Abstract
Objective
To assess the cost-effectiveness of the 6-month Team Education and Adherence Monitoring (TEAM) intervention for black patients with hypertension in community pharmacies using prospectively collected cost data.
Design
Cost-effectiveness analysis of a cluster-randomized trial.
Setting
28 chain pharmacies in five Wisconsin cities from December 2006 to February 2009.
Participants
576 black patients with uncontrolled hypertension
Intervention
Pharmacists and pharmacy technicians using novel tools for improving adherence and feedback to patients and physicians as compared to information only control group.
Main outcome measure(s)
Incremental cost analysis of variable costs from the pharmacy perspective captured prospectively at the participant level. Outcomes (effect measures) were 6-month refill adherence, changes in SBP and DBP, and proportion of patients achieving BP control.
Results
Mean cost of intervention personnel time and tools was $104.8± 45.2. Incremental variable costs per mmHg decrease in SBP and DBP were $22.2 ± 16.3 and $66.0 ± 228.4, respectively. The cost of helping one more person achieve the BP goal (< 140/90) was $665.2 ± 265.2; the cost of helping one more person achieve good refill adherence was $463.3 ± 110.7. Prescription drug costs were higher for the TEAM group ($392.8, SD = 396.3 versus $307.0, SD = 295.2, p = 0.02). The start-up cost for pharmacy furniture, equipment, and privacy screen was $168 per pharmacy.
Conclusions
Our randomized, practice based intervention demonstrated that community pharmacists can implement a cost-effective intervention to improve hypertension control in blacks. This approach imposes a nominal expense at the pharmacy level, can be integrated into the ongoing pharmacist-patient relationship, and can enhance clinical and behavioral outcomes.
Keywords: hypertension, pharmacists, cost-effectiveness, black patients
Introduction
Despite the benefits of antihypertensive drug therapy (AHT), poor adherence to AHT is a common and serious problem in the US and worldwide1. Studies show that nearly 50% of newly diagnosed patients discontinue their AHT within 6–12 months2, 20–80% of established patients have poor medication refill adherence3–6, and that poor refill adherence is associated with a higher risk of cardiovascular events, stroke-related hospitalization, and death in treated hypertension patients3,6–8. Studies also show significant and persistent racial differences in adherence to AHT, with black patients reporting more barriers to adherence and showing lower rates of refill adherence and blood pressure (BP) control -- even in subgroups with good drug benefits and access to care4,5,9,10. Thus, improving antihypertensive medication adherence in black patients could have important public health implications and ultimately improve the outcomes of care for blacks who suffer disproportionately from hypertension and experience poorer cardiovascular outcomes than whites11,12.
Past studies show that team-based interventions involving clinical pharmacists or nurse managers are the most potent methods of improving BP control13–16. However, many team studies have failed to produce significant and sustained improvements in medication adherence15,16. Studies rarely assess intervention costs17–19 or the effectiveness of team interventions in blacks20. In addition, there are concerns about the barriers to implementing team interventions on a large-scale basis. These barriers to implementation include: reliance on complex protocols, leading to poor patient fidelity and retention;20 reliance on expensive software and equipment for home BP telemonitoring, limiting applicability to everyday practice21; reliance on home computers and Web communication, excluding many minority and low income patients22; and reliance on labor-intensive methods, leading to increased pharmacist or nurse time costs23,24. Higher priority must be placed on the design of relatively simple protocols and tools that can be implemented widely.
Objective
To address these issues, we conducted a 28-pharmacy, cluster-randomized trial that was funded by the National Heart, Lung, and Blood Institute to improve hypertension control in black patients25. The primary objective was to assess the effectiveness and sustainability of a relatively simple protocol that involved community pharmacists, pharmacy technicians, and novel tools for improving medication adherence, systolic/diastolic BP, and BP control in black patients with treated but uncontrolled hypertension. We designed the TEAM protocol and tools for community pharmacists because they: are conveniently located or accessible to most patients, have good drug knowledge and refill records, have an opportunity for regular and sustainable contact with patients when they return for refills, and already work with pharmacy technicians who could assist pharmacists in patient outreach, scheduling, collecting data, and other tasks. Compared with the control group, patients in the TEAM group achieved significant improvements in refill adherence, systolic/diastolic BP, and BP control at six months and showed sustained improvements in refill adherence and systolic BP six months after intervention discontinuation26. The present study extends our findings by examining a secondary objective of the TEAM trial, which was to evaluate the cost-effectiveness of the TEAM intervention using prospectively collected data on intervention costs and changes in refill medication adherence, systolic/diastolic BP, and BP control.
Methods
Original Study Design
We prospectively designed and conducted a cost-effectiveness analysis for a cluster randomized trial of community chain pharmacists’ intervention for improving hypertension control. The methods and primary results of that trial have been published elsewhere25,26. Briefly, we enrolled 576 hypertensive Blacks in the Team Education and Adherence Monitoring (TEAM) trial at 28 chain pharmacies: pharmacies were cluster-randomized to a 6-month TEAM program versus usual care patient information (control group). The TEAM intervention involved community pharmacists, pharmacy technicians, and new tools for improving medication adherence and giving feedback to patients and physicians. Primary outcomes at 6 months included refill adherence, changes in SBP and DBP, and proportion of patients achieving blood pressure control (SBP < 140 and DBP <90 mmHg.
