Abstract
Purpose
Guidelines recommend cholesterol screening for all adolescents and young adults (AYAs) ages 17-21 years. Little is known about how screening results impact perceptions of AYA health.
Methods
We recruited 37 AYAs and 35 parents of AYAs with differing risk for abnormal cholesterol results: (1) familial hypercholesterolemia, (2) obesity, and (3) generally healthy. Participants completed quantitative health status ratings using visual analog scales (VAS) and semi-structured interviews regarding three hypothetical cholesterol screening scenarios: a) high likelihood of cardiovascular disease (CVD) before age 40 (“high-risk”), b) some risk of CVD before age 70 (“moderate-risk”), and c) low risk for CVD despite a strong family history of CVD (“low-risk”). We analyzed VAS data with logistic regression and qualitative data with a priori and emergent coding using multiple coders.
Results
Each group perceived all three cholesterol screening scenarios as comparatively less than perfect health; the high-risk result fell furthest from perfect health. While there was no significant difference between AYAs and parents in VAS ratings, qualitative analyses revealed AYAs were more likely than parents to discount the impact of moderate-risk results due to longer length of time before predicted CVD.
Conclusions
AYAs’ and parents’ perceptions of the impact of cholesterol screening results on AYA health varied by presented scenario, ranging from mild to significant decreases in perceptions of AYA health. As universal cholesterol screening continues to be adopted in this age group, further studies of the real-life impact on AYA risk perceptions and subsequent behavior is warranted.
Keywords: Adolescent, Cholesterol, Decision making, Mixed methods
INTRODUCTION
The 2011 National Heart, Lung, and Blood Institute (NHLBI) Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents recommend universal cholesterol screening for adolescents and young adults (AYAs) ages 17-21 years.1 Although uptake of this recommendation has been far from universal,2,3 data from national cohorts4 and large health plans2 indicate that 1 in 5 adolescents in the US have abnormal cholesterol. Almost 500,000 young people ages 17-21 years in the US alone have a low-density lipoprotein cholesterol (LDL-C) level that would qualify for pharmacologic treatment under the 2011 NHLBI guidelines.5
The rationale for universal screening is predicated on the ability to reduce cardiovascular disease later in life through early identification and treatment of abnormal cholesterol in youth. However, not much is known about how AYAs are likely to react to the results of cholesterol screening. Health researchers 6,7 and the lay press 8 often use the term “Young Invincibles” to describe AYAs, representing “their perception that they are not at risk for poor health.” 9 Some studies have found AYAs underestimate their risk for conditions such as sexually transmitted infections,10 teen pregnancy, 11,12 and tobacco addiction.13 However, systematic research does not support the stereotype of adolescents as irrational individuals unaware, or unconcerned about, health risks. For example, one study found AYAs were more likely than adults to consider themselves at risk for developing cardiovascular risk factors such as diabetes and hypertension. 14 Furthermore, it is not clear whether adolescents’ tendency to discount perceptions of future personal health risk differs significantly from those of adults.15,16
Little is known about how AYAs perceive their risk for future diseases of middle and older age including cardiovascular disease (CVD), how screening tests impact these perceptions, or how they impact their current health status. Thus as part of a study assessing the comparative effectiveness of different adolescent lipid screening and treatment strategies, we aimed to assess AYA perceptions of health in response to three hypothetical cholesterol screening results: a high-risk result, a moderate-risk result, and a low-risk result. Because AYAs have varying degrees of parental involvement in their health care during this period of transition to independence, we also aimed to assess how parents of AYAs perceived the screening scenarios would impact their child. We employed a mixed methods design to address this complex issue, choosing simplified hypothetical scenarios in order to reduce variation in the exposure of interest (the cholesterol screening test), a common strategy used to estimate utility or quality of life in comparative effectivness studies. Participants first completed a single-item visual analog scale (VAS) for each scenario to provide a reliable, quantifiable, and valid 17 measure of health status appropriate for our diverse range of stakeholders. 18 Individual qualitative interviews were then used to further explore AYA and parent perspectives regarding cholesterol screening and its impact on AYA health status, allowing for more nuanced perspectives that may not be captured by quantiative measures.
PATIENTS AND METHODS
Sample
We recruited AYAs and parents of AYAs ages 17-21 years from three clinical groups with differing baseline risk for abnormal cholesterol results: generally healthy (healthy, HA), those with obesity (OB), and those with familial hypercholesterolemia (FH), a genetic condition resulting in very high cholesterol and substantially increased CVD risk. We recruited participants from a pediatric preventive cardiology practice (FH only), a general pediatrics practice (HA and OB), and an adolescent/young adult primary care practice (HA and OB) affiliated with an urban academic medical center. For the FH subsample, see full description of recruitment approach in our previously published article.19 For the HA subsample, a trained research assistant approached all AYAs ages 17-21 years of age with a body mass index (BMI) < 30 kg/m2 presenting for routine clinical care and offered them participation in the study. We also requested AYA permission to offer the study to their parents; no parent was contacted without the permission of the AYA. For the OB subsample, we used the same procedure as the HA group (approaching those with a BMI ≥ 30 kg/m2) and also contacted AYAs who had previously participated in an obesity cohort study at the institution. Additional inclusion criteria included (1) no cognitive or communication disorders that would limit participation in interviews, and (2) working knowledge of spoken and written English.
