Abstract
Background
Chest CT scans are frequently performed in radiology departments but have not previously contained detailed depiction of cardiac structures.
Objectives
To evaluate myocardial and coronary visualization on high-pitch non-gated CT of the chest using 3rd generation dual-source computed tomography (CT).
Methods
Cardiac anatomy of patients who had 3rd generation, non-gated high pitch contrast enhanced chest CT and who also had prior conventional (low pitch) chest CT as part of a chest abdomen pelvis exam was evaluated. Cardiac image features were scored by reviewers blinded to diagnosis and pitch. Paired analysis was performed.
Results
3862 coronary segments and 2220 cardiac structures were evaluated by two readers in 222 CT scans. Most patients (97.2%) had chest CT for oncologic evaluation. The median pitch was 2.34 (IQR 2.05, 2.65) in high pitch and 0.8 (IQR 0.8, 0.8) in low pitch scans (p<0.001). High pitch CT showed higher image visualization scores for all cardiovascular structures compared with conventional pitch scans (p<0.0001). Coronary arteries were visualized in 9 coronary segments per exam in high pitch scans versus 2 segments for conventional pitch (p<0.0001). Radiation exposure was lower in the high pitch group compared with the conventional pitch group (median CTDIvol 10.83 vs. 12.36 mGy and DLP 790 vs. 827 mGycm respectively, p <0.01 for both) with comparable image noise (p=0.43).
Conclusion
Myocardial structure and coronary arteries are frequently visualized on non-gated 3rd generation chest CT. These results raise the question of whether the heart and coronary arteries should be routinely interpreted on routine chest CT that is otherwise obtained for non-cardiac indications.
Keywords: CT, Cardiac imaging, incidental findings
1. Introduction
Chest computed tomography (CT) protocols are one of the most commonly performed CT examinations in radiology departments. For oncologic disease, chest CT is performed without ECG gating and with iodinated contrast injected at moderate flow rates. In comparison, cardiac CT protocols typically include a) pharmacologic control of heart rate, b) coronary vasodilation, c) electrocardiogram gating and d) optimization of high flow iodine injection rates and e) diastolic phase imaging. These specialized cardiac CT protocols result in very high sensitivity and specificity of greater than 90% for significant coronary artery disease 1.
However, even using older generation CT scans, coronary artery calcification scores can be obtained from routine non-contrast chest CT (i.e., CT performed for non-cardiac indications) 2. These calcium score findings may be “incidental” to the primary indication for the chest CT, but may be important to patient care 3. Despite the wide availability of treatment for coronary artery disease, there is no consensus in the radiology community as to whether patients and physicians should be made aware of incidental calcium score findings. In contradistinction, pulmonary nodules are common incidental findings on dedicated calcium score CT (23–48% incidence 4). Pulmonary nodules are routinely reported by radiologists despite much less compelling data for follow-up and treatment 4.
New, third generation dual source CT scanners can now image the entire chest in less than 1 second with isotropic 3-dimensional spatial resolution of approximately 0.5 mm 5. With this rapid scan speed, the superior to inferior extent of the heart is imaged in only a few hundred milliseconds. Technical issues including a reduced field of view in high-pitch dual source CT and a potential for increased artifacts have been largely mitigated using a wider second detector and improved reconstruction algorithms. Rapid scanning can “freeze” cardiac motion, providing heart and coronary detail that has not previously been visualized on chest CT 6 and that may require interpretation by the imaging physician. Thus, the purpose of this study was to evaluate visualization of coronary and cardiovascular features on routine chest CT using 3rd generation dual source CT. For comparison, we identified patients who also had undergone 2nd generation dual source CT of the chest.
2. Methods
2.1. Study design and patient selection
Our institution’s Office of Human Research Services reviewed the study design; institutional requirements for IRB review and patient consent were waived. All patient related information (including CT scan date) was anonymized by an independent third party who was not involved in review of CT scan data. We used the hospital information system to identify consecutive patients who had both 3rd generation high pitch (pitch > 1) contrast enhanced chest, abdomen and pelvis scans between 11/5/2014 and 1/5/2015 as well as prior conventional pitch CT (pitch ≤ 1, referred to as “low pitch”), performed within 12 months of the high pitch CT scan. No further selection of studies was applied (i.e., consecutive patient studies were reviewed without further exclusions).