Study patients were self-identified black patients with uncontrolled hypertension (SBP>= 140 and DBP >=90 mmHg based on mean of 2nd and 3rd readings) who took at least one antihypertensive medication and completed a free blood pressure screening at their pharmacy. Blood pressure measurements were conducted by blinded project assistants using a standardizd protocol and an automatic monitor (Microlife Model 3AA1-2; Microlife, Clearwater, FL). Patients were enrolled from December 2006–August 2007. Additional inclusion criteria were age 18 years or older, receipt of all blood pressure medications from the pharmacy chain, able to read, and able to return for six visits. Individual with the following characteristics were excluded: BP values greater than 210/115 mmHg, receiving renal replacement therapy, liver disease, organ transplant, serious memory loss, terminal illness, pregnancy, alcohol/substance use problem, heart failure symptoms, arm circumference greater than 16.5 inches, physician exclusion request, or employment at the pharmacy. For the analyses presented here, we included only TEAM subjects who completed their initial pharmacist visit, and subjects from both arms who had valid blood pressure outcomes measured.
Pharmacy sites included 28 community pharmacies owned by Walgreens or Aurora Pharmacy in five Wisconsin cities. All pharmacies completed the study although four pharmacists had to be replaced because of transfers or medical leaves. Randomization of the pharmacy was concealed from patients until all patients completed the enrollment process at their site.
Control group
The control condition involved usual care with patient information only. Patients received a 14-page guide for lowering blood pressure, a pamphlet about hypertension in black patients, cards showing their blood pressure at baseline and follow-up interviews, and instructions to seek immediate care if their blood pressure exceeded 210/115 mmHg at a follow-up visit. Their primary care providers and pharmacists received a reference card with current treatment guidelines but no special training or tools.
TEAM intervention group
The active intervention patients received the same patient information provided to the control group. In addition, they were invited to complete a series of pharmacist visits (initial with five follow-up visits) based upon the Health Collaboration Model and several unique toolkits designed for this study and detailed elsewhere25. The TEAM tools included Brief Medication Questionnaires (BMQs) and other easy-to-use patient self-report screening tools to identify and assess barriers to adherence. These “pre-visit” tools were completed while waiting to meet with the pharmacist at each visit. Other TEAM tools used by pharmacists included: simple algorithms for the pharmacist to address self-reported barriers, checklists to document and track barriers and interventions, a structured tool to fax requests for medication review and feedback to physicians as needed, and a patient take-home toolkit. Pharmacists distributed and used the patient’s take-home toolkit for improving patient involvement and their use of a wallet card for recording blood pressure readings, a 7-day medication box for remembering doses, easy to read leaflets to improve awareness about managing blood pressure, and a pedometer. The tools were designed to facilitate communication and save staff and patient time for initial and follow-up visits. Intervention teams filed copies of all intervention tools used during the initial and follow-up visits, allowing a research team member to track the cost of all TEAM tools actually used during the 6-month intervention.
Fixed costs for TEAM training and creation of a BP counseling station
Before starting the program, investigators provided 8 hours of TEAM training for one pharmacist and one pharmacy technician per pharmacy (1 hour self-study, 7 hours joint workshop). Pharmacy technicians were trained to assist the pharmacists in making and confirming appointments, setting up a semi-private BP counseling station, measuring BPs, and collecting “pre-visit” tools that were completed by patients before they met with their pharmacist. Pharmacists were trained to utilize the new tools for more rapid and effective management of particular barriers to medication adherence and blood pressure control.
Investigators also provided each TEAM pharmacy with furniture and equipment for creating one semi-private BP counseling station costing a total of $168 for a folding table and two chairs, a validated BP monitor and cuffs, a privacy screen, an appointment book, and supplies. As these items were provided at one time and used regardless of the number of patients, they were considered fixed costs.
Assessment of intervention costs
We examined the cost-effectiveness of the TEAM approach to hypertension control using a prospective, micro-costing approach from a community pharmacy provider perspective. We considered costs directly generated by the intervention18,19,27, 28. We identified the incremental variable costs associated with all initial and follow-up TEAM visits, including: pharmacy personnel time and TEAM tools used for assessing and tracking adherence barriers and interventions at each visit, tools for providing feedback and requests to other providers, and patient take-home toolkits. Since the intervention took place over 6 months, we did not apply any discounting, and costs were valued and reported in 2007 dollars to reflect the time period of project enrollment.
Since the TEAM intervention was delivered by patients’ regular pharmacists and pharmacy technicians, the main intervention cost input was the personnel time devoted to interacting with patients. The pharmacist’s activities depended upon the type of visit, though all visits involved a review of patient data and interaction with the patient. At the initial visit, there was a pharmacist-patient discussion of the patient’s BP readings and history, patient-reported adherence and barriers to adherence, lifestyle issues and patient goals, options for reducing any barriers to adherence and BP control, and encouragement to use the patient toolkit. At follow-up visits, the pharmacist met with the patient to monitor progress and concerns, reinforce adherence, and support behavioral changes. Pharmacists recorded their time (in minutes) at the conclusion of each visit. Pharmacists also filed a copy of any request forms faxed to the patient’s physician as needed, and we assumed 10 minutes for preparing and sending each provider request form. We summed the total pharmacist time for communicating with patients and providers and assigned valuation at the patient level.