We employed a consecutive enrollment process to recruit 72 participants, based on a pre-specified purposeful sampling design for the qualitative analysis (10-13 participants in each of the six groups (HA-AYA, OB-AYA, FH-AYA, HA-parent, OB-parent, and FH-parent). Participants were not required to participate as a dyad although parent-AYA dyads were allowed. We concluded sampling when we achieved saturation in our thematic analyses (see Data Analysis below). The study was approved by the Boston Children's Hospital Committee on Clinical Investigation.
Study procedures
We employed a sequential mixed method study design. Participants first completed a brief demographic survey followed by VAS for each written cholesterol screening scenario.20 Often used clinically to rate level of pain,21 the VAS is a standard psychometric measurement tool employed where responses are believed to range across a continuum of values. The VAS has also been used in medical decision making to measure perceived current health status for hypothetical scenarios along a 10-centimeter line with clearly labeled anchors (in this case, death and perfect health22). For this study, we created seven scenarios related to cholesterol screening results, treatments for elevated cholesterol, and side effects of treatment; we present only the three VAS scenarios related to cholesterol screening results here (found in the Appendix). VAS responses were quantified by measuring a participant's response with a 10-centimeter ruler and are reported on a scale of 0-100.
Immediately after participants completed the demographic survey and VAS, we conducted a face-to-face semi-structured qualitative interview. For details of interview guide domains, see Mackie et al, 2015.19 Interviews lasted approximately 60 minutes, were audiotaped, and transcribed verbatim. During the interview, we asked a series of questions about responses to each VAS scenario, including the perceived impact on current health (cognitive, emotional, and behavioral) upon learning of the result and intention to pursue health behaviors.
Analysis
We analyzed survey data using descriptive statistics in Stata (Stata Statistical Software: Release 12, StataCorp LP: College Station, TX; 2011). We created a multilevel model to account for each respondent's VAS rating for each of the three cholesterol scenarios. Standard errors were specified to account for intra-class correlations among responses.23,24 We used an ordinal logistic regression link to account for the skewed distributions of VAS scores. We conducted Wald tests to determine whether ratings differed by scenario (low, medium, or high risk), respondent groups (AYA or parent), and clinical group (FH, OB, or HA), and explored interactions among predictors.
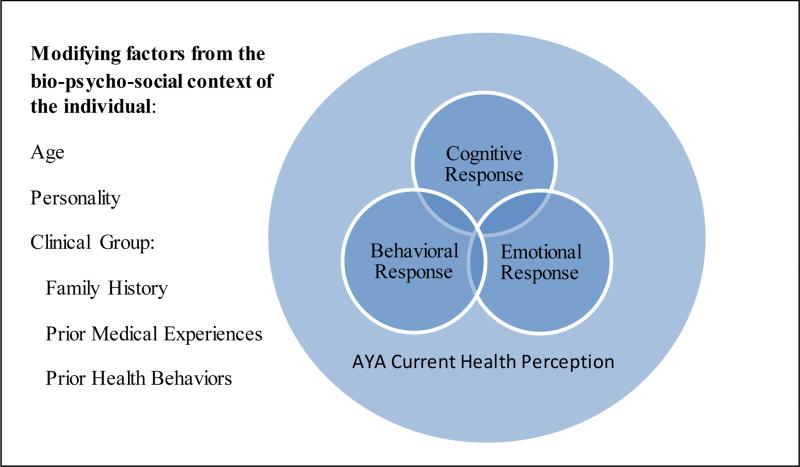
Quantitative data from the VAS then guided the thematic frame for qualitative analysis. We used a modified grounded theory approach, referred to as “Coding Consensus, Co-occurrence, and Comparison,” in which analyses are derived both from extant literature (apriori) and the data (emergent) and then illustrated by characteristic examples.25,26 One investigator (HG) independently read all text pertaining to the three VAS cholesterol screening scenarios to first identify emergent themes. Responses to the three scenarios generally fell into one or more of three inter-related domains – cognitive appraisals regarding the impact of the level of risk on their perceived current health status, emotional reactions to the result, and intentions for behavior change in response to the result. Codes were created based on this conceptual framework, informed by a Cognitive-Behavioral-Emotional Model consistent with past research on patients’ reactions to uncertainty (Figure 1).27 A final set of code definitions were then discussed and delineated by an interdisciplinary team of investigators, including an AYA physician (HG), pediatric cardiologist (SF), clinician-researcher (LKL), two health services researchers (RS, TM) and a trained research assistant (SS). Two team members (HG, SS) then read through and coded each of the 72 transcripts independently before reconciling any differences and applying a final thematic code. Throughout this process, we employed intensive group discussion as our goal was consensual agreement rather than employment of quantitative measures of inter-rater agreement.25,26 Dominant themes are summarized in the main text, with direct quotations chosen to represent heterogeneity of perspectives presented in the tables.
Figure 1.
Conceptual framework of responses to three cholesterol screening scenarios: The Cognitive Behavioral Emotional Model in a bio-psychosocial context
RESULTS
Sample Characteristics
Demographic characteristics of the sample are found in Table 1. White race was more common among FH participants, consistent with the previously described racial/ethnic background of this genetic disorder. Public insurance status, the only indicator of economic status collected in our study, was more common among OB participants. Family history of early CVD was common in all three groups, while cholesterol testing and medication use for high cholesterol were most prevalent in FH groups.
Table 1.