2.2. Image acquisition
The “pitch” of a CT scan is commonly defined as the ratio of table feed per 360 degree gantry rotation and collimated beam width 7. High pitch scans were performed using a 3rd generation dual-source CT scanner as a standard procedure for chest abdomen pelvis exams (Somatom Force, Siemens Medical Systems, Forchheim, Germany). A key feature of 3rd generation dual source CT is a high capacity x-ray tube capable of very high photon flux to allow approximate doubling of scan pitch. Iterative reconstruction methods were also reported by the manufacturer to be improved in order to reduce radiation exposure. For chest CT, scan parameters included peak kilovoltage (kVp) of 120; tube current was set according to manufacturer recommendations to maintain image quality. ECG gating was not used, since ECG gating is not the standard of care for chest CT scans. “High pitch” CT was at a maximum pitch of 3.0 for a field of view of 35.4 cm or smaller (in accordance with manufacturer recommendations). The field of view was chosen by the operator based on clinical indication and independent of pitch considerations. If a FOV > 35.4 cm was selected by the operator, the pitch was automatically reduced by the scanner software to enable the specified FOV (this limitation is due to different detector sizes of the dual source system). Intravenous contrast injection without bolus tracking was used (Iopamidol 300 mg/ml [Isovue, Bracco Diagnostics, Melville, NY], 120–130 ml, 2 ml/sec, 70 sec scan delay).
2.3. Image reconstruction
Images were reconstructed for 2 mm axial thickness and 512×512 in-plane resolution. In addition, thin slices at 0.5 mm were reconstructed for high pitch examinations in order to specifically address coronary artery visualization. Reconstruction kernel was B43f (body kernel) for studies on the Somatom Flash, Br40 (body kernel) for the Somatom Force 2 mm slices and Bv36 (vessel kernel) for 0.5 mm slices. A slice overlap of 50% was used for all reconstructions. For iterative reconstruction, Safire level 2 was used in the Somatom Force and in the Somatom Flash. The maximum field of view available was reconstructed.
2.4. Image Analysis
All scans were fully anonymized using commercially available software (DICOMAnonymizer Pro, Neologica, Italy). Readers were blinded to clinical indication and scan parameters. Datasets were presented in random order. For the mediastinum and heart, two radiologist readers (M.A. and E.J., 8 and >15 years of experience in CT imaging) assessed CT image quality using a 5 point rating scale (5 = excellent and 1 = non-evaluable) as displayed on a DICOM viewer (Radiant, Medixant, Poland). For each structure of interest, readers where given samples of image quality (data supplement, figure 1) in order to standardize image quality readings. For coronary artery images, two cardiologist readers (V.S. and M.C with 5 and 11 years of experience in cardiac CT imaging) scored images using a 4 point scale described previously 8 (4 = excellent and 1 = non-evaluable) using a cardiac CT workstation (Vitrea Software, Vital imaging, MN). Assessment of the coronary segment involvement score (SIS) was performed on blinded axial 2 mm slices by a cardiologist reader (V.S) using the SCCT segment model 9. Image noise was measured as the standard deviation of CT Hounsfield units as previously described 10 using ImageJ software (NIH, Bethesda) 11. Image noise was measured in regions of interest approximately 1 cm2 size in the trachea and left lung (avoiding branch vessels) at a level just above the aortic arch and on the level of the left ventricle in the anterior/posterior subcutaneous fat tissue and descending aorta.
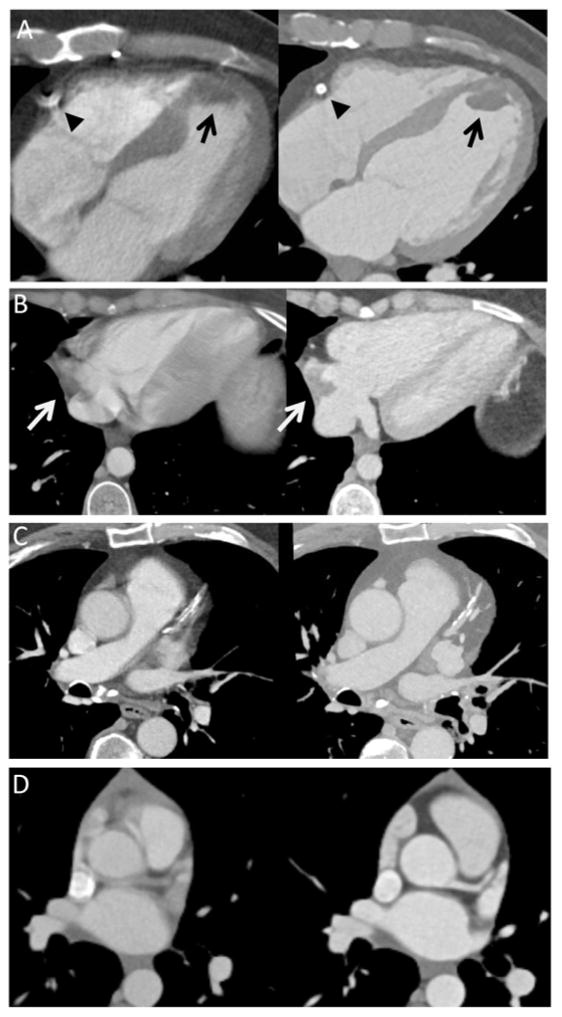
Figure 1. Examples of low pitch (left)/high pitch (right) comparisons.
