Abstract
Study Objective
Language barriers are known to negatively impact many health outcomes among limited English proficiency (LEP) patient populations, but little is known about the quality of care LEP patients receive in the Emergency Department (ED). This study seeks to determine if LEP patients experience different quality of care than English speaking patients in the ED, using unplanned revisit within 72 hours as a surrogate quality indicator.
Methods
We conducted a retrospective cohort from an urban adult ED in calendar year 2012; with a total of 41,772 patients and 56,821 ED visits. We compared 2,943 limited English proficiency patients with 38,829 English speaking patients presenting to ED after excluding patients with psychiatric complaints, altered mental status, non-verbal states, and patients with more than four ED visits in 12 months. Two main outcomes—the risk of inpatient admission from the ED, and risk of unplanned ED revisit within 72 hours—were measured using odds ratios from generalized estimating equation multivariate models.
Results
LEP patients were more likely than English speakers to be admitted (32.0% vs. 27.2%, OR 1.20, 95% CI 1.11-1.30), this association became non-significant after adjustments (OR=1.04, 95% CI 0.95-1.15). 32,857 patients with 45,546 ED visits were included in the ED revisit within 72 hours analysis. 4.2% of all patients (n=1,380) had at least one unplanned revisit. LEP patients were more likely than English speakers to have an unplanned revisit (5.0% vs. 4.1%, OR=1.19, 95% CI 1.02-1.45). This association persisted (OR=1.24, 95% CI 1.02-1.53) after adjustment for potential confounders including insurance status.
Conclusions
We found no difference in hospital admission rates between limited English proficiency patients and English speaking patients. Yet, limited English proficiency patients were 24% more likely to have an unplanned ED revisit within 72 hours, with an absolute difference of 0.9%, suggesting challenges in ED quality of care.
INTRODUCTION
Background
About 55 million people in the United States do not speak English as their primary language and more than 24 million people speak English less than “very well” and are considered as having limited English proficiency (LEP).1 Healthcare providers, including those in Emergency Departments, are required by federal and state laws to provide free language interpreting services (LIS) for patients who have LEP.2,3 The Joint Commission’s Patient-Centered Communication Standards RC.02.01.01 effective July 1, 2012, require organizations to keep medical records containing patient’s race, ethnicity, communication needs, and preferred language.4,5 While these mandates are important steps in being able to address disparities in health care, prior studies have shown that many healthcare providers do not offer adequate LIS.6 Physicians’ tendency to underuse interpreter services even when available, compounded with high level of variation in interpreter training when LIS are offered, further complicate clinical encounters for LEP patients.7-15 Language barriers may be particularly challenging in the ED, where patients’ visits are by nature unscheduled, potentially making it more difficult to provide LIS, and the LEP patient population may be at risk for lower quality ED care.16-22
Importance
A major challenge in examining the ED care received by LEP patients is the lack of a clear clinically relevant quality indicator of ED cares more generally. Previous studies have used admission rate as a surrogate marker for quality of care for LEP patients, yet admission rates can vary as an instance of protective measures by ED physicians who appropriately fear that language barriers may complicate follow up.23-26 The National Quality Forum (NQF) has proposed unplanned ED revisit within 72 hours of ED discharge as an e-Quality measure.27-32 Despite its obvious limitations—a revisit is not a simple reflection of the care received during the initial visit; it may be due to disease progression despite appropriate care, or lack of access to needed outpatient care, the rate of unplanned ED revisit within 72 hours of discharge from an ED is becoming widely accepted as a general indicator of quality of ED care.27-31
Goal of This Investigation
The relationship between patients’ LEP status and unplanned ED revisit within 72 hours of discharge is not known. We used data from a minority serving urban tertiary medical center ED to evaluate the association between patient LEP status and unplanned ED revisit within 72 hours. Recognizing that unplanned ED revisits may result from lower rates of initial hospital admission, which could also be due to language barriers in the index visit, we also examined the association between LEP status and hospital admission.
MATERIALS AND METHODS
Study Design and Setting
A retrospective cohort study was conducted for all patients presenting to the adult ED at Mount Sinai Hospital—a tertiary medical center in New York City—between January 1, 2012, and December 31, 2012. The ED provides care for a socio-economically and racially diverse patient population, with approximately 100,000 annual visits. Data were obtained for review from the Epic electronic health record (EHR) Reporting Workbench—an operational reporting application. The Institutional Review Boards at the Icahn School of Medicine at Mount Sinai approved this study.