In lieu of asking pharmacy technicians to record their time interacting with patients, we estimated 30 minutes of pharmacy technician time per completed visit. We estimated after direct observation of a series of visits. Pharmacy technicians performed various activities before and after visits: calling and reminding patients, printing prescription profiles, setting up table and chairs, using an automatic monitor to measure BPs, and administering patient self-report tools. There was one pharmacy that did not utilize their technician due to scheduling issues: for this site, we excluded technician time since the pharmacist’s time included these tasks in their reporting.
Pharmacists’ and pharmacy technicians’ time were valued at Wisconsin’s mean hourly wage rates using the National Occupational Employment and Wage Estimates 2007 from the US Bureau of Labor statistics (www.bls.gov/oes/2007/may/oes_wit.htm#b29-0000 accessed 7/27/2010). Wisconsin pharmacist mean hourly wages were $49.48 in 2007 ($47.58 for national rate), and technicians earned $13.01 per hour, slightly less than the national mean ($13.25).
The patient take-home toolkits (5 TEAM leaflets, wallet card, pill box, pedometer, folder, and envelope) were valued at their procurement or reproduction costs and assessed at the patient level based on completed visits (Table 1). These initial visit packets totaled $9.62. We also tracked the reproduction costs for all paper-and-pencil tools used to assess and track adherence barriers, interventions, and provider requests. These visit level costs were assessed per completed visit at the patient level.
Table 1.
Baseline characteristics of patients included in the cost analysis, by study group
| Control No. (%) |
TEAM intervention No. (%) |
|
|---|---|---|
| Number of cases | 287 (100) | 207 (100) |
| Women | 194 (67.6) | 129 (62.3) |
| Age (years), mean ± SD | 52.8 ± 11.9 | 54.1 ± 10.5 |
| < 12 years education | 87 (30.3) | 49 (23.7) |
| Household income <$20,000/year | 145 (50.5) | 94 (45.4) |
| Unemployed | 170 (60.5) | 119 (57.8) |
| Medicaid eligible | 60 (21.1) | 43 (20.8) |
| Diabetes | 64 (22.3) | 51 (24.6) |
| Smoker | 107 (37.4) | 73 (35.6) |
| Alcoholic drinks/day, mean ± SD | 1.05 ± 1.46 | 0.80 ± 1.26 |
| Systolic BP (mmHg), mean± SD | 153.1 ± 16.6 | 151.2 ± 15.2 |
| Diastolic BP (mmHg), mean± SD | 92.9 ± 10.0 | 92.0 ± 10.1 |
| No. antihypertensive drugs currently used, mean ± SD | 1.77 ± 1.06 | 1.84 ± 1.03 |
| Reported ≥ 1 missed doses/previous week | 75 (26.1) | 51 (24.6) |
Abbreviations: TEAM, Team Education and Adherence Monitoring; SD, standard deviation. None of the between-Group differences was statistically significant (all p>0.05).
Assessment of clinical and behavioral outcomes
Intervention effectiveness was measured using three clinical outcomes: change in systolic blood pressure, change in diastolic blood pressure, and the proportion of study patients reaching BP control. Blood pressure was measured at the time of enrollment and at 6 months after enrollment. The 6-month BP measurement was compared to the baseline measurement to determine the change score. Achievement of BP control was defined as achieving a SBP <140 and DBP<90 mm Hg at 6 months. We compared the between-group difference in proportions with controlled BP as the effectiveness measure in the cost-effectiveness ratios. Effectiveness was also measured behaviorally as the proportion adherent with their antihypertensive agents during the 6-month intervention, based on refill records provided by each pharmacy chain. Refill dates and days supply per prescription were used to create a day-to-day data array for availability of at least one antihypertensive. The resulting proportion of days covered (PDC) reflected the proportion of days during the intervention period for which the patient had an antihypertensive drug supply. A threshold of 80% (PDC = 0.80) was used to define good refill adherence26.
Calculation of Incremental Cost Effectiveness Ratios (ICERs)
The cost-effectiveness analysis was conducted as an incremental analysis using a health system perspective. For all patients with available cost and outcomes data, we first tested for changes in SBP and DBP (unpaired t-test of means) and differences in effectiveness between the treatment arms at 6 months for proportion achieving blood pressure under 140/90 mmHg and the proportion achieving good refill adherence to antihyperternsive treatment based upon refill records (Fisher’s exact test). We applied bootstrapping (samples of 1,000/subject) to generate means, standard deviations, and 95% confidence intervals for cost and outcome measures. We proceeded with the examination of the incremental costs of the TEAM intervention relative to the control arm divided by the difference in effectiveness for each outcome.
