Abstract
Background
Marijuana is the most commonly used illicit substance in pregnancy. Little is known about how pregnant women who use marijuana obtain and understand information about perinatal marijuana use. We conducted a qualitative study among pregnant women who had used marijuana to understand their information-seeking patterns and perceptions of usefulness of available information about perinatal marijuana use.
Study Design
We conducted semi-structured interviews with 26 pregnant women who were receiving prenatal care and who either disclosed marijuana use or had urine samples testing positive for marijuana. Interviews assessed women’s sources of information about risks of perinatal marijuana use and perceptions regarding the usefulness of such information. Interview data were coded independently by two coders who iteratively refined the codes and reviewed transcripts for themes.
Results
Commonly reported sources of information about perinatal marijuana use included Internet searching and anecdotal experiences or advice from family or friends. Few women reported receiving helpful information from a health care provider or social worker. Women perceived a lack of evidence about harms of perinatal marijuana use, and reported being dissatisfied with the quality of information. Most women said they desired information about the effects of perinatal marijuana use on infant health.
Conclusions
Women who used marijuana before or during pregnancy did not find available information about perinatal marijuana use to be useful, and sought more information pertaining to infant health and well-being. Efforts to reduce perinatal marijuana use should focus on addressing this need in both clinical and public health settings.
INTRODUCTION
Marijuana is a commonly used recreational drug during pregnancy in the United States (Kuczkowski, 2007; Substance Abuse and Mental Health Services Administration, 2008; Westfall, Janssen, Lucas, & Capler, 2006). Seven percent of pregnant women self-report using marijuana during the prior 2–12 months (Ko, Farr, Tong, Creanga, & Callaghan, 2015), although studies measuring marijuana use by self-report or urine screens have identified prevalence ranging from 8% to 29% (J. Chang et al., 2015; Conner, Carter, Tuuli, Macones, & Cahill, 2015; Desai, 2014).
Assessing the causal effects of perinatal marijuana use on health outcomes is difficult because of the need to interpret evidence from observational studies where unmeasured confounders may influence observed relationships (Volkow, Baler, Compton, & Weiss, 2014). Prior observational studies among pregnant women have provided mixed evidence with respect to whether perinatal marijuana use is associated with adverse obstetric or neonatal outcomes (El-Mohandes et al., 2003; Varner et al., 2014; Warshak et al., 2015). There may be a dose-response relationship, with heavy prenatal marijuana consumption associated with reduced birth weight; and poly-substance use (e.g., concurrent use of marijuana with alcohol or tobacco) may contribute to reduced birth weight and gestational age (Bada et al., 2005; Janisse, Bailey, Ager, & Sokol, 2014). The American Academy of Pediatrics has concluded that perinatal marijuana exposure has negative effects on short-term infant neurobehavior and longer-term behavior and cognition in childhood (Behnke, Smith, Committee on Substance Abuse, & Committee on Fetus and Newborn, 2013).
The U.S. policy environment with respect to marijuana use has changed dramatically in recent years. Public opinion data indicate that the public’s support for legalizing marijuana (estimated at 53% support in 2015) has increased since the 1990s, with a dramatic increase in public support since 2010 (Pew Research Center, 2015). Generally, the perception of risk of marijuana use has declined among the public, particularly among youth (Schuermeyer et al., 2014). Concurrently, state policies regarding marijuana’s legal status have changed dramatically in recent years. As of early 2016, 24 states permitted marijuana for medical use, and of those, five also permitted marijuana for recreational use (including the District of Columbia). The changing marijuana policies will inherently affect pregnant women, fetuses, and infants, especially since an estimated 51% of all pregnancies in the U.S. are unintended (Finer & Zolna, 2014).
However, it is unknown how pregnant women who have used marijuana obtain and understand information about the potential risks of perinatal marijuana use. Understanding how pregnant women obtain and understand this information is important because such information can have a profound influence on individuals’ knowledge and attitudes, and can form the basis for behavioral change (Finnegan & Viswanth, 2002; Prochaska & Velicer, 1997). The purpose of our study was to understand information-seeking patterns and perceptions of usefulness of available information about perinatal marijuana use among pregnant women who have used marijuana. Our findings are intended to engender a deeper understanding of pregnant women’s experiences with information about perinatal marijuana use that can inform both clinical and public health efforts to reduce perinatal marijuana use.