Selection of Participants
Patients with psychiatric, substance related, or altered mental status chief complaints were excluded using validated computerized text-parsing algorithm software, Coded Chief Complaints for Emergency Department Systems (CCC-EDS version 7.1).33 We also excluded patients who were dead on arrival, non-verbal due to disease severity, and those missing key administrative data (i.e. patient’s language preference). Finally, we excluded patients with more than four ED visits in the calendar year—the most widely used definition of ED frequent user—from our main analysis as they represent a unique population of superutilizers that may bias our outcomes of interest.34-39
For the unplanned ED revisit within 72 hours analysis, we further excluded patients who presented to the ED within 30 days of a hospital admission as their revisit may be related to care transitions that are beyond the scope of ED practice.40 Finally, we excluded patients with a planned ED revisit denoted by the following primary diagnosis codes: V58 (encounter for other unspecified procedures and aftercare), V67 (follow-up examination), and V04 (need for prophylactic vaccination and inoculation against certain viral diseases) based on the International Classification of Diseases, Ninth Revision, Clinical Modification41
Outcome Measures
The two primary outcomes for this study were risk-adjusted odds of all-cause admission and risk-adjusted odds of all-cause unplanned ED revisit within 72 hours. Unplanned ED revisit within 72 hours was defined as the first unplanned ED visit less than 72 hours from an index treat-and-release ED visit discharge.27-32
For each patient, the following information was available: age, sex, race (White, Black, Asian, other), Ethnicity (Hispanic, non-Hispanic), patient’s language preference, provider documented interpreter usage, emergency severity index (ESI) categories (a scale of 1 to 5 assigned by nursing staff at triage based on the urgency and seriousness of the patient’s presentation), and an updated Charlson Comobidity Score (CCS).42 CCS was calculated for each patient using all available diagnoses entered into the EHR since its inception in June, 2011. We defined LEP status by using the ED code on patient language preference, coded as English vs. non-English.
Analysis
We first described the characteristics of LEP patients and English-speaking patients for the admission as well as unplanned ED revisit within 72 hours analysis. After describing the characteristics of LEP and English speaking patients we compared patients with and without hospital admission, as well as patients with and without unplanned ED revisit within 72 hours on each variable using Wilcoxon tests for continuous data and χ2 tests for categorical data. For our primary outcomes, we used generalized estimating equation (GEE) models with logit link and binomial distribution to assess the independent association with LEP status while incorporating clustering by patients. GEE approach is often used in longitudinal data analysis, while this method behaves robustly against misspecification of the working correlation structure.43,44 The GEE method was used to account for the repeated longitudinal nature of patients on both primary outcomes because some patients had more than two visits within the study period. We began with unadjusted analysis of associations between odds of admission, with each of the patient demographic and clinical characteristics listed above and then repeated this analysis for the second outcome of unplanned ED revisit within 72 hours. Final models were selected after excluding variables with strong collinearity (i.e. interpreter use and LEP status) and testing of interaction terms between language and race. Model fitting was achieved by using various working correlation matrices to achieve best quasi-likelihood under the independence model criterion (QIC).45 Data were analyzed using Statistical Analysis Software (SAS) version 9.4 (SAS Institute, Cary, NC).
RESULTS
Characteristics of Study Subjects
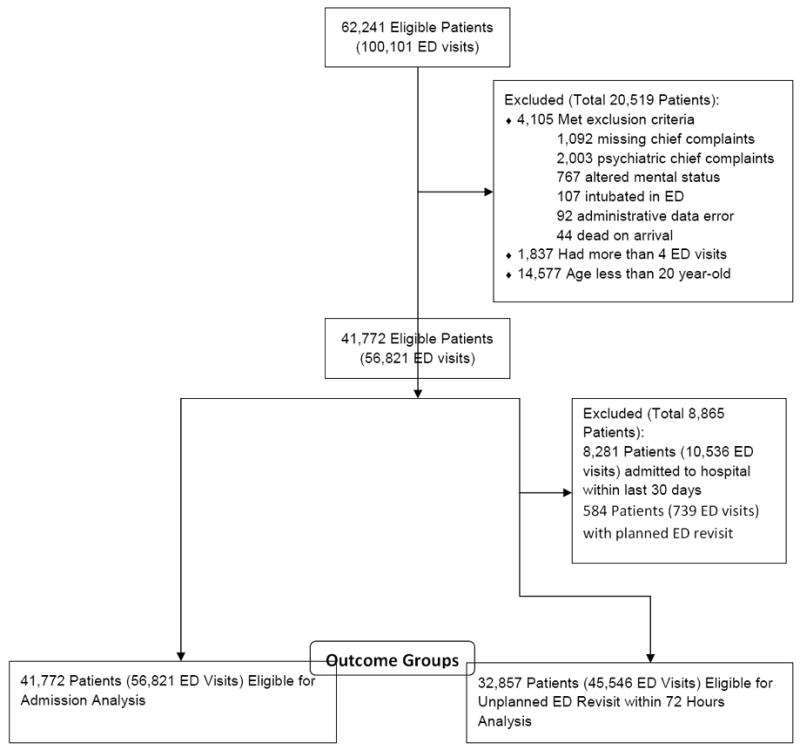
In the calendar year of 2012, 62,241 patients with 100,101 visits to the emergency department were reviewed. For the admission analysis, 20,469 patients were excluded based on the exclusion criteria, resulting in 41,772 adult patients with 56,821 ED visits. For the unplanned ED revisit within 72 hours analysis, we further excluded 8,865 patients; resulting in 32,857 patients and 45,546 ED visits (Figure 1).