Analysis of prescription drug costs and the use of other health care resources
It was beyond the scope of our study to assess changes in the cost of inpatient and outpatient medical care visits, but we prospectively tracked the number of patient self-reported hospitalizations, emergency department visits, visits to medical specialists, and visits to general physicians during the six month intervention. In addition, we retrospectively tracked the number and cost of antihypertensive medication prescriptions using electronic records provided by the pharmacy organizations at the person level. We applied product specific acquisition costs plus dispensing fees ($4.50/prescription) to prescriptions filled during the six month intervention. Acquisition costs were derived from the maximum allowable cost, where applicable, or a discount off average wholesale price (12% for brand name, single source agents, and 25% for generics) using the 2007 Drug Topics Red Book (Montvale, NJ). Unpaired t-tests were used to compare the TEAM versus control group patients. Data analyses were conducted using IBM SPSS Version 22. and Microsoft Excel 2010.
The University of Wisconsin–Madison Institutional Review Board approved all study-related procedures. The University of Kansas Human Subjects Committee approved all secondary analyses of trial data for this cost-effectiveness and medication adherence analyses.
Results
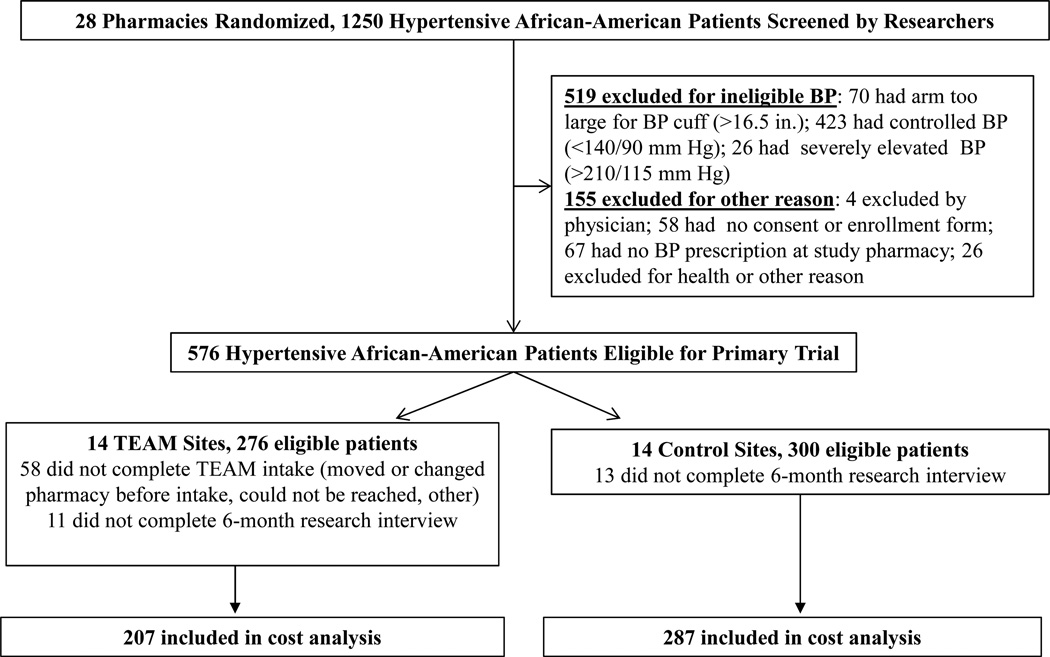
Research assistants screened 1,250 patients at 28 community pharmacies (Figure 1). All patients were self-identified as black and 576 were eligible for the primary trial (276 TEAM, 300 control). Of 276 subjects randomized to TEAM, 58 were excluded from the cost analysis because they did not complete their initial pharmacist visit and 11 were excluded because they did not complete the 6-month research interview and BP measurement, leaving a final TEAM sample of 207 for the cost-effectiveness analyses. For the control group, 13 patients were excluded from the cost analysis because they did not complete the 6-month BP measurement, leaving a control group sample of 287. All patients had uncontrolled BP at the time of enrollment. The TEAM and control group patients were balanced, with no significant between-group differences with respect to baseline SBP, DBP, and other characteristics (Table 1). Approximately two-thirds of each group was female; mean ages were in the early 50s, and 45–50% of all patients had household incomes under $20,000/year. The mean number of antihypertensive drugs at baseline was 1.77 for the control group and 1.84 for the TEAM group, and comparable numbers reported missing one or more doses in the previous week (26.1% for control and 24.6% for TEAM).
Figure 1.
Patient Flow in the Cost Analysis of TEAM Intervention
Intervention costs
TEAM pharmacists recorded their patient consultation time for 204 of 207 initial visits. On average, the initial visit between a TEAM pharmacist and patient lasted 24.8 minutes (Table 2). Overall, 83.6% of the TEAM group completed the first follow-up visit and the majority (59.4%) of TEAM group patients completed four follow-up visits over the 6-month intervention period. The first follow-up visit was 11.7 minutes (SD = 6.2) on average, while the fifth visit lasted 10.1 minutes (SD = 5.7) on average. Total pharmacist reported time for counseling TEAM patients averaged 60.1 minutes (SD = 38.1) per patient across the 6-month intervention. Pharmacist time for preparing and faxing written requests or feedback to primary care providers averaged 2.8 minutes (SD = 5.3) per patient (10 minutes/request × 63 requests). Pharmacy technician estimated time averaged 95.4 minutes (SD = 54.0) per patient across visits. Combined pharmacist and technician time costs came to $90.06 (SD = 43.0) per person. Adding the costs of TEAM tools used during initial and follow-up visits brought the total to $104.8 (SD = 45.2) per patient over the 6-month intervention.
