Abstract
Introduction
Recurrent joint hemarthroses due to hemophilia (Factor VIII and Factor IX deficiency) often lead to invasive orthopedic interventions to decrease frequency of bleeding and/or to alleviate pain associated with end-stage hemophilic arthropathy.
Aim
Identify trends in invasive orthopedic interventions among people with hemophilia who were enrolled in the Universal Data Collection (UDC) program during the period 2000–2010.
Methods
Data were collected from 130 hemophilia treatment centers in the United States annually during the period 2000–2010, in collaboration with the Centers for Disease Control and Prevention (CDC). The number of visits in which an invasive orthopedic intervention was reported was expressed as a proportion of the total visits in each year of the program. Invasive orthopedic interventions consisted of arthroplasty, arthrodesis, and synovectomy. Joints included in this study were the shoulder, elbow, hip, knee, and ankle.
Results
A 5.6% decrease in all invasive orthopedic interventions in all joints of people with hemophilia enrolled in the UDC program over the 11-year study period was observed.
Conclusions
These data reflect a declining trend in invasive orthopedic interventions in people with hemophilia. Further research is needed to understand the characteristics that may influence invasive orthopedic interventions.
Keywords: arthropathy, arthroplasty, hemophilia, orthopedic
Introduction
Hemarthrosis is a common clinical manifestation of hemophilia (Factor VIII or FIX deficiency). Recurrent hemarthrosis can cause chronic joint disease resulting in pain, decreased range of motion, and decreased ability to participate in activities, all of which affect quality of life [1,2]. Orthopedic interventions often are used to decrease pain, decrease bleeding episodes, and maintain or improve quality of life for individuals with severe hemophilic joint disease [3].
The Universal Data Collection (UDC) program [2], in collaboration with federally supported hemophilia treatment centers (HTCs) across the United States, included data from people with bleeding disorders who have undergone an invasive orthopedic intervention. End-stage invasive orthopedic interventions such as arthroplasty and arthrodesis are performed primarily to alleviate pain [4,5]. Non-end-stage invasive orthopedic interventions in hemophilia are performed to disrupt the cycle of recurrent hemarthroses, delay end-stage arthropathy, relieve pain and preserve joint structure [6–8]. Non end-stage invasive interventions may include but are not limited to synovectomy, labral repairs, meniscal repairs and allografts.
The purpose of this study is to report trends in the occurrence of invasive orthopedic interventions, such as arthrodesis, arthroplasty, and synovectomy, among the population with hemophilia A or B, who were enrolled in the UDC program from 2000 to 2010. We hypothesized that there would be a decreasing trend in orthopedic interventions for end-stage arthropathy and an increase in non-end stage arthropathy procedures.
Methods
Data were collected from patients at approximately 130 U.S. HTCs annually during the period 1998–2011 under the UDC program, in collaboration with the Centers for Disease Control and Prevention (CDC). Approximately 24,000 or 80% of individuals with a bleeding disorder seen at an HTC have enrolled in the UDC program from 1998 until September 2011 [2,9]. With input and assistance from hematologists, physical therapists, nurses, other providers of hemophilia care and people with bleeding disorders, the UDC program was developed as a standardized data collection tool for the surveillance of people with bleeding disorders. Participation was voluntary and required informed consent from participants (or parents of minors). Each participating HTC and the CDC provided institutional review board approval. HTC medical providers collected data on demographic characteristics and clinical characteristics on an annual basis. Historic information was collected on an initial registration form for each participant. Data collected represented a mix of self-reports and medical chart abstraction.
Study population
Inclusion and exclusion
Universal Data Collection program participants with a diagnosis of hemophilia A or B, over the age of 2 years who completed at least one UDC visit during the years 2000–2010 were eligible for inclusion in this study. Eligible UDC program participants with incomplete or missing information on variables of interest were excluded from the analysis. Variables of interest were type of invasive orthopedic intervention (arthroplasty, arthrodesis, synovectomy and ‘other’), presence of inhibitor, type of factor replacement, diagnosis, and age. Severity of hemophilia classification is based on plasma levels of Factor VIII or IX activity. Factor levels < 1% are classified as severe, between 1% and 5% is moderate and >5% and <40% of normal is mild [10].
Outcome measures
The outcomes of interest for our study were the proportions of individuals with hemophilia who reported invasive orthopedic interventions for each year of the study. To maintain consistency, proportions were reported for sub-groups as well. However, in a few instances where very small proportions were encountered, they were expressed as a percent. The UDC program data consists of invasive orthopedic interventions on 10 joints: bilateral shoulders, elbows, hips, knees, and ankles. In the UDC program all orthopedic interventions were recorded in one of the following categories: arthrodesis, arthroplasty, synovectomy, and ‘other’. The ‘other’ category represented a nonspecific group of orthopedic interventions that could not be categorized under one of the first three categories. Arthrodesis and arthroplasty procedures were counted once per joint, per side, per subject while synovectomies and ‘other’ procedures were not limited in number per side or per joint. In the hemophilia population, synovectomies are typically performed to decrease pain and recurrence of bleeding; therefore multiple procedures of this type could have been performed in a year. The non-specific ‘other’ procedures may also be recorded multiple times within a year in the same joint due to trauma or revision/complication of an orthopedic procedure.
For a few participants who reported arthrodesis and arthroplasty procedures more than once per joint per side, only the first report of their orthopedic intervention was counted. Since both arthrodesis and arthroplasty procedures are interventions for end-stage joint disease and typically do not occur repeatedly in the same joint, unless there are significant complications, we discounted the repeat reports of either procedure on the same side of the same joint. Therefore, this analysis does not include any repeated procedures that are indicative of complications. Synovectomy in the UDC program was differentiated into groupings of arthroscopic, open, or radioisotopic.
