Abstract
Purpose
This study investigates depression and anxiety in gender minority (i.e., transgender and/or gender nonconforming) compared to non-gender minority (cisgender) young adults.
Methods
Data were from the Growing Up Today Study, a national cohort of U.S. young adults. A two-step method (maternal-reported natal sex in 1996 cross-classified with participant-reported current gender identity in 2010) was used to identify gender minority and non-gender minority respondents (n=7831; mean age=26 years). Differences in past-week depressive symptoms and anxious symptoms were examined cross-sectionally by gender identity. Gender minority and non-gender minority respondents were compared using age-adjusted logistic regression models.
Results
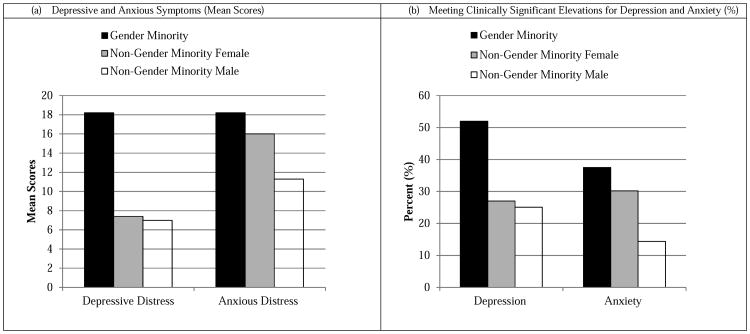
In gender minorities, the prevalence of depressive and anxious symptoms meeting clinical cutoffs was 52% and 38%, respectively compared to non-gender minorities (27% and 30% in females and 25% and 14% in males) (p<0.01).
Conclusion
Gender identity is an understudied social determinant of mental health. Surveillance efforts to monitor mental health disparities should include survey questions to assess gender identity in epidemiologic research. Research and interventions to understand and ameliorate mental health disparities by gender identity are needed.
Keywords: transgender, mental health, depression, anxiety, health disparities
Introduction
In the United States, depression and generalized anxiety represent serious public health problems (1-3). The estimated prevalence of depression is 29.9% (lifetime) and 8.6% (past 12 months) and generalized anxiety is 9.0% (lifetime) and 2.0% (past 12 months) evaluated via clinical diagnostic interview (2), with higher prevalence in studies utilizing screening scales, subthreshold clinical cut-points, or broadened/relaxed clinical diagnostic criteria requiring shorter duration of symptoms (4, 5). Young adulthood represents the most common developmental period of onset for depression and generalized anxiety in the U.S. with median age of onset between ages 23-30 (2).
Gender differences in depression and anxiety have been consistently found with females about twice as likely to have mood disorders compared to males (6-9). Despite the research attention and interest in gender differences, no national U.S. studies that we are aware of have moved beyond a binary conceptualization of gender to examine the epidemiology of depression and anxiety in gender minorities compared to non-gender minorities. Gender minority refers to transgender and/or gender nonconforming people whose sex assigned at birth is different from their current gender identity (10). Gender identity refers to a person's internal, felt sense of self as male, female, transgender, or another diverse nonbinary gender identity (11).
In the past decade there has been increasing research in gender minority health applying a depathologizing framework to understand the health of transgender and gender nonconforming people (10, 12). In the mental health realm, this framework has moved research away from conceptualizing gender minorities as “disordered” to recognizing the mental health concerns that gender minority people face, many of which may be the result of stress- and stigma-related processes due to social exclusion (13, 14). In community and clinic samples of gender minority youth (15-17) and adults (18-21), depression and anxiety are highly prevalent. However, few U.S. comparative epidemiologic data exist to examine whether gender minorities experience higher levels of depression and anxiety relative to non-gender minority populations (22). A barrier to monitoring the physical and mental health of U.S. transgender and gender nonconforming populations is the lack of inclusion of survey items on population-level and epidemiologic surveys with which to identify gender minority respondents (10, 23). Using data from a large national prospective cohort of young adults in the United States, the current study sought to fill this empirical gap. We examine the social epidemiology of depression and anxiety by gender identity, comparing gender minority and non-gender minority young adults.