Table 2.
Variable costs for pharmacy personnel time and tools used during the 6-month TEAM intervention
| No. of patients completing visit (%) |
Mean minutes per visit (SD) | Mean per patient (SD) | ||
|---|---|---|---|---|
| A. Cost of pharmacy personnel time | ||||
| Pharmacist time for consulting patient | ||||
| Initial visit | 207 (100%) | 24.8 (11.5) | ||
| Follow-up visits | ||||
| Follow-up visit 1 | 173 (83.6%) | 11.7 (6.2) | ||
| Follow-up visit 2 | 153 (73.9%) | 11.5 (7.0) | ||
| Follow-up visit 3 | 142 (68.6%) | 10.3 (6.2) | ||
| Follow-up visit 4 | 123 (59.4%) | 10.6 (5.7) | ||
| Follow-up visit 5 | 98 (47.3%) | 10.1 (5.7) | ||
| Total pharmacist time for consulting patient over 6 months, minutes | 60.1 (38.1) | |||
| Total pharmacist time for providing feedback/requests to provider over 6 months, minutes | 2.8 (5.3) | |||
| Total pharmacist time for consulting patient or his/her provider over 6 months, minutes | 62.8 (39.4) | |||
| Total technician time per patient over 6 months, minutes | 95.4 (54.0) | |||
| Total cost for pharmacy personnel time per patient 6 months in US dollars, $ | $ 90.06 (43.0) | |||
| B. Cost of TEAM tools used | ||||
| Cost of tools used at initial visit, $ | $ 9.57 (0.7) | |||
| Cost of tools used at follow-up visit, $ | $ 4.29 (2.5) | |||
| Cost of tools for feedback/requests to provider, $ | $ 0.23 (0.4) | |||
| Total cost of tools used per patient over 6 months, $ | $ 14.10 (2.7) | |||
| C. Total cost of personnel time and tools used per patient, $ | $ 104.80 (45.2) | |||
SD, standard deviation
In 2007, Wisconsin pharmacist mean hourly wages were $49.48/hour; pharmacy technician mean hourly wages were $13.01/hour.
Effectiveness
Table 3 shows the between-group differences in SBP, DBP, BP control, and refill adherence. Consistent with the primary trial results, the 6-month systolic BP decreased significantly more in TEAM versus control group patients (−11.8 mm Hg versus −6.2 mm Hg; t = 3.08, df = 489 p = 0.002). While the diastolic BP change was smaller, the between-group difference was statistically significant (−8.4 for TEAM group and −6.2 for control group ; t = 2.31, df = 491, p = 0.021). BP control was achieved in 53.8% and 36.7% in TEAM group and control group and, respectively (χ2 = 14.19, df = 1, p<0.001) and the percentage of patients achieving good refill adherence was significantly higher for TEAM patients compared with the control group (59.7% versus 36.1%; χ2 = 24.78, df = 1, p<0.001).
Table 3.
Incremental cost-effectiveness analyses of TEAM versus control for blood pressure and adherence outcomes
| Group | SBP change (mmHg) | DBP change (mmHg) |
Met usual BP goal (<140/90) |
Achieved Good refill adherence (80%PDC) |
|---|---|---|---|---|
| Control | ||||
| Mean ± SD | −6.24 ± 22.17 | −6.15 ± 12.44 | 0.367 ± 0.482 | 0.361 ± 0.480 |
| 95% CI | −8.81, −3.68 | −7.59, −4.71 | 0.311,0.423 | 0.303, 0.418 |
| TEAM | ||||
| Mean ± SD | −11.8 ± 17.30 | −8.45 ± 9.32 | 0.538 ± 0.499 | 0.597 ± 0.490 |
| 95% CI | −14.17, −9.46 | −9.72, −7.18 | 0.470, 0.606 | 0.526, 0.668 |
| Differences | ||||
| Mean ± SD | −5.58 ± 1.74* | −2.30 ± 0.99** | 0.172 ± 0.044*** | 0.236 ± 0.047*** |
| 95% CI | −5.68, −5.47 | −2.36, −2.23 | 0.169, 0.174 | 0.233, 0.239 |
| ICERs | ||||
| Mean ± SD | $22.2 ± 16.3 | $66.0 ± 228.4 | $665.2 ± 265.2 | $463.3 ± 110.7 |
| 95% CI | 21.2, 23.2 | 51.9, 80.0 | 648.7, 681.6 | 456.4, 470.1 |
SBP, systolic blood pressure; mmHg, millimeters mercury; DBP, diastolic blood pressure; BP, blood pressure; PDC, proportion days controlled; SD, standard deviation; CI, confidence interval; TEAM, Team Education and Adherence Monitoring; ICER, incremental cost-effectiveness ratio
p = 0.002
p = 0.021
p < 0.001
Incremental analysis
The incremental cost-effectiveness ratios (ICERs) for the primary endpoints are also shown in Table 3. Incremental variable costs per mmHg decrease in SBP and DBP were $22.2 ± 16.3 and $66.0 ± 228.4, respectively. Confidence intervals (95%) are shown in the table for each estimate. The pharmacy intervention cost of helping one more person achieve the BP goal (< 140/90) was $665.2 ± 265.2; the cost of helping one more person achieve good refill adherence was $463.3 ± 110.7.
