Abstract
African Americans (AAs) have an increased risk for hypertension-related cardiovascular outcomes compared with Whites, which may be related to abnormal left ventricular (LV) structure. We examined the association of prevalent hypertension with concentric remodeling (CR: normal LV mass index [LVMI] and increased relative wall thickness: RWT), eccentric hypertrophy (EH: increased LVMI and normal RWT), and concentric hypertrophy (CH: increased LVMI and increased RWT) within the Jackson Heart Study. Among 4,721 participants (mean ± SD age 55.7±12.7 years), 2,841 (60.2%) had prevalent hypertension, defined as mean clinic BP ≥140/90mmHg or antihypertensive medication use. Prevalent hypertension was associated with a statistically significantly increased odds for having CR (odds ratio [OR] 1.78 95% confidence interval CI: 1.42–2.24), EH (OR 1.68 95%CI: 1.15–2.44), and CH (OR 3.86 95%CI: 2.28–6.54) after multivariable adjustment. In conclusion, in a population-based sample of AAs, hypertension was associated with an increased odds for having abnormal LV structure, particularly CH.
Keywords: hypertension, left ventricular structure, echocardiography
INTRODUCTION
African Americans have a higher risk of hypertension and cardiovascular end-organ damage compared to Whites[1–4]. Hypertension is associated with alterations in cardiac structure, including an increase in left ventricular (LV) mass (LVM),[5] left ventricular hypertrophy (LVH), and relative wall thickness (RWT), the latter being a measure of LV geometry.[5] Based on categorization by LVM index (LVMI: increased LVMI or normal LVMI) and also geometry (increased RWT or normal RWT), individuals can also be categorized into having one of four LV structural patterns: normal pattern (normal LVMI and normal RWT), concentric remodeling (normal LVMI and increased RWT), eccentric hypertrophy (increased LVMI and normal RWT), and concentric hypertrophy (increased LVMI and increased RWT).[6, 7] Each of the three abnormal LV patterns is associated with an increased risk for cardiovascular disease (CVD) events.[8–11] Recently, a classification system has been proposed that further subdivides individuals with eccentric hypertrophy and concentric hypertrophy into four categories based on LV chamber size: eccentric non-dilated and dilated hypertrophy, and concentric non-dilated and dilated hypertrophy.[11–14] Studies have demonstrated that individuals with non-dilated LV hypertrophy, particularly those with eccentric non-dilated hypertrophy, do not have an increased CVD risk.[13, 15, 16]
Scarce data are available from epidemiology studies on the prevalence of abnormal LV structural patterns among African Americans.[17–19] The association between prevalent hypertension and each of the abnormal LV structural patterns among African Americans is also understudied.[8, 20] Further, little is known about the factors associated with each abnormal LV structural pattern among African Americans with prevalent hypertension. Understanding the factors associated with abnormal LV structural patterns among African Americans with hypertension may help identify potential targets for risk factor modification among this group.
In the current study, we determined the prevalence of concentric remodeling, eccentric hypertrophy, and concentric hypertrophy among participants in the Jackson Heart Study (JHS), a large population-based cohort study comprised exclusively of African Americans. Further, we examined the association of prevalent hypertension with each abnormal LV pattern and assessed factors associated with each abnormal pattern among participants with prevalent hypertension. We also secondarily examined non-dilated and dilated subtypes of eccentric hypertrophy and concentric hypertrophy.
MATERIALS AND METHODS
Sample Population
The JHS is a population-based cohort study of 5,301 African-American adults. Details of the study design, recruitment, and data collection have been previously described.[21–26] Briefly, African-American participants were recruited from urban and rural areas of the three counties (Hinds, Madison, and Rankin) that make up the Jackson, MS Metropolitan Statistical Area. Recruitment was restricted to non-institutionalized adult African Americans aged 21–84 years old.[27] There were 5,301 participants who underwent a baseline examination (Exam 1) that consisted of interviewer and self-administered questionnaires, clinic blood pressure (CBP) measurements, blood and urine collection, a pill bottle review and 2D echocardiography. Detailed description of data and specimen collection, and specimen processing during Exam 1 can be found in the online supplement (Supplemental Methods).
Participants (n=318) with incomplete CBP or antihypertensive medication data (i.e., missing information on self-reported antihypertensive medication use or pill bottle review) or incomplete data on LVM and/or RWT from echocardiography (n=262) were excluded, leaving a final sample size of 4,721 participants at Exam 1 for the current analyses. The JHS was approved by the institutional review boards of the participating institutions: the University of Mississippi Medical Center, Jackson State University, and Tougaloo College. All participants provided informed consent. The current analysis was approved by the institutional review boards at the University of Alabama at Birmingham and Columbia University.
Clinic Blood Pressure, Antihypertensive Medication, and Prevalent Hypertension
CBP measurements were taken using a Hawksley random zero sphygmomanometer (Hawksley and Sons Ltd.) and an appropriately sized blood pressure cuff determined by measuring the upper-arm circumference. After a five-minute silent rest, while participants were seated with their back and arm supported, 2 BP measurements (1 minute apart) in the right arm were taken. [27] CBP was defined as the average of the 2 recorded measurements.[27] Antihypertensive medication use was determined by self-report. Participants were also asked to bring any medications taken within 2 weeks prior to the baseline examination to the clinic visit. Pill bottle review and medication coding was performed by a pharmacist using the Medispan dictionary and classified into categories according to the Therapeutic Classification System.[25] For the current analysis, antihypertensive medication use (yes/no) was defined as self-reporting antihypertensive medication use and having at least one class of antihypertensive medication identified during the pill bottle review. Prevalent hypertension was defined as a mean clinic systolic blood pressure (SBP) ≥ 140 mmHg, mean clinic diastolic blood pressure (DBP) ≥ 90 mmHg or antihypertensive medication use.
