Abstract
Introduction
Because California is home to one in eight U.S. children and accounts for the highest Medicaid and Children’s Health Insurance Program spending, childhood obesity trends in California have important implications for the entire nation. California’s racial/ethnic diversity and large school-based data set provide a unique opportunity to examine trends by race/ethnicity, including understudied Asian and American Indian youth, which has not been possible using national data sets. This study examined racial/ethnic disparities in prevalence of high BMI from 2003 to 2012.
Methods
This observational study included 11,624,865 BMI records from repeated cross-sections of fifth, seventh, and ninth graders who underwent California’s school-based fitness testing. Analyses conducted in 2015 used logistic regression to identify trends in prevalence of high BMI (BMI ≥85th, 95th, and 97th percentiles) and differences in trends by race/ethnicity from 2003 to 2012.
Results
African American and Hispanic girls and American Indian boys increased in prevalence of high BMI, whereas non-Hispanic white and Asian youth and Hispanic boys decreased in prevalence of high BMI (p-values<0.05) from 2003 to 2012. Over this period, African American, Hispanic, and American Indian youth had higher slopes for trends in high BMI than non-Hispanic white youth (p-values<0.05).
Conclusions
Based on California’s statewide data, there is evidence that racial/ethnic disparities in prevalence of high BMI have widened over time. Minority youth have either decreased more slowly or increased in prevalence compared with non-Hispanic white youth. There continues to be an urgent need for policies and interventions that effectively reduce racial/ethnic obesity prevalence disparities.
Introduction
The prevalence of childhood obesity in the U.S. increased at an unprecedented rate from 1971 to 2000,1 but appears to have leveled off over the last decade.2 Nevertheless, obesity remains stubbornly high among adolescents,2 which is worrisome given the associated risks for serious health conditions3–5 that increase with severity of obesity.6,7
Of further concern are racial/ethnic disparities in obesity prevalence. African American and Hispanic youth have consistently exhibited a higher prevalence of obesity than non-Hispanic white youth.2,8,9 The extent to which disparities are changing over time, both at national and local levels, is a fundamental metric by which progress can be measured toward meeting the Healthy People 2020 goal to “achieve health equity and eliminate health disparities.”10 Recent studies that have examined changes in disparities have had mixed results. An analysis of 1999–2008 National Health and Nutrition Examination Survey (NHANES) data did not find differences in obesity trends over time by race/ethnicity,11 but other studies have indicated growing disparities at either the national12,13 or local and state levels.14–16 Incongruous results between the NHANES analysis11 and others may be due in part to a relatively small sample size with large SEs for prevalence in NHANES, which limits the ability to detect differences in trends by race/ethnicity.
Since 2001, California has collected BMI data on approximately 1 million fifth, seventh, and ninth grade public school students annually through its state-mandated FITNESSGRAM© assessment.17 These data provide a large enough sample size to examine differences in obesity trends by race/ethnicity and include understudied Asian and American Indian youth, who have not been represented in NHANES. Additionally, understanding obesity trends in California can inform not only state but federal allocation of treatment and prevention resources given that California is home to one in eight youth aged <18 years, including >25% of the Hispanic, 30% of the Asian, and >10% of the American Indian youth in the U.S.18 California is also responsible for the highest Medicaid and Children’s Health Insurance Program spending.19
Using BMI data collected through California’s annual FITNESSGRAM© assessment, this study examined trends in childhood obesity by race/ethnicity from 2003 to 2012 to ascertain whether prevalence of high BMI has increased, stabilized, or declined over the past decade.
Methods
This study used STROBE recommendations to guide reporting.20
Population and Measures
To examine trends in high BMI, annual student-level data from 2003 to 2012 were obtained from the California Department of Education (CDE), and total enrollment data were obtained from the CDE website.17 Records included gender, grade, age (months), height, weight, and race/ethnicity (African American, American Indian/Alaskan Native, Asian [including Filipino and Pacific Islander], Hispanic/Latino, and white not of Hispanic origin). Designated school personnel (e.g., school nurse or physical education teacher) measured student height and weight each spring as part of FITNESSGRAM©, a fitness battery developed by the Cooper institute21 that includes six domains (e.g., body composition, aerobic capacity, flexibility). CDE FITNESSGRAM© training materials (https://pftdata.org/) specify that school personnel measure height and weight without shoes in a location that provides privacy for the student. On a standard form, height is recorded to the last whole inch and weight to the nearest pound. Although school personnel are supposed to review training materials to ensure standardized data collection and reporting, compliance is unmonitored. However, in Texas, which also mandates FITNESSGRAM©, a study found 96% agreement between teacher and trained expert FITNESSGRAM© measurements of BMI.22
A total of 13,945,046 student records from 2003 to 2012 were examined, representing 93.5% of fifth, seventh, and ninth graders enrolled during this period. This analysis excluded 2,127, 220 (15%) records because of missing/invalid data: 1,454 records were missing gender; 22,386 were missing or had an implausible age (fifth grader aged <8 years or >13 years; seventh grader aged <10 years or >15 years; ninth grader aged <12 years or >17 years); 1,931,157 were missing height or weight; and 172,223 had biologically implausible23 height, weight, or BMI or absolute BMI z-score >5. This left 11,817,826 records with valid BMI and age. In 2011, the CDE changed its race categories to include the option of two or more races, which applied to 115,933 (4%) records with valid data in 2011 and 2012. To improve the consistency of race/ethnicity categories across years, records with two or more races were replaced with a single race designation if one race had been reported for a student in a prior year (56,976 records, 49% of those with two or more races). Students categorized as two or more races without a prior single designation and students with an unknown or “other” race (n=192,961) were excluded, leaving an analytic sample of 11,624,865 youth aged 8–17 years from 2003 to 2012 (83% of CDE records and 78% of total enrollment). Because records began to be linked in 2008, only 33% of records were linked to another year’s record from 2003 to 2012.