The calculated proportions were plotted as line graphs to show any trends over the 11-year period. Overall proportions, as well as stratifications by various characteristics of interest such as diagnosis (hemophilia A or B), severity, age, factor replacement method, and inhibitor presence, were calculated and plotted. Proportions for each year was determined by counting all participants who reported an invasive orthopedic intervention during a UDC visit divided by the total number of eligible participants with a UDC program visit on record for that year.
For analysis and plotting purposes in this study, age was categorized into four groups: 2–20 years of age, 20–39 years of age, 40–59 years of age, and 60 years of age or older. Age groups were chosen in 20-year intervals for people up to 59 years of age. All participants 60 years of age or older were grouped together, as there were relatively few people in this oldest age group.
Approximately 15–30% of patients with FVIII deficiency and 2–5% of patients with FIX deficiency develop an inhibitor, an alloimmune neutralizing antibody [11]. Inhibitor status or presence for each study year was defined as positive if the recorded inhibitor titer in that year was >1 Bethesda unit or if the person was receiving immune tolerance therapy. Because inhibitor titer can change from one year to another [12], and taking a conservative approach, for this study’s purposes, a person was categorized as inhibitor positive if she or he was positive for the presence of an inhibitor in the year prior to and the year of an invasive orthopedic intervention. Negative inhibitor status was defined as not having a recorded inhibitor in the year prior to and the year of an orthopedic intervention.
The UDC program defines continuous prophylaxis therapy as a person receiving treatment product on a regular schedule to prevent any and all bleeding with the expectation to continue indefinitely. Continuous prophylaxis status for this study was defined as positive when an individual was recorded in the UDC program as being on continuous prophylaxis for both the year prior to and the year of the orthopedic intervention. On demand or intermittent prophylaxis were coded as negative for prophylaxis in our study.
Statistical analysis
The proportion of individuals with hemophilia reporting an invasive orthopedic intervention in a given year was calculated by dividing total number of participants with hemophilia who reported an invasive orthopedic intervention by the total number of individuals with hemophilia who had a UDC visit that year. The calculated proportions were plotted and significant trends (P < 0.05) were identified using Cochran–Armitage trend test. The output for this paper was generated using SAS software (SAS Institute Inc., Cary, NC, USA) [13].
Results
A total of 66,284 annual study visits of individuals with hemophilia participated in the UDC program from 2000 to 2010. Of these individuals 78.9% were diagnosed with hemophilia A and 21.1% with hemophilia B. Close to half (49.6%) of participants had severe hemophilia, 31.5% had moderate hemophilia, 18.8% had mild hemophilia and 0.1% had an unknown severity level of hemophilia during the study. Table 1 includes select demographic and clinical characteristics of the UDC participants who completed an annual UDC visit by year of the visit.
Table 1.
Descriptive statistics of select demographic and clinical characteristics of the UDC participants, who completed an annual UDC visit, by the year of the visit.
| Year of the HTC visit
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
| Age group | |||||||||||
| <20 years | 2722 (58.8) | 2944 (60.3) | 3225 (59.7) | 3348 (59.3) | 3513 (58.3) | 3675 (57.9) | 3778 (57.1) | 3857 (57.2) | 3698 (56.2) | 3755 (54.8) | 3499 (53.3) |
| 20–39 years | 1122 (24.2) | 1113 (22.8) | 1251 (23.2) | 1362 (24.1) | 1460 (24.2) | 1544 (24.3) | 1630 (24.6) | 1689 (25.1) | 1680 (25.5) | 1818 (26.6) | 1794 (27.3) |
| 40–59 years | 648 (14.0) | 679 (13.9) | 749 (13.9) | 756 (13.4) | 856 (14.2) | 896 (14.1) | 952 (14.4) | 926 (13.7) | 922 (14.0) | 968 (14.1) | 947 (14.4) |
| 60 years or older | 141 (3.0) | 149 (3.1) | 173 (3.2) | 182 (3.2) | 197 (3.3) | 230 (3.6) | 257 (3.9) | 266 (4.0) | 284 (4.3) | 306 (4.5) | 323 (4.9) |
| Race | |||||||||||
| White (non-Hispanic) | 3302 (71.3) | 3461 (70.9) | 3828 (70.9) | 3902 (69.1) | 4113 (68.3) | 4309 (67.9) | 4539 (68.6) | 4542 (67.4) | 4458 (67.7) | 4636 (67.7) | 4418 (67.3) |
| White (Hispanic) | 434 (9.4) | 541 (11.1) | 607 (11.2) | 690 (12.2) | 735 (12.2) | 800 (12.6) | 776 (11.7) | 818 (12.1) | 864 (13.1) | 859 (12.6) | 823 (12.5) |