A) 69 year old male referred for a staging CT (colorectal carcinoma). A left ventricular apical thrombus (black arrow) and myocardial thinning due to prior infarction was poorly visualized on the low-pitch CT scan (left) but was clearly seen on the high pitch scan (right). The right coronary artery stent is also clearly seen on the high pitch exam with no motion artifacts (arrow head).
B) 24 year old male reffered for staging/restaging of adrenocortical carcinoma. A mass is seen in the right atrium on the high pitch CT (right side, white arrow, likely catheter associated thrombus). In a low pitch CT this region cannot be reliably evaluated due to motion artifacts (left side).
C) 75 year old male referred for staging/restaging CT (prostate cancer). Plaque in LAD is seen. Significant motion artifacts are visible in the low pitch exam, while no motion artifacts are present in the high pitch exam (right).
D) 27 year old femal referred for staging of lymphoma. Motion/Pulsation artifacts impair visualisation of the aortic bulb and the LAD in the low pitch exam (left). No motion artifacts are present in the high pitch exam.
2.5. Statistical Methods
Median and IQR were calculated for quality scales. Cohen’s kappa and reader agreement was calculated to assess reproducibility of quality assessments. A paired Wilcoxon signed rank test was used for comparison of two groups. A Kruskal-Wallis test was performed for multiple group comparisons, followed by a pairwise Dunn test if applicable. Logistic regression was used to determine the relationship of quality score to patient and CT acquisition factors. All statistical analysis was performed using R Version 3.2.2 12.
3. Results
3.1. Study population and scan parameters
A total of 333 datasets from 111 patients were evaluated (111 low pitch scans and 111 paired high pitch scans at 2 mm slice thickness in addition to 111 high resolution (0.5 mm) reconstructions using high pitch mode). The median time interval between low pitch and high pitch CT was 70 days (IQR 49, 144.5). The majority of patients underwent chest CT for evaluation of oncologic disease (97.3%, 108/111, Table 1). The median body mass index was 26.64 kg/m2 (IQR 23.67, 31.02) and 57% (63/111) of the patients were male. The median age was 56 years (IQR 46, 63).
Table 1.
Indications for CT of the chest, abdomen and pelvis
| Diagnosis Category | N (%) |
|---|---|
| Lymphoma/Leukemia | 17 (15.3 %) |
| Malignancy of | |
| Prostate | 15 (13.5%) |
| Kidney | 11 (9.9%) |
| Skin | 10 (9%) |
| Ovary | 9 (8.1%) |
| Lung | 8 (7.2%) |
| Gastrointestinal | 7 (6.3%) |
| Thyroid | 7 (6.3%) |
| Breast | 6 (5.4%) |
| Genitourinary (other) | 5 (4.5%) |
| Bladder | 4 (3.6%) |
| Extremity | 2 (1.8%) |
| Other | 7 (6.3%) |
| Infection | 2 (1.8%) |
| Other | 1 (0.9%) |
CT scan parameters are shown in table 2. The median pitch in the high pitch exams was 2.3. There was no significant difference in heart rate between the high and low pitch groups (79.5 vs. 78.5 beats per min). The contrast enhancement in the ascending aorta was higher in the high pitch group (229 vs. 205 HU, p=0.0036).
Table 2.