Prescription drug costs and the use of other health care resources
The number of antihypertensive prescriptions filled by the TEAM group during the 6 month intervention period averaged 9.9 (SD = 6.2) as compared to 7.9 (SD = 5.6) for the control group (p = 0.001) (data not shown). Likewise, prescription medication costs were significantly higher for the intervention group ($392.8, SD = 396.3 versus $307.0, SD = 295.2, p = 0.02). There were no significant differences in the number of patient-reported outpatient visits or inpatient visits for TEAM group versus the control group during the six month intervention: visits to general doctors (2.61 versus 2.44, p>0.05), visits to specialists (0.38 versus 0.56, p>0.05), visits to an emergency room (0.49 versus 0.47, p>0.05), or admissions to a hospital (0.25 versus 0.24, p>0.05).
Discussion
Many pharmacist- or nurse-led interventions have been proposed to improve patient adherence with antihypertensive medications and BP control; however, few interventions have been implemented widely because they are viewed as too costly, complex, and labor-intensive23. Our study is the first cluster-randomized trial to examine the cost-effectiveness of the TEAM intervention for monitoring and improving medication adherence and BP control within community pharmacies, where most Americans obtain their medications. Compared with the control group, patients in the TEAM group achieved significant improvements in refill adherence and BP outcomes within six months and maintained net improvements in refill adherence and systolic BP reduction six months after intervention discontinuation26. Our cost results show that the TEAM intervention was implemented by regular pharmacy staff at an average cost of $105/patient and that the incremental cost of helping one additional patient to achieve good refill adherence was $463. A strength of this intervention is that it involved a greater role for pharmacy technicians and the use of relatively simple tools for saving staff time, increasing the applicability to routine practice. In this trial, pharmacist – patient encounters averaged less than 30 minutes per initial visit and less than 15 minutes per follow-up visit compared with 50–60 minutes per initial visit and 20–30 minutes per follow-up visit in previous studies23. Consistent with improved adherence, there was a significant increase in prescription drug costs. We did not observe significant between-group differences in inpatient or outpatient visits, but these effects would likely not be apparent until patients had more time with effective BP control.
Although many team interventions have been investigated, few studies report the per-patient costs associated with different strategies for improving adherence and BP control17,19,23,24,28. Our study adds to this small body of literature in several ways. First, our intervention was implemented successfully in a large and diverse sample of black patients within 28 typical community pharmacies. In contrast, previous studies have often involved predominantly white patients within an integrated health system or a small number of clinics where pharmacy specialists already work with physicians. Second, our study utilized objective measures of refill medication adherence and prospectively tracked pharmacist consultation times. Previous studies have often relied on patient self-reported measures of adherence28 and time estimates that were collected after the primary trials were completed17. Third, our results show that the incremental labor cost of helping one additional patient to achieve BP control was $665 – or nearly 50% lower than the $1338 cost of a physician - pharmacist collaborative intervention in 11 community-based medical offices17. Finally, our study found that the average per-patient cost of the TEAM intervention ($105) is considerably less than a recent pharmacist-led interventions that included home BP telemonitoring28. In their study within an integrated health system, Margolis et al (2013) found that the average intervention cost was $1350/patient, with 52% of the cost for tele-monitoring and 48% of the cost for 390 minutes of pharmacist consultation time per patient. While we cannot directly compare the relative cost-effectiveness of these approaches given the different study designs, there are important considerations about the trade-offs between the relative roles and costs of technology and community pharmacists.
Implications for Practicing Pharmacists
We believe the success of the TEAM intervention can be attributed to several factors. First, we designed and supplied each team with a “clinical toolkit” that included a 2-page Brief Medication Questionnaire (BMQ) and a 1-page BP Goal Check for more systematic and rapid “pre-visit” screening and tracking of the most common modifiable barriers to adherence, based on our previous studies and the Health Collaboration Model25. Our “pre-visit” screening tools were written in checklist format and 5th grade reading level, allowing patients to identify their drug-specific concerns and understandings before each visit. Second, we provided a joint workshop for one pharmacist and one pharmacy technician at each site. Pharmacy technicians were trained to assist the pharmacist in various labor-intensive tasks, saving pharmacist time and increasing staff fidelity to the intervention protocol. Third, we provided pharmacists with a 1-page tool for providing written feedback and requests to physicians, reducing the time required for communicating with other providers. This 1-page form, referred to as a “Request for Medication Review”(RMR), was written in a checklist format and included space for identifying current drug orders, BP readings, adherence issues, and any pharmacist recommendations, if needed. A copy of all intervention tools and photographs of a typical BP counseling station can be accessed at the TEAM study website: http://www.pharmacy.wisc.edu/team-study/intervention-tools.
There are additional considerations for pharmacists who wish to adopt this program. Our intervention was implemented in 28 typical community chain pharmacies where pharmacists have experience and responsibility for dispensing antihypertensive medications, working with pharmacy technicians, using refill records to identify early or late refill patterns, and responding to patient questions and concerns about their medications. Like many new programs, the TEAM program does require 8 hours of staff training and does impose a fixed cost for new equipment and materials. However, the cost of creating a pharmacy-based BP counseling station ($168) is modest compared with the cost of the equipment and software required for home BP tele-monitoring. In addition, as more patients are involved in the intervention, the average per patient cost declines with economies of scale.