| Black (non-Hispanic) | 581 (12.5) | 570 (11.7) | 667 (12.4) | 664 (11.8) | 737 (12.2) | 767 (12.1) | 806 (12.2) | 821 (12.2) | 784 (11.9) | 803 (11.7) | 767 (11.7) |
| Black (Hispanic) | 25 (0.5) | 21 (0.4) | 33 (0.6) | 41 (0.7) | 31 (0.5) | 40 (0.6) | 38 (0.6) | 34 (0.5) | 36 (0.6) | 34 (0.5) | 36 (0.6) |
| Asian/Pacific islander | 122 (2.6) | 126 (2.6) | 95 (1.8) | 159 (2.8) | 159 (2.6) | 170 (2.7) | 170 (2.6) | 215 (3.2) | 187 (2.8) | 195 (2.9) | 191 (2.9) |
| Native American | 38 (0.8) | 41 (0.8) | 37 (0.7) | 40 (0.7) | 66 (1.1) | 60 (1) | 72 (1.1) | 61 (0.9) | 61 (0.9) | 66 (1) | 62 (0.9) |
| Diagnosis | |||||||||||
| Hemophilia-A | 3686 (79.6) | 3851 (78.8) | 4245 (78.6) | 4432 (78.5) | 4787 (79.4) | 5010 (79.0) | 5173 (78.2) | 5340 (79.3) | 5181 (78.7) | 5370 (78.4) | 5207 (79.3) |
| Hemophilia-B | 947 (20.4) | 1034 (21.2) | 1153 (21.4) | 1216 (21.5) | 1239 (20.6) | 1335 (21.0) | 1444 (21.8) | 1398 (20.7) | 1403 (21.3) | 1477 (21.6) | 1356 (20.7) |
| Hemophilia severity | |||||||||||
| Mild | 909 (19.6) | 1047 (21.4) | 1166 (21.6) | 1213 (21.5) | 1227 (20.4) | 1359 (21.4) | 1371 (20.7) | 1453 (21.6) | 1377 (20.9) | 1480 (21.6) | 1438 (21.9) |
| Moderate | 1012 (21.8) | 1081 (22.1) | 1161 (21.5) | 1299 (23.0) | 1373 (22.8) | 1450 (22.9) | 1524 (23.0) | 1540 (22.9) | 1526 (23.2) | 1620 (23.7) | 1491 (22.7) |
| Severe | 2709 (58.5) | 2755 (56.4) | 3067 (56.8) | 3130 (55.4) | 3419 (56.7) | 3525 (55.6) | 3712 (56.1) | 3739 (55.5) | 3673 (55.8) | 3740 (54.6) | 3623 (55.2) |
| Unknown | 3 (0.1) | 2 (0.1) | 4 (0.1) | 6 (0.1) | 7 (0.1) | 11 (0.2) | 10 (0.2) | 6 (0.1) | 8 (0.1) | 7 (0.1) | 11 (0.2) |
Enrollees reported a total of 2582 invasive orthopedic interventions over the entire study period. Table 2 represents the distribution of invasive orthopedic interventions reported over the study period. We found the knee joint had the largest proportion of invasive orthopedic interventions with 1172 (45.4%) of all orthopedic interventions, followed by the ankle (658, 25.5%), elbow (497, 19.2%), hip (169, 6.5%), and shoulder (86, 3.3%). Overall the most commonly reported invasive orthopedic interventions were synovectomies (1180, 45.7%), followed by arthroplasties (669, 25.9%), ‘other’ invasive orthopedic interventions (556, 23.5%), and arthrodesis (177, 6.9%).
Table 2.
Distribution of invasive orthopedic interventions reported by the study participants over the study period.
| Arthrodesis | Arthroplasty | All synovectomies | Other invasive interventions | Total | Synovectomies by subtypes
|
|||
|---|---|---|---|---|---|---|---|---|
| Arthroscopic synovectomy | Radioisotopic synovectomy | Open synovectomy | ||||||
| Hip | 3 | 124 | 3 | 39 | 169 | 2 | 0 | 1 |
| Procedure percentage | 1.8 | 73.4 | 1.8 | 23.1 | 66.7 | 0.0 | 33.3 | |
| Joint percentage | 1.7 | 18.5 | 0.3 | 7 | 0.4 | 0.0 | 0.4 | |
| Knee | 38 | 473 | 454 | 207 | 1172 | 237 | 108 | 109 |
| Procedure percentage | 3.2 | 40.4 | 38.7 | 17.7 | 52.2 | 23.8 | 24.0 | |
| Joint percentage | 21.5 | 70.7 | 38.5 | 37.2 | 42.3 | 29.3 | 43.3 | |
| Ankle | 126 | 20 | 355 | 157 | 658 | 186 | 110 | 59 |
| Procedure percentage | 19.1 | 3.0 | 54.0 | 23.9 | 52.4 | 31.0 | 16.6 | |
| Joint percentage | 71.2 | 3.0 | 30.1 | 28.2 | 33.2 | 29.9 | 23.4 | |
| Shoulder | 2 | 17 | 25 | 42 | 86 | 13 | 6 | 6 |
| Procedure percentage | 2.3 | 19.8 | 29.1 | 48.8 | 52.0 | 24.0 | 24.0 | |
| Joint percentage | 1.1 | 2.5 | 2.1 | 7.6 | 2.3 | 1.6 | 2.4 | |
| Elbow | 8 | 35 | 343 | 111 | 497 | 122 | 144 | 77 |
| Procedure percentage | 1.6 | 7.0 | 69.0 | 22.3 | 35.6 | 42.0 | 22.4 | |
| Joint percentage | 4.5 | 5.2 | 29.1 | 20.0 | 21.8 | 39.1 | 30.6 | |
| Total | 177 | 669 | 1180 | 556 | 2582 | 560 | 368 | 252 |
Row percentage, proportion of specific invasive orthopedic intervention (IOI) per joint; Column percentage, proportion of a joint relative to the IOI. Other, represents a non-specific group of invasive orthopedic interventions that could not be categorized as arthrodesis, arthroplasty or synovectomy.
We found arthroplasty was the most frequent invasive orthopedic intervention reported on the hip (124, 73.4%) and knee joint (473, 40.4%), accounting for about three-quarters of all orthopedic interventions reported. Synovectomy (all three types combined) was the most frequently reported invasive orthopedic intervention on the ankle joint (355, 54.0%). In the upper extremity, synovectomy was the most frequently reported invasive orthopedic intervention on the elbow joint (343, 69.0%), whereas procedures categorized as ‘other’ were the most commonly reported orthopedic interventions on the shoulder joint (Table 2).