Methods
Participants
The Growing Up Today Study 1 (GUTS1) is a national longitudinal cohort of children of participants of the Nurses' Health Study II (NHSII), a prospective cohort of female registered nurses across the United States. At enrollment in 1996, the GUTS sample consisted of more than 16,000 youth ages 9 to14 (7,843 boys and 9,039 girls) (24). GUTS1 participants have completed quantitative assessments assessing their health and health-related indicators approximately every two years since 1996. The institutional review board at Brigham and Women's Hospital approved the GUTS1 study. Activities for the current study were approved by the Brigham and Women's Hospital institutional review board. To be included in secondary analyses, GUTS1 participants had to complete the gender identity question asked in the 2010 survey wave (n=7,831). A complete case analysis (i.e., listwise deletion) has been found to yield non-biased estimates in the GUTS1 cohort (25). As with other GUTS1 analyses using data from the 2010 wave (26, 27), a higher proportion of 2010 wave respondents were female versus male (maternal reported natal sex at baseline in 1996) as compared to baseline enrollment (p<0.05).
Measures
Gender Minority
A two-step method was used to identify gender minority and cisgender respondents (step 1: assigned sex at birth; step 2: current gender identity) (28). Natal sex (male or female) at baseline in 1996 was reported by respondents' mothers when GUTS1 participants were first enrolled. A single-item gender identity measure (28) was asked in the 2010 GUTS1 questionnaire wave: “How do you describe yourself?” with the response options: “Female,” “Male,” “Transgender,” and “Do not identify as female, male, or transgender.” Gender identity was operationalized by cross-classifying sex and gender as follows: (1) “Male”, respondents who completed the boys survey at baseline in 1996 and checked “Male” on the gender identity 2010 item; (2) “Female”, respondents who completed the girls survey at baseline in 1996 and checked “Female”; and (3) “Gender minority” participants who selected who indicated a cross-sex identity (i.e., filled out the boys survey at baseline in 1996 and identified as “Female” on the gender identity item in 2010), “Transgender”, or “Do not identify as male, female, or transgender”.
Depression
Depressive distress was assessed using the validated and reliable 10-item Center for Epidemiologic Studies Depression (CES-D 10) Scale (29), a screener used widely with adolescent and young adult populations (26, 30, 31) GUTS1 participants were asked to indicate how often in the past week they felt or behaved certain ways on a response scale ranging from 0=rarely/never to 3=all the time (e.g., “During the past week, I was bothered by things that usually don't bother me”). After reverse coding two items, scores were summed. Items correlated from 0.10-0.51 (p<0.0001). Scores ranged from 0 to 30 and higher scores indicated more depressive distress (Cronbach's α=0.81). As in previous research (30), a clinical cut point of CESD-10 score ≥ 10 was used to categorize a positive screen for clinically significant depressive distress.
Anxiety
Anxious distress was assessed with 9 items from the Worry/Sensitivity Subscale of the Revised Children's Manifest Anxiety Scale (RCMAS) (the “What I Think and Feel” instrument) (32). The RCMAS (33-35) and the Worry/Sensitivity Subscale (36) are well-validated in youth. Of RCMAS' subscales, this subscale most closely represents the excessive worry characteristic of generalized anxiety disorder as outlined in the Diagnostic and Statistical Manual of Mental Disorders IV-Text Revision (DSM-IV-TR) (37). Participants were asked how often in the past week they felt symptoms of anxiety on a Likert-response scale ranging from 0=none of the time to 5=all of the time (e.g., “I worry about what is going to happen”, “I worry about what other people think about me”, “I am nervous”). Item scores were summed, with a higher scores indicating more anxious distress. Scores ranged from 0 to 45 (Cronbach's α=0.93). Items correlated from 0.49-0.76 (p<0.0001). Scores were categorized to create a binary indicator of a clinically significant elevation in anxious distress, using scores at or above the 75% percentile (score ≥ 18).
Demographic Characteristics
Age (in years) was reported in 2010. Race/ethnicity was reported in 1996 was categorized as a binary indicator of any racial/ethnic minority (yes/no).