Figure 1. Flow of Participants through Inclusion and Exclusion Criteria.
Overall, 2,943 patients (7.1%) had LEP; resulting in 4,225 ED visits (Table 1). Of these visits, interpreter usage, which could include family members or ED staff, was documented in 2,209 visits (52.3%). In 527 (23.9%) of these visits, a professional interpreter was documented as involved.
Table 1.
Demographic and Baseline Patient Characteristics for Limited English Proficiency vs. English-Speaking Patients at Index Visit.
| Characteristic | Admission Analysis
|
Unplanned ED Revisit within 72 hours Analysis
|
||||
|---|---|---|---|---|---|---|
| LEP | English-Speaking | Total | LEP | English-Speaking | Total | |
| No. (% of total) | 2,943 (7.1) | 38,779 (92.9) | 41,722 (100.0) | 2,282 (6.9) | 30,575 (93.1) | 32,857 (100.0) |
| Age, mean (SD), y | 55.5 (19.1) | 48.0 (19.4) | 48.6 (19.4) | 53.0 (18.8) | 45.0 (18.2) | 45.5 (18.4) |
| Sex No. (Column %) | ||||||
| Men | 1,119 (38.0) | 16,181 (41.7) | 17,300 (41.5) | 813 (35.6) | 12,095 (39.6) | 12,908 (39.3) |
| Women | 1,824 (62.0) | 22,596 (58.3) | 24,420 (58.5) | 1,469 (64.4) | 18,478 (60.4) | 19,947 (60.7) |
| Insurance, No. (Column %) | ||||||
| Medicaid | 264 (9.0) | 2,716 (7.0) | 2,980 (7.1) | 180 (7.9) | 2,090 (6.8) | 2,270 (6.9) |
| Medicare | 844 (28.7) | 7,707 (19.9) | 8,551 (20.5) | 568 (24.9) | 4,618 (15.1) | 5,186 (15.8) |
| Private | 927 (31.5) | 18,503 (47.7) | 19,430 (46.6) | 783 (34.3) | 15,653 (51.2) | 16,436 (50.0) |
| Uninsured | 869 (29.5) | 9,246 (23.8) | 10,115 (24.2) | 721 (31.6) | 7,700 (25.2) | 8,421 (25.6) |
| Missing | 39 (1.3) | 607 (1.6) | 646 (1.5) | 30 (1.3) | 514 (1.7) | 544 (1.7) |
| Race, No. (Column %) | ||||||
| Asian | 147 (5.0) | 922 (2.4) | 1,069 (2.7) | 78 (3.4) | 656 (2.1) | 734 (2.2) |
| Black | 91 (3.1) | 12,580 (32.4) | 12,671 (31.5) | 79 (3.5) | 10,708 (35.0) | 10,787 (32.8) |
| White | 163 (5.5) | 9,633 (24.8) | 9,796 (24.3) | 85 (3.7) | 6,194 (20.3) | 6,279 (19.1) |
| Other | 2,475 (84.1) | 14,240 (36.7) | 16,715 (41.5) | 1,993 (87.3) | 11,993 (39.2) | 13,986 (42.6) |
| Missing | 67 (2.3) | 1,404 (3.6) | 1,471 (3.7) | 47 (2.1) | 1,024 (3.3) | 1,071 (3.3) |
| Ethnicity, No. (Column %) | ||||||
| Hispanic | 2,325 (79.0) | 11,512 (29.7) | 13,837 (33.2) | 1,870 (81.9) | 9,890 (32.3) | 11,760 (35.8) |
| Non-Hispanic | 511 (17.4) | 23,438 (60.4) | 23,949 (57.4) | 334 (14.6) | 17,803 (58.2) | 18,137 (55.2) |
| Missing | 107 (3.6) | 3,829 (9.9) | 3,936 (9.4) | 78 (3.4) | 2,882 (9.4) | 2,960 (9.0) |
| Charlson Comorbidity Score, mean (SD) | 0.39 (1.11) | 0.26 (0.91) | 0.27 (0.92) | 0.27 (0.91) | 0.16 (0.69) | 0.17 (0.71) |
Table 2 shows demographic and clinical characteristics of patients at their index visit. 11,495 (27.6%) patients had at least one hospital admission during the study period. Patients with at least one hospital admission had a higher mean age (60.7 vs. 43.9, P<.01) and higher CCS (0.83 vs. 0.05, P<.01) than patients who were never admitted to the hospital. For the unplanned ED revisit within 72 hours analysis, 1,380 patients (4.2%) had at least one unplanned revisit. Patients who had at least one unplanned ED revisit within 72 hours had a somewhat lower mean age (44.1 vs. 45.6, P<.01) and higher CCS (0.27 vs.0 .16, P<.01) than patients who had no unplanned ED revisit within 72 hours.