Demographic characteristics of Adolescents/Young Adults (AYAs) and Parents of AYAs participating in the HEARYA study, n=72
| HA-AYA (n=12) | HA-PT (n=13) | OB-AYA (n=13) | OB-PT (n=10) | FH-AYA (n=12) | FH-PT (n=12) | |
|---|---|---|---|---|---|---|
| Mean Age (Range), years | 18.8 (17-21) | 50.3 (41-60) | 18.3 (17-21) | 48.8 (41-55) | 18.4 (17-21) | 49.3 (40-62) |
| Sex | ||||||
| Male | 4 | 0 | 4 | 1 | 6 | 2 |
| Female | 8 | 13 | 9 | 9 | 6 | 10 |
| Ethnicity | ||||||
| Hispanic or Latino | 1 | 2 | 4 | 1 | 2 | 1 |
| Not Hispanic or Latino | 11 | 11 | 9 | 9 | 10 | 10 |
| Race | ||||||
| Asian | 0 | 1 | 0 | 0 | 1 | 0 |
| Black or African American | 6 | 5 | 5 | 6 | 1 | 1 |
| White | 4 | 7 | 3 | 3 | 9 | 9 |
| Multiple Races | 1 | 0 | 2 | 1 | 0 | 0 |
| Insurance Status | ||||||
| Private | 7 | 10 | 4 | 3 | 7 | 9 |
| Public | 4 | 3 | 3 | 6 | 1 | 2 |
| Other/Don't know | 1 | 0 | 6 | 1 | 4 | 0 |
| Family History | ||||||
| Early heart disease or stroke, 1st or 2nd degree relative | 7 | 4 | 9 | 7 | 8 | 9 |
| High cholesterol, 1st or 2nd degree relative | 5 | 7 | 10 | 8 | 10 | 11 |
| AYA Had Prior Test for High Cholesterol | ||||||
| Yes | 2 | 6 | 5 | 3 | 12 | 12 |
| No | 7 | 4 | 1 | 4 | 0 | 0 |
| I don't know | 3 | 3 | 7 | 3 | 0 | 0 |
| AYA On Medication for High Cholesterol | ||||||
| Yes | 0 | 0 | 0 | 0 | 9 | 10 |
| No | 12 | 13 | 11 | 9 | 3 | 2 |
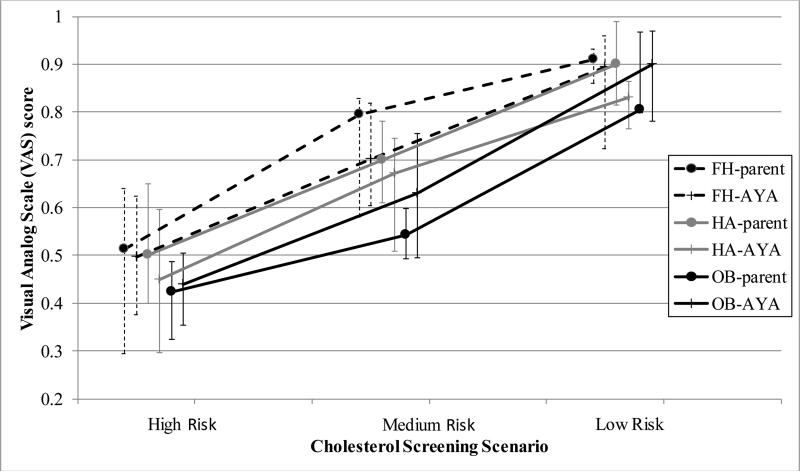
Visual Analog Scale
Each of the six groups indicated that results of the high-risk, moderate-risk, and low-risk scenarios led to less than perfect current health status for the AYA (Figure 2). The high-risk scenario was rated on average as halfway between death and perfect health (Median = 0.50; IQR = 0.31-0.60). Most participants rated the low-risk scenario as close to perfect health (Median = 0.89; IQR = 0.80-0.96). The moderate-risk scenario received ratings intermediate to the two other scenarios (Median = 0.67; IQR = 0.51-0.80). Pairwise differences between median values among the three questions were all highly significant (p<.0001) although there was a wide range of responses from individuals in each of the six groups. Median scores of parents were closer to perfect health than those of AYAs in the FH and HA groups. Visual inspection revealed that medians for the FH group were closer to perfect health than for the HA group, which in turn were higher than the OB group. These descriptively different findings, which did not reach statistical significance, were then further investigated qualitatively to better understand how preferences and values influenced individual VAS scores.
Figure 2.
Responses of Adolescents/Young Adults (AYAs) and Parents of AYAs with familial hypercholesterolemia (FH), no risk factors for high cholesterol (healthy, HA), and obesity (OB) to three cholesterol screening scenarios on a Visual Analog Scale (where 0=death and 1=perfect health)
Qualitative Analysis
AYA and Parental Reactions to High-Risk Result – Table 2
Table 2.