Based on gender- and age-specific BMI percentile, each record was assigned an indicator for high BMI for each cut-point: BMI ≥85th (CDC definition of “overweight or obese”24), BMI ≥95th percentile (CDC definition of “obese”24), and BMI ≥97th percentile. BMI ≥97th percentile was included because of the added health risks associated with severe obesity. BMI percentiles were determined using BMI z-scores calculated in SAS, version 9.3 using CDC’s program.23 The University of California, Berkeley Committee for the Protection of Human Subjects approved this research.
Statistical Analysis
Prevalence of high BMI in 2012 was calculated overall and by gender, race/ethnicity, and age category (8–11 and 12–17 years, similar to those used for NHANES2). Logistic regression was used to examine differences in prevalence by these variables, adjusting for gender, race/ethnicity, and age, except in stratified models.
To examine trends by race/ethnicity, gender- and race-specific prevalence is presented by BMI cut-point for each year from 2003 to 2012. To test for trends by race/ethnicity across these years, gender- and race/ethnicity-specific logistic regression models were used in which the dependent variable was a binary indicator for high BMI and the independent variable of interest was ordinal year. Models adjusted for age and used robust SEs to account for clustering by school district and clustering nested within district (e.g., within schools and students).
To determine if the trends in prevalence of high BMI differed significantly by race/ethnicity, gender-specific logistic regression models were used that adjusted for race/ethnicity and included interaction terms for race/ethnicity and ordinal year. Analyses were conducted in 2015 using Stata IC, version 11.2.
Results
Of the 11,624,865 student records, 49.1% were Hispanic, 30.0% non-Hispanic white, 12.7% Asian, 7.4% African American, and 0.8% American Indian; 49% were female and 51% male; and 67% were aged 12–17 and 33% aged 8–11 years. Compared with the analytic sample, observations excluded because of missing or invalid data were more like to be African American (9.2% vs 7.3%) and American Indian (1.0% vs 0.8%) and less likely to be Asian (8.9% vs 12.5%).
In 2012, 38.1% of California public school students were overweight or obese (BMI ≥85th percentile), 19.9% were obese (BMI ≥95th percentile), and 13.4% had a BMI ≥97th percentile (Table 1). Boys had a higher prevalence than girls, and students aged 8–11 years had a higher prevalence than those aged 12–17 years for all BMI cut-points (p-values<0.001).
Table 1.
Prevalence of High BMI Among California Fifth, Seventh, and Ninth Graders in 2012
| All | NH white | African American |
Hispanic | Asian | American Indian |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % (SE) |
N | % (SE) |
N | % (SE) | N | % (SE) |
N | % (SE) |
N | % (SE) | |
| BMI≥97th %tile | ||||||||||||
| Both genders | ||||||||||||
| 8–17 | 1,271,955 | 13.4b | 341,154 | 7.5b | 84,541 | 14.3 (0.1) | 679,371 | 17.7b | 157,414 | 7.3a | 9,475 | 15.6 (0.4) |
| 8–11 | 413,463 | 15.2a | 108,665 | 7.9a | 26,828 | 15.5 (0.2) | 224,916 | 20.2a | 50,335 | 8.4 (0.1) | 2,719 | 17.2 (0.7) |
| 12–17 | 858,492 | 12.6b | 232,489 | 7.3a | 57,713 | 13.8 (0.1) | 454,455 | 16.4a | 107,079 | 6.8a | 6,756 | 15.0 (0.4) |
| Boys’ age | ||||||||||||
| 8–17 | 648,869 | 15.5b | 175,655 | 8.8a | 42,761 | 13.1 (0.2) | 344,703 | 20.6a | 80,979 | 9.7 (0.1) | 4,771 | 17.4 (0.5) |
| 8–11 | 209,924 | 17.5a | 55,805 | 9.1 (0.1) | 13,502 | 14.7 (0.3) | 113,477 | 23.4 (0.1) | 25,772 | 11.2 (0.2) | 1,368 | 19.2 (1.1) |
| 12–17 | 438,945 | 14.6a | 119,850 | 8.7a | 29,259 | 12.3 (0.2) | 231,226 | 19.2a | 55,207 | 9.0 (0.1) | 3,403 | 16.7 (0.6) |
| Girls’ age | ||||||||||||
| 8–17 | 623,086 | 11.3b | 165,499 | 6.1a | 41,780 | 15.6 (0.2) | 334,668 | 14.7a | 76,435 | 4.7a | 4,704 | 13.8 (0.5) |
| 8–11 | 203,539 | 12.8a | 52,860 | 6.5 (0.1) | 13,326 | 16.4 (0.3) | 111,439 | 17.0 (0.1) | 24,563 | 5.4 (0.1) | 1,351 | 15.2 (1.0) |
| 12–17 | 419,547 | 10.5b | 112,639 | 5.9a | 28,454 | 15.2 (0.2) | 223,229 | 13.6a | 51,872 | 4.4a | 3,353 | 13.2 (0.6) |
| BMI≥95th %tile | ||||||||||||
| Both genders | ||||||||||||