Table 2.
Demographic and Baseline Patient Characteristics for Admission and ED Revisit within 72 hours Analysis at Index Visit
| Characteristic | Admission to Hospital
|
Unplanned ED Revisit within 72 hours
|
||||
|---|---|---|---|---|---|---|
| No | Yes | Total | No | Yes | Total | |
| No. (% of total) | 30,227 (72.4) | 11,495 (27.6) | 41,722 (100.0) | 31,477 (95.8) | 1,380 (4.2) | 32,857 (100.0) |
| Age, mean (SD), y | 43.9 (17.5) | 60.7 (18.9) | 48.6 (19.4) | 45.6 (18.3) | 44.1 (18.7) | 45.5 (18.4) |
| Sex No. (Column %) | ||||||
| Men | 11,839 (39.2) | 5,461 (47.5) | 17,300 (41.5) | 12,340 (39.2) | 568 (41.2) | 12,908 (39.3) |
| Women | 18,386 (60.8) | 6,034 (52.5) | 24,420 (58.5) | 19,135 (60.8) | 812 (58.8) | 19,947 (60.7) |
| Insurance, No. (Column %) | ||||||
| Medicaid | 1,976 (6.5) | 1,004 (8.7) | 2,980 (7.1) | 2,137 (6.8) | 133 (9.6) | 2,270 (6.9) |
| Medicare | 4,048 (13.4) | 4,503 (39.2) | 8,551 (20.5) | 4,957 (15.7) | 229 (16.6) | 5,186 (15.8) |
| Private | 15,738 (52.1) | 3,692 (32.1) | 19,430 (46.6) | 15,747 (50.0) | 689 (49.9) | 16,436 (50.0) |
| Uninsured | 7,928 (26.2) | 2,187 (19.0) | 10,115 (24.2) | 8,099 (25.7) | 322 (23.3) | 8,421 (25.6) |
| Missing | 537 (1.8) | 109 (0.9) | 646 (1.5) | 537 (1.7) | 7 (0.5) | 544 (1.7) |
| Race, No. (Column %) | ||||||
| Asian | 660 (2.2) | 409 (3.6) | 1,069 (2.7) | 709 (2.3) | 25 (1.8) | 734 (2.2) |
| Black | 9,997 (33.1) | 2,674 (23.3) | 12,671 (31.5) | 10,304 (32.7) | 483 (35.0) | 10,787 (32.8) |
| White | 5,518 (18.3) | 4,278 (37.2) | 9,796 (24.3) | 6,049 (19.2) | 230 (16.7) | 6,279 (19.1) |
| Other | 13,045 (43.2) | 3,670 (31.9) | 16,715 (41.5) | 13,366 (42.5) | 620 (44.9) | 13,986 (42.6) |
| Missing | 1,007 (3.3) | 464 (4.0) | 1,471 (3.7) | 1,049 (3.3) | 22 (1.6) | 1,071 (3.3) |
| Ethnicity, No. (Row %) | ||||||
| Hispanic | 10,937 (79.0) | 2,900 (21.0) | 13,837 | 11,218 (95.4) | 542 (4.6) | 11,760 |
| Non-Hispanic | 16,421 (68.6) | 7,528 (31.4) | 23,949 | 17,340 (95.6) | 797 (4.4) | 18,137 |
| Missing | 2,869 (72.9) | 1,067 (27.1) | 3,936 | 2,919 (98.6) | 41 (1.4) | 2,960 |
| Language, No. (Row %) | ||||||
| Limited English Proficiency | 2,000 (68.0) | 943 (32.0) | 2,943 | 2,167 (95.0) | 115 (5.0) | 2,282 |
| English-speaking | 28,227 (72.8) | 10,552 (27.2) | 38,779 | 29,310 (95.9) | 1,265 (4.1) | 30,575 |
| Charlson Comorbidity Score, mean (SD) | 0.05 (0.27) | 0.83 (1.56) | 0.27 (0.92) | 0.16 (0.70) | 0.27 (0.87) | 0.17 (0.71) |
Main Results
Table 3 displays the association of LEP status for admission and for unplanned ED revisit within 72 hours in both unadjusted and adjusted models. The unadjusted odds ratio between LEP status and hospital admission was 1.20 (95% CI 1.11-1.30). After adjusting for age, sex, insurance, race, ethnicity, triage category, and CCS, the association was non-significant, AOR 1.04 (95% CI 0.95-1.15).
Table 3.