Echocardiography
Certified technicians performed 2D transthoracic echocardiograms (Sonos-4500, Philips Medical Systems) using standardized protocols.[21] Echocardiograms were reviewed for clinical interpretation and analytical measurements by experienced cardiologists on networked image workstations (Vericis, Camtronics Medical Systems).[21] LV dimensions including LV internal diameter at end diastole (LVEDD, millimeters), interventricular septal thickness in diastole (IVSD, millimeters), and posterior wall thickness in diastole (PWTD, millimeters), were assessed according to the 2D method based on American Society of Echocardiography (ASE) recommendations.[28]
Calculation of Echocardiographic Derived Variables
LVM, LVMI, LVH, and RWT were derived according to ASE recommendations.[28] LVM was calculated using the ASE formula: 0.8 X (1.04 X ((IVSD + LVEDD + PWTD)3 – (LVEDD)3)) + 0.6. LVMI was calculated as LVM/body surface area. LVH was defined as increased LVMI (≥ 96 g/m2 in females; ≥ 116 g/m2 in males).[28] Normal LVMI was defined as < 96 g/m2 in females and <116 g/m2 in males. RWT was calculated using the ASE formula: RWT = 2 x posterior wall thickness in diastole/left ventricular internal dimension in diastole).[28] Increased RWT was defined as RWT > 0.42 and normal RWT was defined as RWT ≤ 0.42.[28] A dilated LV chamber was defined as increased LVEDD (≥ 5.3 cm in females; ≥ 5.9 cm in males); and a non-dilated LV chamber was defined as normal LVEDD (< 5.3 cm in females; < 5.9 cm in males).[28] LV structural patterns (Supplemental Figure 1) were defined as: normal (normal LVMI and normal RWT); concentric remodeling (normal LVMI and increased RWT); eccentric hypertrophy (LVH and normal RWT); and concentric hypertrophy (LVH and increased RWT).[6, 28] In secondary analyses, participants with LVH were subdivided into four groups based on LV chamber size: eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy and concentric dilated hypertrophy. Eccentric non-dilated hypertrophy was defined as LVH, normal RWT, and normal LVEDD, and eccentric dilated hypertrophy was defined as LVH, normal RWT, and increased LVEDD. Concentric non-dilated hypertrophy was defined as LVH, increased RWT, and normal LVEDD, and concentric dilated hypertrophy was defined as LVH, increased RWT, and increased LVEDD.
Clinical Covariates
Trained interviewers administered standard questionnaires to assess demographic characteristics (age, sex, education, marital status), medical history, medication use, and selected health behaviors (alcohol consumption, current smoking, and physical activity).[21, 25] Height and weight were measured and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2). Fasting blood samples and urinary samples were also collected following standardized procedures.[21] Plasma glucose, serum creatinine, hemoglobin A1c, and a lipid profile (including total cholesterol, low density lipoprotein [LDL] cholesterol, and high density lipoprotein [HDL] cholesterol) were quantified using standardized methods.[21] Estimated glomerular filtration rate (eGFR) was calculated via the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.[29] Reduced eGFR was defined as <60 ml/min/1.73 m2.
Statistical Analyses
Baseline characteristics of participants were calculated for participants with normal pattern, eccentric remodeling, eccentric hypertrophy, and concentric hypertrophy, and secondarily, eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy and concentric dilated hypertrophy. These analyses were performed for the overall analytical sample (n=4,721) and among participants with prevalent hypertension (n=2,841). Further, the prevalence of each LV structural pattern was also determined overall, and stratified by prevalent hypertension status. Using normal LV pattern as the reference group, multinomial logistic regression was used to calculate the odds ratios (OR) and 95% confidence intervals (95% CI) for the association of prevalent hypertension with concentric remodeling, eccentric hypertrophy, and concentric hypertrophy. Three models including an unadjusted model were calculated. Multivariable adjusted model 1 included adjustment for age, sex, and BMI. Model 2 included the variables in model 1 plus diabetes, education level, alcohol consumption, smoking status, physical activity, and reduced eGFR (< 60 ml/min/1.73m2). The analytic sample was further restricted to participants with prevalent hypertension to identify correlates of each abnormal LV pattern. Factors that were investigated included the variables in Model 2 plus hemoglobin A1c, total, LDL, and HDL cholesterol, SBP, DBP, and number of classes of antihypertensive medication being taken. Multinomial logistic regression was also used to assess the associations of each exposure variable with the odds of concentric remodeling, eccentric hypertrophy, and concentric hypertrophy compared with normal pattern. All of the variables from Model 2 were included simultaneously in the regression model. In secondary analyses, we repeated the aforementioned analyses for eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy. Sensitivity analyses were performed indexing LVM to height2.7 instead of body surface area. LVH was defined as LVMI ≥ 45 g/m2.7 in females and ≥ 49 g/m2.7 in males.[7, 30] A p-value <0.05 was considered to be statistically significant. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Baseline characteristics
Table 1 shows the characteristics of the 4,721 participants overall, and by LV structural pattern (normal pattern, concentric remodeling, eccentric hypertrophy, and concentric hypertrophy). Among these participants, 64.1% was female, mean ± SD age was 55.7 ± 12.7 years and mean BMI was 31.8 ± 7.2 kg/m2. Also, 60.2% (n=2,841) had prevalent hypertension and 2,299 (48.7%) were taking antihypertensive medication. Diuretics and calcium channel blockers were the most commonly prescribed class of antihypertensive medication. Supplemental Table 1 shows the characteristics of the participants with prevalent hypertension overall, and by LV structural pattern (normal pattern, concentric remodeling, eccentric hypertrophy, and concentric hypertrophy). The characteristics of the participants with eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy among the overall sample and those with prevalent hypertension are shown in Supplemental Tables 2 and 3, respectively.
