout issue indicated that inability to use the primary pharmacy computer to deliver the intervention may have resulted in inconsistent intervention implementation (Weinberger et al., 2002b). In that study, pharmacists were required to access data on a separate computer located in the pharmacy each time a program participant filled a prescription. However, pharmacists actually accessed the data only 50% of the time and documented their actions only 50% of the times the data were accessed. This study found that the intervention, which targeted patients with reactive airways disease, improved peak expiratory flow rates in the intervention group compared with a usual care control group. However, no difference in this outcome was shown between the intervention group and a control group that received peak flow meters to facilitate self-monitoring.
Manpower issues were not discussed in a consistent way across articles. Only one article described how clinical services were integrated into the pharmacy workflow (Berringer et al., 1999). Three other articles indicated that a specific pharmacist or pharmacy residents were designated to deliver the intervention (Blalock et al., 2010; Fincham & Wallace, 2000; McKenney et al., 1973). Another article suggested that lack of manpower may have limited the number of patients reached by the intervention (Chrischilles et al., 2004). This study evaluated the Iowa Medicaid Pharmaceutical Case Management program. This program targeted Medicaid patients who were at high risk for experiencing adverse drug reactions. Pharmacists were required to contact patients after receiving a list of the names of eligible patients from a central office. Of the 3,037 patients eligible for the program, only 690 received the services available. Although the investigators attributed this problem to pharmacy staffing issues, it is possible that patients declined the services when offered to them. Despite these issues, however, this study demonstrated substantial improvements in the quality of medication use among those participants who did receive the services available. Finally, in the study described by Hirsch, Rosenquist, et al. (2009) and Hirsch et al. (2011), intervention pharmacies were required to be able to begin offering medication therapy management services immediately after selection into the program and have qualified staff to identify patients who should receive the services available. This study demonstrated consistent positive effects of the intervention on measures of medication adherence and appropriate medication use.
None of the articles reviewed directly addressed the effect of the availability of external support in terms of either facilitating or hindering service delivery. However, three of the articles evaluated interventions that were delivered as part of employer-sponsored programs (Cranor & Christensen, 2003; Cranor et al., 2003; John et al., 2006) and three other articles evaluated interventions that were delivered as part of statewide Medicaid programs (Chrischilles et al., 2004; Hirsch et al., 2011; Hirsch, Oen, Robertson, Nguyen, & Daniels, 2009). In all these studies, pharmacists were compensated for the clinical services they provided. It seems likely that participating pharmacies may have received additional support from the sponsoring organizations. However, the articles provided little information concerning the nature or extent of support that was available.
Nine of the articles reported that pharmacists were reimbursed for the clinical services they provided (Chrischilles et al., 2004; Cranor & Christensen, 2003; Cranor et al., 2003; Doucette et al., 2009; Grabenstein et al., 2001; Hirsch et al., 2011; Hirsch, Rosenquist, et al., 2009; John et al., 2006; Zillich et al., 2005). These articles tended to report more favorable outcomes compared with the other articles reviewed. However, only two of the studies reported in these articles (Kradjan et al., 1999; Zillich et al., 2005) used RCT designs. Therefore, it is not possible to determine whether reimbursing pharmacists for the clinical services provided had an impact on the effectiveness of the intervention.
Discussion
Many studies conducted over the past 40 years have demonstrated the beneficial effects that pharmacist-provided direct patient care services can have on patient health outcomes. In their recent systematic review, Chisholm-Burns et al. (2010) concluded that “Pharmacist-provided direct patient care has favorable effects across various patient outcomes, health care settings, and disease states.” Because community pharmacists are among the most accessible health care providers, community pharmacist-provided clinical services have the potential to have a major impact on patient health outcomes. However, only 29 of the studies reviewed by Chisholm-Burns et al. (2010) were conducted in community pharmacy settings. Moreover, our findings suggest that the evidence supporting the effectiveness of pharmacist-provided direct patient care services in this setting is more limited. The 21 articles included in our review were less likely to report favorable intervention effects than suggested in the review by Chisholm-Burns et al. (2010) in which study findings were aggregated across diverse practice settings. Only 50 of the 134 outcomes (37.3%) examined in the 21 articles that we reviewed revealed statistically significant between-group differences or changes over time that were consistent with beneficial intervention effects. Moreover, in studies that used RCT designs only 20% of the outcomes examined demonstrated statistically significant beneficial effects.