Scan related parameters. 111 patients had both low and high pitch CT scans with a median time interval between low pitch and high pitch scans of 70 days (IQR 49, 144.5). Median and interquartile ranges are shown. (n.s. not significant, p>0.05)
| Variable | Low pitch | High pitch | P-value |
|---|---|---|---|
| N | 111 patients | 111 patients | |
| Pitch | 0.8 (0.8,0.8) | 2.34 (2.05, 2.65) | <0.001 |
| kVp | 120 (120,120) | 120 (120, 120) | n.s. |
| CTDIvol (mgy) | 12.4 (9.7,15.2) | 10.83 (8.6, 13.0) | <0.001 |
| DLP (mgy cm) | 827 (668,1064) | 790 (600.5,950) | 0.0012 |
| Heart rate | 79.5 (70, 90) | 78.5 (71, 88) | n.s. |
| Aortic HU | 205 (178, 236) | 229 (184, 257) | 0.0036 |
3.2. Quality comparison
3.2.1. Cardiovascular structures overview
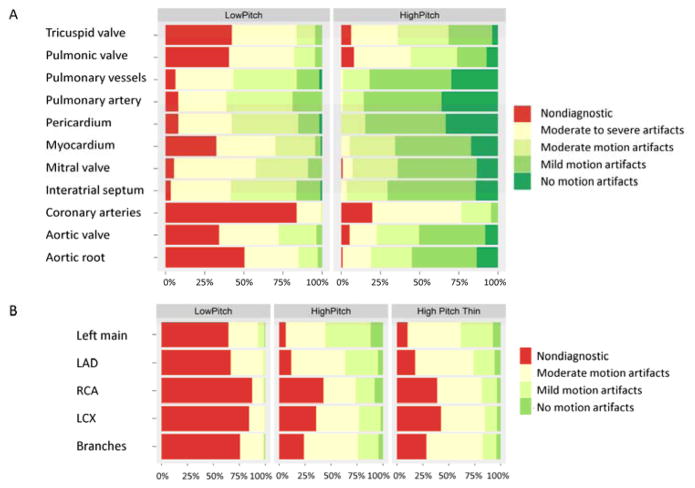
Image quality scores are shown in table 3 for the low and pitch groups. All cardiac and mediastinal quality scores were superior for high pitch exams compared with low pitch exams (p < 0.001). Clinically relevant structures including aortic root, pulmonary artery and branches, myocardium and pericardium showed large improvements in image quality due to reduction of motion artifacts (clinical examples shown in figure 1).
Table 3.
Evaluation of scan quality parameters: High and low pitch body CT scans for 111 patients. Significance of group differences was calculated with Wilcoxon signed rank sum test (paired).
| Variable | Low pitch median (IQR) | High pitch median (IQR) | P-value (paired) |
|---|---|---|---|
| Aortic valve quality | 2 (1,3) | 4 (3,4) | <0.0001 |
| Pulmonic valve quality | 2 (1,2) | 3 (2,4) | <0.0001 |
| Mitral valve quality | 2 (2,3) | 4 (3,4) | <0.0001 |
| Tricuspid valve quality | 2 (1,2) | 3 (2,4) | <0.0001 |
| Aortic root quality | 1 (1,2) | 4 (3,4) | <0.0001 |
| Pulmonary artery quality | 3 (2,3) | 4 (4,5) | <0.0001 |
| Interatrial septum quality | 3 (2,3) | 4 (3,4) | <0.0001 |
| Myocardium quality | 2 (1,3) | 4 (3,4) | <0.0001 |
| Pericardial quality | 3 (2,3) | 4 (4,5) | <0.0001 |
| Pulmonary vessels quality | 3 (2,3) | 4 (4,5) | <0.0001 |
| Coronary artery quality | 1 (1,1) | 2 (2,2.5) | <0.0001 |
| Number of coronary segments | 11 (11,11) | 12 (11,13) | <0.0001 |
| Number of diagnostic coronary segments | 2 (0,4) | 9 (6.5,12) | <0.0001 |
In multivariable analysis (adjusted for pitch category, age, gender, body mass index, heart rate, and aortic enhancement), high pitch CT and degree of vascular enhancement were associated with higher image quality scores (score > 50th percentile, table 4; O.R. 57, 95% CI 22–148, reference, low pitch CT, p < 0.001; O.R. 9.4, 95% CI 3.3 – 27, reference less than or equal to median vascular enhancement, p < 0.001, respectively.)
Table 4.