Data Analysis
SAS v9.3 was used for all statistical analyses. The univariate distribution of all variables (frequency, proportion, mean, standard deviation) was examined by gender identity (gender minority versus non-gender minority females and males). Bivariate analyses first tested for an overall global effect of gender identity in mean depressive and anxious symptoms scores using analysis of variance (ANOVA) and proportional differences in meeting clinical cut-offs using chi-square (χ2) tests. Tests for normality were conducted to ensure statistical assumptions required for ANOVA were met. Pairwise comparisons were subsequently conducted to compare gender minorities each to non-gender minority female and males, respectively, using t-tests (equal variances) for mean scores and Fisher's exact tests for proportions. Cohen's d effect size estimates (38) were calculated for main differences to provide a sense of the magnitude of differences in symptom scores by gender identity. Age-adjusted linear regression models were fit to examine differences by gender identity in continuous symptom scores. Age-adjusted logistic regression models were fit to examine whether gender minority and non-gender minority female respondents each had increased odds of elevated depressive and anxious distress relative to non-gender minority male respondents. Non-gender minority males were selected as the referent group for regression models given psychiatric epidemiologic studies showing lowest prevalence of depression and anxiety in this population group (6-9). Models were age adjusted because of developmental differences in onset of depressive and anxious symptoms (2).
Results
Table 1 presents current gender identity (2010) by maternal-reported sex at baseline (1996). Overall 0.33% of the respondent cohort was gender minority. The mean age of the sample was 25.7 years (SD=1.7); no statistically significant age differences were found by gender identity (F=0.74 (df=2,7065), p=0.48). The majority (96.4%) were White (non-Hispanic), and the proportion of racial/ethnic minority respondents was comparable across gender identity groups (χ2=1.48, df=2, p=0.47).
Table 1.
Self-Reported Current Gender Identity (2010; mean age 26 years) By Maternal-Reported Natal Sex (1996).
| Maternal-Reported Natal Sex (1996) | |||
|---|---|---|---|
| Female (n=5226) % (n) | Male (n=2605) | Total Sample (n=7831) | |
|
|
|||
| Self-Reported Current Gender Identity (2010) | |||
| Non-Gender Minority Female a | 99.69 (5210) | 0.00 (0) | 66.53 (5210) |
| Non-Gender Minority Male | 0.00 (0) | 99.62 (2595) | 33.14 (2595) |
| Gender Minority b | 0.31 (16) | 0.38 (10) | 0.33 (26) |
| Cross-Sex Identified c | 0.06 (3) | 0.15 (4) | 0.09 (7) |
| Transgender Identified d | 0.06 (3) | 0.08 (2) | 0.06 (5) |
| Do Not Identify as Female, Male, or Transgender e | 0.19 (10) | 0.15 (4) | 0.18 (14) |
Non-Gender Minority = Concordant maternal-reported natal sex and current gender identity (i.e., female natal sex and female current gender identity, or male natal sex and male current gender identity).
Gender Minority = Combined respondents who endorsed a cross-sex identity, transgender identity, and who indicated they do not identify as female, male, or transgender.
Cross-Sex Identified = Discordant maternal-reported natal sex and current gender identity (i.e., female natal sex and male current gender identity, or male natal sex and female current gender identity).
Transgender = Participant selected “Transgender” as current gender identity.
Do Not Identify as Female, Male, or Transgender = Participant endorsed a different non-binary (not female or male) current gender identity.
Table 2 shows the distribution of depressive and anxious symptom scores and depression and anxiety meeting clinical cut-offs by gender identity. Gender minority respondents had elevated levels of depressive distress compared to non-gender minority respondents (M=10.7 gender minority, M=7.4 females, M=7.0 males; p<0.0001). Anxious symptoms were also higher comparing gender minority and non-gender minority respondents (M=16.7 gender minority, M=14.6 females, M=10.3 males; p<0.0001). In gender minorities, the prevalence of depressive and anxious symptoms meeting clinical cut-offs was 52% and 38%, respectively compared to non-gender minorities (27% and 30% in females and 25% and 14% in males) (p<0.01). Results are shown graphically in Figure 1.