METHODS
Study participants and settings
The present study was nested in a large observational study investigating patient-provider communication about substance use in obstetric visits(J. C. Chang et al., 2015). The broad study goals were to assess perinatal illicit substance use screening and disclosure by urine screening and direct observation of obstetric visits, with follow-up qualitative interviews of participating patients to assess their views about health communication pertaining to substance use. The study took place in five clinical settings in the Pittsburgh, PA area, including one large hospital outpatient clinic and community clinics providing prenatal, gynecologic, and family planning services. The parent study recruited obstetric health care providers and pregnant patients presenting for their first obstetric visit at one of study sites. Obstetric care providers were recruited and consented prior to start of study activity in their scheduled clinic sessions. Patients were informed of the study when they registered for their first obstetric visit and those who expressed interest were then approached by study staff, who reviewed the study and obtained written consent for participation in a patient-provider communication study. All patients had their first obstetric visits audio-recorded.
Following the first obstetric visit, patients were asked to complete an interviewer-administered questionnaire. At this time, patient participants were debriefed on the study focus regarding substance use communication and invited to participate in a second phase of the study that involved providing a urine sample for testing for illicit substance use. Participants who agreed signed a second separate consent form. Patient participants who either reported or tested positive for any substance use—tobacco, alcohol, illicit drugs—were invited to return for semi-structured interviews within four weeks to review their audio-recorded obstetric visit and provide their thoughts regarding the substance use communication.
During the course of the parent study, we noted a higher than expected prevalence of perinatal marijuana use and our preliminary semi-structured interviews suggested that women viewed perinatal marijuana use differently than tobacco, alcohol, or other illicit drug use. We thus initiated a study arm to better understand perinatal marijuana use by asking patient participants who reported or tested positive for marijuana use to participate in two additional study visits during the second and third trimesters which included semi-structured interviews. These patients were asked to describe their thoughts, beliefs, and decision-making regarding using marijuana during pregnancy. Among the interview questions, we asked the women to describe where they sought and obtained information about marijuana use during pregnancy and their thoughts regarding this information and information seeking process.
In compensation for their time and participation, patient participants received $20 for the first phase of the study (the audio-recording, post-visit questionnaire and agreement to allow medical record abstraction), $10 for the second phase (urine testing), and $30 for each semi-structured interview. This study was approved by the University of Pittsburgh Institutional Review Board (IRB # PR008090530). A Certificate of Confidentiality from the National Institutes of Health (NIH) was also obtained for this study, which is designed to provide additional privacy protection for individuals who participate in sensitive health-related research.
Semi-structured interviews
All interviews were conducted in person. In the interviews, broad and open-ended questions were asked to assess specific steps women took to obtain information about marijuana during pregnancy and perceptions of usefulness of information they received about perinatal marijuana use (Table 1). All interviews were audio-recorded and transcribed verbatim. Interviews took place over approximately two years, between December 2012 and February 2015. Interview duration ranged from 18 to 43 minutes, with a mean interview duration of 29 minutes.
Table 1.
Questions to guide semi-structured interviews by domain
| Domain | Question |
|---|---|
| Information seeking | Where do women get information about marijuana use during pregnancy? |
| Information quality | How do you figure out whether this information is good or not? |
| Health care provider communication |
Have you talked to anyone else about your marijuana use, such as a nurse, social work or anyone else here at [health care facility]? [If yes] How did you feel about that communication? |
| Obstetric care provider communication |
Have any obstetric provider(s) asked or talked about marijuana use with you since that first visit? [If yes] How did you feel about that communication? |
Interview transcripts were analyzed using directed content analysis methods to identify and code themes about women’s information seeking pertaining to perinatal marijuana use. This approach allowed us to create categories of content related to our a priori outcomes of interest, as well as to address related categories of content that occur in the data (Hsieh & Shannon, 2005). Although our data coding was based on a priori outcomes of interest, the interviews were open-ended and allowed for substantial variation in women’s responses. Two authors separately coded the first two interviews, met to compare codes, discuss inconsistency in coding approaches, and alter or add codes for content not related to predetermined outcomes. This iterative content analysis was repeated, with coders meeting periodically to arbitrate any differences in coding and to refine and expand codes in response to new themes that emerged. After finalizing the coding scheme and a coding rulebook that provided definitions, rules, and examples for each code, the final coding scheme was used to code all interview transcripts using Atlas TI software. We identified major themes and present illustrative quotes for each theme that we describe.