Sample responses from Adolescents/Young Adults (AYAs) and Parents of AYAs with no risk factors for high cholesterol (healthy, HA), obesity (OB), and familial hypercholesterolemia (FH) to three cholesterol screening scenarios
| Reponses to the high-risk result | AYA (n=37) | Parent (n=35) | ||
|---|---|---|---|---|
| Cognitive | N | Example | N | Example |
| No/minimal change in risk perception | 1 | “Well I feel pretty healthy so I don't think that just knowing another number would really make me feel any different” (FH) | 7 | “How he would react to the news? As an eighteen year old man there's not that much that concerns him other than video games and what have you, I think he would be rather nonchalant in terms of the way that he takes the news.” (FH) |
| Future risk perception related to age at predicted CVD event | 23 | “I put it like about three tick marks away from death...Because I think 40 is a kind of close age and 40's kind of young. So, to know that I might have a heart attack before then I think is kind of like death. It's like I'm not getting a chance to live really.” (OB) | 14 | “So that would really affect her because even looking at, “I'm twenty now and then at forty,” like ... That's twenty years and at forty like, “I should still be doing fabulous things not thinking about whether I'm going to have a ... or be at high risk by having a heart attack.” (HA) |
| Impact on perception of current health | 17 | “I don't know, imaging myself being told that I have a good chance of having a heart attack before I turn 40 I might rate myself lower. But, I don't know. Like I feel like otherwise if you have otherwise perfect health and you're living a good life and you're pretty healthy and pretty happy then I would still consider myself more healthy than not.” (HA) | 9 | “I'm thinking something's really, you know must be wrong with his metabolism because he...just judging from my son, he doesn't look like he should have high cholesterol so I'd be worried that there was something dramatically wrong with him.” (HA) |
| Emotional | N | Example | N | Example |
| No/minimal emotional response | 3 | “Well, I probably wouldn't get too emotional about it, because of the medical issues that I've dealt with in the past. I don't like to get stressed out about those type of things, so I would probably just keep my composure.” (HA) | 4 | “I don't think it would affect her emotionally, I think it would be in the back of her mind. But she's young enough that I think she'd be fine.” (OB) |
| Negative emotional response | 26 | “I'd be sad. I'm cutting my life short. I'm not going to be able to have the same experiences that everybody else would.” (OB) | 28 | “Well, knowing that she has that and she can get sick from it or you know have a heart attack before she's 40 years old is pretty scary and nervous, probably make her nervous because she'll worry about that.” (OB) |
| Positive emotional response | 0 | n/a | 0 | n/a |
| Behavioral | N | Example | N | Example |
| No/minimal behavioral response | 1 | “I feel like I wouldn't have the motivation to go out and workout and stuff and keep training for football. I feel like I would be just like mopey and just and I wouldn't have the energy.” (OB) | 3 | “So then their tendency is to shelve it because, “I got more important things to do. I got to graduate from college. I'm going to have a career. Buy my first car. I'm going to get married.” You know, “So I'll solve this cholesterol problem later.” (FH) |
| Plan to initiate or improve health behaviors | 22 | “I'd definitely change some of the things I do in life. Like physically I just would exercise all the time and I wouldn't eat half the things I throw in my mouth.” (HA) | 27 | “Well, depending on what the doctor said, whatever they recommended, she would try doing whether it was changing her diet, or taking some kind of medication, or exercising I think she would try, but I think she would feel... I think she would feel kind of bad about it, but she would do it.” (OB) |
| Reponses to the moderate-risk result | AYA (n=37) | Parent (n=35) | ||
| Cognitive | N | Example | N | Example |
| No/minimal change in risk perception | 1 | “I was just thinking that's about what seems normal nowadays almost in America, with the way everybody eats and the slight lack of exercise.” (OB) | 10 | “I think if you told a kid, ‘You know, this means that you might have a heart attack sometime, you know, 70.’ Like he can't even imagine 70. So I don't think that's meaningful at all.” (FH) |
| Future risk perception related to age at predicted CVD event | 30 | “I think it's better to have a heart attack when your that old than...I shouldn't say that it's better but it's more common for it to happen when your later in life and I will have done a lot more things that I wanted to do with my life before I turn 70.” (OB) | 27 | “My impression of knowing him is like I said there is a big difference in very high and somewhat. Very high sounds like a tougher diagnosis, I guess than in 40 you might have a heart attack before 40 versus 70. Those years from 40 – 70 that's pretty much middle age so you have gone from young to middle age, I mean to elderly.” (HA) |
| Impact on perception of current health | 3 | “I just figured that this probably wouldn't affect me as much until I was older, so for now I was in better health, I guess.” (FH) | 2 | “I don't think that you're again perfect health. I think you still have to maintain that vigilance for the rest of your life.” (FH) |
| Emotional | N | Example | N | Example |
| No/minimal emotional response | 17 | “I probably wouldn't be as freaked out as the first one. I'd probably still be calm, but still a little weary about what it is I do.” (OB) | 9 | “Emotional health, I'm not sure it would really impact. At this young age, 70 seems like you know forever.” (HA) |
| Negative emotional response | 12 | “I'd still be pretty scared. I don't know, whenever I hear the word ‘heart attack’ for some reason I automatically think negative. I know it's not a good thing but I always either think really, really sick or close to death so it would still probably scare me.” (OB) | 11 | “I mean, I think she'd be upset and nervous but kind of might be like, ‘Oh, it's not there, you know it's not high yet.’ and kind of let things go.” (OB) |
| Positive emotional response | 0 | n/a | 0 | n/a |
| Behavioral | N | Example | N | Example |