Multivariable analysis to determine the relationship between CT scan parameters and demographic factors associated with average image quality score (average of 11 features, see figure 2A) above the median (reference, image quality score at or below the median. 222 paired exams were included).
| Paired CT scans (n = 222) | ||
|---|---|---|
|
| ||
| Odds ratio | p | |
| Exam Type | ||
| Low Pitch | 1 (reference) | |
| High Pitch | 56.83 (21.7, 148.8) | <0.001 |
|
| ||
| Age | ||
| Age ≤ Median | 1 (reference) | |
| Age > Median | 1.27 (0.48, 3.38) | 0.635 |
|
| ||
| BMI | ||
| BMI ≤ Median | 1 (reference) | |
| BMI > Median | 0.45 (0.17, 1.17) | 0.103 |
|
| ||
| Sex | ||
| Women | 1 (reference) | |
| Men | 2.46 (0.98, 6.19) | 0.056 |
|
| ||
| Heart rate | ||
| HR ≤ Median | 1 (reference) | |
| HR > Median | 0.34(0.1, 1.09) | 0.07 |
|
| ||
| Aortic enhancement | ||
| > Median | 1 (reference) | |
| ≤ Median | 9.38 (3.29, 26.75) | <0.001 |
3.2.2. Coronary arteries
The quality of coronary artery visualization was assessed by two cardiologist readers using axial images with 2 mm slice thickness in low and high pitch chest CTs. In addition, 0.5 mm slice thickness datasets were reconstructed for the high pitch acquisitions to assess suitability for coronary artery 3D visualization. In total, 3862 coronary segments were scored for image quality (median of 12 coronary segments per exam). For 2 mm slice thickness reconstruction, the median number of coronary segments ranked as diagnostically evaluable by readers was 2 per patient for the low pitch scans (IQR 0, 4) and 9 segments per patient for the high pitch exams (IQR 6.5, 12) (p<0.0001). For 0.5 mm reconstructions in high pitch CT using a dedicated coronary artery visualization software, a median of 9 coronary segments was diagnostically evaluable (IQR 5.8, 12, p<0.0001).
Quality scores by coronary vessel are shown in figure 2B. The left main coronary artery had the greatest percentage of CT scans rated as evaluable (score ≥2) (90 and 94% evaluable for high pitch 2mm and high pitch 0.5 mm scans, respectively, vs. 35 % for low pitch exams, figure 3B). The left anterior descending coronary artery had the second highest percentage of evaluable segments (88 % and 82 % in the high pitch groups vs. 33 % in the low pitch group). The lowest quality scores were seen in the left circumflex and right coronary arteries mainly due to motion artifacts. Overlap with nearby venous signal was rarely the reason for a low quality score (18 segments).
Figure 2. Image quality scores for cardiac and mediastinal structures for 111 patients with both low and high pitch CT examinations.
A (top): Graph showing the distribution of the quality scores (1 lowest quality, 5 highest quality) by radiology readers. High pitch exams resulted in higher quality scores for all cardiovascular structures (p<0.001).
B (bottom): Graph showing the distribution of quality scores (1 nondiagnostic, 4 highest quality) by cardiology readers. Image quality was determined with both low pitch chest CT and high pitch CT with 2 mm slice thickness. In addition, 0.5 mm slice reconstructions of high pitch CT scans (labeled as “High Pitch Thin”) were evaluated on a dedicated coronary artery workstation. Higher quality of high pitch exams is seen in all vessels (p<0.001). The left main and left anterior descending coronary arteries showed the best overall image quality. (LAD: left anterior descending, RCA: Right coronary artery, LCX: Left circumflex artery, Branches: Any branch vessel originating from LAD, LCX or RCA).
Figure 3. Assessment of diagnostically evaluable (image quality score ≥2) coronary arteries by segment.
A: Number of evaluable coronary segments by exam type (low pitch 2 mm, high pitch 2 mm slice thickness, high pitch 0.5 mm slice thickness).
B: The percentage of a coronary segment being evaluable (score ≥ 2) in a certain vessel (see legend) is shown for each exam type. More than 80 % of left main coronary artery (black) and left anterior descending (dark grey) segments are evaluable for disease.
Evidence of coronary artery disease was seen more frequently in high pitch compared to low pitch CT examinations (53/111 (48%) vs. 46/111 (41%), respectively, figure 4A). The segment involvement score per patient was higher in the high pitch scans compared with low pitch exams (paired Wilcoxon test, p<0.0001, figure 4B).
Figure 4.
A: Coronary artery disease was identified in a numerically higher number of patients using high-pitch scans compared to low-pitch scans (53/111 vs. 46/111 respectively).
B: The segment involvement score (number of segments with evidence of coronary artery disease) was significantly higher in high-pitch exams compared with low-pitch exams (only data of patients with any coronary disease is plotted).