Our findings suggest that setting matters. As reflected by the conceptual model that guided this review, the effectiveness of patient care services can be affected by many factors operating at different levels of the ecological framework. Unfortunately, most of the articles reviewed provided little information about factors that can affect intervention effectiveness, including patient receptivity to the services offered. This makes it impossible to assess the impact of different factors on intervention effectiveness. However, some general observations are possible that may account for the limited effectiveness of the community pharmacy–based interventions that we reviewed.
First, several studies noted difficulties that participating pharmacists experienced when communicating with physicians, sometimes reflected in low acceptance rates of pharmacist recommendations. As noted by others, developing strong collaborative relationships with physicians and other prescribers is likely to be critical to the success of pharmacist-delivered interventions (Kellerman & Kirk, 2007). Therefore, future studies should attend carefully to this issue in the planning stages and report the processes and structures put in place to ensure that adequate collaborative relationships were established and maintained over the course of the study.
Second, several studies noted that patient receptivity to the interventions evaluated was mixed. Because most patients do not expect clinical services to be offered at community pharmacies (Worley et al., 2007), they may not understand why the services are being offered, how they might benefit, and how the new services will be coordinated with the care they currently receive from other health care providers. Future research in this area should systematically assess patient receptivity, including knowledge of services, outcome expectations (both positive and negative), perceived barriers to care, and skills that may be needed to either access or fully participate in care delivery. In addition, changes in patient receptivity should be tracked longitudinally, as the findings from one study suggest that receptivity increases over time (Hirsch et al., 2011), as would be expected based on the literature concerning the dissemination of innovations.
Third, pharmacists were reimbursed for the services they delivered in several of the studies reviewed and these studies tended to yield more positive findings, suggesting beneficial intervention effects, compared with the remaining studies. Reimbursement is likely to increase pharmacist motivation to engage in service delivery. Thus, reimbursement may enhance fidelity to intervention protocols. However, because reimbursement was usually provided by insurance providers, other systems-level factors may account for the differences observed.
Finally, it appears that lack of adequate manpower and pharmacy layout issues may have limited the effectiveness of the interventions evaluated in two of the studies reviewed. However, information concerning these factors was not discussed consistently enough to know the extent to which they may have attenuated the effectiveness of interventions in other studies as well.
Our findings highlight the need for rigorous, systematic research to better understand the patient-level, pharmacist-level, pharmacy-level, and health system–level factors that can affect the effectiveness of direct patient care services provided by community pharmacists. Without understanding the factors that are critical for success, investigators are likely to weaken interventions that have demonstrated effectiveness in other settings when attempting to implement them in the community pharmacy setting.
Implementation research is also needed to understand the mechanisms through which pharmacist-provided patient care services may lead to improved patient outcomes. Identifying all hypothesized intervention outcomes a priori, including hypothesized mediating and moderating variables, would allow for more complete evaluation of intervention effects (DeVellis & Blalock, 2008). In addition, future research evaluating pharmacist-provided direct patient care services in community pharmacy settings should use adequate research methods to ensure internal validity. Inadequate sample sizes, lack of fidelity to intervention protocols, and insensitive outcome measures may have contributed to the null findings that we observed.
This review has several limitations. First, we relied on published articles. Because studies with null results are less likely to be published, our findings may overestimate the effectiveness of pharmacist patient care services delivered in community pharmacy settings (Song et al., 2010). Second, we relied entirely on information reported in published reports of study findings. These reports often provided limited information concerning the exact services that were delivered or intervention intensity. Third, the information available was not sufficient to support a meta-analysis. Therefore, our conclusions are based on a qualitative synthesis of study findings.