| No/minimal behavioral response | 5 | “I don't think I would take it seriously. I would brush it off kind of. I would probably work to stay away from salty foods and stuff that make cholesterol high for like a month. But after that I wouldn't care because it's not that high. It's not going to affect me probably until later on.” (HA) | 5 | “With her attitude she would say, ‘Okay, I'm not forty but I'm seventy so I have longer to live so I have more time to eat the way I want to eat.’” (HA) |
| Plan to initiate or improve health behaviors | 12 | “I think I'd just make sure exercise was a big one with eating healthy, but when you want crappy food once in a while then okay it's not as big of a concern.” (FH) | 14 | “I think that she would look at her health as something that she needed to work on through diet, or whatever her doctor would recommend.” (OB) |
| Reponses to the low-risk result | AYA (n=37) | Parent (n=35) | ||
| Cognitive | N | Example | N | Example |
| No/minimal change in risk perception | 7 | “I kind of had like that teenage mind set where oh like you're Mr. Invincible like nothing will ever happen to you so I thought I'd be fine just because it like happened to a few people, almost impossible. I mean just because it happened to like people in my family, and why would it ever happen to me. I mean I'm healthy and fit.” (FH) | 8 | “Oh, I think he would see himself as a 100 percent healthy. He would just say that, that's them, not me.” (FH) |
| Future risk perception related to normalcy of result | 5 | I'd move it up to about ninety because I mean normal...In perspective of the other ones before it that one is pretty good. They said the risk isn't any earlier than anybody else; it's about the same as most people. (OB) | 2 | “Because the test is normal so, you know there's nothing really to get alarmed at right now like the other two questions and you know and work to improve whatever she's doing to keep it normal.” (OB) |
| Impact on perception of current health | 4 | “The only reason that I'd be feeling like unhealthy at all is because I know that like at some point like my cholesterol could get higher. And like I could have a problem because everyone in my family. But at this point like I'm feeling fine and the test says that I'm fine for now.” (HA) | 7 | “I would think that would mean that okay, he's eating correctly, he's eating his vegetables, fruits, he's exercising and he's doing all the right things to monitor his cholesterol. And if he continues hopefully it will stay normal. I think he would feel like that.” (HA) |
| Emotional | N | Example | N | Example |
| No/minimal emotional response | 5 | “I feel like that if I got a result that was normal, I wouldn't be worried at all, I would just kind of brush it off and go on with what I was doing.” (FH) | 6 | “She wouldn't worry about because it's normal.” (OB) |
| Negative emotional response | 5 | “It would still make me nervous...Because it's like everybody else is dying from the same thing in my family and you never know, one day you could have good cholesterol and a couple of weeks later you might not. It's all about what you do with yourself.” (OB) | 2 | “So I gave this one a 95. And I think it's because if I had a biological history of heart attack there'd still be some level of worry. I'd be very relieved that it isn't high cholesterol now. But I'd still be looking at, you know, you're young and we're gonna be checking this again later.” (FH) |
| Positive emotional response | 22 | “I'd feel relief because seeing it around us, you know, uncles have it and my grandparents had, you know, high cholesterol health, heart problems. So it would probably take a load off of my shoulders if I didn't have that to deal with.” (FH) | 23 | “Oh he would be very happy of having it normal but I think that we would point out to him that still the family history's there. Like there's nothing you can do about your genes, you know?” (HA) |
| Behavioral | N | Example | N | Example |
| No/minimal behavioral response | 1 | “I would keep it in the back of my head, but I wouldn't be like oh, I must do something to keep it normal. I would just kind of keep doing whatever I was doing.” (FH) | 1 | “You know, it's normal but she is still overweight and my daughter, the way her brain works is, ‘I (inaudible) and I can just lay in bed and watch TV all day. I don't have to get out of bed and do anything.’” (OB) |
| Plan to initiate or improve health behaviors | 12 | “Well I mean if you're genetically predisposed to it you're more likely to get it. So you could do more to counteract that in as far as your lifestyle decisions then you're less likely to get a heart attack.” (HA) | 10 | “Yeah, make sure you get it checked every year. Make sure you're feeding your body right.” (FH) |
Most AYAs and parents described a significant decrease in the AYA's perception of their current and future health in response to the high-risk scenario. While many parents expressed concerns that AYAs would not take the high-risk result seriously, only an occasional AYA said the high-risk result would not change their perception of their current health. The vast majority of AYAs felt knowing they might have a heart attack at such a young age (40 years) greatly impacted their sense of health and related their concerns to what they hoped to be doing with their lives at that age (parenting, working).
AYAs almost uniformly expressed negative emotional reactions to the high-risk result, including fear, anxiety, depression, and worry. A few AYAs noted that receiving such a result would make them feel guilty that they had not done more to protect their health. Most parents also felt the result would worry their AYAs, although several parents were concerned AYAs would have inadequate emotional reaction to anything related to future risk of disease—even in the high-risk result scenario—at this young age.
Most AYAs said the high-risk result would motivate them to take action in some way, typically by improving their dietary choices or starting/intensifying their exercise routine. In contrast, several parents expressed concern that their AYAs would not change their current behaviors either due to the competing demands of young adulthood or a sense of invincibility despite the high-risk result. Most parents remained hopeful that their AYA would be motivated to take action to address the high risk for future heart disease and were prepared to help them to do so by encouraging and facilitating healthy behaviors.