Table 1.
Characteristics of the Jackson Heart Study Cohort and Participants with Normal Pattern, Concentric Remodeling, Eccentric Hypertrophy, and Concentric Hypertrophy Included in the Current Analyses
| Overall Cohort (n=4,721) | Normal Pattern (n=3,774) | Concentric Remodeling (n=558) | Eccentric Hypertrophy (n=204) | Concentric Hypertrophy (n=185) | |
|---|---|---|---|---|---|
| Demographic Characteristics | |||||
| Age, years | 55.7 ± 12.7 | 54.3 ± 12.6 | 59.9 ± 11.7 | 63.1 ± 10.8 | 64.1 ± 10.4 |
| Female Sex, % | 64.1 | 64.5 | 54.1 | 75.5 | 74.1 |
| Education < HS, % | 20.2 | 17.8 | 26.3 | 34.8 | 35.1 |
| Clinical Characteristics | |||||
| Body mass index (kg/m2) | 31.8 ± 7.2 | 31.6 ± 7.3 | 32.5 ± 7.1 | 31.6 ± 6.6 | 32.5 ± 6.6 |
| Diabetes, % | 22.4 | 20.1 | 30.1 | 29.5 | 37.7 |
| Fasting Glucose, mg/dL | 99.8 ± 32.0 | 98.2 ± 29.0 | 106.8 ± 45.4 | 105.1 ± 38.4 | 106.9 ± 30.9 |
| Hemoglobin A1c, % | 6.0 ± 1.3 | 5.9 ± 1.2 | 6.3 ± 1.5 | 6.2 ± 1.5 | 6.3 ± 1.3 |
| Total Cholesterol, mg/dL | 199.1 ± 39.8 | 198.2 ± 39.0 | 202.0 ± 41.9 | 203.6 ± 42.3 | 204.6 ± 44.8 |
| LDL, mg/dL | 126.2 ± 36.2 | 125.7 ± 36.0 | 128.8 ± 37.8 | 126.4 ± 36.4 | 126.8 ± 37.0 |
| HDL, mg/dL | 52.0 ± 14.7 | 51.9 ± 14.5 | 50.1 ± 15.3 | 55.6 ± 15.9 | 54.4 ± 15.0 |
| eGFR <60 ml/min/1.73 m2 | 7.6 | 6.1 | 11.0 | 17.1 | 18.9 |
| Health Behaviors | |||||
| Alcohol consumption, % | 44.5 | 45.8 | 43.7 | 36.3 | 30.6 |
| Current Smoking, % | 12.7 | 12.6 | 10.3 | 16.7 | 16.4 |
| Total Physical activity score | 8.3 ± 2.6 | 8.5 ± 2.6 | 8.0 ± 2.6 | 7.5 ± 2.6 | 7.3 ± 2.7 |
| Blood pressure measures | |||||
| Mean clinic SBP, mmHg | 127.1 ± 18.3 | 125.1 ± 17.1 | 132.8 ± 19.9 | 136.9 ± 21.8 | 139.6 ± 21.1 |
| Mean clinic DBP, mmHg | 78.7 ± 10.5 | 78.5 ± 10.2 | 80.4 ± 11.5 | 78.5 ± 11.8 | 78.9 ± 11.8 |
| Antihypertensive medication use, % | 48.7 | 44.9 | 62.0 | 62.3 | 71.9 |
| Class of Antihypertensive Medication | |||||
| Diuretics | 65.6 | 66.0 | 62.4 | 67.7 | 66.2 |
| Beta-blocker | 23.7 | 22.8 | 23.4 | 31.5 | 27.8 |
| Calcium Channel Blockers | 40.4 | 38.4 | 44.5 | 44.9 | 51.1 |
| ACE-I | 39.7 | 38.7 | 43.9 | 44.9 | 36.8 |
| ARBs | 17.7 | 18.0 | 17.6 | 14.2 | 18.1 |
| Prevalent hypertension, % | 60.2 | 55.8 | 74.6 | 76.0 | 88.1 |
| Echocardiographic measures | |||||
| Interventricular septum thickness in diastole, mm | 9.1 ± 1.9 | 8.6 ± 1.2 | 10.4 ± 1.4 | 10.7 ± 1.4 | 12.9 ± 5.4 |
| Left ventricular internal dimension in diastole, mm | 48.5 ± 4.6 | 48.6 ± 4.0 | 44.4 ± 3.9 | 56.1 ± 6.0 | 49.0 ± 4.5 |
| Posterior wall thickness in diastole, mm | 8.6 ± 1.7 | 8.1 ± 1.0 | 10.4 ± 1.0 | 9.7 ± 1.2 | 12.6 ± 3.5 |
| Relative wall thickness | 0.36 ± 0.08 | 0.33 ± 0.04 | 0.47 ± 0.05 | 0.35 ± 0.05 | 0.52 ± 0.15 |
| Left ventricular mass index (g/m2) | 75.0 ± 24.0 | 69.5 ± 13.6 | 78.7 ± 14.7 | 117.7 ± 20.8 | 129.5 ± 65.0 |
Data are expressed as percentage or mean ± SD
ACE-I=angiotensin converting enzyme inhibitors, ARBs=angiotensin II receptor blockers, DBP= diastolic blood pressure, eGFR= estimated glomerular filtration ratio, HDL= high density lipoprotein, HS= high school, LDL= low density lipoprotein, SBP=systolic blood pressure
LVH: left ventricular hypertrophy, LVMI: left ventricular mass index, RWT: relative wall thickness
LVH is defined as increased LVMI ≥ 96 g/m2 in females and ≥ 116 g/m2 in males. Normal LVMI is defined as < 96 g/m2 in females and < 116 g/m2 in males. Increased RWT is defined as RWT > 0.42. Normal RWT is defined as RWT ≤ 0.42.