RESULTS
Description of study participants and major themes
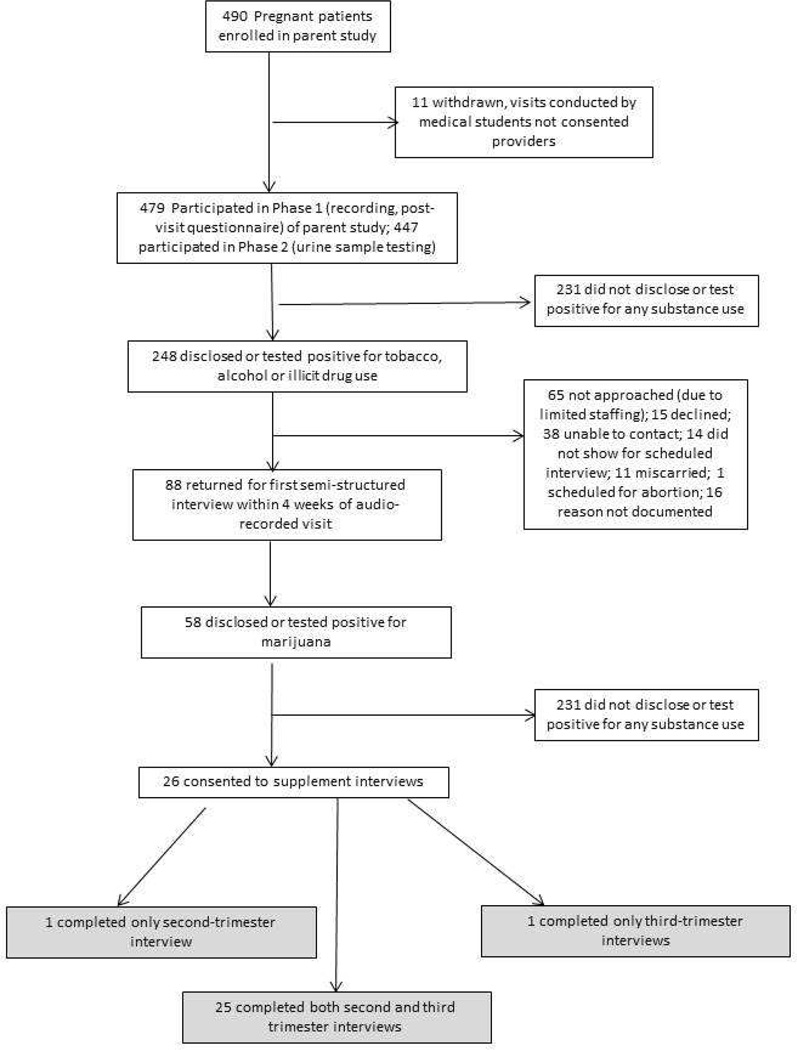
We describe the study flow diagram regarding the patient study participants in this portion of the study in Figure 1. Twenty-six women participated in supplement interviews focusing on perinatal marijuana use. Table 2 shows characteristics of the 26 women who participated in this study. Most women (22) were age 30 or younger. Eighteen women were African-American, four were white, three reported another race/ethnicity, and one was Hispanic/Latina. Approximately half of women were single, 12 were currently living with a partner, and one was married. Eight women were nulliparous, 10 had one previous birth, and eight had more than one previous birth. The majority of women had high school education or greater (11 had a high school education, while 11 had some education beyond high school). Participants tended to have low individual incomes; the majority reported a personal annual income (not including a partner’s income or other household members’ incomes) of less than $10,000.
Figure 1.
Study Flow Diagram
Table 2.
Demographic characteristics of study participants
| Characteristic | No. (n=26) |
|---|---|
| Age | |
| 19–24 | 11 |
| 25–30 | 11 |
| 31–36 | 4 |
| Race/Ethnicity | |
| Black | 18 |
| White | 4 |
| Hispanic/Latina | 1 |
| Other/Multiple Races | 3 |
| Partner status | |
| Single | 12 |
| Living with partner | 12 |
| Married | 1 |
| Separated | 1 |
| Parity | |
| 0 | 8 |
| 1 | 10 |
| ≥1 | 8 |
| Education | |
| <High school | 4 |
| High school/GED | 11 |
| >High school | 11 |
| Annual Income | |
| <$10,000 | 18 |
| $10,000–$19,999 | 5 |
| ≥$20,000 | 3 |
Note: Study participants included 26 pregnant patients who disclosed or tested positive for marijuana use at the time of their first obstetric visit.
We identified four major themes that emerged during the qualitative interviews. First, the most commonly reported sources of information about perinatal marijuana use included Internet searching and anecdotal experiences observed among family or friends. Second, even though all women in the study were engaged in prenatal care, few reported receiving helpful information from a health care provider or social worker. Third, women perceived that the quality of the information they did obtain was mixed and they were not sure whether research had shown any ill effects of perinatal marijuana use. Fourth, women shared that the primary type of information they wanted regarding perinatal marijuana use was the potential health and developmental effects on infants and children.
Sources of information about perinatal marijuana use
Women most commonly reported conducting Internet searches for information about perinatal marijuana use. When asked where they received information about perinatal marijuana use, several women said simply, “I Googled it.” One woman said, “I’ve been looking online, you know, things like that. I go to babycenter.com and pregnancy.com, and I’ve been watching videos on how smoke affects the baby.”