GEE models for predictors on admission and Unplanned ED Revisit within 72 hours
| Admission to Hospital
|
Unplanned ED Revisit within 72 Hours
|
|||
|---|---|---|---|---|
| Univariate
|
Complete Model
|
Univariate
|
Complete Model
|
|
| OR (95%) | OR (95%) | OR (95%) | OR (95%) | |
| Age | 1.05 (1.05-1.05) | 1.03 (1.02-1.03) | 0.99 (0.99-1.00) | 0.99 (0.98-1.00) |
| Sex | ||||
| Men | 1.44 (1.38-1.51) | 1.32 (1.25-1.39) | 1.12 (1.01-1.25) | 1.15 (1.03-1.28) |
| Women | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Insurance | ||||
| Medicaid | 1.98 (1.83-2.15) | 1.49 (1.35-1.65) | 1.20 (1.00-1.44) | 1.19 (0.98-1.44) |
| Medicare | 4.28 (4.06-4.52) | 1.20 (1.10-1.30) | 0.93 (0.80-1.08) | 1.19 (0.98-1.45) |
| Private | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Uninsured | 1.19 (1.12-1.26) | 0.85 (0.79-0.91) | 0.93 (0.82-1.06) | 0.96 (0.83-1.10) |
| Race | ||||
| Asian | 0.64 (0.72-0.92) | 0.95 (0.82-1.10) | 0.98 (0.65-1.47) | 0.93 (0.61-1.42) |
| Black | 0.32 (0.30-0.34) | 0.42 (0.39-0.45) | 1.08 (0.92-1.26) | 0.99 (0.84-1.17) |
| White | 1.00 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Other | 0.33 (0.32-0.35) | 0.58 (0.53-0.64) | 1.07 (0.92-1.25) | 0.89 (0.70-1.13) |
| Ethnicity | ||||
| Hispanic | 0.55 (0.52-0.58) | 0.65 (0.59-0.71) | 1.01 (0.90-1.12) | 1.08 (0.87-1.34) |
| Non-Hispanic | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Language | ||||
| Limited English Proficiency | 1.20 (1.11-1.30) | 1.04 (0.95-1.15) | 1.19 (1.02-1.48) | 1.24 (1.02-1.53) |
| English-speaking | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Triage Category | ||||
| Immediate | 494.97 (234.3-1045.7) | 229.04 (91.7-572.0) | Excluded | Excluded |
| Emergent | 97.41 (65.9-146.2) | 51.29 (31.0-84.9) | 0.33 (0.24-0.45) | 0.33 (0.24-0.46) |
| Urgent | 33.20 (22.2-49.8) | 21.06 (12.7-34.8) | 0.53 (0.40-0.59) | 0.53 (0.41-0.70) |
| Semiurgent | 2.72 (1.81-4.09) | 2.43 (1.46-4.03) | 0.43 (0.32-0.56) | 0.43 (0.33-0.57) |
| Nonurgent | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Charlson Comorbidity Score | 2.48 (2.39-2.58) | 1.90 (1.83-1.97) | 1.01 (0.95-1.06) | 1.01 (0.96-1.07) |
Patients with LEP had an odds ratio of 1.19 (95% CI 1.02-1.48) in unadjusted association with unplanned ED revisit within 72 hours. This association became stronger after adjusting for age, sex, insurance, race, ethnicity, triage category, and CCS with an odds ratio of 1.24 (95% CI 1.02-1.53). Of note, older age and higher acuity triage category were strong predictors of hospital admission and were protective against unplanned ED revisit within 72 hours.
LIMITATIONS
Our study has several limitations. First, our data were derived from a single center. Currently, large national ED databases like the National Hospital Ambulatory Medical Care Survey (NHAMCS), and the Healthcare Cost and Utilization Project (HCUP) do not contain data on patient’s preferred language. Our institutional data did allow us to collect patient level information including language and reason for return visit. Nonetheless, results from this single site study cannot necessarily be generalized to disparate clinical settings.
Second, we defined limited English proficiency based on patient’s self-reported preferred language as coded in the ED administrative database; our study did not assess patients or physicians actual language skills. As a result of our definition, our study might conflate general language proficiency and English proficiency. In some cases, a person’s poor communication may result from poor overall language proficiency. In other cases, this is linked to education and social economic status that are beyond the ability of our study to detect. In this retrospective study design, we were unable to evaluate patient’s health literacy. Limited health literacy, separated from language proficiency, might be prevalent among LEP patients and could impact and confound findings. While we obtained insurance status in our study as a surrogate of social economic status, it was not a direct measurement of patient’s social resources. In addition, documentation of professional LIS usage did not guarantee LIS was used without direct observation. Resident physicians have been observed to misreport their LIS usage in an observational study.15 Accessing LIS usage among those with LEP would be a more ideal proximal risk factor for our outcomes; however, missing data regarding whether professional LIS was used, together with the collinearly between LIS and LEP status limited our ability to answer the correlation between LIS usage and our outcomes directly. Finally, patients chose a primary language other than English may still be proficient in English, or family members might have served as ad hoc interpreters, or some physicians might have provided language-concordant care to their LEP patients; these cases would have biased our results toward the null.46 Given the above reasons, LEP status only represented one of the many risk factors in admissions and ED revisit within 72 hours.