Limitations
First, our study involved black patients within typical community pharmacies located in Milwaukee and other Wisconsin cities. Therefore, our findings may not be generalized to other populations. Second, we did not have pharmacy technicians directly record their time during the intervention, though our estimate was derived from direct observation of a series of interventions. Third, we conducted the analysis from a limited perspective, capturing only direct costs and intermediate outcomes (BP and adherence) of the intervention. A more complete societal perspective would include patient time costs and long-term implications, such as downstream cardiovascular events, life expectancy and quality of life. Finally, we did not conduct a sensitivity analysis since there were very few measures included in the incremental cost-effectiveness ratio and we directly observed them. We chose instead to rely upon the costs and outcomes generated in the trial itself and allow the confidence intervals generated through bootstrapping reflect variation in the measures.
Future Research
Future research is needed to evaluate alternative strategies for engaging large corporations who are in a position to adopt and promote adherence interventions in a large number of pharmacy outlets nationwide. We previously reported a “dose-response relationship” for the TEAM intervention, that is, patients who received the “full” intervention (4–6 visits) achieved significantly higher rates of adherence and BP control than patients who received a “partial” intervention (1–3 visits) or information only.26 Additional studies are needed to determine if the TEAM intervention might be even more cost-effective for black patients if the intervention was somewhat longer (9 or 12 months). As our study was not designed to evaluate the long-term benefits of achieving good refill adherence and BP control, future projects could evaluate the impact of long-term pharmacist-patient interactions in active hypertension management. A long term study of 18,806 newly diagnosed hypertensive patients has found that good refill adherence (≥ 80% days covered) was associated with a 38% decreased risk of acute cardiovascular events6. Additional studies are needed to determine the extent to which a TEAM intervention could lead to changes in quality of life and decreased risks of acute cardiovascular events particularly in black hypertensive patients and possibly other patients with treated but uncontrolled hypertension.
Conclusion
Our randomized, practice based intervention demonstrated that Wisconsin community pharmacists provided a cost-effective intervention to assist Blacks with achieving better adherence and hypertension control. The TEAM approach can be readily integrated into the ongoing pharmacist-patient relationship. Broader recognition and adoption of this intervention model can readily fit into the existing scope of pharmacy practice. As such, community pharmacies would not require special permissions from physicians, and the intervention would derive from existing pharmacist-patient relationships. This approach requires basic technology widely available in community practice, easing economic and literacy burdens for patients as well as pharmacies.
Key Points.
- Background
-
◦Implementation of the TEAM intervention led to improved BP control and better BP medication adherence in black patients with uncontrolled hypertension as has been previously reported
-
◦While a variety of interventions have demonstrated effectiveness, there continue to be barriers to implementation including reliance on expensive software and equipment for home BP tele-monitoring, and labor-intensive methods, leading to increased pharmacist or nurse time costs.
-
◦
- Findings
-
◦We documented the incremental cost-effectiveness of a community pharmacy based intervention along with the documentation of fixed costs at the pharmacy level, to demonstrate that the TEAM intervention is feasible, effective, and efficient.
-
◦
Acknowledgments
We gratefully acknowledge the contributions of our co-investigators in the primary TEAM trial, including: Jane Morley Kotchen, MD, MPH (Department of Medicine, Medical College of Wisconsin, Milwaukee); Roger L. Brown, PhD (Schools of Nursing and Medicine, University of Wisconsin–Madison); Stephanie Y. Crawford, PhD, MPH (College of Pharmacy, University of Illinois at Chicago); Jeanine K. Mount, PhD (Bouve´ College of Health Sciences and School of Pharmacy, Northeastern University); Pamela A. Palmer, BSPharm (retired); and Eva M. Vivian, PharmD and Dale A. Wilson, MA (School of Pharmacy, University of Wisconsin–Madison. We also thank the participating pharmacists, pharmacy technicians, supervisors, and management of Walgreens and Aurora Pharmacy
Funding: National Heart, Lung, and Blood Institute research grant HL78580 (to Dr. Svarstad)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinicaltrials.gov identifier: NCT00205153
Disclosure: The authors declare no conflicts of interest or financial interests in any product or service mentioned in this article, including grants, employment, gifts, stock holdings, or honoraria.
Contributor Information
Theresa I. Shireman, Health Services Policy & Practice, Brown University School of Public Health, Providence, RI.
Bonnie L. Svarstad, School of Pharmacy, University of Wisconsin - Madison, Madison, WI.