Invasive orthopedic interventions trends 2000–2010
The UDC program data reflects a 5.6% declining trend in all invasive orthopedic interventions for all joints during 2000–2010 (Fig. 1). In the year 2000, 7.2% of the enrollees reported undergoing an orthopedic intervention during the year prior to 2000; whereas in the last year of the study (2010), only 1.7% reported undergoing an invasive orthopedic intervention during the previous year. This trend is statistically significant (P < 0.01).
Fig. 1.
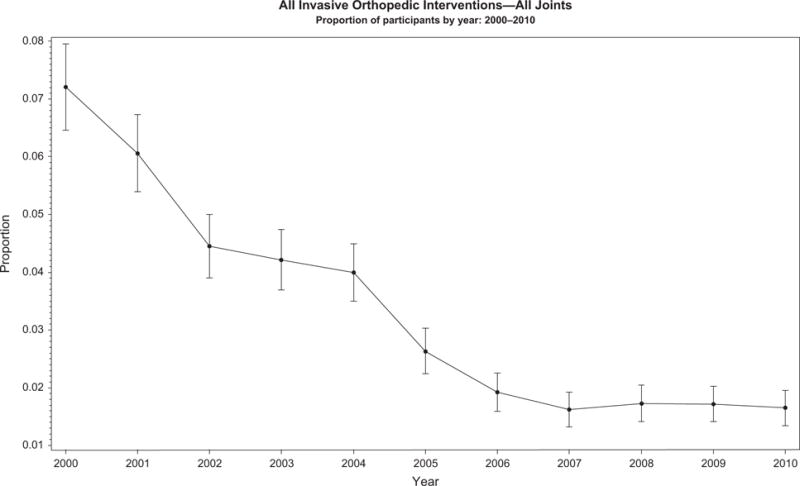
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) summed over all joints. Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
To explore whether or not the observed overall declining trend in the use of invasive orthopedic interventions was consistent across strata of characteristics that could influence use of orthopedic interventions, separate graphs that displayed trends by various variables of interest (diagnosis, age, inhibitor status, prophylaxis status) were produced. The proportions of orthopedic interventions at the start of the study (2000) and at the end (2010), along with the statistical significance (P-value) of the Cochran–Armitage, trend test, for various characteristics of interest (type of orthopedic intervention, joint diagnosis, age, inhibitor status and prophylaxis status), are summarized in Table 3. All trend tests revealed a statistically significant decline over the decade. All strata showed strong significance with all P-values <0.01.
Table 3.
Proportion of Universal Data Collection program enrollees reporting an invasive orthopedic intervention (IOI) in the starting and ending years of the study, along with the statistical significance of the trend test.
| Percentage of IOI in 2000 | Percentage of IOI in 2010 | Minimum percentage value (Year) | P-value* | |
|---|---|---|---|---|
| All IOIs combined, all joints | 7.21 | 1.65 | 1.62 (2007) | <0.01 |
| Individual IOIs, all joints | ||||
| Arthrodesis | 0.71 | 0.15 | 0.06 (2008) | <0.01 |
| Arthroplasty | 1.96 | 0.55 | 0.52 (2007) | <0.01 |
| Synovectomy | ||||
| Arthroscopic | 1.79 | 0.44 | 0.38 (2006) | <0.01 |
| Open | 1.10 | 0.15 | 0.13 (2007) | <0.01 |
| Radioscopic | 1.01 | 0.18 | 0.15 (2006) | <0.01 |
| Other IOIs | 1.86 | 0.29 | 0.29 (2010) | <0.01 |
| Individual joints, all IOIs | ||||
| Hip | 0.50 | 0.14 | 0.07 (2009) | <0.01 |
| Knee | 4.53 | 0.76 | 0.76 (2010) | <0.01 |
| Ankle | 2.24 | 0.52 | 0.38 (2009) | <0.01 |
| Shoulder | 0.17 | 0.06 | 0.03 (2007) | <0.01 |
| Elbow | 1.36 | 0.38 | 0.35 (2009) | <0.01 |
| Diagnosis | ||||
| Hemophilia A | 7.57 | 1.75 | 1.65 (2007) | <0.01 |
| Hemophilia B | 5.81 | 1.25 | 1.25 (2010) | <0.01 |
| Hemophilia severity | ||||
| Mild | 3.19 | 0.76 | 0.54 (2009) | <0.01 |
| Moderate | 5.34 | 1.41 | 1.36 (2009) | <0.01 |
| Severe | 9.27 | 2.10 | 2.03 (2007) | <0.01 |
| Age in years | ||||
| <20 | 3.86 | 0.71 | 0.56 (2009) | <0.01 |
| 20–39 | 11.23 | 2.56 | 2.32 (2008) | <0.01 |
| 40–59 | 14.04 | 3.06 | 2.81 (2007) | <0.01 |
| ≥60 | 8.51 | 2.48 | 1.63 (2009) | <0.01 |
| Inhibitor status | ||||
| Positive | 8.06 | 1.00 | 1.00 (2010) | <0.01 |
| Negative | 7.16 | 1.68 | 1.64 (2007) | <0.01 |
| Prophylaxis status | ||||
| Continuous prophylaxis | 4.61 | 1.57 | 0.12 (2007) | <0.01 |
| Intermittent or on demand | 12.06 | 2.29 | 2.24 (2008) | <0.01 |
Cochran–Armitage Trend Test.