In conclusion, community pharmacies are an important component of the health care system. They are widespread, located in nearly every community across the United States, providing easy access for most patients. Increasing community pharmacist involvement in patient care has the potential to help solve many of the medication use problems that currently plague our health system. However, we are unlikely to realize this potential unless future intervention studies address the unique barriers present in the community pharmacy setting that can compromise intervention effectiveness and the factors operating at different levels of the ecological framework that are necessary to increase the chances of success. Thus, we hope that this review will serve as a call-to-action for the development of theoretically informed community pharmacy–based interventions that address the implementation issues that may have limited the effectiveness of past intervention attempts.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society. 2012;60:616–631. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ascione FJ, Brown GH, Kirking DM. Evaluation of a medication refill reminder system for a community pharmacy. Patient Education and Counseling. 1985;7:157–165. doi: 10.1016/0738-3991(85)90006-0. [DOI] [PubMed] [Google Scholar]
- Berringer R, Shibley MC, Cary CC, Pugh CB, Powers PA, Rafi JA. Outcomes of a community pharmacy-based diabetes monitoring program. Journal of the American Pharmacists Association (Wash) 1999;39:791–797. [PubMed] [Google Scholar]
- Blalock SJ. The theoretical basis for practice-relevant medication use research: Patient-centered/behavioral theories. Research in Social & Administrative Pharmacy. 2011;7:317–329. doi: 10.1016/j.sapharm.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Blalock SJ, Casteel C, Roth MT, Ferreri S, Demby KB, Shankar V. Impact of enhanced pharmacologic care on the prevention of falls: A randomized, controlled trial. American Journal of Geriatric Pharmacotherapy. 2010;8:428–440. doi: 10.1016/j.amjopharm.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Chisholm-Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, Wunz T. US pharmacists’ effect as team members on patient care: Systematic review and meta-analyses. Medical Care. 2010;48:923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- Chrischilles EA, Carter BL, Lund BC, Rubenstein LM, Voelker MD, Park T-R, Kuehl AK. Evaluation of the Iowa Medicaid pharmaceutical case management program. Journal of the American Pharmacists Association. 2004;44:337–349. doi: 10.1331/154434504323063977. [DOI] [PubMed] [Google Scholar]
- Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice. McGraw-Hill; New York, NY: 1998. [Google Scholar]
- Cooksey JA, Knapp KK, Walton SM, Cultice JM. Challenges to the pharmacist profession from escalating pharmaceutical demand. Health Affairs. 2002;21(5):182–188. doi: 10.1377/hlthaff.21.5.182. [DOI] [PubMed] [Google Scholar]
- Cranor CW, Bunting BA, Christensen DB. The Asheville Project: Long-term clinical and economic outcomes of a community pharmacy diabetes care program. Journal of the American Pharmacists Association (Wash) 2003;43:173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- Cranor CW, Christensen DB. The Asheville Project: Short-term outcomes of a community pharmacy diabetes care program. Journal of the American Pharmacists Association (Wash) 2003;43:149–159. doi: 10.1331/108658003321480696. [DOI] [PubMed] [Google Scholar]
- DeVellis RF, Blalock SJ. Outcomes of self-management interventions. In: Newman S, Steed E, Mulligan K, editors. Chronic physical illness: Self-management and behavioural interventions. McGraw-Hill; London, England: 2008. pp. 148–167. [Google Scholar]
- DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: A meta-analysis. Medical Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- Doucette WR, Witry MJ, Farris KB, McDonough RP. Community pharmacist-provided extended diabetes care. Annals of Pharmacotherapy. 2009;43:882–889. doi: 10.1345/aph.1L605. [DOI] [PubMed] [Google Scholar]
- Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: Updating the cost-of-illness model. Journal of the American Pharmacists Association (Wash) 2001;41:192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- Fincham JE, Wallace IA. Ticlopidine compliance enhancement: A community pharmacy based study. Journal of Pharmacoepidemiology. 2000;8:51–66. [Google Scholar]
- Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13:238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Flack JM, Grimm RH. Health Status Questionnaire 2.0. Health Outcomes Institute; Bloomington, MN: 1993. [Google Scholar]
- Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy-based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Annals of Pharmacotherapy. 2010;44:80–87. doi: 10.1345/aph.1M328. [DOI] [PubMed] [Google Scholar]
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Grabenstein JD, Guess HA, Hartzema AG, Koch GG, Konrad TR. Effect of vaccination by community pharmacists among adult prescription recipients. Medical Care. 2001;39:340–348. doi: 10.1097/00005650-200104000-00005. [DOI] [PubMed] [Google Scholar]