3.2.3. Image Noise and Radiation Dose
Radiation exposure was lower in the high pitch group compared with the low pitch group (median CTDIvol 10.83 vs. 12.36 mGy and DLP 790 vs. 827 mGy cm respectively, p <0.01 for both). There was no significant difference in regard to image noise (1110 regions of interest [222 exams x 5 regions], p= 0.58, paired comparison accounting for within patient clustering of multiple measurements).
3.3. Reproducibility
Intra-reader reproducibility was evaluated in 22 patients and was excellent (Cohen’s kappa 0.88, agreement within one scoring grade: 98.8%). Inter-reader reproducibility was evaluated in 59 patients and was good to excellent (Cohen’s kappa of 0.79, agreement within one scoring grade: 94.9%).
4. Discussion
Incidental coronary and cardiac findings on CT scanning may have direct implications for patient care. In this study, we evaluated visualization of cardiovascular features on non-gated chest CT scans (mostly performed for oncologic disease) using rapid, third generation dual-source CT technology. New CT scans can evaluate the entire chest in less than 1 second with isotropic 0.5 mm slice thickness using high pitch (>2) mode. We observed high image quality for coronary vessels, myocardium, aorta and pulmonary arteries at similar or lower radiation doses compared to prior generation, low pitch (≤1) CT scans. In multivariable analysis, the most important factor that resulted in improved cardiac image quality was high-pitch scan mode. Importantly, coronary arteries anatomy was often “incidentally” visualized (e.g. diagnostic assessment of the left anterior descending coronary artery was feasible in more than 80% of cases (figure 2)). High image quality translated into identification of more segments with coronary artery disease in high pitch compared to low pitch CT exams (figure 4). These results raise the question of whether radiologists and/ or cardiologists should routinely evaluate the heart on CTs obtained for non-cardiac reasons. Nongated CT scans are standard for oncologic and infectious disease applications of chest CT. ECG gating improves image quality and reduces motion artifacts, but requires additional time for patient preparation. Motion artifacts in the mediastinum can be severe for conventional, non-gated CT, but radiologists have learned to avoid interpreting regions of the mediastinum with motion artifact. However, motion artifact at the aortic root and ascending aorta are known to be a potential source of false positive diagnosis for aortic dissection 13. In this study, experienced radiologists and cardiologists blinded to CT scanner type found significantly improved image quality on 3rd generation compared to 2nd generation CT (figure 2a). In an emergency setting, availability of a reliable non-gated CT protocol would reduce technologist set-up time and simplify CT scan procedures while providing good visualization of vascular structures.
Incidental cardiac findings tend to be underreported by radiologists 14, 15 despite the potential to provide relevant prognostic information 16, 17. With conventional chest CT, coronary artery evaluation is usually not relevant due to obvious and marked motion artifacts. The results of the current study may provide new motivation for assessment of cardiac structures.
Besides better visualization of the great vessels and pulmonary arteries, we observed incidental coronary artery visualization in a high percentage of patient examinations. In multivariable analysis, high pitch scan mode and high vascular contrast attenuation were both strong predictors of a high image quality score. We had anticipated that relatively low intravascular contrast levels used with routine body CT (injection rate, 2 ml/sec) would be problematic for assessment of the coronary arteries, since high injection rate protocols are used for dedicated coronary CT angiography (4–5 ml/sec). This assumption was often incorrect – we observed adequate visualization of the left main and left anterior descending coronary artery in 90 and 88 % of cases, respectively, with high pitch CT. In retrospect, this may be understood by considering that vascular enhancement sufficient for aortic visualization is apparently also adequate for the coronary arteries in the absence of motion artifacts. Dual energy or spectral CT is increasingly used; when implemented in high-pitch mode, that technology may ultimately provide further improvements in vascular signal 18.
A prior report on high pitch CT also noted lack of motion artifacts in pulmonary vessels and improved quality in coronary vessels 19 in select patients using high iodine contrast injection rates (4 ml/ sec). In comparison, we used a moderate injection rate (2 ml/sec) and evaluated consecutive patient studies without exclusion of patients with high body mass index or high heart rate. Since we evaluated consecutive patients, our results are likely to be applicable to a wide range of patients referred for CT scan of the chest.
Prior results have shown good correlation of the calcium score on non-gated CT compared to dedicated ECG gated calcium CT scoring 2, 20. Although a high calcium score is predictive of coronary artery disease, the calcium score is understood as a marker of disease, rather than direct visualization of coronary stenosis. We observed that contrast enhanced high-pitch CT provided frequent and direct visualization of coronary vessels as well as cardiac structures. In addition, high-pitch CT identified more segments with coronary artery disease than low-pitch CT. A limitation of our findings is that the phase of the cardiac cycle is unknown on non-gated CT. Thus, cardiac parameters such as myocardial wall thickness and LV diameter assessment cannot be accurately assessed at end-diastole. In the future, software revisions could allow simultaneous recording of ECG tracing as well as image data.