Normal pattern is defined as: normal LVMI and normal RWT.
Concentric remodeling is defined as: normal LVMI and increased RWT.
Eccentric hypertrophy is defined as: LVH and normal RWT.
Concentric hypertrophy is defined as: LVH and increased RWT.
The Prevalence of LV Structural Patterns
Among the overall sample, 8.2% of participants had LVH and 15.7% had increased RWT. The prevalence of concentric remodeling, eccentric hypertrophy, and concentric hypertrophy was 11.8%, 4.3%, and 3.9%, respectively; 80.0% had a normal pattern. The prevalence of eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy was 2.0%, 2.3%, 3.4%, and 0.5%, respectively. Among participants with eccentric hypertrophy, 46.1% and 53.9% had eccentric non-dilated hypertrophy and eccentric dilated hypertrophy, respectively. Among participants with concentric hypertrophy, 88.1% and 11.9% had concentric non-dilated hypertrophy and concentric dilated hypertrophy, respectively.
Association of prevalent hypertension with each abnormal LV pattern
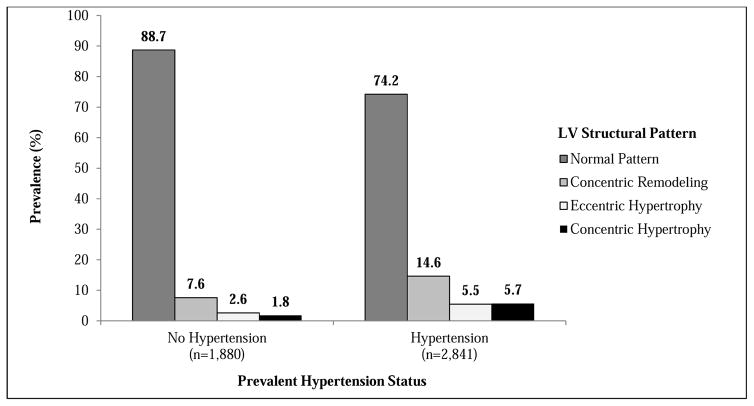
Concentric remodeling was the most common abnormal LV pattern among participants with versus without prevalent hypertension (Figure 1). In an unadjusted model (Table 2), prevalent hypertension was associated with increased odds of having concentric remodeling, eccentric hypertrophy, and concentric hypertrophy. These associations remained present after adjustment for age, sex, and BMI (Model 1) and further adjusting for diabetes, education level, alcohol consumption, smoking status, physical activity, and reduced eGFR (Model 2).
Figure 1.
Prevalence of Normal Pattern, Concentric Remodeling, Eccentric Hypertrophy, and Concentric Hypertrophy Stratified by Prevalent Hypertension Status
Abbreviations: LV=Left ventricular
Table 2.
Association of Prevalent Hypertension with Concentric Remodeling, Eccentric Hypertrophy, and Concentric Hypertrophy versus Normal Pattern
| Odds Ratio (95% Confidence Interval) | |||
|---|---|---|---|
| Crude | Model 1 | Model 2 | |
| Normal Pattern | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| Concentric Remodeling | 2.32 (1.90 – 2.83) | 1.72 (1.39 – 2.13) | 1.78 (1.42 – 2.24) |
| Eccentric Hypertrophy | 2.50 (1.80 – 3.47) | 1.58 (1.12 – 2.23) | 1.68 (1.15 – 2.44) |
| Concentric Hypertrophy | 5.86 (3.74 – 9.19) | 3.54 (2.23 – 5.62) | 3.86 (2.28 – 6.54) |
Model 1- adjusted for age, sex, body mass index.
Model 2- adjusted for age, sex, body mass index, diabetes, education less than high school, alcohol consumption (none: 0 drinks/week; moderate consumption: 1–14 and 1–7 alcoholic drinks/week for men and women; heavy consumption: >14 and >7 alcoholic drinks/week for men and women), current smoking status, physical activity, and estimated glomerular filtration rate <60 ml/min/1.73 m2.
LVH: left ventricular hypertrophy, LVMI: left ventricular mass index, RWT: relative wall thickness
LVH is defined as increased LVMI ≥ 96 g/m2 in females and ≥ 116 g/m2 in males. Normal LVMI is defined as < 96 g/m2 in females and < 116 g/m2 in males. Increased RWT is defined as RWT > 0.42.
Normal RWT is defined as RWT ≤ 0.42.
Normal pattern is defined as: normal LVMI and normal RWT.
Concentric remodeling is defined as: normal LVMI and increased RWT.
Eccentric hypertrophy is defined as: LVH and normal RWT.
Concentric hypertrophy is defined as: LVH and increased RWT.
Supplemental Figure 2 shows the prevalence of eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy among participants with versus without prevalent hypertension. In unadjusted and adjusted models, prevalent hypertension was associated with increased odds of having eccentric non-dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy (Supplemental Table 4).
Correlates of each abnormal LV pattern among participants with prevalent hypertension
After full multivariable adjustment and among participants with prevalent hypertension, older age was associated with increased odds of concentric remodeling, eccentric hypertrophy, and concentric hypertrophy (Table 3). Also, male sex was associated with increased odds of having concentric remodeling, but a lower odds of having eccentric hypertrophy. Current smoking was associated with lower odds of having concentric remodeling but higher odds of having eccentric hypertrophy and concentric hypertrophy. Higher clinic SBP was associated with higher odds of having concentric remodeling, eccentric hypertrophy, and concentric hypertrophy. Taking one class and ≥ 4 classes of antihypertensive medication was associated with higher odds of having concentric remodeling and eccentric hypertrophy, respectively. Supplemental Table 5 shows the correlates of eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy among participants with prevalent hypertension.