- Gurwitz JH, Rochon P. Improving the quality of medication use in elderly patients: A not-so-simple prescription. Archives of Internal Medicine. 2002;162:1670–1672. doi: 10.1001/archinte.162.15.1670. [DOI] [PubMed] [Google Scholar]
- Hirsch JD, Gonzales M, Rosenquist A, Miller TA, Gilmer TP, Best BM. Antiretroviral therapy adherence, medication use, and health care costs during 3 years of a community pharmacy medication therapy management program for Medi-Cal beneficiaries with HIV/AIDS. Journal of Managed Care Pharmacy. 2011;17:213–223. doi: 10.18553/jmcp.2011.17.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JD, Oen A, Robertson S, Nguyen N, Daniels C. Patient request for pharmacist counseling and satisfaction: Automated prescription delivery system versus regular pick-up counter. Journal of the American Pharmacists Association. 2009;49:73–77. doi: 10.1331/JAPhA.2009.08037. [DOI] [PubMed] [Google Scholar]
- Hirsch JD, Rosenquist A, Best BM, Miller TA, Gilmer TP. Evaluation of the first year of a pilot program in community pharmacy: HIV/AIDS medication therapy management for Medi-Cal beneficiaries. Journal of Managed Care Pharmacy. 2009;15:32–41. doi: 10.18553/jmcp.2009.15.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohl CM, Nosyk B, Kuramoto L, Zed PJ, Brubacher JR, Abu-Laban RB, Sobolev B. Outcomes of emergency department patients presenting with adverse drug events. Annals of Emergency Medicine. 2011;58:270–279. doi: 10.1016/j.annemergmed.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Priority areas for national action: Transforming health care quality. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- John EJ, Vavra T, Farris K, Currie J, Doucette W, Button-Neumann B, Bullock T. Workplace-based cardiovascular risk management by community pharmacists: Impact on blood pressure, lipid levels, and weight. Pharmacotherapy. 2006;26:1511–1517. doi: 10.1592/phco.26.10.1511. [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: Development of a questionnaire for use in clinical trials. Thorax. 1992;47:76–83. doi: 10.1136/thx.47.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellerman R, Kirk L. Principles of the patient-centered medical home. American Family Physician. 2007;76:774–775. [PubMed] [Google Scholar]
- Kelly S, Melnyk BM, Belyea M. Predicting physical activity and fruit and vegetable intake in adolescents: A test of the information, motivation, behavioral skills model. Research in Nursing & Health. 2012;35:146–163. doi: 10.1002/nur.21462. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: Building a safer health system. National Academies Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- Kradjan WA, Schulz R, Christensen DB, Stergachis A, Sullivan S, Fullerton DS, Schneider G. Patients’ perceived benefit from and satisfaction with asthma-related pharmacy services. Journal of the American Pharmacists Association(Wash) 1999;39:658–666. doi: 10.1016/s1086-5802(15)30350-8. [DOI] [PubMed] [Google Scholar]
- Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: A comprehensive review. Advances in Therapy. 2005;22:313–356. doi: 10.1007/BF02850081. [DOI] [PubMed] [Google Scholar]
- MacKeigan LD, Larson LJ. Development and validation of an instrument to measure patient satisfaction with pharmacy services. Medical Care. 1989;27:522–536. doi: 10.1097/00005650-198905000-00007. [DOI] [PubMed] [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. New England Journal of Medicine. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–1111. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . Health, United States, 2011: With special feature on socioeconomic status and health. Government Printing Office; Hyattsville, MD: 2012. [PubMed] [Google Scholar]
- Nietert PJ, Tilley BC, Zhao W, Edwards PF, Wessell AM, Mauldin PD, Polk P. Two pharmacy interventions to improve refill persistence for chronic disease medications: A randomized, controlled trial. Medical Care. 2009;47:32–40. doi: 10.1097/MLR.0b013e3181808c17. [DOI] [PubMed] [Google Scholar]
- Nola KM, Gourley DR, Portner TS, Gourley GK, Solomon DK, Elam M, Regel B. Clinical and humanistic outcomes of a lipid management program in the community pharmacy setting. Journal of the American Pharmacists Association (Wash) 2000;40:166–173. doi: 10.1016/s1086-5802(16)31060-9. [DOI] [PubMed] [Google Scholar]
- Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC). Patient Education and Counseling. 2010;79:49–54. doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain setting. Journal of the American Pharmacists Association (Wash) 1996;36:443–451. doi: 10.1016/s1086-5802(16)30099-7. [DOI] [PubMed] [Google Scholar]
- Pinto SL, Lively BT, Siganga W, Holiday-Goodman M, Kamm G. Using the Health Belief Model to test factors affecting patient retention in diabetes-related pharmaceutical care services. Research in Social & Administrative Pharmacy. 2006;2:38–58. doi: 10.1016/j.sapharm.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hyper-tension medication therapy management program in patients with diabetes. Journal of the American Pharmacists Association. 2009;49:164–170. doi: 10.1331/JAPhA.2009.08164. [DOI] [PubMed] [Google Scholar]