Increasingly improved visualization of cardiac structures with new generations of CT scanners may require additional consideration of workflow and clinical relevance of incidental findings. For example, coronary artery reconstruction at 0.5 mm slice thickness provides about 500 additional images for interpretation. For 50 to 100 CT scans per CT device per day, the transmission and interpretation of all image data may not be practically feasible. Information may also be provided by CT (i.e. coronary stenosis) that is irrelevant to the clinical question (e.g., progression of tumor). It seems likely that most of these issues would ultimately be handled by practice guidelines similar to Fleischner society guidelines 21 for incidental pulmonary nodules. However as opposed to pulmonary nodule evaluation, effective and cost effective treatment strategies for many cardiovascular diseases are known 22. A study of non-contrast chest CT found that the cost of imaging follow up of cardiac abnormalities was only 4% of all incidental finding related costs 23. Improved management of incidental cardiac findings may include education of referrers and radiologists, inclusion of cardiologists in interpretation and discussion of treatment plans 24. In our practice, we currently perform 0.5 mm reconstructions for all high pitch CT scans. These images are archived without prospective review. When needed, these additional reconstructions are readily retrieved from the PACS system to clarify standard chest reconstructions.
Limitations
In this study, the low pitch CT scan was always performed prior to high pitch CT (median interval of 70 days). This could introduce an unknown bias in our evaluation despite blinding of cardiology and radiology readers. In addition, experienced readers may recognize the scanner type even in blinded datasets. Image quality scores are difficult to standardize, but we found reproducibility of cardiology and radiology readers to be high. Also, similar to other studies of incidental CT findings 25, we did not evaluate the clinical impact of improved image quality. There was no gold standard for the cardiac abnormalities available (e.g. invasive angiography), thus the possibility of false positive cardiac findings from high pitch CT must be considered. The third generation CT scanner had improved iterative reconstruction technique stated by the manufacturer to reduce image noise. Routine use of ECG gating would likely further improve image quality but that approach is not the current standard of care.
5. Conclusion
Cardiovascular structures are often visualized with high quality and minimal motion artifacts on non-gated routine chest imaging using high pitch scanning mode. This provides a large and previously under-utilized opportunity to diagnose clinically unsuspected cardiovascular disease. Radiologists and cardiologists should be aware of the increased clarity of findings in and around the heart when interpreting chest images using high pitch CT. Future studies are needed to determine if incidental detection of coronary artery disease and other cardiac abnormalities would be cost effective and improve patient outcomes.
Acknowledgments
Funding was provided by the NIH intramural program.
Abbreviations
- IQR
Interquartile Range
- CAD
Coronary Artery Disease
- DLP
Dose Length Product
- CTDIvol
CT Dose Index (Volume)
- CI
Confidence Interval
- HU
Hounsfield Units
- IRB
Institutional Review Board
Footnotes
No conflicts of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation. 2009;120:867–875. doi: 10.1161/CIRCULATIONAHA.109.859280. [DOI] [PubMed] [Google Scholar]
- 2.Hughes-Austin JM, Dominguez A, III, Allison MA, et al. Relationship of Coronary Calcium on Standard Chest CT Scans With Mortality. JACC: Cardiovascular Imaging. 2016 doi: 10.1016/j.jcmg.2015.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 4.Goehler A, McMahon PM, Lumish HS, et al. Cost-effectiveness of follow-up of pulmonary nodules incidentally detected on cardiac computed tomographic angiography in patients with suspected coronary artery disease. Circulation. 2014;130:668–675. doi: 10.1161/CIRCULATIONAHA.113.007306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flohr TG, Leng S, Yu L, et al. Dual-source spiral CT with pitch up to 3.2 and 75 ms temporal resolution: image reconstruction and assessment of image quality. Medical physics. 2009;36:5641–5653. doi: 10.1118/1.3259739. [DOI] [PubMed] [Google Scholar]