AYA and Parental Reactions to Moderate-Risk Result – Table 2
There was a wider range of AYA responses to the moderate-risk result, which was described as indicating risk of heart attack by age 70 years. Many AYAs felt that any elevation in their risk for heart disease decreased their current health status, although most conceded that this result would impact them less than the high-risk result. Again, AYAs and parents related their perceptions of the AYA's current health status to the age at predicted heart attack. Many AYAs rationalized that this was close to the average life expectancy in the US and/or was when people were expected to have heart attacks anyway. Parents were often skeptical that AYAs would have much of a reaction to a predicted event 50 years in the future.
Many AYAs still believed the moderate-risk result would cause anxiety or worry, simply because it would mean they were “abnormal.” Most felt their level of concern would be less than in response to the high-risk result. This lesser concern and the long lag time before a predicted heart attack was also linked to decreased expressed motivation to change behaviors by many AYAs and parents. AYAs and parents both commented that AYAs would either initiate behavior change but have difficulty sustaining it in response to this scenario or would procrastinate and wait to initiate behavior change until they were older and closer to the age at predicted CVD events.
AYA and Parental Reactions to Low-Risk Result – Table 2
Most AYAs and parents felt the low-risk result would have little impact on their perceived current health status. Some individuals described the family history/genetics as indicative of potential poor health, but most focused on the normalcy of the result. AYAs and parents were apt to note happiness or relief in response to this reassuring result. While some AYAs and parents said they would continue to work on healthy behaviors and actively monitor their cholesterol due to the strong family history of heart disease, others said they would simply keep doing what they are doing given the normal result.
Modifying Factors Including Clinical Groups – Table 3
Table 3.
Modifying factors of the cognitive, emotional, and behavioral responses to high-risk cholesterol screening results from Adolescents/Young Adults (AYA) and Parents (PT) of AYAs with no risk factors for high cholesterol (healthy, HA), obesity (OB), and familial hypercholesterolemia (FH)
| Responses | HA | n | OB | n | FH | n |
|---|---|---|---|---|---|---|
| Role of personality | “But this child in particular, does tend to be conscientious. He lives a pretty healthy life. He would never consider smoking or anything like that. Something like this would only just cement that.” (PT) | n=9 | “I think she would be very concerned, but I think knowing her, she has a very positive attitude, so I think she would approach it with trying to do what she needs to do to get her health in a better state.” (PT) | n=6 | “I don't think he has a thorough understanding of what all this means. And, you know, even though we've been coming here for years and there's been a lot of discussion and monitoring, I think it's, some of it's his personality and some of it's his developmental level.” (PT) | n=2 |
| Role of family history | “It would definitely scare her. She has a grandparent who had a young heart attack and has a pace maker. She knows that it's life altering if you have heart disease.” (PT) | n=1 | “It would scare me. I'd probably cry just because I do have people in my family who have had heart attacks so it would probably really scare me.” (AYA) | n=3 | “Yeah, well, my dad passed away of a heart attack, he had high cholesterol until about 300. He was on medicine, overall a healthy guy. It was exercising. But, so the worry comes from that. You know, what if that happens to me if I don't keep it under control. So it's always a stress and anxiety trigger.” (AYA) | n=6 |
| Role of prior medical experiences and prior health behaviors | “Well, because she's had eating disorder I would worry that it might spark that. You know, it might be a trigger for some of those behaviors.” (PT) | n=2 | “I think it would go downhill at first; it would be a battle. It would be a battle to come up. It would be very stressful for me. I only say that because I'm already dealing with a child with severe ADHD behavior. He's eighteen but really twelve. I mean it's not an easy household right now.” (PT) | n=1 | “So I know I've seen results myself with exercise. I've seen my HDL go up and then with diet I've seen my LDL go down. With the medication I've really seen a reduction in my LDL so it seems like just something that you can...I've been lucky though; I know other people have trouble managing it.” (AYA) | n=5 |
The overall pattern of responses to the high-risk, moderate-risk and low-risk scenarios was similar for all three clinical groups. However, individuals within the three groups often spoke of unique experiences that would modify their reaction to a given scenario. These modifying factors were commonly attributed to elements of the individuals’ bio psychosocial context (see Figure 1), most notably their demographic (i.e., age), psychological (i.e., personality factors), and clinical group. Personality factors – including the tendency to act in response to health threats or the tendency to worry about one's health – were mentioned by individuals in all three groups. Family histories of heart disease were most frequently mentioned by the OB and FH groups compared to the HA group, likely reflecting the increased likelihood of a related family history for these clinical sub-populations. Similarly, individuals in the FH group were more likely to mention prior experiences with cholesterol testing and cholesterol medications.
DISCUSSION
Our study demonstrates that test results commonly encountered in adolescent cholesterol screening have the potential to impact AYA's perceptions of their current health status, with screening results consistent with the FH phenotype associated with the lowest health status ratings. If universal cholesterol screening was fully implemented in the US, based on our prior epidemiologic work, we anticipate around 78,000 AYAs living in the US today (0.4% of the AYAs ages 17-21 years) would be impacted by such a result.5 Moderate-risk results, expected to affect up to 2.5% of US AYAs ages 17-21 years,11 were also associated with less than perfect health status. Interestingly, AYAs and parents of AYAs responded similarly on quantitative measures of AYA health status in response to cholesterol screening.