One woman described where she read information about perinatal marijuana use: “Um, just online. Just like Facebook, you know, the Internet has everything. … And it is like you click on something and it leads to something else. And it leads to something else and it is just like: You find out way more than what you thought you was going to find out.
In many cases, women juxtaposed information they read online with their own personal experiences or those of their family or friends. For example, one woman related that online information suggested that perinatal marijuana use was harmful, but stated that other women she knew had not experienced negative effects after using marijuana in pregnancy:
“I know people who were pregnant; some smoked [marijuana]; some didn’t. I mean their kids are fine. … I heard it helps with nausea, I heard it just helps calm them down and that was just something they did before [becoming pregnant] so they just kept going. And like I said, they didn’t say it really affected the baby in any way, but like everybody’s bodies are different, so what may not have affected that person may affect someone else. So I just don’t want to take that risk whether or not it can affect my child, I just would rather not take the risk.”
Another source of information women described using was the anecdotal experiences of friends, family members, or acquaintances. They described listening to and observing other women’s experiences using marijuana during pregnancy. One woman described observing her cousin’s nearconstant marijuana use in pregnancy, noting that: “This is her fifth baby, she smoked through all of her pregnancies. So it ain’t going to hurt her.”
Women also described learning from their own past experiences. In the following quotation, this woman reflected on her use of marijuana in a previous pregnancy:
“I had just stopped [using marijuana] and then after that, my son was born and he had, like, some medical issues. I still didn’t think it was like marijuana related. But in the back of my mind, I knew that I smoked. So for me, it was like maybe this, maybe the reason why. But nobody ever came out right and said it like: ‘Oh well, you know, marijuana is the reason why.’ …So it wasn’t like, upfront in my mind like, ‘Ok, well I did this to my child.’”
Conversations about sources of information revealed that women did not feel that the information they received about marijuana was consistent. While women generally felt that marijuana was “natural”, they also felt that perinatal use was probably harmful, and they juxtaposed information from Internet searches with personal experiences and observations.
Lack of information from health care providers and social workers
Most women reported that, despite being engaged in prenatal care, they did not receive any helpful information about perinatal marijuana use from health care providers or social workers. Some women said that the lack of information did not bother them because they had easily stopped using marijuana when they became pregnant. Others assumed that when the obstetric providers or social workers did not address the marijuana or did not provide counseling, this indicated that marijuana did not represent a significant concern for the outcome of their pregnancy. One woman described her interpretation of her obstetric providers’ lack of response as: “The only thing they’re telling me about marijuana is: ‘Just don’t do it.’ They’re not telling me: ‘Don’t do it because this could happen, that could happen, your baby could have this.’ … Right now, I don’t feel like that they are really concerned.”
Another woman said that she felt the lack of information from her doctor implied that perinatal marijuana use was not a serious risk: “Like I said, my doctor, when I brought [perinatal marijuana use] up to her, she was just like ‘Oh, like don’t worry about it.’ Basically, like ‘Oh, OK.’”
Other reactions were stronger, with women stating that they sought information about the risks of prenatal marijuana use or how to stop marijuana use and did not receive adequate resources in the health care setting. One woman relayed, “I feel like [the social worker] should have told me something. You’re a social worker. …you’re supposed to have all the advice in the world, and she didn’t tell me anything.”
One common experience was that social workers focused on child welfare agencies’ potential involvement after delivery, rather than providing resources to help women stop using marijuana during pregnancy. One woman described her experience with a social worker as such:
“[The social worker] came in there and she was like well, you know if there’s still marijuana in your system when you are 36 weeks [the child welfare agency] will be involved. Did you need any help with anything else?”
Other women reported receiving only punitive communication rather than information about prenatal marijuana use from their health care providers, stating that health care providers “talked down” to them and made them “feel targeted.” One woman described a lack of information about how to stop using marijuana in pregnancy, recounting that she received no information about “a phone number you can call, no person you can call and talk to. Nothing, it’s either quit or we’re going to call [child welfare agency].”
Another woman described the type of resources that she might have found helpful pertaining to marijuana use in pregnancy:
“‘If you need help you need to talk, here’s a number, we can help you.’ Give [women] every option possible to quit. And every like helping mechanism that will help them quit, something to help cope so they won’t want to [use marijuana]. And provide them with information about what it does to their child.”
Women often expressed resilience in the face of possible punitive measures, and stated that despite the lack of resources, they had or would be able to stop using marijuana to avoid involvement of the child welfare agencies after delivery.