IOI, invasive orthopedic intervention, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Invasive orthopedic interventions by diagnosis
The data show an overall decreasing trend in the reported number of invasive orthopedic interventions for participants regardless of the type or severity of hemophilia. Throughout the 11-year study period the proportion of enrollees with hemophilia A was approximately 80% and hemophilia B was 20%. During the study period, both groups of people with hemophilia A or B showed a decrease in invasive orthopedic interventions by 5.8% and 4.6% respectively (Fig. 2). With the exception of 2003, people with mild hemophilia consistently reported fewer orthopedic interventions than people with moderate hemophilia who in turn showed consistently fewer orthopedic interventions than people with a severe form of the disorder (Fig. 3). The percentages reported in the year 2000 and in the year 2010 represent a 2.4%, 3.9% and 7.2% reduction of invasive orthopedic interventions for people with mild, moderate and severe hemophilia respectively. These trends are statistically significant (P < 0.01).
Fig. 2.
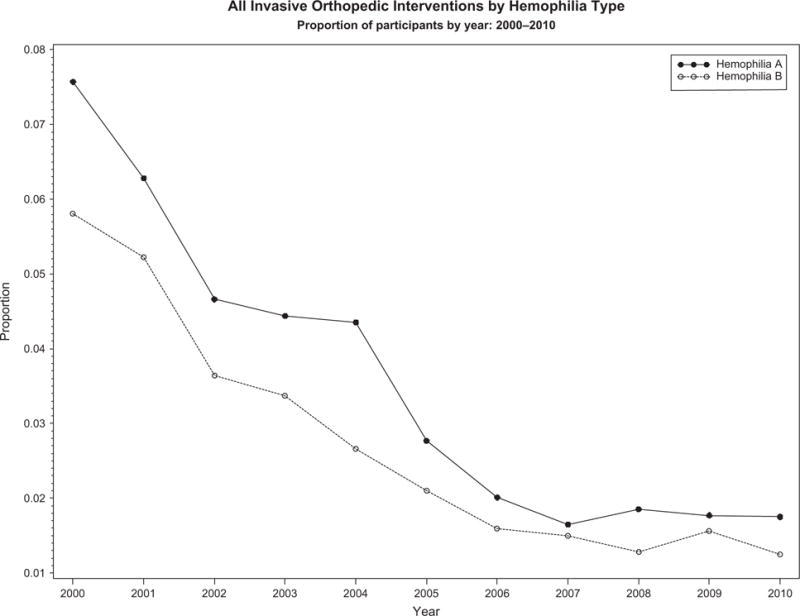
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) by diagnosis. Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Fig. 3.
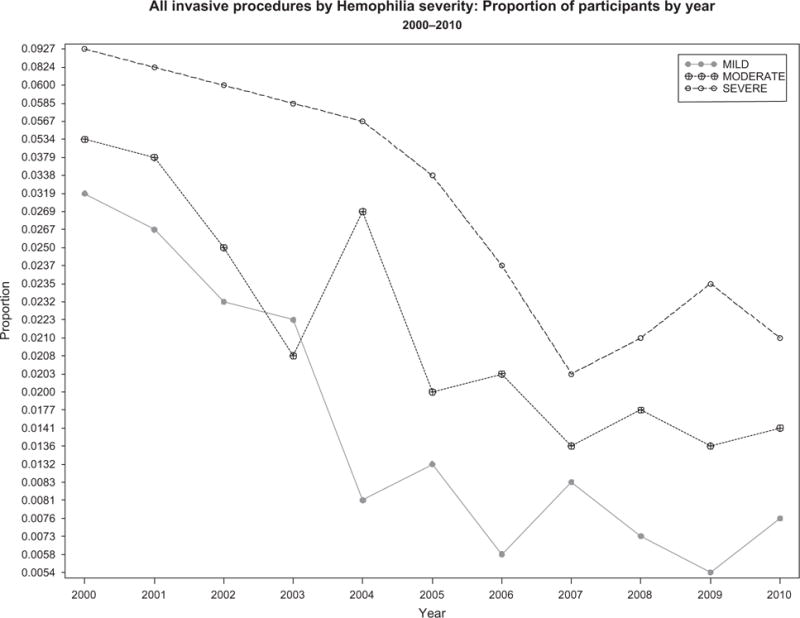
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) by hemophilia severity. Figure excludes 75 individuals whose severity was unknown. Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Invasive orthopedic interventions by age group
A decreasing trend in all invasive orthopedic interventions was observed among all age groups (Fig. 4). As expected, considerable variation was seen in reported proportions of orthopedic interventions across all age groups. Larger differences in reported proportions of orthopedic interventions were observed between people in different age groups in 2000 than at the end of the study period in 2010. The greatest change (8.7%) was observed among the 20–39 years-of-age group, in which the proportion of invasive orthopedic interventions dropped from 11.2% in 2000 to 2.6% in 2010. A significant change (P < 0.01) was observed among all age strata.
Fig. 4.