References
- 1.Chobanian AV. Impact of nonadherence to antihypertensive therapy. Circulation. 2009;120:1558–1560. doi: 10.1161/CIRCULATIONAHA.109.906164. [DOI] [PubMed] [Google Scholar]
- 2.Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. American Journal of Hypertension. 2006;19:1190–1196. doi: 10.1016/j.amjhyper.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence, ambulatory visits, and risk of stroke and death. Journal General Internal Medicine. 2010;25:495–503. doi: 10.1007/s11606-009-1240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. American Journal of Public Health. 1996;86:1805–1808. doi: 10.2105/ajph.86.12.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaya FT, Du D, Gbarayor CM, Frech-Tamas F, Lau H, Weir MR. Predictors of compliance with antihypertensive therapy in a high-risk Medicaid population. Journal of the National Medical Association. 2009;101:34–39. doi: 10.1016/s0027-9684(15)30808-7. [DOI] [PubMed] [Google Scholar]
- 6.Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299. [DOI] [PubMed] [Google Scholar]
- 7.Dragomir A, Cote R, Roy L, Blais L, Lalonde L, Berard A, Perreault S. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Medical Care. 2010;48:418–425. doi: 10.1097/MLR.0b013e3181d567bd. [DOI] [PubMed] [Google Scholar]
- 8.Herttua K, Tabak AG, Martikainen P, Vahtera J, Kivimaki M. Adherence to antihypertensive therapy prior to the first presentation of stroke in hypertensive adults: population-based study. European Heart Journal. 2013;34:2933–2939. doi: 10.1093/eurheartj/eht219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. American Journal of Medicine. 2006;119:70 e9–70 e15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacoepidemiology and Drug Safety. 2009;18:672–681. doi: 10.1002/pds.1766. [DOI] [PubMed] [Google Scholar]
- 11.Holmes HM, Luo R, Hanlon JT, Elting LS, Suarez-Almazor M, Goodwin JS. Ethnic disparities in adherence to antihypertensive medications of Medicare Part D beneficiaries. Journal of the American Geriatrics Society. 2012;60:1298–1303. doi: 10.1111/j.1532-5415.2012.04037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circulation Cardiovascular Quality and Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, Owens DK, Goldstein MK. Quality improvement strategies for hypertension management: a systematic review. Medical Care. 2006;44:646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 14.Carter BL, Ardery G, Dawson JD, James PA, Bergus GR, Doucette WR, Chrischilles EA, Franciscus CL, Xu Y. Physician and pharmacist collaboration to improve blood pressure control. Archives of Internal Medicine. 2009;169:1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chisholm-Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, Graff Zivin J, Abraham I, Palmer J, Martin JR, Kramer SS, Wunz T. US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Medical Care. 2010;48:923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 16.van Dalem J, Krass I, Aslani P. Interventions promoting adherence to cardiovascular medicines. International Journal of Clinical Pharmacy. 2012;34:295–311. doi: 10.1007/s11096-012-9607-5. [DOI] [PubMed] [Google Scholar]
- 17.Kulchaitanaroaj P, Brooks JM, Ardery G, Newman D, Carter BL. Incremental costs associated with physician and pharmacist collaboration to improve blood pressure control. Pharmacotherapy. 2012;32:772–780. doi: 10.1002/j.1875-9114.2012.01103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cote I, Gregoire JP, Moisan J, Chabot I, Lacroix G. A pharmacy-based health promotion programme in hypertension: cost-benefit analysis. PharmacoEconomics. 2003;21:415–428. doi: 10.2165/00019053-200321060-00005. [DOI] [PubMed] [Google Scholar]
- 19.Okamoto MP, Nakahiro RK. Pharmacoeconomic evaluation of a pharmacist-managed hypertension clinic. Pharmacotherapy. 2001;21:1337–1344. doi: 10.1592/phco.21.17.1337.34424. [DOI] [PubMed] [Google Scholar]
- 20.Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, Pickering T, Schwartz JE. Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129:2044–2051. doi: 10.1161/CIRCULATIONAHA.113.006650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circulation Cardiovascular Quality and Outcomes. 2013;6:157–163. doi: 10.1161/CIRCOUTCOMES.112.968172. [DOI] [PubMed] [Google Scholar]
- 22.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA : Journal of the American Medical Association. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chapman RH, Ferrufino CP, Kowal SL, Classi P, Roberts CS. The cost and effectiveness of adherence-improving interventions for antihypertensive and lipid-lowering drugs. International Journal of Clinical Practice. 2010;64:169–181. doi: 10.1111/j.1742-1241.2009.02196.x. [DOI] [PubMed] [Google Scholar]
- 24.Wang V, Smith VA, Bosworth HB, Oddone EZ, Olsen MK, McCant F, Powers BJ, Van Houtven CH. Economic evaluation of telephone self-management interventions for blood pressure control. American Heart Journal. 2012;163:980–986. doi: 10.1016/j.ahj.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 25.Svarstad BL, Kotchen JM, Shireman TI, Crawford SY, Palmer PA, Vivian EM, Brown RL. The Team Education and Adherence Monitoring (TEAM) trial: pharmacy interventions to improve hypertension control in blacks. Circulation Cardiovascular Quality and Outcomes. 2009;2:264–271. doi: 10.1161/CIRCOUTCOMES.109.849992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Svarstad BL, Kotchen JM, Shireman TI, Brown RL, Crawford SY, Mount JK, Palmer PA, Vivian EM, Wilson DA. Improving refill adherence and hypertension control in black patients: Wisconsin TEAM trial. Journal of the American Pharmacists Association. 2013;53:520–529. doi: 10.1331/JAPhA.2013.12246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA : Journal of the American Medical Association. 1996;276:1253–1258. [PubMed] [Google Scholar]
- 28.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O'Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA : Journal of the American Medical Association. 2013;310:46–56. doi: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]