Consistent with recent empirical evidence on adolescent risk perceptions,15,16 we found little evidence for the “Young Invincible” narrative in our sample. AYAs who participated in our study consistently expressed worry about future risks for heart disease and related intentions to engage in risk-reducing health behaviors. These qualitative findings were in contrast to the concerns of many parents but are consistent with recent research on decision making among AYAs.16 We did find a graded response from AYAs related to the age at future risk for heart disease, with many AYAs discounting the relevance of the moderate-risk scenario when evaluating their current health. This is consistent with prior findings in the tobacco literature that suggests young people have a poor understanding of the relevance of cumulative risk of an exposure over the lifetime.28 Given data demonstrating the importance of early young adult factors for later life cardiovascular health,29 this lower motivation to address health threats many years in the future represents an opportunity for targeted health promotion efforts. In particular, these findings are suggestive of the promise for health counseling, within a motivational interviewing framework, in delivering results of cholesterol screening with AYAs; further research examining the effectiveness of such approaches is warranted.
Although there was a consistency in responses from both our quantitative and qualitative results across clinical groups with varying CVD risk, our findings also demonstrate that AYAs are likely to respond to cholesterol screening within their given bio psychosocial context. Perhaps because they had already developed strategies for coping with the health threat of early heart disease, AYAs and parents of AYAs with FH had the highest health ratings overall. OB respondents had the lowest ratings, which may reflect prior challenges addressing the health threat of obesity or unmeasured demographic and sociocultural covariates. These results emphasize the importance for providers to consider the overall context in which a patient is engaging in disease screening and interpreting results.
Our results should be interpreted in the context of several limitations. Participants were volunteers from academic-affiliated practices in the US and results are not generalizable to the general population of AYAs. It is likely that AYAs less connected to a medical home and/or less likely to participate in research would have different attitudes toward cholesterol screening results; we speculate they may be more likely to minimize the impact of cholesterol results on their current health. Sample sizes, while sufficient to reach saturation for qualitative analyses, may have been insufficient to fully evaluate observed differences between parents and AYAs on the quantitative VAS. Participants were responding to hypothetical and simplified cholesterol testing scenarios, and with the exception of FH participants, few had actually received a personal cholesterol result. Likewise, parents were speculating on the likely responses of their AYA child. Future naturalistic studies that follow the response of AYAs in response to actual cholesterol screening results will be important to fully understand the impact of universal cholesterol screening for this age group. Expressed likelihood of behavior change should be greeted with caution in light of these limitations, especially given the existing literature on lack of behavior change in the general population in response to cardiac screening results.30
CONCLUSION
Results suggest that both AYAs and parents are likely to feel the impact of abnormal cholesterol screening results, creating the potential for positive behavioral changes that could reduce the burden of CVD. However, AYAs with abnormal screening results may also experience a decrease in their perceptions of current health. To maximize the potential for benefit and mitigate the potential for harm, providers will need to engage AYAs and their parents in a discussion of patient-centered values and likely responses to results before ordering this simple screening test.
Supplementary Material
Acknowledgements
The authors wish to acknowledge the twenty member stakeholder panel for assistance with study design and interpretation of results. The authors would like to thank Jacqueline O'Brien, Allegra Spaulding, and Currie Touloumtzis for assistance with participant recruitment and Currie Touloumtzis for assistance with manuscript preparation.
Funding Source: This work was (partially) supported through a Patient-Centered Outcomes Research Institute (PCORI) Assessment of Prevention, Diagnosis, and Treatment Options Program Award (1443). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Footnotes
Implications and Contribution:
Adolescents and parents of adolescents perceive reductions in the adolescents’ current health status in response to abnormal cholesterol screening results. The cognitive, emotional, and behavioral impact of abnormal cholesterol results is related to the predicated age of future heart disease
Financial Disclosure Statement: Dr. de Ferranti receives royalties from UpToDate for review topics on cholesterol screening and treatment in childhood. The other authors have no financial disclosures relevant to this article.
Conflicts of Interest Statement: Dr. de Ferranti serves on the American Academy of Pediatrics Committee on Nutrition. Dr. de Ferranti and Dr. Gooding serve on the American Heart Association Atherosclerosis, Hypertension and Obesity in Youth Committee. The other authors have no conflicts of interest relevant to this article to disclose.