| 8–17 | 1,271,955 | 19.9b | 341,154 | 12.1a | 84,541 | 20.5 (0.1) | 679,371 | 25.6a | 157,414 | 11.8a | 9,475 | 22.8 (0.4) |
| 8–11 | 413,463 | 22.5a | 108,665 | 12.9(0.1) | 26,828 | 22.0 (0.3) | 224,916 | 29.0a | 50,335 | 13.9 (0.2) | 2,719 | 25.6 (0.8) |
| 12–17 | 858,492 | 18.7b | 232,489 | 11.7a | 57,713 | 19.8 (0.2) | 454,455 | 24.0a | 107,079 | 10.8a | 6,756 | 21.6 (0.5) |
| Boys’ age | ||||||||||||
| 8–17 | 648,869 | 22.4a | 175,655 | 13.8a | 42,761 | 18.6 (0.2) | 344,703 | 28.9a | 80,979 | 15.3 (0.1) | 4,771 | 24.5 (0.6) |
| 8–11 | 209,924 | 25.4a | 55,805 | 14.8 (0.2) | 13,502 | 20.8 (0.3) | 113,477 | 32.8 (0.1) | 25,772 | 18.2 (0.2) | 1,368 | 29.2 (1.2) |
| 12–17 | 438,945 | 21.0a | 119,850 | 13.4a | 29,259 | 17.6 (0.2) | 231,226 | 27.0a | 55,207 | 13.9 (0.1) | 3,403 | 22.6 (0.7) |
| Girls’ age | ||||||||||||
| 8–17 | 623,086 | 17.4b | 165,499 | 10.2a | 41,780 | 22.5 (0.2) | 334,668 | 22.3a | 76,435 | 8.2a | 4,704 | 21.0 (0.6) |
| 8–11 | 203,539 | 19.4a | 52,860 | 10.9 (0.1) | 13,326 | 23.3 (0.4) | 111,439 | 25.2 (0.1) | 24,563 | 9.4 (0.2) | 1,351 | 22.0 (1.1) |
| 12–17 | 419,547 | 16.4a | 112,639 | 9.9a | 28,454 | 22.1 (0.2) | 223,229 | 20.9a | 51,872 | 7.6 (0.1) | 3,353 | 20.6 (0.7) |
| BMI≥85th %tile | ||||||||||||
| Both genders | ||||||||||||
| 8–17 | 1,271,955 | 38.1b | 341,154 | 27.4a | 84,541 | 39.2 (0.2) | 679,371 | 45.8a | 157,414 | 27.1 (0.1) | 9,475 | 42.0 (0.5) |
| 8–11 | 413,463 | 41.2a | 108,665 | 28.5 (0.1) | 26,828 | 40.7 (0.3) | 224,916 | 49.8 (0.1) | 50,335 | 30.5 (0.2) | 2,719 | 45.2 (1.0) |
| 12–17 | 858,492 | 36.6a | 232,489 | 26.9a | 57,713 | 38.4 (0.2) | 454,455 | 43.9a | 107,079 | 25.5 (0.1) | 6,756 | 40.7 (0.6) |
| Boys’ age | ||||||||||||
| 8–17 | 648,869 | 40.2a | 175,655 | 29.2 (0.1) | 42,761 | 35.4 (0.2) | 344,703 | 48.1a | 80,979 | 32.2 (0.2) | 4,771 | 42.6 (0.7) |
| 8–11 | 209,924 | 44.4 (0.1) | 55,805 | 31.0 (0.2) | 13,502 | 38.3 (0.4) | 113,477 | 53.3 (0.1) | 25,772 | 37.2 (0.3) | 1,368 | 47.8 (1.4) |
| 12–17 | 438,945 | 38.1a | 119,850 | 28.4 (0.1) | 29,259 | 34.0 (0.3) | 231,226 | 45.6 (0.1) | 55,207 | 29.9 (0.2) | 3,403 | 40.5 (0.8) |
| Girls’ age | ||||||||||||
| 8–17 | 623,086 | 36.0a | 165,499 | 25.5 (0.1) | 41,780 | 43.0 (0.2) | 334,6 | 43.4a | 76,435 | 21.7 (0.1) | 4,704 | 41.4 (0.7) |
| 8–11 | 203,539 | 37.9 (0.1) | 52,860 | 25.9 (0.2) | 13,326 | 43.2 (0.4) | 68111,4 | 46.2 (0.1) | 24,563 | 23.3 (0.3) | 1,351 | 42.6 (1.3) |
| 12–17 | 419,547 | 35.0a | 112,639 | 25.4a | 28,454 | 42.9 (0.2) | 39223,229 | 42.1a | 51,872 | 20.9a | 3,353 | 40.9 (0.6) |
SE<0.05%.
SE<0.1%.
NH, non-Hispanic
Among African American, Hispanic, and American Indian girls, the odds of having a high BMI in 2012 were more than twice the odds among non-Hispanic white girls (p-values<0.001), with disparities increasing with severity of high BMI (Table 2). Asian girls had significantly lower odds of high BMI than non-Hispanic white girls for all cut-points. Boys displayed similar patterns of disparities (p-values<0.001), with Hispanic and American Indian boys exhibiting the highest prevalence. In contrast to the girls, Asian boys had significantly higher odds of high BMI than non-Hispanic white boys.
Table 2.
Prevalence ORsa of High BMI Among Minority Youth Compared to White Youth in 2012
| Prevalence OR (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| n | ≥97th percentile of the CDC growth chart |
≥95th percentile of the CDC growth chart |
≥85th percentile of the CDC growth chart |
|||||
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 175,655 | 165,499 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| African American | 42,761 | 41,780 | 1.56 (1.51, 1.61) | 2.83 (2.74, 2.93) | 1.42 (1.38, 1.46) | 2.55 (2.48, 2.62) | 1.33 (1.30, 1.36) | 2.20 (2.16, 2.25) |
| Hispanic | 344,703 | 334,668 | 2.68 (2.63, 2.73) | 2.64 (2.58, 2.70) | 2.53 (2.49, 2.57) | 2.52 (2.47, 2.56) | 2.25 (2.22, 2.27) | 2.24 (2.21, 2.27) |
| Asian | 80,979 | 76,435 | 1.11 (1.08, 1.14) | 0.76 (0.73, 0.79) | 1.12 (1.10, 1.15) | 0.78 (0.76, 0.80) | 1.15 (1.13, 1.17) | 0.81 (0.79, 0.82) |
| American Indian | 4,771 | 4,704 | 2.20 (2.04, 2.37) | 2.46 (2.26, 2.68) | 2.04 (1.90, 2.18) | 2.36 (2.19, 2.53) | 1.81 (1.71, 1.92) | 2.07 (1.95, 2.20) |
Estimated from logistic regression models.
Note: Boldface indicates statistical significance (p<0.05).