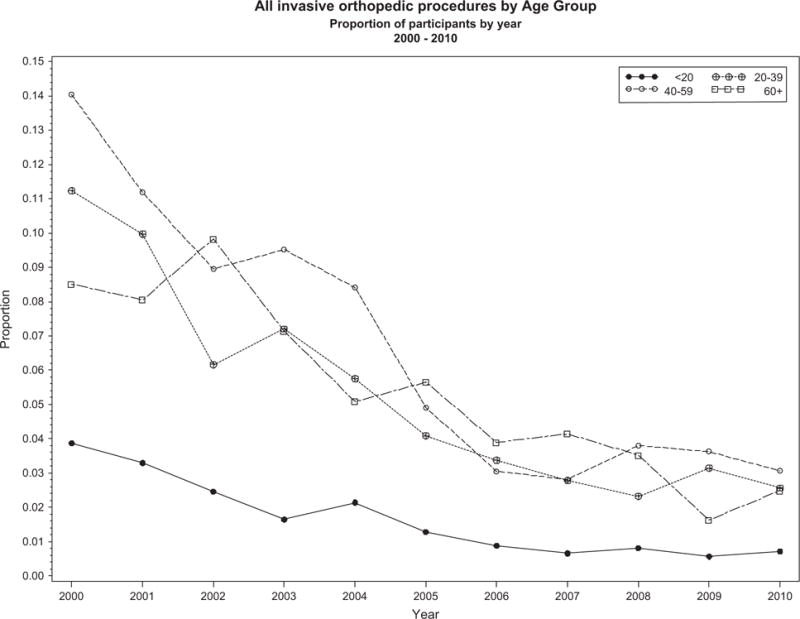
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) by age groups (in years). Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Invasive orthopedic interventions by inhibitor status
We observed a reduction of 7.0% from 2000 to 2010 in invasive orthopedic interventions in people with hemophilia who had a positive inhibitor status and a 5.5% reduction was observed in individuals with a negative inhibitor status (Fig. 5). Much larger year-to-year variations were observed among people positive for inhibitors than among those negative for inhibitors. Excluding the first few years of the study period, a larger proportion of people with inhibitors reported undergoing an orthopedic intervention than people without inhibitor.
Fig. 5.
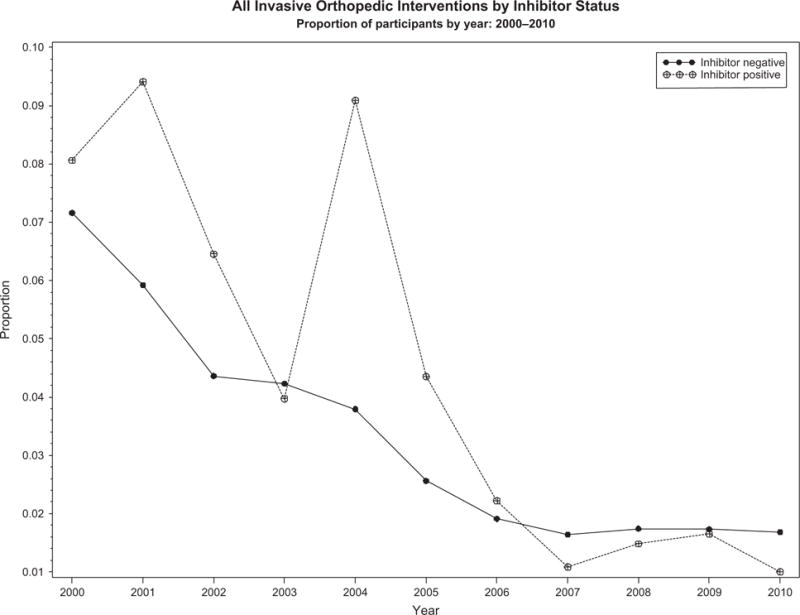
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) by inhibitor status. Inhibitor negative is no reported inhibitor presence in the year prior to and year of an orthopedic intervention. Inhibitor positive is presence of inhibitor the year prior to and year of an orthopedic intervention. Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Invasive orthopedic interventions by prophylaxis status
Among all participants, regardless of their prophylaxis status, a declining trend was identified for all invasive orthopedic interventions (Fig. 6). Throughout the study, a higher proportion of people on intermittent prophylaxis or on demand therapy reported undergoing an orthopedic intervention than did those utilizing continuous prophylaxis. At the start of the study, almost three times as many orthopedic interventions were reported among people on intermittent prophylaxis or on demand therapy (12.06) compared to those who were utilizing continuous prophylaxis (4.61). By the final years of the study, this proportion had decreased to comparable levels in both groups (2.29, 1.57). A reduction of 9.8% in intermittent or on demand group and 3.0% in the continuous prophylaxis group was observed for orthopedic interventions by the year 2010; the trend test was significant for both groups.
Fig. 6.
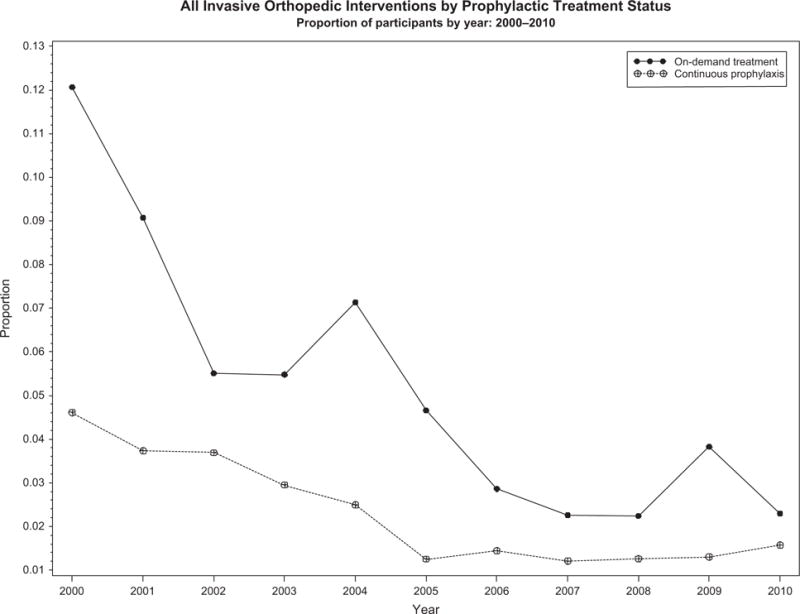
All invasive orthopedic interventions (arthrodesis, arthroplasty, synovectomy, and other) by factor use. ‘On demand’ is defined as intermittent use of factor replacement as recorded by the Universal Data Collection (UDC) program in the year prior to and year of an invasive orthopedic intervention. Continuous prophylaxis is defined recorded continuous prophylaxis by the UDC program in the year prior to and year of an invasive orthopedic intervention. Other, represents a non-specific group of invasive orthopedic interventions not categorized as arthrodesis, arthroplasty or synovectomy.