Table 2.
Mental Health Indicators by Current Gender Identity (2010): Comparing Gender Minority a and Non-Gender Minority b Female and Male Respondents.
| Gender Minority n=26 | Non-Gender Minority | Non-Gender Minority | Global Bivariate Statistical Comparisons* | Total Sample n=7831 | ||||
|---|---|---|---|---|---|---|---|---|
| Female n=5210 | Male n=2595 | |||||||
| Past-Week Symptom Scores | Mean (SD) | Mean (SD) | p-value | Mean (SD) | p-value | F-Value(df) | p-value | Mean (SD) |
| Depressive Symptoms | 10.7 (5.3) | 7.4 (4.7) | 0.0005 | 7.0 (4.5) | <0.0001 | 240.59 (2,7775) | <0.0001 | 7.3 (4.7) |
| Anxious Symptoms | 16.7 (9.2) | 14.6 (8.4) | 0.22 | 10.3 (7.3) | <0.0001 | 243.74 (2,7672) | <0.0001 | 13.2 (8.3) |
| Past-Week Clinical Elevations | % | % | p-value | % | p-value | χ2 (df) | p-value | % |
| Clinically Significant Depressive Distress c | ||||||||
| Yes (CESD-10 score ≥ 10) | 52.0 | 27.0 | 0.005 | 25.1 | 0.002 | 11.48 (2) | 0.003 | 26.4 |
| No | 48.0 | 73.0 | 74.9 | 73.6 | ||||
| Clinically Significant Anxious Distress d | ||||||||
| Yes (RCMAS score ≥ 75 percentile) | 37.5 | 31.2 | 0.51 | 15.2 | 0.003 | 227.93 (2) | <0.0001 | 26.0 |
| No | 62.5 | 68.8 | 84.8 | 74.0 | ||||
Gender Minority = Combined respondents who endorsed a cross-sex identity, transgender identity, and who indicated they do not identify as female, male, or transgender.
Non-Gender Minority = Concordant maternal-reported natal sex and current gender identity (i.e., female natal sex and female current gender identity, or male natal sex and male current gender identity).
Clinically significant depressive distress: Center for Epidemiologic Studies Depression (CESD-10) score ≥ 10.
Clinically significant anxious distress: Revised Children's Manifest Anxiety Scale (RCMAS) Worry/Sensitivity Subscale score 75 percentile or above (score ≥ 18 within the GUTS sample, not a standardized population).
SD = Standard Deviation. Note: The total number of cases included in each bivariate global statistical comparison differed due to missing data. The number of cases included in each comparison is indicated in parentheses as degrees of freedom.
p-values are generated from bivariate analyses examining the overall global effect of gender identity (ANOVA and Fisher's exact tests). Pairwise comparisons were implemented using t-tests (equal variances) and Fisher's exact tests.
Figure 1.
Mental Health Disparities by Gender Identity: Comparing Gender Minority a and Non-Gender Minority Females and Males.
aGender Minority = Combined respondents who endorsed a cross-sex identity, transgender identity, and who indicated they do not identify as female, male, or transgender.
Age-adjusted linear and logistic regression models are presented in Table 3. Compared to non-gender minority males, gender minority young adults had significantly elevated depressive and anxious scores (p<0.01). Effect sizes for past-week mental health symptom scores were moderate to large. For past-week depressive distress, the Cohen's d for gender minority compared to females was 0.66, and relative to males was 0.75. Past-week anxious distress Cohen's d for gender minority versus females was 0.22, and compared to males was 0.74. Gender minorities were also found to have two- to- three-fold significantly increased odds of depression and anxiety (p<0.05) relative to non-gender minority males. Non-gender minority females evidenced higher depressive and anxious symptom scores (p<0.01) and increased odds of anxiety relative to non-gender minority males (p<0.0001).
Table 3.