Third, we used the Charlson Comobidity Score to adjust for comorbidity; the score was calculated using all available diagnoses in our EHR system since its inception. A previous admission could result in better capture of comorbidities, and a higher score compared to similar patients without a prior admission. This is important for the hospital admission analysis, as CCS significantly affects estimates of the association between LEP status and admissions. On the other hand, CCS has little effect on the analysis of the relationship between LEP status and unplanned ED revisit within 72 hours and this potential bias should not impact our results.
Finally, ED revisit within 72 hours may not be due to quality of care issues in the first visit, but may result from the natural progression of disease, or other unmeasurable factors. Unplanned ED revisit within 72 hours, while widely viewed as a marker of quality of care in the ED, has not been proven to have an impact on patient outcomes and may not be a true reflection of the quality of care received in the ED. Therefore, 72-hour return visits are controversial as a measure of quality of care in the ED. It may instead reflect differential opportunities to access primary care or community based care. In addition, the lack of patient’s accessibility to primary care providers in our data further limited our understanding of whether these observed increase in 72-hours return visits are due to lack of primary care provider’s access, or truly an issue with quality of care in the ED. Finally, our data did not address patients returning to a different ED. From a recent study using communitywide data from a health information exchange for 4 EDs, it was found that 3% of all ED users visit more than one ED in the New York City area in a twelve-month period after excluding ED frequent users similar to our study definition. However, unplanned 72-hour revisit among LEP population across the hospital system is still unknown at this point.47 Furthermore, LEP status is not routinely collected in EHR prior to the Joint Commission’s Patient-Centered Communication Standards RC.02.01.01 effective July 1, 2012.4,5 The lack of knowledge between LEP vs. non-LEP patients pattern in visiting another ED in the area, resulted as a potentially significant confounder.
DISCUSSION
Our study is the largest study to date examining the association of limited English proficiency and a quality of care indicator in Emergency Medicine. We found that limited English proficiency patients were more likely than English speakers to have an unplanned revisit (5.0% vs. 4.1%). This association persisted after adjusting for potential confounders with an adjusted odds ratio of 1.24 (95% CI 1.02-1.53).
Studies on the quality of emergency department care experienced by LEP patients are limited, yet taken together they suggest that language barriers complicated many aspects of care. Studies have documented less comprehension of ED discharge instructions, less referral for follow up appointment, and less satisfaction with ED care when care is delivered across a language barrier.6,48-50 Studies in other settings have shown that language barriers are associated with poorer self-management, medical errors, and worse clinical outcomes.6,11,13,20,51 While access to language interpreting services critical to effective communication, multiple studies have shown substantial under-utilization of in clinical settings.6,15 In our study, professional LIS was documented to be provided for less than a quarter of the LEP patients. While this usage of LIS services may appear low, it is consistent with other prospective ED studies that report an LIS utilization rate between 12% and 18%6,9,11,17
Rate of unplanned ED revisits is a widely used quality measure in emergency care, with a range of 0.4% to 4.9% reported in previous studies.27,28,30,31,52 Similar to our study, a recent pediatric ED study showed similar association between LEP patients and rate of unplanned revisit to the ED in the Boston area.52 Yet, the definition of an “ED revisit” varies between researchers, with some reporting on 24-hour revisits and some on 7-day revisits. In addition, previous studies did not establish clear exclusion criteria. One such important exclusion criteria is admitted patients. A competing risk exists between ED admission and ED revisit. Patients who were admitted to the hospital cannot—by definition—have an ED revisit, which is usually defined as a revisit after discharge from the ED. In our study, we used the more conservative 72 hours definition after excluding admitted patients, and found that LEP status is an independent risk factor for unplanned ED revisit within 72 hours. We chose to exclude patients with a hospital admission within 30 days of ED visit in order to focus on the bulk of patients with LEP. Our finding that older age and higher triage score are protective for unplanned ED revisit within 72 hours likely results from this aspect of our study design, as these high risk patients were likely excluded in our analysis.
We found no association between patients’ language status and hospital admission rate. Previous studies, with smaller sample sizes and inability to of adjust for clinical risk factors like comorbidity, have reported conflicting results.21,22,25 While our unadjusted analyses showed that LEP patients had a higher admission rate than English speaking patients, this relationship disappeared after adjusting for other known risk factors for admission.
In conclusion, we found that limited English proficiency is a risk factor for unplanned ED 72 hour revisits for adult patients who presented to an urban tertiary academic Emergency Department. We also note low usage of language interpreting services. Further studies are needed to assess the quality of care provided in the ED and if consistent use of professional interpreters by ED physicians during clinical encounters reduces unplanned ED revisits for LEP patients.
Acknowledgments
We thank Drs. Charles DiMaggio and Gary Winkel for their statistical expertise. We also thank Dr. David Thompson for his assistance with the computerized text-parsing algorithm software Coded Chief Complaints for Emergency Department Systems (CCC-EDS version 7.1).
Grant:
KMN received a career development award from NIH National Heart Lung and Blood Institutes (NHLBI) 5K12HL109005.