Discussion
In our study of a large cohort of people with hemophilia enrolled in the UDC in the United States, who had invasive orthopedic interventions, the descriptive trends show a declining number of reported orthopedic interventions for all joints, types and severity of hemophilia, age groups, and groups categorized by inhibitor status and prophylaxis status. Specifically, people with hemophilia enrolled in the UDC program had an average of 5.6% fewer invasive orthopedic interventions by the end of the 11-year study period. Our data show a decreasing trend in both end-stage arthropathy procedures (arthrodesis and arthroplasty) and non-end stage arthropathy procedures (synovectomy and all other invasive interventions). This information confirms what many hemophilia providers have observed over the years of less joint morbidity leading to less invasive orthopedic procedures in the hemophilia population. Understanding the magnitude and trend of invasive orthopedic interventions performed provides a foundation for identifying characteristics associated with orthopedic interventions in people with hemophilia.
The effects of early onset continuous prophylaxis are well documented [14–16]; therefore, the role of prophylaxis in the overall decrease in the number of invasive orthopedic interventions cannot be ruled out. Advances such as the availability of high-quality factor concentrates and recombinant factor concentrates, and the adoption of primary prophylaxis for individuals with severe hemophilia as the standard of care adopted by developed countries [15,16], might decrease the need for orthopedic interventions over time for individuals with hemophilia due to general improvement in joint health and management of joint disease. Our data show that over the study period, the number of UDC enrollees on continuous prophylaxis therapy and on demand therapy reporting invasive orthopedic decreased. The on demand therapy group had a 9.8% decrease in invasive orthopedic interventions compared to the 3% change in the continuous prophylaxis therapy group. The authors hypothesize that over the study period, since approximately over 50% of the people with hemophilia who had undergone invasive orthopedic interventions had severe disease, may have changed their factor replacement practice from on demand therapy to continuous prophylaxis. Our study did not examine this specifically.
An inhibitor creates challenges in obtaining proper factor replacement levels to control bleeding which leads to severe arthropathy and increased risk of bleeding during invasive procedures [17–20]. Despite the increased accessibility to factor replacement and advancements in factor replacement products, an increase in the number of inhibitor patients having orthopedic interventions has been hypothesized by the authors but not observed in our study.
The advancement of minimal invasive synovectomies either by arthroscopy or radioisotope has increased over the years, resulting in a reduction of a more invasive procedure, such as an open synovectomy [21,22]. We anticipated the number of non-end stage procedures such as synovectomy would increase overall; however, our study shows an overall decrease in all three types of synovectomies (1.4% arthroscopic, 0.95% open and 0.83% radioisotopic). We hypothesize the decrease in synovectomies may be related to an increase use of continuous prophylaxis in our study population resulting in overall decrease hemarthrosis.
The category of ‘other’, a group of non-specific orthopedic invasive interventions, shows a slow increase over the study period. The authors hypothesize that because the data for ‘other’ invasive orthopedic interventions refer to a non-specific intervention, many non end-stage interventions such as joint injections and unrelated bleeding disorders complications interventions such as ligamentous repairs are categorized here.
The demographic and clinical characteristics of our study population reflect what previously has been reported in the literature on the occurrence of hemophilia in the United States population [23]. There are limitations to this study to consider. Data were collected from individuals who were enrolled in the UDC program and, therefore, did not represent all individuals with hemophilia in the United States. Additionally, our study consisted of retrospective reporting, which has inherent limitations of underreporting of orthopedic interventions as well as inaccurate reporting (e.g. joint fusion might be recorded under the ‘other’ category vs. being included in the ‘arthrodesis’ category).
Conclusions
Upon examination of proportions of invasive orthopedic interventions in people with hemophilia enrolled in the UDC program during the period 2000–2010, results reveal a decreasing trend in invasive orthopedic interventions across all joints, diagnoses, and age groups regardless of their inhibitor or prophylaxis status. Changes in the standard of care for people with hemophilia, to an early and aggressive factor replacement protocol, as well as availability of high quality factor products are possible reasons for the declining trend in orthopedic interventions in people with hemophilia. Further prospective studies with detailed analysis of characteristics that may influence rates of invasive orthopedic interventions, including factor replacement protocols are recommended.
Acknowledgments
The authors would like to thank the Joint Outcome Committee of the Universal Data Collection Program for their assistance in the preparation of this manuscript and the Hemophilia Treatment Centers Network for their participation in the Universal Data Collection Program.
Footnotes
Author contributions
Patricia Tobase and Azfar Siddiqi wrote the paper. Patricia Tobase, Heidi Lane and Azfar Siddiqi designed the research study. Robina Ingram-Rich, and R. Scott Ward contributed to authorship of the paper and assisted in designing the research study. Azfar Siddiqi performed the statistical analysis.