Table 3.
Correlates of Concentric Remodeling, Eccentric Hypertrophy and Concentric Hypertrophy versus Normal Pattern among Participants with Prevalent Hypertension
| Participant Characteristics | Odds Ratioa (95% Confidence Interval) | ||
|---|---|---|---|
| Concentric Remodeling | Eccentric Hypertrophy | Concentric Hypertrophy | |
| Age (per 10 year increase) | 1.33 (1.15 – 1.55) | 1.44 (1.12 – 1.85) | 1.37 (1.08 – 1.73) |
| Sex (male vs. female) | 1.52 (1.14 – 2.01) | 0.44 (0.26 – 0.76) | 0.68 (0.43 – 1.09) |
| BMI (per 5 kg/m2 increase) | 1.07 (0.98 – 1.18) | 0.96 (0.82 – 1.11) | 1.01 (0.88 – 1.16) |
| Education less than high school (yes vs. no) | 0.97 (0.71 – 1.32) | 1.23 (0.79 – 1.93) | 1.05 (0.69 – 1.62) |
| Alcohol consumption | |||
| None | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.31 (1.00 – 1.73) | 0.96 (0.59 – 1.57) | 0.67 (0.41 – 1.08) |
| Heavy | 1.87 (0.89 – 3.91) | 0.32 (0.04 – 2.53) | 0.49 (0.11 – 2.25) |
| Current smoking (yes vs. no) | 0.61 (0.38 – 0.97) | 2.36 (1.33 – 4.18) | 2.23 (1.29 – 3.85) |
| Diabetes (yes vs. no) | 1.08 (0.74 – 1.59) | 0.87 (0.47 – 1.63) | 1.43 (0.83 – 2.48) |
| Hemoglobin A1c (per 1% increase) | 1.04 (0.91 – 1.19) | 1.08 (0.87 – 1.35) | 0.99 (0.81 – 1.22) |
| Total Physical activity score (per unit increase) | 1.03 (0.98 – 1.08) | 1.03 (0.95 – 1.12) | 1.01 (0.94 – 1.10) |
| Total Cholesterol, mg/dL (per 10mg/dL increase) | 1.05 (0.94 – 1.17) | 1.03 (0.85 – 1.24) | 1.04 (0.88 – 1.23) |
| LDL, mg/dL (per 10mg/dL increase) | 0.97 (0.86 – 1.09) | 0.97 (0.80 – 1.19) | 0.98 (0.82 – 1.18) |
| HDL, mg/dL (per 10mg/dL increase) | 0.91 (0.81 – 1.03) | 1.00 (0.83 – 1.22) | 1.01 (0.84 – 1.21) |
| eGFR <60 ml/min/1.73 m2 (yes vs. no) | 1.04 (0.69 – 1.57) | 1.46 (0.84 – 2.54) | 1.48 (0.88 – 2.49) |
| Clinic SBP (per 10 mmHg increase) | 1.15 (1.06 – 1.24) | 1.31 (1.17 – 1.47) | 1.28 (1.15 – 1.42) |
| Clinic DBP (per 5 mmHg increase) | 1.02 (0.94 – 1.09) | 0.96 (0.86 – 1.07) | 0.96 (0.87 – 1.07) |
| Number of classes of antihypertensive medications | |||
| 0 | 1 (referent) | 1 (referent) | 1 (referent) |
| 1 | 1.48 (1.01 – 2.16) | 1.24 (0.67 – 2.30) | 1.09 (0.62 – 1.90) |
| 2 | 1.41 (0.96 – 2.08) | 1.33 (0.73 – 2.44) | 1.02 (0.58 – 1.78) |
| 3 | 1.39 (0.88 – 2.21) | 1.27 (0.61 – 2.66) | 1.17 (0.61 – 2.26) |
| ≥ 4 | 1.14 (0.93 – 1.40) | 1.48 (1.17 – 1.88) | 1.16 (0.89 – 1.52) |
All participant characteristics are included in the multivariable adjusted model: age, sex, body mass index, diabetes, education less than high school, alcohol consumption (none: 0 drinks/week; moderate consumption: 1–14 and 1–7 alcoholic drinks/week for men and women; heavy consumption: >14 and >7 alcoholic drinks/week for men and women), current smoking status (yes vs. no), physical activity, total cholesterol, low density lipoprotein cholesterol, high density lipoprotein cholesterol, estimated glomerular filtration rate <60 ml/min/1.73 m2, clinic systolic blood pressure, clinic diastolic blood pressure, and number of classes of antihypertensive medications.
DBP: diastolic blood pressure, eGFR: estimated glomerular filtration rate, HDL: high density lipoprotein cholesterol, HS: high school, LDL: low density lipoprotein cholesterol, SBP: systolic blood pressure.
LVH: left ventricular hypertrophy, LVMI: left ventricular mass index, RWT: relative wall thickness
LVH is defined as increased LVMI ≥ 96 g/m2 in females and ≥ 116 g/m2 in males. Normal LVMI is defined as < 96 g/m2 in females and < 116 g/m2 in males. Increased RWT is defined as RWT > 0.42. Normal RWT is defined as RWT ≤ 0.42.
Normal pattern (referent) is defined as: normal LVMI and normal RWT.
Concentric remodeling is defined as: normal LVMI and increased RWT.