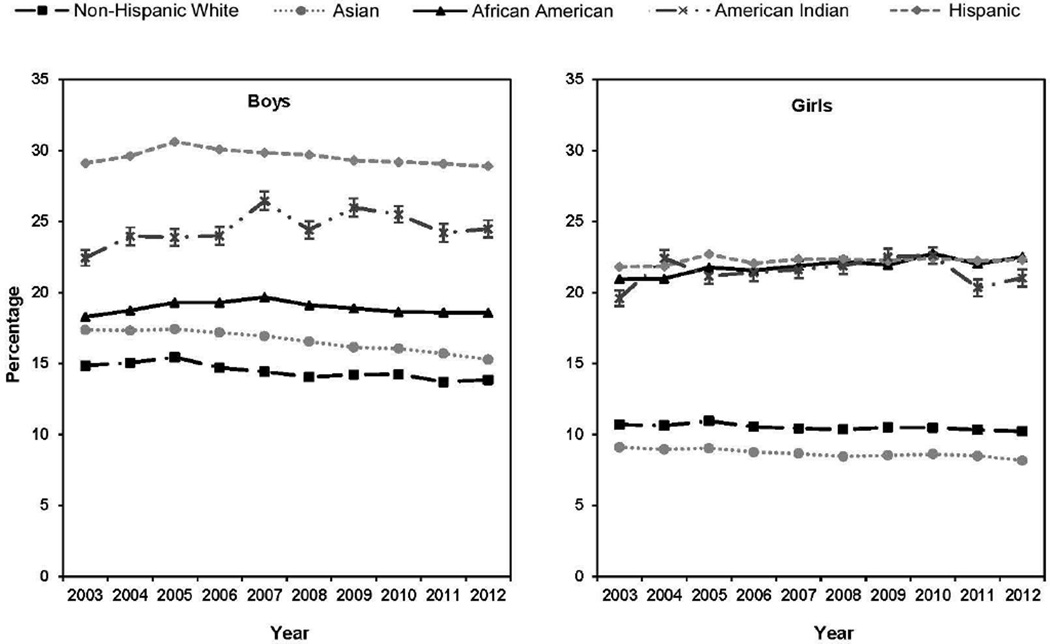
Table 3 presents prevalence of high BMI by gender and race/ethnicity for 2003 to 2012 as well as linear trends in prevalence by race/ethnicity. Among girls, African American girls experienced a trend of increasing prevalence for all BMI cut-points (p-values<0.001), and Hispanic girls had a trend of increasing prevalence for BMI ≥ 95th and 97th percentiles (p-values<0.001). Among American Indian girls, the prevalence of high BMI increased above prevalence in 2003 for all cut-points; however, these trends were not statistically significant. By contrast, Asian girls experienced a trend of decreasing prevalence for all BMI cut-points (p-values<0.05), and non-Hispanic white girls had a trend of decreasing prevalence of BMI ≥85th percentile only (p=0.03). Among boys, only American Indian boys had significant trends of increasing prevalence of high BMI (BMI ≥95th and 97th percentiles, p-values=0.02). By contrast, non-Hispanic white, Hispanic, and Asian boys experienced trends of decreasing prevalence of high BMI for all cut-points (p-values<0.05). Table 3 also includes mean BMI z-scores by gender, race/ethnicity, and year for comparison. Unadjusted trends in prevalence of obesity by race/ethnicity are shown in Figure 1.
Table 3.
Trends in High BMI by Race/Ethnicity Among 11,624,865 California Fifth, Seventh, and Ninth Gradersa
| Linear trendb | Interxn by race |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Directionc |
p-for- trend |
ORd |
p-for- interxn |
| 97th%tile | ||||||||||||||
| NH white | 9.4 | 9.6 | 10.0 | 9.4 | 9.2 | 9.0 | 9.1 | 9.1 | 8.8 | 8.8 | − | <0.001 | ref | ref |
| African American | 12.6 | 13.0 | 13.6 | 13.6 | 13.8 | 13.5 | 13.1 | 13.0 | 12.9 | 13.1 | 0 | 0.70 | 1.01 | <0.001 |
| Hispanic | 20.6 | 21.1 | 21.9 | 21.6 | 21.3 | 21.2 | 20.9 | 20.9 | 20.7 | 20.6 | − | 0.01 | 1.01 | <0.01 |
| Asian | 11.2 | 11.0 | 11.1 | 11.1 | 10.8 | 10.6 | 10.3 | 10.1 | 9.8 | 9.7 | − | <0.001 | 0.99 | 0.04 |
| American Indian | 15.5 | 17.3 | 17.1 | 17.0 | 19.1 | 17.6 | 18.3 | 18.5 | 17.2 | 17.4 | + | 0.02 | 1.03 | <0.001 |
| 95th%tile | ||||||||||||||
| NH white | 14.8 | 15.0 | 15.4 | 14.7 | 14.4 | 14.1 | 14.2 | 14.2 | 13.7 | 13.8 | − | <0.001 | ref | ref |
| African American | 18.3 | 18.7 | 19.3 | 19.3 | 19.7 | 19.1 | 18.9 | 18.6 | 18.6 | 18.6 | 0 | 0.86 | 1.01 | <0.001 |
| Hispanic | 29.1 | 29.6 | 30.6 | 30.1 | 29.8 | 29.7 | 29.3 | 29.2 | 29.1 | 28.9 | − | <0.01 | 1.01 | <0.001 |
| Asian | 17.4 | 17.3 | 17.4 | 17.2 | 16.9 | 16.5 | 16.1 | 16.1 | 15.7 | 15.3 | − | <0.001 | 0.99 | 0.05 |
| American Indian | 22.4 | 24.0 | 23.9 | 24.0 | 26.4 | 24.4 | 26.0 | 25.5 | 24.2 | 24.5 | + | 0.02 | 1.03 | <0.001 |
| 85th%tile | ||||||||||||||
| NH white | 31.6 | 31.7 | 32.1 | 30.9 | 30.5 | 30.0 | 29.9 | 30.0 | 29.2 | 29.2 | − | <0.001 | ref | ref |
| African American | 35.5 | 35.9 | 37.1 | 36.9 | 37.0 | 36.4 | 35.9 | 36.1 | 36.1 | 35.4 | 0 | 0.66 | 1.01 | <0.001 |
| Hispanic | 49.1 | 49.7 | 50.8 | 50.1 | 49.7 | 49.4 | 49.0 | 48.7 | 48.4 | 48.1 | − | <0.001 | 1.01 | <0.001 |
| Asian | 34.7 | 34.5 | 34.9 | 34.5 | 33.8 | 33.8 | 33.0 | 33.4 | 32.5 | 32.2 | − | <0.001 | 1.00 | 0.46 |