REFERENCES
- 1.Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011 Dec;128(Suppl 5):S213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Margolis KL, Greenspan LC, Trower NK, et al. Lipid screening in children and adolescents in community practice: 2007 to 2010. Circ Cardiovasc Qual Outcomes. 2014 Sep;7(5):718–726. doi: 10.1161/CIRCOUTCOMES.114.000842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vinci SR, Rifas-Shiman SL, Cheng JK, Mannix RC, Gillman MW, de Ferranti SD. Cholesterol testing among children and adolescents during health visits. JAMA. 2014 May 7;311(17):1804–1807. doi: 10.1001/jama.2014.2410. [DOI] [PubMed] [Google Scholar]
- 4.Kit BK, Carroll MD, Lacher DA, Sorlie PD, DeJesus JM, Ogden C. Trends in serum lipids among US youths aged 6 to 19 years, 1988-2010. JAMA. 2012 Aug 8;308(6):591–600. doi: 10.1001/jama.2012.9136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gooding HC, Rodday AM, Wong JB, et al. Application of Pediatric and Adult Guidelines for Treatment of Lipid Levels Among US Adolescents Transitioning to Young Adulthood. JAMA Pediatr. 2015 Apr 6; doi: 10.1001/jamapediatrics.2015.0168. [DOI] [PubMed] [Google Scholar]
- 6.Solar-tuttle R. Harvard AIDS review. Spring-Summer; 2000. The invincible ones. pp. 12–14. [PubMed] [Google Scholar]
- 7.Elnicki DM. Hypertension among the young invincibles. J. Gen. Intern. Med. 2014 Aug;29(8):1085–1086. doi: 10.1007/s11606-014-2866-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amsden D. The Young Invincibles. New York Magazine; New York City, NY: 2007. [Google Scholar]
- 9.Bibbins-Domingo K, Burroughs Pena M. Caring for the “young invincibles”. J. Gen. Intern. Med. 2010 Jul;25(7):642–643. doi: 10.1007/s11606-010-1388-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ethier KA, Kershaw T, Niccolai L, Lewis JB, Ickovics JR. Adolescent women underestimate their susceptibility to sexually transmitted infections. Sex. Transm. Infect. 2003 Oct;79(5):408–411. doi: 10.1136/sti.79.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witte K. Preventing teen pregnancy through persuasive communications: realities, myths, and the hard-fact truths. J. Community Health. 1997 Apr;22(2):137–154. doi: 10.1023/a:1025116923109. [DOI] [PubMed] [Google Scholar]
- 12.Aubrey JS, Behm-Morawitz E, Kim K. Understanding the effects of MTV's 16 and Pregnant on adolescent girls' beliefs, attitudes, and behavioral intentions toward teen pregnancy. Journal of health communication. 2014;19(10):1145–1160. doi: 10.1080/10810730.2013.872721. [DOI] [PubMed] [Google Scholar]
- 13.Viscusi WK. Age variations in risk perceptions and smoking decisions. The Review of Economics and Statistics. 1991;73:577–588. [Google Scholar]
- 14.Cohn LD, Macfarlane S, Yanez C, Imai WK. Risk-perception: differences between adolescents and adults. Health Psychol. 1995 May;14(3):217–222. doi: 10.1037//0278-6133.14.3.217. [DOI] [PubMed] [Google Scholar]
- 15.Steinberg L, Graham S, O'Brien L, Woolard J, Cauffman E, Banich M. Age differences in future orientation and delay discounting. Child Dev. 2009 Jan-Feb;80(1):28–44. doi: 10.1111/j.1467-8624.2008.01244.x. [DOI] [PubMed] [Google Scholar]
- 16.Steinberg L. Risk taking in adolescence: new perspectives from brain and behavioral science. Current Directions in Psychological Science. 2007;16(2):55–59. [Google Scholar]
- 17.de Boer AG, van Lanschot JJ, Stalmeier PF, et al. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual. Life Res. 2004 Mar;13(2):311–320. doi: 10.1023/B:QURE.0000018499.64574.1f. [DOI] [PubMed] [Google Scholar]
- 18.Gaskin DJ, Frick KD. Race and ethnic disparities in valuing health. Med. Decis. Making. 2008 Jan-Feb;28(1):12–20. doi: 10.1177/0272989X07309641. [DOI] [PubMed] [Google Scholar]
- 19.Mackie TI, Tse LL, De Ferranti S, Ryan HR, Leslie LK. Treatment decision-making for adolescents with familial hypercholesterolemia: role of family history and past experiences. Journal of Clinical Lipidology. 2015;9(4):583–593. doi: 10.1016/j.jacl.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parkin D, Devlin N. Is there a case for using visual analogue scale valuations in cost-utility analysis? Health Econ. 2006 Jul;15(7):653–664. doi: 10.1002/hec.1086. [DOI] [PubMed] [Google Scholar]
- 21.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad. Emerg. Med. 2001 Dec;8(12):1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 22.Torrance GW, Feeny D, Furlong W. Visual analog scales: do they have a role in the measurement of preferences for health states? Med Decis Making. 2001 Jul-Aug;21(4):329–334. doi: 10.1177/0272989X0102100408. [DOI] [PubMed] [Google Scholar]
- 23.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000 Jun;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 24.White H. A heteroskedasticity-consistent covariance matrix estimator with a direct test for heteroskedasticity. Econometrica. 1980;48:817–830. [Google Scholar]
- 25.Willms DG, Best JA, Taylor DW, et al. A systematic approach for using qualitative methods in primary prevention research. Med. Anthropol. Q. 1990;4(4):391–409. [Google Scholar]
- 26.Harry B, Sturges K, Klingner J. Qualitative data analysis: mapping the process. Educational Researcher. 2005;34(2):3–13. [Google Scholar]
- 27.Grenier S, Barrette A-M, Ladouceur R. Intolerance of uncertainty and intolerance of ambiguity: similarities and differences. Personality and Individual Differences. 2005;39(3):593–600. [Google Scholar]
- 28.Slovic P. What does it mean to know a cumulative risk? Adolescents' perceptions of short-term and long-term consequences of smoking. Journal of Behavioral Decision Making. 2000;13(2):259–266. [Google Scholar]
- 29.Gooding HC, Shay CM, Ning H, et al. Optimal Lifestyle Components in Young Adulthood Are Associated With Maintaining the Ideal Cardiovascular Health Profile Into Middle Age. J Am Heart Assoc. 2015;4(11) doi: 10.1161/JAHA.115.002048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodondi N, Collet TH, Nanchen D, et al. Impact of carotid plaque screening on smoking cessation and other cardiovascular risk factors: a randomized controlled trial. Arch. Intern. Med. 2012 Feb 27;172(4):344–352. doi: 10.1001/archinternmed.2011.1326. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.