Eccentric hypertrophy is defined as: LVH and normal RWT.
Concentric hypertrophy is defined as: LVH and increased RWT.
Sensitivity analysis after indexing LVM to height2.7 instead of body surface area
Prevalent hypertension was associated with concentric remodeling, eccentric hypertrophy, and concentric hypertrophy (Supplemental Table 6), and eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy (Supplemental Table 7) when indexing LVM to height2.7 instead of body surface area. The correlates of concentric remodeling, eccentric hypertrophy, and concentric hypertrophy among participants with prevalent hypertension in a fully adjusted model are shown in Supplemental Table 8. The results are similar to the analyses for which LVM was indexed to body surface area with a few notable exceptions including BMI, alcohol use, reduced eGFR, and number of antihypertensive classes. Higher BMI was associated with an increased odds of having eccentric hypertrophy and concentric hypertrophy. Further, moderate and heavy alcohol consumption was also associated with increased odds of concentric remodeling, whereas reduced eGFR was associated with having an increased odds of eccentric hypertrophy. Taking ≥ 4 classes of antihypertensive medication was associated with a higher odds of having eccentric hypertrophy and concentric hypertrophy.
DISCUSSION
An abnormal LV pattern (concentric remodeling, eccentric hypertrophy, and concentric hypertrophy) was present in 20% of African Americans in the JHS cohort. Concentric remodeling was the most common abnormal LV pattern followed by eccentric hypertrophy and concentric hypertrophy. Further, after multivariable adjustment, prevalent hypertension was associated with an approximately two-fold greater odds for having concentric remodeling and eccentric hypertrophy and an approximately four-fold greater odds for having concentric hypertrophy.
The current findings that among JHS participants, concentric remodeling was the most common abnormal LV structural pattern, is consistent with the findings of Nkomo et al.[18] and Fox et al.[17] who both examined the prevalence of LV structural patterns in a smaller number of African American participants (1,543 and 1,849 participants, respectively) within the Atherosclerosis Risk in Communities (ARIC) study. In both studies, concentric hypertrophy was the second most common abnormal LV pattern. Scarce data exist on the associations between prevalent hypertension and abnormal LV structural patterns in African Americans. Among 1,849 African Americans in the ARIC study, the prevalence of hypertension was higher in individuals who had concentric remodeling, concentric hypertrophy, or eccentric hypertrophy compared to those with a normal pattern.[17] However, this previous study did not report whether prevalent hypertension was associated with an abnormal LV pattern after adjusting for potential confounders. In the current study, prevalent hypertension was associated with a higher odds of having all three abnormal LV patterns after multivariable adjustment with the strongest association observed with concentric hypertrophy.
It has been proposed that LVH is a compensatory mechanism that reduces wall stress and maintains LV systolic function in response to increased BP and afterload. However, once increased BP and afterload have exceeded the heart’s compensatory mechanism, the LV chamber eventually dilates, leading to a reduced ejection fraction and systolic heart failure.[31] A recently proposed classification subdivides eccentric hypertrophy and concentric hypertrophy into four new categories based on the presence or absence of LV chamber dilation: eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy.[11–14] Few prior studies have examined these LVH patterns in African Americans.[13, 16] In the current study, in a fully adjusted model, prevalent hypertension was associated with a higher odds of eccentric non-dilated hypertrophy, eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy with the strongest association being observed for concentric dilated hypertrophy. In a substudy of the Dallas Heart Study, which included approximately 48% African Americans, participants with eccentric dilated hypertrophy, concentric non-dilated hypertrophy, and concentric dilated hypertrophy had an increased risk of CVD events, compared to participants without LVH.[16] In contrast, participants with eccentric non-dilated hypertrophy had no increased CVD risk. Similar findings were found in a Losartan Intervention for Endpoint Reduction (LIFE) substudy, which included participants with hypertension of whom approximately 14% were African American.[13] Therefore, African Americans with eccentric non-dilated hypertrophy, which comprised 46.1% of those with eccentric hypertrophy in the current study, may not have an increased CVD risk.
The current study also provides a better understanding of the clinical factors associated with abnormal LV patterns among African American adults with prevalent hypertension. In the current analysis, older age was associated with concentric remodeling, eccentric hypertrophy, and concentric hypertrophy among participants with prevalent hypertension, a finding consistent with prior studies.[32] Current smoking status was associated with increased odds for eccentric hypertrophy and concentric hypertrophy among African Americans with prevalent hypertension. These results extend the findings of Gidding et al. [20] who reported an association between smoking and increased LVM and increased RWT among African American and White participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. In the current analysis, higher SBP was also associated with concentric remodeling, eccentric hypertrophy, and concentric hypertrophy. In contrast, higher BMI was not associated with any of the three abnormal LV patterns. This latter finding may be explained by the high prevalence of obesity in JHS, and that defining LVH using LVM indexed to body surface area may obscure an association between BMI and LVH.[7, 33] In the current study, higher BMI was associated with a higher odds of eccentric and concentric hypertrophy when LVH was defined using LVM indexed to height2.7. Although a prior study by Fox et al.[19] demonstrated that impaired fasting blood glucose was associated with a higher prevalence of concentric remodeling (p=0.05) among 1,512 African American women in the JHS cohort, the current study did not find an association between diabetes and elevated hemoglobin A1c levels with any of the three abnormal LV structural patterns. Methodological differences between the study by Fox et al.[19] and the current study include the overall sample size (2,399 men and women vs. 4,721 men and women, respectively) and the prevalence of diabetes (12.6% vs. 22.4%, respectively). Further, sex-stratified analyses were utilized in the study by Fox et al.[19] Therefore, by studying all three abnormal LV structural patterns, the current study extends the analyses of Fox, which examined the association between fasting blood glucose categories and concentric remodeling.[19]
There are several strengths and limitations of our study. First we used data from a large population-based cohort of African Americans. This study also had missing echocardiographic data in only a small number of JHS participants. Although duration of hypertension has been shown to influence LV structural patterns,[34, 35] we were unable to examine the association between hypertension duration and abnormal LV patterns within the JHS. Lastly, since the JHS only included echocardiographic assessment at baseline exam, we could not examine the change in abnormal LV patterns or the determinants of each abnormal LV pattern over time.