Footnotes
Author Contributions
KMN, LDR, and AF were responsible for conception and design of the study. LDR and AF supervised the conduct of the study. KMN managed the data. KMN and RL provided statistical advice on study design and analyzed the data. KMN and AL drafted the article, and all authors contributed substantially to its revision. KMN takes responsibility for the paper as a whole.
Meetings
We presented an earlier version of the results as a poster at Society for Academic Emergency Medicine Annual Meeting in Dallas, Texas, in May 2014.
Conflicts of Interest
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shin H, Kominski R. Language Use in the United States: 2007. [November 12, 2011];2010 http://www.census.gov/prod/2010pubs/acs-12.pdf.
- 2.42 U.S.C. §2000d. 1964 [Google Scholar]
- 3.Services USDoHH. The National CLAS Standards. [July 1st, 2013]; http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15.
- 4.The Joint Commission: R3 Report Requirement, Rationale, Reference. 2011;(1) [Google Scholar]
- 5.The Joint Commission: Advancing Effective Communication, Cultural Competence, and Patient and Family-Centered Care: A Roadmap for Hospitals. 2010 [Google Scholar]
- 6.Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. Journal of health care for the poor and underserved. 2008 May;19(2):352–362. doi: 10.1353/hpu.0.0019. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez A. Improving the quality of informed consent: it is not all about the risks. Annals of internal medicine. 2010 Sep 7;153(5):342–343. doi: 10.7326/0003-4819-153-5-201009070-00011. [DOI] [PubMed] [Google Scholar]
- 8.Chen AH, Youdelman MK, Brooks J. The legal framework for language access in healthcare settings: Title VI and beyond. Journal of general internal medicine. 2007 Nov;22(Suppl 2):362–367. doi: 10.1007/s11606-007-0366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ginde AA, Clark S, Camargo CA., Jr Language barriers among patients in Boston emergency departments: use of medical interpreters after passage of interpreter legislation. Journal of immigrant and minority health / Center for Minority Public Health. 2009 Dec;11(6):527–530. doi: 10.1007/s10903-008-9188-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ku L, Flores G. Pay now or pay later: providing interpreter services in health care. Health affairs. 2005;24(2):435–444. doi: 10.1377/hlthaff.24.2.435. [DOI] [PubMed] [Google Scholar]
- 11.Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA : the journal of the American Medical Association. 1996 Mar 13;275(10):783–788. [PubMed] [Google Scholar]
- 12.Bernstein J, Bernstein E, Dave A, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J Immigr Health. 2002 Oct;4(4):171–176. doi: 10.1023/A:1020125425820. [DOI] [PubMed] [Google Scholar]
- 13.Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Annals of emergency medicine. 2012 Nov;60(5):545–553. doi: 10.1016/j.annemergmed.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Schenker Y, Fernandez A, Sudore R, Schillinger D. Interventions to improve patient comprehension in informed consent for medical and surgical procedures: a systematic review. Medical decision making : an international journal of the Society for Medical Decision Making. 2011 Jan-Feb;31(1):151–173. doi: 10.1177/0272989X10364247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. Journal of general internal medicine. 2009 Feb;24(2):256–262. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do Professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? A Systematic Review of the Literature. Health services research. 2007 Apr;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. Journal of general internal medicine. 2007 Nov;22(Suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Medical care research and review : MCRR. 2005 Jun;62(3):255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of Interpreter Services on Delivery of Health Care to Limited–English-proficient Patients. Journal of general internal medicine. 2001 Jul;16(7):468–474. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) Journal of general internal medicine. 2011 Feb;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hampers L, McNulty J. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Archives of pediatrics & adolescent medicine. 2002;156(11):1108–1113. doi: 10.1001/archpedi.156.11.1108. [DOI] [PubMed] [Google Scholar]
- 22.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6):1253–1256. doi: 10.1542/peds.103.6.1253. [DOI] [PubMed] [Google Scholar]
- 23.Lee ED, Rosenberg CR, Sixsmith DM, Pang D, Abularrage J. Does a physician-patient language difference increase the probability of hospital admission? Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 1998 Jan;5(1):86–89. doi: 10.1111/j.1553-2712.1998.tb02585.x. [DOI] [PubMed] [Google Scholar]
- 24.Rogers AJ, Delgado CA, Simon HK. The effect of limited English proficiency on admission rates from a pediatric ED: stratification by triage acuity. Am J Emerg Med. 2004 Nov;22(7):534–536. doi: 10.1016/j.ajem.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Waxman MA, Levitt MA. Are diagnostic testing and admission rates higher in non-Englishspeaking versus English-speaking patients in the emergency department? Annals of emergency medicine. 2000 Nov;36(5):456–461. doi: 10.1067/mem.2000.108315. [DOI] [PubMed] [Google Scholar]