Quality of information about perinatal marijuana use
Women who sought information about prenatal marijuana use reported that although they had the overall impression that marijuana use posed risks in pregnancy, they perceived a lack of evidence about specific harms to the fetus. Typical comments included statements that exact effects of prenatal marijuana use are unknown. For example, one woman described a lack of information about perinatal marijuana use, compared to information about other substances in pregnancy:
“I could not tell you one thing that happens to you when you smoke marijuana while your pregnancy…. I mean, I know what cigarettes and alcohol does. …And I’m not even a drinker so I don’t even need to know that. But it would be nice to know that there is an effect [from using marijuana during pregnancy] and what might happen.”
Additionally, women reported that internet searching left her with the impression that there is a debate about whether or not perinatal marijuana use was truly harmful. Women similarly reported receiving conflicting anecdotal evidence from friends and family members. As one woman put it: “There’s a lot of people that tell me I should quit; there’s a lot of people say I shouldn’t. Some people are telling me, like, ‘Oh, you’re probably killing your baby right now;’ some people are telling me, ‘Oh, that’s not affecting the baby at all.’” Since marijuana use was a consistent part of their life prior to pregnancy, women tended to seek less information earlier in pregnancy. As their pregnancies progressed, however, they felt that quality of information became more important. However, they tended to encounter conflicting messages about perinatal marijuana use.
Information about marijuana’s effects on infant health
When asked about the type of information that would have been helpful, women identified both improved communication from health care providers, as well as resources specific to the effects on the fetus. However, women also said that simply being handed a pamphlet at the first prenatal visit would probably not be helpful. One woman identified how a clinician might communicate about prenatal marijuana use:
“[If she] had a conversation with their doctor, and a doctor says, ‘Well these are the effects it would have on your baby, your baby could possibly come out with asthma, you know problems with breathings things like that if.’ If that’s addressed more from the beginning I think it would have more of an effect on me.”
By far, the most important factor to women was their infant’s health. Women reported that websites where they could follow fetal development were particularly powerful for them. As such, presenting communications about prenatal marijuana use that included pictures of developing fetuses seemed to be a particularly salient idea for improving information quality.
It is notable that women’s decisions about perinatal marijuana use tended to focus almost exclusively on the well-being of their baby, rather than being a longer-term decision relating to their own health. When asked what type of information would be useful to her, one woman expressed: “How does it [perinatal marijuana use] affect the baby. That is basically all I want to know, really.” For this reason, information that addressed fetal and infant health outcomes was deemed to be especially important. In contrast, women noted that information about the effect of cigarette smoking on fetal development and infant health was clear, and asked why similar information on perinatal marijuana use did not seem to be available.
DISCUSSION
During semi-structured interviews with 26 pregnant women who had used marijuana before or in pregnancy, women commonly reported that they sought information about the risks of perinatal marijuana use, they identified a lack of information from health care providers or social workers, and they desired more specific information regarding risks of fetal harm from exposure to marijuana. This study is the first, to our knowledge, to examine information-seeking patterns as well as perceptions of usefulness of available information about perinatal marijuana use. Findings suggest that pregnant patients do not find currently available information sources to be useful, highlight the power of anecdotal as well as scientific evidence, and suggest that salient messages about perinatal marijuana use will pertain to fetal and infant health and well-being.
That women reported currently available information about perinatal marijuana use was not perceived as actionable, even among women engaged in prenatal care, is striking. Patients’ perceptions were consistent with current scientific uncertainty about the nature of a causal relationship between marijuana consumption and perinatal health outcomes (Volkow et al., 2014). While additional rigorous study of perinatal marijuana use is needed to better understand health effects, better public health and clinical communication is needed to disseminate to pregnant women what is currently known about marijuana use in pregnancy (Jaques et al., 2014). Evidencebased information from public health agencies or health care providers may be particularly important, given that the public is already being exposed to marketing communications intended to promote marijuana use (MacCoun & Mello, 2015).
Women in our study overwhelmingly reported receiving information about punitive legal consequences of perinatal marijuana use; that is, that child welfare agencies would intervene and possibly take custody of their infant if women tested positive for substance use at delivery. Given that the majority of women in this study identified as black, this finding is consistent with prior literature documenting that infants of substance-using black women are far more likely to be reported to child protection agencies relative to infants of substance-using white women (Ellsworth, Stevens, & D'Angio, 2010; Osterling, D'Andrade, & Austin, 2008; Roberts & Nuru-Jeter, 2012). This is troubling given that a threat of involvement of child protection services may lead women to disengage with the health care system (Roberts & Pies, 2011), which is contrary to the intended effects of social welfare programs to intervene and provide services (Mikton & Butchart, 2009). Several women indicated that knowledge of specific health effects would have a powerful impact on their decision to stop marijuana use in pregnancy. In contrast, information about legal consequences seemed to motivate women to have a “clean” urine test at delivery rather than consider health consequences of perinatal marijuana use for themselves or their infants.