- Rivet Amico K. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): An IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. Journal of Health Psychology. 2011;16:1071–1081. doi: 10.1177/1359105311398727. [DOI] [PubMed] [Google Scholar]
- Roberts AS, Benrimoj SI, Chen TF, Williams KA, Aslani P. Practice change in community pharmacy: Quantification of facilitators. Annals of Pharmacotherapy. 2008;42:861–868. doi: 10.1345/aph.1K617. [DOI] [PubMed] [Google Scholar]
- Samsa GP, Hanlon JT, Schmader KE, Weinberger M, Clipp EC, Uttech KM, Cohen HJ. A summated score for the Medication Appropriateness Index: Development and assessment of clinimetric properties including content validity. Journal of Clinical Epidemiology. 1994;47:891–896. doi: 10.1016/0895-4356(94)90192-9. [DOI] [PubMed] [Google Scholar]
- Shell DF, Newman IM, Perry CM, Folsom AR. Changing intentions to use smokeless tobacco: An application of the IMB model. American Journal of Health Behavior. 2011;35:568–580. doi: 10.5993/ajhb.35.5.6. [DOI] [PubMed] [Google Scholar]
- Smith LR, Fisher JD, Cunningham CO, Amico KR. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated Information, Motivation, Behavioral Skills Model of care initiation and maintenance. AIDS Patient Care and STDs. 2012;26:344–355. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SR, Clancy CM. Medication therapy management programs: Forming a new cornerstone for quality and safety in medicare. American Journal of Medical Quality. 2006;21:276–279. doi: 10.1177/1062860606290031. [DOI] [PubMed] [Google Scholar]
- Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, Harvey I. Dissemination and publication of research findings: An updated review of related biases. Health Technology Assessment. 2010;14(8):iii, ix–xi, 1–193. doi: 10.3310/hta14080. [DOI] [PubMed] [Google Scholar]
- Tierney WM, Overhage JM, Murray MD, Harris LE, Zhou XH, Eckert GJ, Wolinsky FD. Effects of computerized guidelines for outpatient management of ischemic heart disease and heart failure. Journal of General Internal Medicine. 1999;14(Suppl.):125. doi: 10.1111/j.1525-1497.2003.30635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong HA, Layson-Wolf C, de Bittner MR, Owen JA, Haupt S. Perceptions of patients on Medicare Part D medication therapy management services. Journal of the American Pharmacists Association. 2009;49:392–398. doi: 10.1331/JAPhA.2009.08008. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters LM, Treadwell JR. Assessing the risk of bias of individual studies in systematic reviews of health care interventions (Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews, AHRQ Publication No. 12-EHC047-EF) 2012 Retrieved from http://effectivehealthcare.ahrq.gov/ehc/products/322/998/MethodsGuideforCERs_Viswanathan_IndividualStudies.pdf.
- Ware JE, Kosinski M, Keller SD. SF-12: How to score the SF-12 Physical and Mental Health Summary Scales. QualityMetric; Lincoln, RI: 2000. [Google Scholar]
- Ware JE, Snyder ML, Wright WR, Davies AR. Defining and measuring patient satisfaction with medical care. Evaluation and Program Planning. 1983;6:247–263. doi: 10.1016/0149-7189(83)90005-8. [DOI] [PubMed] [Google Scholar]
- Weinberger M, Murray MD, Marrero DG, Brewer N, Lykens M, Harris LE, Tierney WM. Issues in conducting randomized controlled trials of health services research interventions in nonacademic practice settings: The case of retail pharmacies. Health Services Research. 2002a);37:1067–1077. doi: 10.1034/j.1600-0560.2002.66.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger M, Murray MD, Marrero DG, Brewer N, Lykens M, Harris LE, Tierney WM. Effectiveness of pharmacist care for patients with reactive airways disease: A randomized controlled trial. Journal of the American Medical Association. 2002b;288:1594–1602. doi: 10.1001/jama.288.13.1594. [DOI] [PubMed] [Google Scholar]
- Weingart SN, Simchowitz B, Padolsky H, Isaac T, Seger AC, Massagli M, Weissman JS. An empirical model to estimate the potential impact of medication safety alerts on patient safety, health care utilization, and cost in ambulatory care. Archives of Internal Medicine. 2009;169:1465–1473. doi: 10.1001/archinternmed.2009.252. [DOI] [PubMed] [Google Scholar]
- Worley MM, Schommer JC, Brown LM, Hadsall RS, Ranelli PL, Stratton TP, Uden DL. Pharmacists’ and patients’ roles in the pharmacist-patient relationship: Are pharmacists and patients reading from the same relationship script? Research in Social & Administrative Pharmacy. 2007;3:47–69. doi: 10.1016/j.sapharm.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Zarani F, Besharat MA, Sadeghian S, Sarami G. The effectiveness of the information-motivation-behavioral skills model in promoting adherence in CABG patients. Journal of Health Psychology. 2010;15:828–837. doi: 10.1177/1359105309357092. [DOI] [PubMed] [Google Scholar]
- Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). Journal of General Internal Medicine. 2005;20:1091–1096. doi: 10.1111/j.1525-1497.2005.0226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]