Age-Adjusted Linear and Logistic Regression Models Examining Differences in Mental Health By Gender Identity.
| (a) Linear Regression Models | (b) Logistic Regression Models | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Depressive Symptoms | Anxious Symptoms | Depression | Anxiety | |||||
| Beta (95% CL) | p-value | Beta (95% CL) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
|
|
||||||||
| Age (Years) | −0.11 (−0.17, −0.04) | 0.001 | −0.10 (−0.21, 0.01) | 0.088 | 0.96 (0.93, 0.99) | 0.022 | 0.97 (0.94, 1.01) | 0.112 |
| Gender Identity | ||||||||
| Non-Gender Female | 0.33 (0.09, 0.56) | 0.006 | 4.21 (3.80, 4.62) | <0.0001 | 1.09 (0.97, 1.23) | 0.133 | 2.46 (2.16, 2.80) | <0.0001 |
| Non-Gender Minority Male | Ref | Ref | Ref | Ref | ||||
| Gender Minority a | 2.95 (1.01, 4.89) | 0.003 | 6.11 (2.61, 9.60) | 0.0006 | 2.50 (1.07, 5.82) | 0.034 | 3.36 (1.38, 8.19) | 0.008 |
Gender Minority = Combined respondents who endorsed a cross-sex identity, transgender identity, and who indicated they do not identify as female, male, or transgender. 95% CL = 95% Confidence Limit. OR = Odds Ratio. 95% CI = 95% Confidence Interval.
Discussion
In this large national prospective cohort study of U.S. young adults, disparities in past-week depression and anxiety were found by gender identity. Specifically, compared to non-gender minority males, gender minority respondents had higher symptom scores on each mental health outcome and were more likely to meet clinical thresholds for past-week depression and anxiety. These findings replicate previous studies showing high levels of psychological distress among transgender and gender nonconforming people (15-21). Our results extend previous research by documenting mental health disparities with comparative data of gender minority and non-gender minority young adults. Future studies that examine the etiology of the higher depressive and anxious symptoms burdening gender minority compared to non-gender minority young adults are recommended to inform interventions.
Study findings should be interpreted in light of several limitations. First, the GUTS1 cohort is a homogenous sample in terms of age, race/ethnicity, and maternal employment (young adults, largely white race/ethnicity, children of nurses). Whether these mental health disparities would be similar in effect size in cohort studies and surveillance systems that are comprised of more diverse populations requires additional study. Second, small sample size represents a limitation given 0.33% of the cohort identified as transgender. However, given statistical power is partly a function of the magnitude of differences (e.g., effect sizes), the large mean differences between gender minority and cisgender young adults enabled statistically powered analyses despite the small sample size. Due to a small number of transgender and gender nonconforming respondents, we were unable to test for mental health subgroup differences by gender identity or by natal sex (female-to-male versus male-to-female) or to disaggregate transgender, cross-sex, and gender variant respondents (binary versus nonbinary identification). Future research would benefit from considering subgroup differences. Although this study used clinically validated screening instruments for depression and anxiety, the screener for anxiety was comprised of 9 items instead of full 11 items from the RCMAS Worry/Sensitivity Subscale (36). Findings therefore require replication using clinical diagnostic interviews, the “gold standard” which would allow lifetime and past-12 month prevalence estimates by gender identity. An additional strength is that the documented prevalence of 0.33% gender minority respondents in the GUTS1 cohort is on par with other U.S. estimates which range from 0.3% to 0.5% (39, 40).
Limitations notwithstanding, findings from this study suggest that gender identity is an understudied social determinant of mental health. Surveillance efforts to monitor mental health disparities should include survey questions to assess gender identity. The two-step approach is recommended to identify gender minority respondents in population studies of health (23). Capturing assigned sex at birth and current gender identity will allow for greater understanding of the social epidemiology of depression, anxiety, and other mental health outcomes. It may also lead to additional insights regarding sex and gender differences and etiologic pathways relevant for mental health of all people, gender minority and non-gender minority alike. In light of the current findings, and alongside prior research showing gender minority people represent an underserved population who face significant barriers to accessing quality gender-affirming, non-stigmatizing mental health care (14), research and interventions to understand and ameliorate mental health disparities by gender identity are needed (10).