- 26.Jacobs EA, Fu PC, Jr, Rathouz PJ. Does a Video-Interpreting Network Improve Delivery of Care in the Emergency Department? Health services research. 2011 Oct 18; doi: 10.1111/j.1475-6773.2011.01329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu SC. Analysis of patient revisits to the emergency department. Am J Emerg Med. 1992 Jul;10(4):366–370. doi: 10.1016/0735-6757(92)90022-p. [DOI] [PubMed] [Google Scholar]
- 28.Keith KD, Bocka JJ, Kobernick MS, Krome RL, Ross MA. Emergency department revisits. Annals of emergency medicine. 1989 Sep;18(9):964–968. doi: 10.1016/s0196-0644(89)80461-5. [DOI] [PubMed] [Google Scholar]
- 29.Kelly AM, Chirnside AM, Curry CH. An analysis of unscheduled return visits to an urban emergency department. The New Zealand medical journal. 1993 Aug 11;106(961):334–336. [PubMed] [Google Scholar]
- 30.Lerman B, Kobernick MS. Return visits to the emergency department. J Emerg Med. 1987 Sep-Oct;5(5):359–362. doi: 10.1016/0736-4679(87)90138-7. [DOI] [PubMed] [Google Scholar]
- 31.Pierce JM, Kellerman AL, Oster C. “Bounces”: an analysis of short-term return visits to a public hospital emergency department. Annals of emergency medicine. 1990 Jul;19(7):752–757. doi: 10.1016/s0196-0644(05)81698-1. [DOI] [PubMed] [Google Scholar]
- 32.JS S. Advancing Quality Measurement and Care Improvement with Health Information Exchange. [April 24, 2013];2012 http://healthit.ahrq.gov/ahrq-funded-projects/advancing-quality-measurement-and-careimprovement-health-information-exchange.
- 33.Thompson DA, Eitel D, Fernandes CM, Pines JM, Amsterdam J, Davidson SJ. Coded Chief Complaints--automated analysis of free-text complaints. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2006 Jul;13(7):774–782. doi: 10.1197/j.aem.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Doupe MB, Palatnick W, Day S, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Annals of emergency medicine. 2012 Jul;60(1):24–32. doi: 10.1016/j.annemergmed.2011.11.036. [DOI] [PubMed] [Google Scholar]
- 35.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Annals of emergency medicine. 2006 Jul;48(1):1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 36.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Annals of emergency medicine. 2010 Jul;56(1):42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 37.Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: real-time identification and remediable risks. Journal of urban health : bulletin of the New York Academy of Medicine. 2009 Mar;86(2):230–241. doi: 10.1007/s11524-008-9336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weber EJ. Defining frequent use: the numbers no longer count. Annals of emergency medicine. 2012 Jul;60(1):33–34. doi: 10.1016/j.annemergmed.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 39.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Medical care. 2004 Feb;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 40.Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA : the journal of the American Medical Association. 2013 Jan 23;309(4):364–371. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.CDC. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) [November 26, 2013];2013 http://www.cdc.gov/nchs/icd/icd9cm.htm.
- 42.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. American journal of epidemiology. 2011 Mar 15;173(6):676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 43.Westgate PM. Criterion for the simultaneous selection of a working correlation structure and either generalized estimating equations or the quadratic inference function approach. Biometrical journal Biometrische Zeitschrift. 2014 May;56(3):461–476. doi: 10.1002/bimj.201300098. [DOI] [PubMed] [Google Scholar]
- 44.Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 45.Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001 Mar;57(1):120–125. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- 46.Gee GC, Walsemann KM, Takeuchi DT. English proficiency and language preference: testing the equivalence of two measures. American journal of public health. 2010 Mar;100(3):563–569. doi: 10.2105/AJPH.2008.156976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Garg N, Kuperman G, Onyile A, et al. Validating Health Information Exchange (HIE) Data For Quality Measurement Across Four Hospitals. AMIA … Annual Symposium proceedings / AMIA Symposium AMIA Symposium; 2014. pp. 573–579. [PMC free article] [PubMed] [Google Scholar]
- 48.Gany F, Leng J, Shapiro E, et al. Patient satisfaction with different interpreting methods: a randomized controlled trial. Journal of general internal medicine. 2007 Nov;22(Suppl 2):312–318. doi: 10.1007/s11606-007-0360-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. Journal of general internal medicine. 2000 Apr;15(4):256–264. doi: 10.1111/j.1525-1497.2000.06469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. Journal of general internal medicine. 1999 Feb;14(2):82–87. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 51.Wisnivesky JP, Krauskopf K, Wolf MS, et al. The association between language proficiency and outcomes of elderly patients with asthma. Annals of Allergy, Asthma & Immunology. 2012;109(3):179–184. doi: 10.1016/j.anai.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 52.Gallagher RA, Porter S, Monuteaux MC, Stack AM. Unscheduled return visits to the emergency department: the impact of language. Pediatric emergency care. 2013 May;29(5):579–583. doi: 10.1097/PEC.0b013e31828e62f4. [DOI] [PubMed] [Google Scholar]