Findings fit into the broader communication literature about how pregnant women seek or obtain health information related to risks of substances. In the case of tobacco, decades of research about the risks of use in pregnancy has resulted in clear clinical guidelines about advising pregnant patients to quit (Cnattingius, 2004), and public health communication campaigns have been mounted to communicate risks of prenatal tobacco use to the public to discourage prenatal smoking (Hawkins, Baum, Oken, & Gillman, 2014; Thomson, Wilson, & Howden-Chapman, 2006). Likewise, universal prevention efforts, including public health campaigns and product labeling, have been undertaken to reduce fetal alcohol spectrum disorders caused by prenatal alcohol use (Hankin, 2002). Illicit substances, in contrast, have not had the same volume of observational research and subsequent dissemination of clinical and public health guidelines. Health care providers’ responses to pregnant patients’ disclosure of use of illicit substances typically includes general statements of risk rather than a discussion or referral to treatment (Chang et al., 2008). Results from the present study are consistent with the notion that pregnant women who use marijuana are left to sort through conflicting evidence about the health effects on their own.
Limitations
Findings should be interpreted in light of limitations. First, our qualitative study design used a sample population in a limited geographic area which does not allow us to present comprehensive or generalizable data on women who use marijuana in pregnancy. Our qualitative data do, however, allow for an in-depth view of distinct patient experiences pertaining to understanding of information about perinatal marijuana use. Second, our data lack longer-term follow-up on women’s marijuana use in the postpartum period; thus, we are not able to assess whether information they received during prenatal care may have influenced their longer-term health behavior. Third, marijuana use in pregnancy was a requirement for inclusion in this study, so findings may not be generalizable to women of childbearing age who use marijuana and but stop marijuana use prior to becoming pregnant. Finally, our interviews were conducted over a time period when several U.S. states liberalized their marijuana laws and some state public health agencies (including in Colorado and Alaska) published websites describing potential risks of perinatal marijuana use. Therefore, women interviewed later in our study timeline may have had more access to information about perinatal marijuana use relative to women interviewed at earlier dates.
Implications for policy and practice
The current debate about the true causal effects of marijuana on health poses a challenging environment for public health officials or clinicians to effectively communicate the risks of perinatal marijuana use. The creation of state-based medical or recreational markets for marijuana means it is likely that women of childbearing age and pregnant women will be exposed to new marijuana marketing messages (Barry, Hiilamo, & Glantz, 2014). A large literature has documented the impact of media content and presentation (including marketing, the news media, and public health communication) on the public’s knowledge and attitudes (Farrelly et al., 2002; Finnegan & Viswanth, 2002; Popova & Ling, 2014). It is plausible that marijuana legalization policies, in the absence of better health communication about the risk of perinatal use, will lead to increased marijuana use in the perinatal period.
Our qualitative data suggest that pregnant women are receptive to messages about marijuana’s health effects, highlighting the need for evidence-based health communication about perinatal marijuana use. Psychosocial interventions, including communication interventions, are effective in reducing cigarette smoking in pregnancy (Chamberlain et al., 2013). Interventions tailored to both health care providers, as well as public health communications, may be warranted. Since our data were collected, the Colorado public health department and the American College of Obstetricians and Gynecologists have disseminated information to health care providers recommending screening for and counseling pertaining to marijuana use in pregnancy (American College of Obstetricians and Gynecologists Committee on Obstetrc Practice, 2015; Colorado Department of Public Health and Environment, 2016).
Conclusions
Among our sample of pregnant women who used marijuana before or during pregnancy, most reported a lack of useful communication about the health effects of perinatal marijuana use. Our findings suggest that health communication should address changing marijuana policies and changing social norms regarding marijuana use. Additionally, findings suggest that the most salient messages will pertain to infant health and well-being.
Acknowledgments
Judy C. Chang, MD, MPH, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis
Funding Statement:
This research was supported by a grant from the National Institute on Drug Abuse of the National Institutes of Health (NIH) (R01 DA026410 AND R01 DA026410-S, Chang), the National Center for Research Resources, a component of the NIH and NIH Roadmap for Medical Research (5UL1 RR024153-05), the Health Research Formula Fund from the Pennsylvania Department of Health (TRK_02-Chang-Magee_2014F), and the Magee-Womens Hospital of UPMC Volunteer Service Board Grant Award. The funding sources had no involvement in study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Biographies
Marian Jarlenski, PhD, MPH, is an Assistant Professor in the Department of Health Policy and Management at the University of Pittsburgh Graduate School of Public Health. Her research aims to improve women's health and healthcare, particularly in underserved populations.