| American Indian | 40.3 | 40.9 | 42.4 | 42.5 | 43.0 | 42.0 | 43.7 | 43.3 | 40.7 | 42.6 | 0 | 0.06 | 1.02 | <0.001 |
| Mean BMI z-score | ||||||||||||||
| NH white | 0.46 | 0.46 | 0.47 | 0.44 | 0.42 | 0.41 | 0.41 | 0.41 | 0.38 | 0.37 | ||||
| African American | 0.60 | 0.61 | 0.64 | 0.65 | 0.65 | 0.64 | 0.63 | 0.62 | 0.62 | 0.59 | ||||
| Hispanic | 0.89 | 0.90 | 0.93 | 0.91 | 0.90 | 0.89 | 0.88 | 0.87 | 0.86 | 0.85 | ||||
| Asian | 0.48 | 0.47 | 0.48 | 0.47 | 0.45 | 0.45 | 0.43 | 0.43 | 0.41 | 0.39 | ||||
| American Indian | 0.71 | 0.72 | 0.75 | 0.73 | 0.76 | 0.73 | 0.77 | 0.76 | 0.69 | 0.73 | ||||
| Girls | ||||||||||||||
| 97th%tile | ||||||||||||||
| NH white | 6.4 | 6.4 | 6.6 | 6.3 | 6.3 | 6.3 | 6.4 | 6.3 | 6.2 | 6.1 | 0 | 0.17 | ref | ref |
| African American | 14.3 | 14.2 | 15.0 | 14.7 | 15.0 | 15.3 | 15.0 | 15.8 | 15.1 | 15.6 | + | <0.001 | 1.01 | <0.001 |
| Hispanic | 14.4 | 14.4 | 15.1 | 14.6 | 14.8 | 14.8 | 14.7 | 14.8 | 14.7 | 14.7 | + | <0.001 | 1.01 | <0.01 |
| Asian | 5.4 | 5.3 | 5.4 | 5.2 | 5.1 | 5.0 | 5.0 | 5.1 | 4.9 | 4.7 | − | <0.01 | 0.99 | 0.08 |
| American Indian | 12.7 | 15.4 | 14.7 | 14.5 | 14.5 | 15.2 | 15.0 | 15.2 | 14.6 | 13.8 | 0 | 0.15 | 1.01 | 0.03 |
| 95th%tile | ||||||||||||||
| NH white | 10.7 | 10.6 | 10.9 | 10.5 | 10.4 | 10.4 | 10.5 | 10.5 | 10.3 | 10.2 | 0 | 0.10 | ref | ref |
| African American | 20.9 | 21.0 | 21.8 | 21.6 | 21.9 | 22.2 | 21.9 | 22.7 | 22.0 | 22.5 | + | <0.001 | 1.02 | <0.001 |
| Hispanic | 21.8 | 21.9 | 22.7 | 22.0 | 22.4 | 22.3 | 22.2 | 22.4 | 22.2 | 22.3 | + | <0.001 | 1.01 | <0.01 |
| Asian | 9.1 | 8.9 | 9.0 | 8.8 | 8.7 | 8.5 | 8.5 | 8.6 | 8.5 | 8.2 | − | <0.01 | 0.99 | 0.16 |
| American Indian | 19.6 | 22.4 | 21.2 | 21.4 | 21.6 | 21.9 | 22.5 | 22.6 | 20.3 | 21.0 | 0 | 0.17 | 1.01 | 0.02 |
| 85th%tile | ||||||||||||||
| NH white | 26.5 | 26.4 | 26.7 | 26.0 | 25.7 | 25.8 | 25.9 | 26.0 | 25.5 | 25.5 | − | 0.03 | ref | ref |
| African American | 41.5 | 41.0 | 42.1 | 41.7 | 42.2 | 42.5 | 42.1 | 43.1 | 42.8 | 43.0 | + | <0.001 | 1.01 | <0.001 |
| Hispanic | 43.3 | 43.2 | 44.3 | 43.4 | 43.6 | 43.7 | 43.8 | 43.7 | 43.4 | 43.4 | 0 | 0.07 | 1.01 | <0.01 |
| Asian | 23.0 | 22.9 | 22.8 | 22.8 | 22.1 | 22.2 | 22.4 | 22.5 | 21.9 | 21.7 | − | 0.02 | 1.00 | 0.60 |
| American Indian | 39.4 | 41.4 | 41.1 | 41.5 | 40.6 | 41.7 | 42.3 | 42.0 | 40.8 | 41.4 | 0 | 0.06 | 1.01 | <0.01 |
| Mean BMI z-score | ||||||||||||||
| NH white | 0.37 | 0.36 | 0.38 | 0.35 | 0.34 | 0.34 | 0.35 | 0.35 | 0.33 | 0.33 | ||||
| African American | 0.76 | 0.75 | 0.78 | 0.77 | 0.78 | 0.78 | 0.78 | 0.79 | 0.79 | 0.78 | ||||
| Hispanic | 0.78 | 0.77 | 0.80 | 0.78 | 0.78 | 0.78 | 0.78 | 0.78 | 0.77 | 0.77 | ||||
| Asian | 0.25 | 0.24 | 0.25 | 0.24 | 0.23 | 0.24 | 0.24 | 0.24 | 0.22 | 0.21 | ||||
| American Indian | 0.70 | 0.75 | 0.75 | 0.74 | 0.72 | 0.76 | 0.76 | 0.77 | 0.73 | 0.73 | ||||
Sample included 1,788,324 non-Hispanic white, 431,463 African American, 2,892,175 Hispanic, 759,248 Asian, and 48,828 American Indian male student records and 169,9128 non-Hispanic white, 427,724 African American, 2,813,475 Hispanic, 716,115 Asian, and 48,385 American Indian female student records.