In conclusion, approximately 1 out of 5 African Americans in the current study had an abnormal LV pattern. Prevalent hypertension was associated with an increased odds of having concentric remodeling, eccentric hypertrophy (both non-dilated and dilated eccentric hypertrophy), and concentric hypertrophy (both non-dilated and dilated concentric hypertrophy). The odds were highest for concentric hypertrophy, particularly concentric dilated hypertrophy. Our results also indicate that smoking is a risk factor for eccentric and concentric hypertrophy whereas older age and higher SBP are risk factors associated with concentric remodeling, eccentric hypertrophy, and concentric hypertrophy among African Americans with prevalent hypertension. Additional studies are needed to examine which abnormal LV structural pattern explains the increased CVD risk associated with hypertension in African Americans. Future studies should also examine whether smoking cessation and blood pressure control reduce the risk of having alterations in cardiac structure among African Americans with prevalent hypertension.
Supplementary Material
HIGHLIGHTS.
In the Jackson Heart Study, 20% of African Americans have abnormal LV structural patterns.
Concentric remodeling is the most common abnormal LV structural pattern.
Among participants with LVH, concentric non-dilated hypertrophy is the most common abnormal LV structural pattern.
Prevalent hypertension is strongly associated with concentric hypertrophy, especially concentric dilated hypertrophy.
Acknowledgments
The authors would like to thank the Jackson Heart Study participants, investigators, and staff for their valuable contributions and long-term commitment to the study.
FUNDING SOURCES
The Jackson Heart Study is supported and conducted in collaboration with Jackson State University (N01-HC-95170); University of Mississippi Medical Center (N01-HC-95171); and Touglaoo College (N01-HC-95172) and contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD) at the National Institutes of Health (NIH). This work was also supported by the NIH (HL047540, HL117323, HL117323-02S2, K24-HL125704) from the NHLBI, Bethesda, MD.
Footnotes
Conflict of Interest: Dr. Paul Muntner received an institutional grant from Amgen Inc. There are no other potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
John N. Booth, III, Email: Booth-jnbooth@uab.edu.
Keith M. Diaz, Email: Diaz-kd2442@cumc.columbia.edu.
Mario Sims, Email: Sims-msims2@umc.edu.
Paul Muntner, Email: Muntner-pmuntner@uab.edu.
Daichi Shimbo, Email: Shimbo-ds2231@cumc.columbia.edu.
References
- 1.Cooper RS, Wolf-Maier K, Luke A, Adeyemo A, Banegas JR, Forrester T, et al. An international comparative study of blood pressure in populations of European vs. African descent. BMC Med. 2005;3:2. doi: 10.1186/1741-7015-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH, Jr, et al. Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56(5):780–800. doi: 10.1161/HYPERTENSIONAHA.110.152892. [DOI] [PubMed] [Google Scholar]
- 3.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–52. [PubMed] [Google Scholar]
- 4.Oparil S, Wright JT., Jr Ethnicity and blood pressure. J Clin Hypertens (Greenwich) 2005;7(6):357–64. doi: 10.1111/j.1524-6175.2005.04103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devereux RB, de Simone G, Ganau A, Roman MJ. Left ventricular hypertrophy and geometric remodeling in hypertension: stimuli, functional consequences and prognostic implications. Journal of hypertension Supplement : official journal of the International Society of Hypertension. 1994;12(10):S117–27. [PubMed] [Google Scholar]
- 6.Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19(7):1550–8. doi: 10.1016/0735-1097(92)90617-v. [DOI] [PubMed] [Google Scholar]
- 7.Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the Use of Echocardiography in Adult Hypertension: A Report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) J Am Soc Echocardiogr. 2015;28(7):727–54. doi: 10.1016/j.echo.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Santos M, Shah AM. Alterations in cardiac structure and function in hypertension. Curr Hypertens Rep. 2014;16(5):428. doi: 10.1007/s11906-014-0428-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sehgal S, Drazner MH. Left ventricular geometry: does shape matter? Am Heart J. 2007;153(2):153–5. doi: 10.1016/j.ahj.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Toprak A, Wang H, Chen W, Paul T, Srinivasan S, Berenson G. Relation of childhood risk factors to left ventricular hypertrophy (eccentric or concentric) in relatively young adulthood (from the Bogalusa Heart Study) Am J Cardiol. 2008;101(11):1621–5. doi: 10.1016/j.amjcard.2008.01.045. [DOI] [PubMed] [Google Scholar]
- 11.Cuspidi C, Facchetti R, Bombelli M, Sala C, Tadic M, Grassi G, et al. Risk of mortality in relation to an updated classification of left ventricular geometric abnormalities in a general population: the Pamela study. J Hypertens. 2015 doi: 10.1097/HJH.0000000000000658. [DOI] [PubMed] [Google Scholar]
- 12.Khouri MG, Peshock RM, Ayers CR, de Lemos JA, Drazner MH. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: the Dallas heart study. Circ Cardiovasc Imaging. 2010;3(2):164–71. doi: 10.1161/CIRCIMAGING.109.883652. [DOI] [PubMed] [Google Scholar]