Jill A. Tarr, MSW, is a Senior Clinical Research Associate at the Magee-Womens Research Institute. She has expertise in clinical research with patients, including interview studies and analyzing qualitative data.
Cynthia Holland, MPH, is a Project Manager at the Magee-Womens Research Institute. She has participated in research focusing on pregnant patients’ perspectives and has expertise working with qualitative data.
David Farrell, MPH, is the Founder of People Designs. His work has focused health education and health promotion, and health communications.
Judy C. Chang, MD, MPH, is an Associate Professor of Obstetrics, Gynecology and Reproductive Sciences at the Magee-Womens Research Institute and the University of Pittsburgh School of Medicine. Her work aims to improve women’s health via the study of behavioral and interpersonal components of women’s health, safety, and health services.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Marian Jarlenski, Email: marian.jarlenski@pitt.edu.
Jill A. Tarr, Email: tarrja@upmc.edu.
Cynthia L. Holland, Email: hollandcl2@upmc.edu.
David Farrell, Email: dfarrell@peopledesigns.com.
Judy C. Chang, Email: chanjc@mail.magee.edu.
REFERENCES
- American College of Obstetricians and Gynecologists Committee on Obstetrc Practice. Committee Opinion No. 637: Marijuana Use During Pregnancy and Lactation. Obstet Gynecol. 2015;126(1):234–238. doi: 10.1097/01.AOG.0000467192.89321.a6. [DOI] [PubMed] [Google Scholar]
- Bada HS, Das A, Bauer CR, Shankaran S, Lester BM, Gard CC, Higgins R. Low birth weight and preterm births: etiologic fraction attributable to prenatal drug exposure. J Perinatol. 2005;25(10):631–637. doi: 10.1038/sj.jp.7211378. [DOI] [PubMed] [Google Scholar]
- Barry RA, Hiilamo H, Glantz SA. Waiting for the opportune moment: the tobacco industry and marijuana legalization. Milbank Q. 2014;92(2):207–242. doi: 10.1111/1468-0009.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnke M, Smith VC Committee on Substance Abuse, & Committee on Fetus and Newborn. Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics. 2013;131(3):e1009–e1024. doi: 10.1542/peds.2012-3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain C, O'Mara-Eves A, Oliver S, Caird JR, Perlen SM, Eades SJ, Thomas J. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev. 2013;10:CD001055. doi: 10.1002/14651858.CD001055.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J, Holland C, Tarr J, Rodriguez K, Kraemer K, Rubio D, Arnold R. Direct observation of screening for and disclosure of illicit drug use in pregnancy visits. American Journal of Health Promotion. 2015 In Press. [Google Scholar]
- Chang JC, Dado D, Frankel RM, Rodriguez KL, Zickmund S, Ling BS, Arnold RM. When pregnant patients disclose substance use: missed opportunities for behavioral change counseling. Patient Educ Couns. 2008;72(3):394–401. doi: 10.1016/j.pec.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang JC, Holland CL, Tarr JA, Rubio D, Rodriguez KL, Kraemer KL, Arnold RM. Perinatal Illicit Drug and Marijuana Use: An Observational Study Examining Prevalence, Screening, and Disclosure. Am J Health Promot. 2015 doi: 10.4278/ajhp.141215-QUAL-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;6(Suppl 2):S125–S140. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- Colorado Department of Public Health and Environment. Marijuana: Health care provider resources. 2016 Retrieved from https://www.colorado.gov/cdphe/marijuana-clinical-guidelines.