Estimated from race-stratified logistic regression models in which an indicator for high BMI was the dependent variable, and ordinal year was the independent variable. Models adjusted for age and used robust SEs.
Direction indicates increasing prevalence (+) if OR for year >1.00, decreasing prevalence (−) if OR for year <1.00, and no trend (0) if OR was not significant.
Estimated from logistic regression models in which an indicator for high BMI was the dependent variable and year, age, race/ethnicity, and interaction terms (race/ethnicity × year) were the independent variables. OR for interaction term >1.00 indicates a higher slope and <1.00 indicates a lower slope for trend for a racial/ethnic group compared to NH white.
Note: Boldface indicates statistical significance (p<0.05).
NH, Non-Hispanic; intxn, interaction.
Figure 1. BMI≥95th percentile by race/ethnicity from 2003–2012.
Error bars indicate 95% CIs and are visualized only for American Indian youth; all other ethnicities had negligible SE. Includes 11,624,865 student records from fifth, seventh, and ninth grades.
Among girls, the largest relative increases in prevalence (difference in prevalence between 2003 and 2012, divided by 2003 prevalence) were generally observed among African American girls, who experienced a 4%, 8%, and 9% relative increase in prevalence of BMI ≥85th, 95th, and 97th percentiles, respectively. Although trends were not significant among American Indian girls, for all BMI cut-points, the magnitudes of relative increases from 2003 to 2012 (5%, 7%, and 9% for BMI ≥85th, 95th, and 97th percentiles, respectively) were similar to those among African American girls. Among boys, American Indian boys had relative increases in prevalence of BMI ≥95th and 97th percentiles of 9% and 12%, respectively. In both genders, Asian youth had the largest relative decrease in prevalence of high BMI, ranging from −5% to −13%.
Tests for interaction compared linear trends in minority youth with those among non-Hispanic white youth (Table 3). Among girls and boys, African American, Hispanic, and American Indian youth had higher slopes for trends in prevalence of high BMI than non-Hispanic white youth (p-values<0.05) across all cut-points. This indicated that prevalence of high BMI among these groups either decreased more slowly or increased compared with trends among non-Hispanic white youth. Among boys, trends among American Indian boys worsened the most. Trends among Asian youth were not significantly different from those among white youth, except that Asian boys decreased in prevalence of BMI ≥97th percentile more steeply than non-Hispanic white boys (p=0.04).
By 2012, the prevalence of high BMI across all cut-points returned to or fell below 2003 levels for non-Hispanic white youth, Asian youth, and Hispanic boys (Table 3). However, prevalence in 2012 remained higher than in 2003 for American Indian youth, African American girls, and Hispanic girls for all BMI cut-points, as well as for African American boys for two cut-points.
Discussion
Using statewide data from California public schools, prevalence of high BMI in 2012 and racial/ethnic disparities in trends in high BMI from 2003 to 2012 were examined among fifth, seventh, and ninth graders. In 2012, the prevalence of high BMI was markedly higher for African American, Hispanic, and American Indian youth than for non-Hispanic white youth, especially for the highest BMI cut-point. Greater disparities at BMI ≥97th percentile are especially concerning owing to added risks for serious health conditions3–5 associated with severe obesity.6,7 Disparities have widened over the past decade. Compared with non-Hispanic white youth, African American, Hispanic, and American Indian youth showed significantly less favorable trends in prevalence of high BMI from 2003 to 2012, with American Indian boys and African American girls exhibiting the largest relative increases in prevalence.
Consistent with a recent NHANES analysis,25 this study detected increasing prevalence of obesity among Hispanic girls but not among non-Hispanic white girls. In contrast to NHANES,25 increasing prevalence of overweight and obesity was observed among African American girls but not boys, highlighting potential regional differences in gender disparities among African American youth. Importantly, the present study had a large enough sample size to demonstrate that the slopes of the trends among minority youth were significantly higher than among non-Hispanic white youth in California. This addresses a limitation of NHANES—that relatively small sample sizes hinder detection of small differences in obesity trends over time.
This study also addresses the lack of data on trends in American Indian and Asian youth in NHANES. The worsening disparities the authors detected for American Indian youth are troubling, especially for American Indian boys, the only group of boys who continued to increase in prevalence of high BMI through 2012. Other than CDE student records, few data sources exist for studying obesity trends in American Indian school-aged youth. One study, analyzing a smaller sample of school-based height and weight measurements from students in South Dakota, found increasing obesity trends among American Indian youth and decreasing trends among white youth from 1998 to 2010.26 Another study conducted in the Aberdeen Area (Dakotas, Iowa, and Nebraska) measured height and weight of American Indian school-aged children living on eight reservations in 1995–1996 and 2002–2003 and found an increasing prevalence of obesity among these youth.27
Despite troubling signs of increasing disparities by race/ethnicity, in the present study, there were also signs of improvement. Overall, Asian girls and boys had the largest relative reductions in prevalence of high BMI and were the only groups to meet or exceed the Healthy People 2020 goal of a 10% relative reduction in childhood obesity28; in 2003, Asian girls had a 9.1% prevalence of BMI ≥95th percentile, which fell to 8.2% by 2012—a 10% relative reduction, and the prevalence among Asian boys was 17.4% in 2003 and dropped to 15.3%, a 12% relative reduction. Additionally, non-Hispanic white girls decreased in prevalence of overweight (BMI ≥85th percentile), and non-Hispanic white and Hispanic boys decreased in prevalence for all BMI cut-points. Although these data cannot reveal the causes of these positive changes, these changes may reflect progress achieved in California by state and local actions. For instance, California enacted more childhood obesity–related bills than any other state from 2003 to 2009.29,30
Based on this study’s findings of widening disparities over time, there is still a clear need for wide-reaching action to reduce obesity disparities. Although many policy approaches have been recommended to reduce obesity disparities,31 more recently, researchers have begun to quantify and rank these approaches on potential impact and cost effectiveness. In a simulation study, Kristensen et al.32 found that a nationwide excise tax on sugar-sweetened beverages (SSBs) would reduce adolescent obesity the most, while expanded afterschool physical activity would reduce obesity in younger children (aged 6–12 years) the most. These policies would both reduce racial/ethnicity disparities in childhood obesity, with SSB taxes reducing disparities the most.32 In another study, an SSB excise tax was predicted to generate the greatest 10-year savings per dollar spent.33 However, all examined interventions—an SSB tax, eliminating tax subsidies for child-directed TV ads, early care and education policy change, and active physical education— were considerably more cost effective than commonly reimbursed medical treatments for obesity.33
Adoption of these policies can be complemented by culturally tailored and targeted interventions.34–38 Several warrant further study and replication. For example, Bright Start—a school-based intervention for kindergarten and first grade American Indian youth on the Pine Ridge Reservation—targeted family involvement and food and physical activity at school.37 It resulted in a 10% reduction in prevalence of child overweight. Another intervention, which aimed to increase availability and promote purchases of healthy foods in stores on the Navajo Nation, was associated with reduced adult overweight/obesity.39 Although impacts on children were not assessed, it is possible that Navajo children could also have benefitted because adults shape children’s food environments. Although these interventions are promising, what is unclear is if interventions designed for or tested in specific reservations would have similar impacts elsewhere. In contrast to other ethnic groups, Asian and Pacific Islander American youth have been understudied with there being a notable lack of tailored obesity interventions for these groups. This may be because lower prevalence of overweight and obesity has been observed among Asian American youth.12,14 However, compared with Caucasians, Asian children have lower BMIs at a given body fat percentage,40 and adults of Asian and Pacific Islander heritage have a higher risk of Type 2 diabetes at lower BMIs,41 suggesting that Asian and Pacific Islander American youth should not be overlooked in obesity prevention efforts.