Disclosures
PT received honoraria for speaking for Bayer Pharmaceuticals. HL received honoraria for speaking and consulting for Bayer and Baxter Pharmaceuticals. All other authors have no conflicts of interest that might be perceived as posing a conflict or bias.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Klamroth R, Pollmann H, Hermans C, et al. The relative burden of haemophilia A and the impact of target joint development on health-related quality of life: results from the ADVATE Post-Authorization Safety Surveillance (PASS) study. Haemophilia. 2011;17:412–21. doi: 10.1111/j.1365-2516.2010.02435.x. [DOI] [PubMed] [Google Scholar]
- 2.Soucie JM, McAlister S, McClellan A, Oakley M, Su Y. The universal data collection surveillance system for rare bleeding disorders. Am J Prev Med. 2010;38:S475–81. doi: 10.1016/j.amepre.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 3.Rahme M, Ehlinger M, Faradji A, et al. Total knee arthroplasty in severe haemophilic patients under continuous infusion of clotting factors. Knee Surg Sports Traumatol Arthrosc. 2012;20:1781–6. doi: 10.1007/s00167-011-1766-8. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Merchan EC. Aspects of current management: orthopaedic surgery in haemophilia. Haemophilia. 2012;18:8–16. doi: 10.1111/j.1365-2516.2011.02544.x. [DOI] [PubMed] [Google Scholar]
- 5.Goddard NJ, Rodriguez-Merchan EC, Wiedel JD. Total knee replacement in haemophilia. Haemophilia. 2002;8:382–6. doi: 10.1046/j.1365-2516.2002.00604.x. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez-Merchan EC. Ankle surgery in haemophilia with special emphasis on arthroscopic debridement. Haemophilia. 2008;14:913–9. doi: 10.1111/j.1365-2516.2008.01820.x. [DOI] [PubMed] [Google Scholar]
- 7.Liras A, Gaban AS, Rodriguez-Merchan EC. Cartilage restoration in haemophilia: advanced therapies. Haemophilia. 2012;18:672–9. doi: 10.1111/j.1365-2516.2012.02816.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez-Merchan EC, De la Corte-Rodriguez H, Jimenez-Yuste V. Radiosynovectomy in haemophilia: long-term results of 500 procedures performed in a 38-year period. Thromb Res. 2014;134:985–90. doi: 10.1016/j.thromres.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Blood safety monitoring among persons with bleeding disorders–United States, May 1998–June 2002. MMWR Morb Mortal Wkly Rep. 2003;51:1152–4. [PubMed] [Google Scholar]
- 10.White GC, 2nd, Rosendaal F, Aledort LM, et al. Definitions in hemophilia. Recommendation of the scientific subcommittee on factor VIII and factor IX of the scientific and standardization committee of the International Society on Thrombosis and Haemostasis. Thromb Haemost. 2001;85:560. [PubMed] [Google Scholar]
- 11.Carcao MD. The diagnosis and management of congenital hemophilia. Semin Thromb Hemost. 2012;38:727–34. doi: 10.1055/s-0032-1326786. [DOI] [PubMed] [Google Scholar]
- 12.Key NS. Inhibitors in congenital coagulation disorders. Br J Haematol. 2004;127:379–91. doi: 10.1111/j.1365-2141.2004.05168.x. [DOI] [PubMed] [Google Scholar]
- 13.SAS/STAT 9.3. SAS Institute Inc; Cary, NC: [Google Scholar]
- 14.Larsson SA. Hemophilia in Sweden. Studies on demography of hemophilia and surgery in hemophilia and von Willebrand’s disease. Acta Med Scand Suppl. 1984;684:1–72. [PubMed] [Google Scholar]
- 15.Lofqvist T, Nilsson IM, Berntorp E, Pettersson H. Haemophilia prophylaxis in young patients–a long-term follow-up. J Intern Med. 1997;241:395–400. doi: 10.1046/j.1365-2796.1997.130135000.x. [DOI] [PubMed] [Google Scholar]
- 16.Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357:535–44. doi: 10.1056/NEJMoa067659. [DOI] [PubMed] [Google Scholar]
- 17.Faradji A, Bonnomet F, Lecocq J, et al. Knee joint arthroplasty in a patient with haemophilia A and high inhibitor titre using recombinant factor VIIa (NovoSeven): a new case report and review of the literature. Haemophilia. 2001;7:321–6. doi: 10.1046/j.1365-2516.2001.00501.x. [DOI] [PubMed] [Google Scholar]
- 18.Ballal RD, Botteman MF, Foley I, Stephens JM, Wilke CT, Joshi AV. Economic evaluation of major knee surgery with recombinant activated factor VII in hemophilia patients with high titer inhibitors and advanced knee arthropathy: exploratory results via literature-based modeling. Curr Med Res Opin. 2008;24:753–68. doi: 10.1185/030079908X273048. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez-Merchan EC, Quintana M, Jimenez-Yuste V. Orthopaedic surgery in haemophilia patients with inhibitors as the last resort. Haemophilia. 2008;14(Suppl 6):56–67. doi: 10.1111/j.1365-2516.2008.01891.x. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Merchan EC, Rocino A, Ewenstein B, et al. Consensus perspectives on surgery in haemophilia patients with inhibitors: summary statement. Haemophilia. 2004;10(Suppl 2):50–2. doi: 10.1111/j.1365-2516.2004.00941.x. [DOI] [PubMed] [Google Scholar]
- 21.Siegel HJ, Luck JV, Jr, Siegel ME. Advances in radionuclide therapeutics in orthopaedics. J Am Acad Orthop Surg. 2004;12:55–64. doi: 10.5435/00124635-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Silva M, Luck JV, Jr, Siegel ME. 32P chromic phosphate radiosynovectomy for chronic haemophilic synovitis. Haemophilia. 2001;7(Suppl 2):40–9. doi: 10.1046/j.1365-2516.2001.00109.x. [DOI] [PubMed] [Google Scholar]
- 23.Soucie JM, Evatt B, Jackson D. Occurrence of hemophilia in the United States. The Hemophilia Surveillance System Project Investigators. Am J Hematol. 1998;59:288–94. doi: 10.1002/(sici)1096-8652(199812)59:4<288::aid-ajh4>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]