- Conner SN, Carter EB, Tuuli MG, Macones GA, Cahill AG. Maternal marijuana use and neonatal morbidity. Am J Obstet Gynecol. 2015 doi: 10.1016/j.ajog.2015.05.050. [DOI] [PubMed] [Google Scholar]
- Desai A, Mark K, Terplan M. Marijuana use and pregnancy: Prevalence, associated behaviors, and birth outcomes. Obstet Gynecol. 2014;123:46S. [Google Scholar]
- El-Mohandes A, Herman AA, Nabil El-Khorazaty M, Katta PS, White D, Grylack L. Prenatal care reduces the impact of illicit drug use on perinatal outcomes. J Perinatol. 2003;23(5):354–360. doi: 10.1038/sj.jp.7210933. [DOI] [PubMed] [Google Scholar]
- Ellsworth MA, Stevens TP, D'Angio CT. Infant race affects application of clinical guidelines when screening for drugs of abuse in newborns. Pediatrics. 2010;125(6):e1379–e1385. doi: 10.1542/peds.2008-3525. [DOI] [PubMed] [Google Scholar]
- Farrelly MC, Healton CG, Davis KC, Messeri P, Hersey JC, Haviland ML. Getting to the truth: evaluating national tobacco countermarketing campaigns. Am J Public Health. 2002;92(6):901–907. doi: 10.2105/ajph.92.6.901. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12036775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health. 2014;104(Suppl 1):S43–S48. doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finnegan J, Viswanth K. Communication theory and health behavior change: the media studies framework. In: R. B. Glanz K, Lewis FM, editors. Health Behavior and Health Education: Theory, Research and Practice. San Francisco: Jossey-Bass; 2002. [Google Scholar]
- Hankin JR. Fetal alcohol syndrome prevention research. Alcohol Res Health. 2002;26(1):58–65. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12154653. [PMC free article] [PubMed] [Google Scholar]
- Hawkins SS, Baum CF, Oken E, Gillman MW. Associations of tobacco control policies with birth outcomes. JAMA Pediatr. 2014;168(11):e142365. doi: 10.1001/jamapediatrics.2014.2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Janisse JJ, Bailey BA, Ager J, Sokol RJ. Alcohol, tobacco, cocaine, and marijuana use: relative contributions to preterm delivery and fetal growth restriction. Subst Abus. 2014;35(1):60–67. doi: 10.1080/08897077.2013.804483. [DOI] [PubMed] [Google Scholar]
- Jaques SC, Kingsbury A, Henshcke P, Chomchai C, Clews S, Falconer J, Oei JL. Cannabis, the pregnant woman and her child: weeding out the myths. J Perinatol. 2014;34(6):417–424. doi: 10.1038/jp.2013.180. [DOI] [PubMed] [Google Scholar]
- Ko JY, Farr SL, Tong VT, Creanga AA, Callaghan WM. Prevalence and Patterns of Marijuana Use among Pregnant and Non-Pregnant Women of Reproductive Age. Am J Obstet Gynecol. 2015 doi: 10.1016/j.ajog.2015.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczkowski K. The effects of drug abuse on pregnancy. Curr Opin Obstet Gynecol. 2007;19:578–585. doi: 10.1097/GCO.0b013e3282f1bf17. [DOI] [PubMed] [Google Scholar]
- MacCoun RJ, Mello MM. Half-Baked - The Retail Promotion of Marijuana Edibles. N Engl J Med. 2015;372(11):989–991. doi: 10.1056/NEJMp1416014. [DOI] [PubMed] [Google Scholar]
- Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ. 2009;87(5):353–361. doi: 10.2471/BLT.08.057075. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19551253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterling KL, D'Andrade A, Austin MJ. Understanding and addressing racial/ethnic disproportionality in the front end of the child welfare system. J Evid Based Soc Work. 2008;5(1–2):9–30. doi: 10.1300/J394v05n01_02. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. In debate over legalizing marijuana, disagreement over drug's dangers. 2015 Retrieved from http://www.peoplepress.org/files/2015/04/04-14-15-Marijuana-release.pdf. [Google Scholar]
- Popova L, Ling PM. Nonsmokers' responses to new warning labels on smokeless tobacco and electronic cigarettes: an experimental study. BMC Public Health. 2014;14:997. doi: 10.1186/1471-2458-14-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10170434. [DOI] [PubMed] [Google Scholar]
- Roberts SC, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39(1):3–16. doi: 10.1007/s11414-011-9247-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts SC, Pies C. Complex calculations: how drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health J. 2011;15(3):333–341. doi: 10.1007/s10995-010-0594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, Min SJ, Sakai JT. Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–11. Drug Alcohol Depend. 2014;140:145–155. doi: 10.1016/j.drugalcdep.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings (NSDUH Series H-34, DHHS Publication No. SMA-08-4343. Rockville, MD: 2008. Retrieved from. [Google Scholar]
- Thomson G, Wilson N, Howden-Chapman P. Population level policy options for increasing the prevalence of smokefree homes. J Epidemiol Community Health. 2006;60(4):298–304. doi: 10.1136/jech.2005.038091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varner MW, Silver RM, Rowland Hogue CJ, Willinger M, Parker CB, Thorsten VR Human Development Stillbirth Collaborative Research, N. Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol. 2014;123(1):113–125. doi: 10.1097/AOG.0000000000000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshak CR, Regan J, Moore B, Magner K, Kritzer S, Van Hook J. Association between marijuana use and adverse obstetrical and neonatal outcomes. J Perinatol. 2015;35(12):991–995. doi: 10.1038/jp.2015.120. [DOI] [PubMed] [Google Scholar]
- Westfall R, Janssen P, Lucas P, Capler R. Survey of medicinal cannabis use among childbearing women: patterns of its use in pregnancy and retroactive self-assessment of its efficacy against 'morning sickness'. Complement Ther Clin Pract. 2006;12(1):27–33. doi: 10.1016/j.ctcp.2005.09.006. [DOI] [PubMed] [Google Scholar]