Limitations
Although FITNESSGRAM© data provided objective measurements of student BMI from across California, this study was limited by uncertainty about data quality.14 Though districts are supposed to provide training to FITNESSGRAM© coordinators, documentation of school participation in training is not available. Variations in data collection may have resulted in reduced precision. Secondly, studying individuals of different ethnic heritages (e.g., Filipino and Vietnamese) using a single race category (e.g., Asian) may mask variable trends within these groups. Future studies should examine changes in prevalence by specific ethnic heritages. Thirdly, in 2011–2012, the CDE added the race designation of two or more races. Although this applied to only a small fraction of records, estimates from 2011–2012 may be slightly skewed if switching race classifications was associated with differences in adiposity. Also, the lack of an indicator for SES in the CDE data set precludes examining changes in weight status according to student SES; given the strong association between SES and obesity, this study may miss differences in trends by SES, limiting the ability to target interventions to those groups most in need. Lastly, although this sample included a large majority of CDE records (83%), minimizing the impact of missing data, records with missing or invalid data were more likely to be from African American and American Indian youth. This suggests that generalizability to the entire population of African American and American Indian youth in California is more limited than for other groups. Also, because it is possible that children with a higher BMI are less likely to attend school on FITESSGRAM© testing days, prevalence estimates in this study may be lower, particularly for groups with a higher BMI, than if all children in California were measured.
Conclusions
Statewide data from California suggest that racial/ethnic disparities in the prevalence of high BMI among youth have increased over time, with least progress having occurred among American Indian and African American youth and Hispanic girls. These growing disparities provide a compelling rationale for investing in policies and environmental interventions that are likely to reduce obesity among minority youth.
Acknowledgments
This work was supported in part by the following grants: American Heart Association Postdoctoral Fellowship 14POST20140055 (J. Falbe) and NIH/National Heart, Lung, and Blood Institute R01HL120666 (K. Madsen, J. Falbe). The funders had no role in the study.
The views expressed in this paper do not represent the positions of the California Department of Education. No official endorsement by the California Department of Education is intended or should be inferred.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
JF conceptualized and designed the study, carried out the analysis, interpreted the data, drafted the manuscript, revised the manuscript, and approved the final manuscript as submitted. CC contributed to the concept and design, carried out the analysis, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted. JL contributed to the analysis and interpretation, reviewed and revised the manuscript, and approved the final manuscript as submitted. KAM conceptualized and designed the study, supervised the analysis and interpretation, reviewed and revised the manuscript, and approved the final manuscript as submitted.
No financial disclosures were reported by the authors of this paper.
References
- 1.Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000. Int J Obes Relat Metab Disord. 2004;28(1):4–9. doi: 10.1038/sj.ijo.0802421. http://dx.doi.org/10.1038/sj.ijo.0802421. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz MB, Puhl R. Childhood obesity: a societal problem to solve. Obes Rev. 2003;4(1):57–71. doi: 10.1046/j.1467-789x.2003.00093.x. http://dx.doi.org/10.1046/j.1467-789X.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17. e12. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 5.Sutherland ER. Obesity and asthma. Immunol Allergy Clin North Am. 2008;28(3):589–602. doi: 10.1016/j.iac.2008.03.003. ix. http://dx.doi.org/10.1016/j.iac.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 7.Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9(5):322–329. doi: 10.1016/j.acap.2009.04.005. http://dx.doi.org/10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. http://dx.doi.org/10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. http://dx.doi.org/10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 10.U.S. DHHS. Healthy People 2020: Disparities. [Accessed April 3, 2014]; www.healthypeople.gov/2020/about/disparitiesAbout.aspx. Published 2010.
- 11.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in U.S. children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. http://dx.doi.org/10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr. 2011;2(1):23–31. doi: 10.3945/an.110.000083. http://dx.doi.org/10.3945/an.110.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iannotti RJ, Wang J. Trends in physical activity, sedentary behavior, diet, and BMI among U.S. adolescents, 2001–2009. Pediatrics. 2013;132(4):606–614. doi: 10.1542/peds.2013-1488. http://dx.doi.org/10.1542/peds.2013-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madsen KA, Weedn AE, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics. 2010;126(3):434–442. doi: 10.1542/peds.2009-3411. http://dx.doi.org/10.1542/peds.2009-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC. Obesity in K-8 students - New York City, 2006–07 to 2010–11 school years. Morb Mortal Wkly Rep. 2011;60(49):1673–1678. [PubMed] [Google Scholar]
- 16.Oza-Frank R, Hade EM, Norton A, Scarpitti H, Conrey EJ. Trends in body mass index among Ohio's third-grade children: 2004–2005 to 2009–2010. J Acad Nutr Diet. 2013;113(3):440–446. doi: 10.1016/j.jand.2012.11.005. http://dx.doi.org/10.1016/j.jand.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.California Department of Education (CDE) Physical Fitness Testing (PFT) [Accessed August 1, 2014]; www.cde.ca.gov/ta/tg/pf/. Published 2013.