Acknowledgments
Funding: The Growing Up Today Study is supported by the National Institutes of Health (NIH) under Award Numbers R01 HD057368 and R01 HD066963. Dr. Katz-Wise is supported by K99/R00 HD082340 from the National Institutes of Health. Dr. Austin is additionally supported by Maternal and Child Health Bureau, Health Resources and Services Administration grants T71-MC00009 and T76-MC00001. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no financial conflicts of interest to disclose.
Implications and Contribution Statement: Gender identity is an understudied social determinant of mental health. This study contributes epidemiologic data showing a higher prevalence of depressive and anxious symptoms in gender minorities (i.e., transgender and/or gender nonconforming) relative to non-gender minorities in an U.S. cohort of young adults.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kessler RC, Keller MB, Wittchen HU. The epidemiology of generalized anxiety disorder. Psychiatr Clin North Am. 2001;24(1):19–39. doi: 10.1016/s0193-953x(05)70204-5. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Petukhova M, Samposon NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime com orbid risk of anxiety and mood disorders in the United States. Int J Methods Psychitr Res. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Ruscio AM, Shear K, Wittchen HU. Epidemiology of anxiety disorders. Curr Top Behav Neurosci. 2010;2:21–35. [PubMed] [Google Scholar]
- 4.Kessler RC, Calabrese JR, Farley PA, Gruber MJ, Jewell MA, Katon W, et al. Composite International Diagnostic Interview screening scales for DSM-IV anxiety and mood disorders. Psychol Med. 2013;43(8):1625–37. doi: 10.1017/S0033291712002334. [DOI] [PubMed] [Google Scholar]
- 5.Ruscio AM, Chiu WT, Roy-Byrne P, Stang PE, Stein DJ, Wittchen HU, et al. Broadening the definition of generalized anxiety disorder: effects on prevalence and associations with other disorders in the National Comorbidity Survey Replication. J Anxiety Disord. 2007;21(5):662–76. doi: 10.1016/j.janxdis.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. 2009;66(7):785–95. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pigott TA. Gender differences in the epidemiology and treatment of anxiety disorders. J Clin Psychiatry. 1999;60(18):4–15. [PubMed] [Google Scholar]
- 8.Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. 2003;108(3):163–74. doi: 10.1034/j.1600-0447.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- 9.Weisberg RB. Overview of generalized anxiety disorder: epidemiology, presentation, and course. J Clin Psychiatry. 2009;70(2):4–9. [PubMed] [Google Scholar]
- 10.Institute of Medicine (IOM) The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academic Press; 2011. [PubMed] [Google Scholar]
- 11.Egan SK, Perry DG. Gender identity: a multidimensional analysis with implications for psychosocial adjustment. Dev Psychol. 2001;37(4):451–63. doi: 10.1037//0012-1649.37.4.451. [DOI] [PubMed] [Google Scholar]
- 12.Bockting WO. Transforming the paradigm of transgender health: A field in transition. Sexual and Relationship Therapy. 2009;24(2):103–107. [Google Scholar]
- 13.Hendricks M, Testa R. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychology: Research and Practice. 2012;43:460–467. [Google Scholar]
- 14.American Psychological Association (APA) Task Force on Gender Identity and Gender Variance Report of the Task Force on Gender Identity and Gender Variance. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 15.Simons L, Schrager SM, Clark LF, Belzer M, Olson J. Parental support and mental health among transgender adolescents. J Adolesc Health. 2013;53(6):791–793. doi: 10.1016/j.jadohealth.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129(3):418–25. doi: 10.1542/peds.2011-0907. [DOI] [PubMed] [Google Scholar]