- 6.Lembcke A, Schwenke C, Hein PA, et al. High-pitch dual-source CT coronary angiography with low volumes of contrast medium. Eur Radiol. 2014;24:120–127. doi: 10.1007/s00330-013-2988-6. [DOI] [PubMed] [Google Scholar]
- 7.Silverman PM, Kalender WA, Hazle JD. Common terminology for single and multislice helical CT. AJR Am J Roentgenol. 2001;176:1135–1136. doi: 10.2214/ajr.176.5.1761135. [DOI] [PubMed] [Google Scholar]
- 8.Chen MY, Steigner ML, Leung SW, et al. Simulated 50 % radiation dose reduction in coronary CT angiography using adaptive iterative dose reduction in three-dimensions (AIDR3D) The international journal of cardiovascular imaging. 2013;29:1167–1175. doi: 10.1007/s10554-013-0190-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raff GL, Abidov A, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. Journal of cardiovascular computed tomography. 2009;3:122–136. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Guimarães LS, Fletcher JG, Harmsen WS, et al. Appropriate Patient Selection at Abdominal Dual- Energy CT Using 80 kV: Relationship between Patient Size, Image Noise, and Image Quality. Radiology. 2010;257:732–742. doi: 10.1148/radiol.10092016. [DOI] [PubMed] [Google Scholar]
- 11.Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; 2015. [Google Scholar]
- 13.Batra P, Bigoni B, Manning J, et al. Pitfalls in the Diagnosis of Thoracic Aortic Dissection at CT Angiography. RadioGraphics. 2000;20:309–320. doi: 10.1148/radiographics.20.2.g00mc04309. [DOI] [PubMed] [Google Scholar]
- 14.Winkler MA, Hobbs SB, Charnigo RJ, et al. Identification of Coronary Artery Calcification and Diagnosis of Coronary Artery Disease by Abdominal CT: A Resident Education Continuous Quality Improvement Project. Acad Radiol. 2015;22:704–707. doi: 10.1016/j.acra.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sverzellati N, Arcadi T, Salvolini L, et al. Under-reporting of cardiovascular findings on chest CT. Radiol Med. 2015 doi: 10.1007/s11547-015-0595-0. [DOI] [PubMed] [Google Scholar]
- 16.Jairam PM, Gondrie MJ, Grobbee DE, Mali WP, Jacobs PC, van der Graaf Y. Incidental imaging findings from routine chest CT used to identify subjects at high risk of future cardiovascular events. Radiology. 2014;272:700–708. doi: 10.1148/radiol.14132211. [DOI] [PubMed] [Google Scholar]
- 17.Gondrie MJ, van der Graaf Y, Jacobs PC, Oen AL, Mali WP. The association of incidentally detected heart valve calcification with future cardiovascular events. Eur Radiol. 2011;21:963–973. doi: 10.1007/s00330-010-1995-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apfaltrer P, Sudarski S, Schneider D, et al. Value of monoenergetic low-kV dual energy CT datasets for improved image quality of CT pulmonary angiography. Eur J Radiol. 2014;83:322–328. doi: 10.1016/j.ejrad.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 19.de Malherbe M, Duhamel A, Tacelli N, et al. Ultrafast imaging of the entire chest without ECG synchronisation or beta-blockade: to what extent can we analyse the coronary arteries? Insights Imaging. 2012;3:73–79. doi: 10.1007/s13244-011-0133-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hutt A, Duhamel A, Deken V, et al. Coronary calcium screening with dual-source CT: reliability of ungated, high-pitch chest CT in comparison with dedicated calcium-scoring CT. Eur Radiol. 2015 doi: 10.1007/s00330-015-3978-7. [DOI] [PubMed] [Google Scholar]
- 21.MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395–400. doi: 10.1148/radiol.2372041887. [DOI] [PubMed] [Google Scholar]
- 22.Bluemke DA. Coronary computed tomographic angiography and incidental pulmonary nodules. Circulation. 2014;130:634–637. doi: 10.1161/CIRCULATIONAHA.114.011634. [DOI] [PubMed] [Google Scholar]
- 23.Kucharczyk MJ, Menezes RJ, McGregor A, Paul NS, Roberts HC. Assessing the impact of incidental findings in a lung cancer screening study by using low-dose computed tomography. Can Assoc Radiol J. 2011;62:141–145. doi: 10.1016/j.carj.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Hecht HS. “See No Evil”*. JACC: Cardiovascular Imaging. 2016 doi: 10.1016/j.jcmg.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 25.Lumbreras B, Gonzalez-Alvarez I, Lorente MF, Calbo J, Aranaz J, Hernandez-Aguado I. Unexpected findings at imaging: predicting frequency in various types of studies. Eur J Radiol. 2010;74:269–274. doi: 10.1016/j.ejrad.2009.01.029. [DOI] [PubMed] [Google Scholar]