- 18.U.S. Census Buereau. 2011–2013 American Community Survey 3-Year Estimates. [Accessed February 3, 2015];American Fact Finder. http://factfinder.census.gov/
- 19.Georgetown University Health Policy Institute, Center for Children and Families. Federal and State Financing. [Accessed February 23, 2015];Facts and Statistics. http://ccf.georgetown.edu/medicaid-facts-statistics/. Published 2014. [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. http://dx.doi.org/10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 21.The Cooper Institute. FITNESSGRAM©. [Accessed November 1, 2015]; www.cooperinstitute.org/youth/fitnessgram. Published 2014. Updated 2014.
- 22.Morrow JR, Jr, Martin SB, Jackson AW. Reliability and validity of the FITNESSGRAM: quality of teacher-collected health-related fitness surveillance data. Res Q Exerc Sport. 2010;81(3 Suppl):S24–S30. doi: 10.1080/02701367.2010.10599691. http://dx.doi.org/10.1080/02701367.2010.10599691. [DOI] [PubMed] [Google Scholar]
- 23.Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 y) [Accessed January 13, 2014]; www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Published 2014.
- 24.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;(25):1–5. [PubMed] [Google Scholar]
- 25.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014;168(6):561–566. doi: 10.1001/jamapediatrics.2014.21. http://dx.doi.org/10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 26.Hearst MO, Biskeborn K, Christensen M, Cushing C. Trends of overweight and obesity among white and American Indian school children in South Dakota, 1998–2010. Obesity. 2013;21(1):E26–E32. doi: 10.1002/oby.20022. http://dx.doi.org/10.1002/oby.20022. [DOI] [PubMed] [Google Scholar]
- 27.Zephier E, Himes JH, Story M, Zhou X. Increasing prevalences of overweight and obesity in Northern Plains American Indian children. Arch Pediatr Adolesc Med. 2006;160(1):34–39. doi: 10.1001/archpedi.160.1.34. http://dx.doi.org/10.1001/archpedi.160.1.34. [DOI] [PubMed] [Google Scholar]
- 28.U.S. DHHS. Healthy People 2020: Nutrition and Weight Status. [Accessed Novmber, 3, 2015]; www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives. Published 2010.
- 29.Boehmer TK, Luke DA, Haire-Joshu DL, Bates HS, Brownson RC. Preventing childhood obesity through state policy: Predictors of bill enactment. Am J Prev Med. 2008;34(4):333–340. doi: 10.1016/j.amepre.2008.01.003. http://dx.doi.org/10.1016/j.amepre.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Eyler AA, Nguyen L, Kong J, Yan Y, Brownson R. Patterns and predictors of enactment of state childhood obesity legislation in the United States: 2006–2009. Am J Public Health. 2012;102(12):2294–2302. doi: 10.2105/AJPH.2012.300763. http://dx.doi.org/10.2105/AJPH.2012.300763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.IOM. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, D.C.: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 32.Kristensen AH, Flottemesch TJ, Maciosek MV, et al. Reducing childhood obesity through U.S. federal policy: A microsimulation analysis. Am J Prev Med. 2014;47(5):604–612. doi: 10.1016/j.amepre.2014.07.011. http://dx.doi.org/10.1016/j.amepre.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gortmaker SL, Long MW, Resch SC, et al. Cost effectiveness of childhood obesity interventions: Evidence and methods for CHOICES. Am J Prev Med. 2015;49(1):102–111. doi: 10.1016/j.amepre.2015.03.032. http://dx.doi.org/10.1016/j.amepre.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164(11):995–1004. doi: 10.1001/archpediatrics.2010.197. http://dx.doi.org/10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falbe J, Cadiz AA, Tantoco NK, Thompson HR, Madsen KA. Active and Healthy Families: A randomized controlled trial of a culturally-tailored obesity intervention for Latino children. Acad Pediatr. 2015;15(4):386–395. doi: 10.1016/j.acap.2015.02.004. http://dx.doi.org/10.1016/j.acap.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 36.Caballero B, Clay T, Davis SM, et al. Pathways: A school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–1038. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Story M, Hannan PJ, Fulkerson JA, et al. Bright Start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity. 2012;20(11):2241–2249. doi: 10.1038/oby.2012.89. http://dx.doi.org/10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gatto NM, Ventura EE, Cook LT, Gyllenhammer LE, Davis JN. LA Sprouts: a garden-based nutrition intervention pilot program influences motivation and preferences for fruits and vegetables in Latino youth. J Acad Nutr Diet. 2012;112(6):913–920. doi: 10.1016/j.jand.2012.01.014. http://dx.doi.org/10.1016/j.jand.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 39.Gittelsohn J, Kim EM, He S, Pardilla M. A food store-based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo nation. J Nutr. 2013;143(9):1494–1500. doi: 10.3945/jn.112.165266. http://dx.doi.org/10.3945/jn.112.165266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu A, Byrne NM, Kagawa M, et al. Ethnic differences in the relationship between body mass index and percentage body fat among Asian children from different backgrounds. Br J Nutr. 2011;106(9):1390–1397. doi: 10.1017/S0007114511001681. http://dx.doi.org/10.1017/S0007114511001681. [DOI] [PubMed] [Google Scholar]
- 41.Jih J, Mukherjea A, Vittinghoff E, et al. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev Med. 2014;65:1–6. doi: 10.1016/j.ypmed.2014.04.010. http://dx.doi.org/10.1016/j.ypmed.2014.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]