- 17.Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline Physiologic and Psychosocial Characteristics of Transgender Youth Seeking Care for Gender Dysphoria. J Adolesc Health. 2015;57(4):374–380. doi: 10.1016/j.jadohealth.2015.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Budge SL, Adelson JL, Howard KA. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J Consult Clin Psychol. 2013;81(3):545–57. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- 19.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943–51. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. J Homosex. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 21.Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, et al. Gender Abuse and Major Depression Among Transgender Women: A Prospective Study of Vulnerability and Resilience. Am J Public Health. 2014;104(11):2191–2198. doi: 10.2105/AJPH.2013.301545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. J Adolesc Health. 2015;56(3):274–279. doi: 10.1016/j.jadohealth.2014.10.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reisner SL, Deutsch MB, Bhasin S, Bockting W, Brown GR, Feldman J, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):198–207. doi: 10.1097/MED.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Field AE, Camargo CA, Jr, Taylor CB, Berkey CS, Frazier AL, Gillman MW, et al. Overweight, weight concerns, and bulimic behaviors among girls and boys. J Am Acad Child Adolesc Psychiatry. 1999;38(6):754–60. doi: 10.1097/00004583-199906000-00024. [DOI] [PubMed] [Google Scholar]
- 25.Calzo J, Blood E, Austin S, Spiegelman D, Horton N. Recommendations for managing missing data in the Growing Up Today Study. Boston, MA: Boston Children's Hospital; 2014. [Google Scholar]
- 26.Rosario M, Reisner SL, Corliss HL, Wypij D, Frazier AL, Austin SB. Disparities in Depressive Distress by Sexual Orientation in Emerging Adults: The Roles of Attachment and Stress Paradigms. Arch Sex Behav. 2014;43(5):901–916. doi: 10.1007/s10508-013-0129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts AL, Rosario M, Slopen N, Calzo JP, Austin SB. Childhood gender nonconformity, bullying victimization, and depressive symptoms across adolescence and early adulthood: an 11-year longitudinal study. J Am Acad Child Adolesc Psychiatry. 2013;52(2):143–52. doi: 10.1016/j.jaac.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: Validity of natal sex and gender identity survey items in a U.S. national cohort of young adults. BMC Public Health. 2014;14:1224. doi: 10.1186/1471-2458-14-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 30.Bradley KL, Bagnell AL, Brannen CL. Factorial validity of the Center for Epidemiological Studies Depression 10 in adolescents. Issues Ment Health Nurs. 2010;31(6):408–12. doi: 10.3109/01612840903484105. [DOI] [PubMed] [Google Scholar]
- 31.Van Voorhees BW, Fogel J, Reinecke MA, Gladstone T, Stuart S, Gollan J, et al. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. J Dev Behav Pediatr. 2009;30(1):23–37. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reynolds CR, Paget KD. Factor analysis of the revised Children's Manifest Anxiety Scale for blacks, whites, males, and females with a national normative sample. J Consult Clin Psychol. 1981;49(3):352–9. doi: 10.1037//0022-006x.49.3.352. [DOI] [PubMed] [Google Scholar]
- 33.Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH. Assessment of worry in children and adolescents: an adaptation of the Penn State Worry Questionnaire. Behav Res Ther. 1997;35(6):569–81. doi: 10.1016/s0005-7967(96)00116-7. [DOI] [PubMed] [Google Scholar]
- 34.Myers K, Winters NC. Ten-year review of rating scales. II: Scales for internalizing disorders. J Am Acad Child Adolesc Psychiatry. 2002;41(6):634–59. doi: 10.1097/00004583-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Seligman LD, Ollendick TH, Langley AK, Baldacci HB. The utility of measures of child and adolescent anxiety: a meta-analytic review of the Revised Children's Manifest Anxiety Scale, the State-Trait Anxiety Inventory for Children, and the Child Behavior Checklist. J Clin Child Adolesc Psychol. 2004;33(3):557–65. doi: 10.1207/s15374424jccp3303_13. [DOI] [PubMed] [Google Scholar]
- 36.Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: their reliability and validity in a normal adolescent sample. Behav Res Ther. 2002;40(7):753–72. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- 37.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 38.Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Academic Press; 1969. [Google Scholar]
- 39.Gates GJ. How many people are lesbian, gay, bisexual, and transgender? Los Angeles, CA: The Williams Institute, University of California School of Law; 2011. [Google Scholar]
- 40.Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: results from a household probability sample of adults. Am J Public Health. 2012;102(1):118–22. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]