- 13.Bang CN, Gerdts E, Aurigemma GP, Boman K, de Simone G, Dahlof B, et al. Four-group classification of left ventricular hypertrophy based on ventricular concentricity and dilatation identifies a low-risk subset of eccentric hypertrophy in hypertensive patients. Circ Cardiovasc Imaging. 2014;7(3):422–9. doi: 10.1161/CIRCIMAGING.113.001275. [DOI] [PubMed] [Google Scholar]
- 14.Tadic M, Cuspidi C, Majstorovic A, Kocijancic V, Celic V. The relationship between left ventricular deformation and different geometric patterns according to the updated classification: findings from the hypertensive population. J Hypertens. 2015;33(9):1954–61. doi: 10.1097/HJH.0000000000000618. discussion 61. [DOI] [PubMed] [Google Scholar]
- 15.de Simone G, Izzo R, Aurigemma GP, De Marco M, Rozza F, Trimarco V, et al. Cardiovascular risk in relation to a new classification of hypertensive left ventricular geometric abnormalities. J Hypertens. 2015;33(4):745–54. doi: 10.1097/HJH.0000000000000477. discussion 54. [DOI] [PubMed] [Google Scholar]
- 16.Garg S, de Lemos JA, Ayers C, Khouri MG, Pandey A, Berry JD, et al. Association of a 4-Tiered Classification of LV Hypertrophy With Adverse CV Outcomes in the General Population. JACC Cardiovascular imaging. 2015;8(9):1034–41. doi: 10.1016/j.jcmg.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fox ER, Taylor J, Taylor H, Han H, Samdarshi T, Arnett D, et al. Left ventricular geometric patterns in the Jackson cohort of the Atherosclerotic Risk in Communities (ARIC) Study: clinical correlates and influences on systolic and diastolic dysfunction. Am Heart J. 2007;153(2):238–44. doi: 10.1016/j.ahj.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Nkomo VT, Arnett DK, Benjamin EJ, Liebson PR, Hutchinson RG, Skelton TN. Left ventricular structure and systolic function in African Americans: the Atherosclerosis Risk in Communities (ARIC) study. Ethn Dis. 2004;14(4):483–8. [PubMed] [Google Scholar]
- 19.Fox ER, Sarpong DF, Cook JC, Samdarshi TE, Nagarajarao HS, Liebson PR, et al. The relation of diabetes, impaired fasting blood glucose, and insulin resistance to left ventricular structure and function in African Americans: the Jackson Heart Study. Diabetes Care. 2011;34(2):507–9. doi: 10.2337/dc10-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gidding SS, Liu K, Colangelo LA, Cook NL, Goff DC, Glasser SP, et al. Longitudinal determinants of left ventricular mass and geometry: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Circ Cardiovasc Imaging. 2013;6(5):769–75. doi: 10.1161/CIRCIMAGING.112.000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, et al. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328(3):131–44. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Dubbert PM, Carithers T, Ainsworth BE, Taylor HA, Jr, Wilson G, Wyatt SB. Physical activity assessment methods in the Jackson Heart Study. Ethn Dis. 2005;15(4 Suppl 6):S6-56–61. [PubMed] [Google Scholar]
- 23.Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez-Mohammed ML, Calvin RL, et al. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15(4 Suppl 6):S6-38–48. [PubMed] [Google Scholar]
- 24.Taylor HA., Jr The Jackson Heart Study: an overview. Ethn Dis. 2005;15(4 Suppl 6):S6-1–3. [PubMed] [Google Scholar]
- 25.Taylor HA, Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, et al. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15(4 Suppl 6):S6-4–17. [PubMed] [Google Scholar]
- 26.Fuqua SR, Wyatt SB, Andrew ME, Sarpong DF, Henderson FR, Cunningham MF, et al. Recruiting African-American research participation in the Jackson Heart Study: methods, response rates, and sample description. Ethn Dis. 2005;15(4 Suppl 6):S6-18–29. [PubMed] [Google Scholar]
- 27.Wyatt SB, Akylbekova EL, Wofford MR, Coady SA, Walker ER, Andrew ME, et al. Prevalence, awareness, treatment, and control of hypertension in the Jackson Heart Study. Hypertension. 2008;51(3):650–6. doi: 10.1161/HYPERTENSIONAHA.107.100081. [DOI] [PubMed] [Google Scholar]
- 28.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr. 2015;28(1):1–39. e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Lip G, Hall JE. Comprehensive Hypertension. Mosby Elsevier; 2007. [Google Scholar]
- 32.Kizer JR, Arnett DK, Bella JN, Paranicas M, Rao DC, Province MA, et al. Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network study. Hypertension. 2004;43(6):1182–8. doi: 10.1161/01.HYP.0000128738.94190.9f. [DOI] [PubMed] [Google Scholar]
- 33.Cuspidi C, Meani S, Negri F, Giudici V, Valerio C, Sala C, et al. Indexation of left ventricular mass to body surface area and height to allometric power of 2. 7: is the difference limited to obese hypertensives? J Hum Hypertens. 2009;23(11):728–34. doi: 10.1038/jhh.2009.16. [DOI] [PubMed] [Google Scholar]
- 34.Akintunde A, Akinwusi O, Opadijo G. Left ventricular hypertrophy, geometric patterns and clinical correlates among treated hypertensive Nigerians. The Pan African medical journal. 2010;4:8. doi: 10.4314/pamj.v4i1.53602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silangei LK, Maro VP, Diefenthal H, Kapanda G, Dewhurst M, Mwandolela H, et al. Assessment of left ventricular geometrical patterns and function among hypertensive patients at a tertiary hospital, Northern Tanzania. BMC cardiovascular disorders. 2012;12:109. doi: 10.1186/1471-2261-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.