Abstract
Objectives
Individuals with mental illness face an increased risk of oral disease compared to those without mental illness. The goals of this study were to examine the self-reported oral health and dental access of individuals filing psychotropic medication prescriptions; and to determine whether pharmacy patients would choose to speak with a pharmacist about their oral health if given the option to do so.
Design
Pharmacists across 6 community pharmacies within a local chain identified and surveyed adult patients filling prescriptions for psychotropic medications. Surveys included questions about oral health, dry mouth, and dental care utilization.
Setting
Six community pharmacy locations.
Participants
Adults (18+ years) filling prescriptions for psychotropic medications.
Intervention
Not applicable.
Main Outcome Measures
Self-reported oral health, dental utilization, desire to discuss oral health with a pharmacist.
Results
Participants (N=178) filling prescriptions were mostly (65.9%) female with a mean age of 48.2 years (s.d.=14.3; range 19–82 years). One in four (24.9%) said their mouths “always” or “frequently” felt dry; these individuals were significantly more likely to have last seen a dentist for emergency (rather than routine) treatment (p<0.01) and rated their oral health as significantly worse (p<0.001) than participants whose mouths “never” or “occasionally” feel dry. A small percentage (5.7%) requested to speak with pharmacists about oral health; they reported poorer oral health than those who opted not to speak with a pharmacist (p<0.05).
Conclusions
One in four patients reported having dry mouth, and those with dry mouth reported significantly worse oral health than patients without dry mouth. While dry mouth and poor oral health were common in this sample of individuals taking psychotropic medications, this did not consistently translate into information seeking regarding oral health. Future research will focus on pharmacist-initiated oral health interventions with high-risk patients.
Introduction
Individuals with mental illness are often at an increased risk for developing oral health problems. Heaton and colleagues found adults with at least one mental health condition were twice as likely to report having unmet dental need than adults without mental illness.1 Having some kind of mental illness has been associated with a host of poor oral health outcomes,2 including periodontal disease,3 edentulism,4–5 and increased caries rates in hospitalized patients.6
Side effects of psychotropic medications (i.e., medications used to treat conditions such as mood, anxiety, or psychotic disorders) have been linked with dry mouth7 and increased caries rates.8–9 Lalloo and colleagues found higher levels of dental disease in outpatient adults in Queensland taking psychotropic medications when compared to national or state averages.10 A systematic review by Matevosyan found psychotropic medication use was a significant predictor of poor oral health in adults with serious mental illness.2 In addition to oral health impacts of psychotropic medications, adults with more severe forms of mental illness, such as schizophrenia, are often unable to access regular dental care, placing their oral health at greater risk.11–12
As healthcare providers, pharmacists have been enlisted to provide access to health care resources for underserved populations (Goyette et al., 2003).13 Some large retail pharmacies are beginning to employ additional healthcare providers for in-pharmacy clinics (e.g., “MinuteClinic” in CVS and “Healthcare Clinic” in Walgreen’s; McClatchy, 2015) with the goal of increasing access to healthcare.14 A retrospective, national study in the United States (U.S.) found in 2009–2010, one-third of influenza vaccines were provided by pharmacists in medically underserved areas (MUAs).15 Low-income women have expressed interest in being able to receive contraceptives in pharmacies rather than through primary care settings.16 After health care reform in Massachusetts allowed women to obtain contraception in pharmacies, focus groups found increased access to contraceptives.17
There has been increasing interest in pharmacists providing oral health recommendations in recent years, both from pharmacists and the public health sector. In 2011, the American Dental Association (ADA) and American Pharmacists’ Association (APhA) joined efforts to increase awareness of the potential oral health side effects of medications.18 Cohen called for the use of pharmacists as an oral health resource for populations who lack access to regular dental care, and found that pharmacy patients with recent toothache were likely to ask their pharmacist about their oral health.19–20 Bawazir noted while pharmacists surveyed in Saudi Arabia were willing to speak with patients about their oral health, most (94%) felt their oral health knowledge was lacking and would be improved through continuing education.21 Interviews with New Zealand pharmacists similarly found pharmacists thought oral health fell within their counseling objectives, yet felt their lack of training in oral health issues limited their ability to provide optimal recommendations.22
Maunder and colleagues further noted while pharmacists in the United Kingdom (U.K.) were willing to advise individuals about oral health, they were unaware of dental resources to which they could refer patients.23 These results echo those found in the U.S.,24 England,25 and India.26 Steel & Wharton surveyed pharmacy assistants about their confidence in providing recommendations about a variety of oral health topics (e.g., dry mouth, denture hygiene) and found that most reported being “fairly confident” or “neutral” about their level of knowledge of oral health issues.27 An oral health knowledge survey of pharmacy students in Malaysia showed poor oral health knowledge among these students, although the students reported being interested in and willing to provide oral health guidance to patients.28 Pharmacists, pharmacy students and assistants, therefore, recognize the importance of addressing oral health issues in the pharmacy setting given appropriate training, which places them in an optimal position to provide oral health recommendations to individuals who lack regular access to dental care, such as individuals with mental illness.
Objectives
The goal of this study was to conduct a pilot oral health project in community pharmacies in which pharmacists surveyed patients filling prescriptions for psychotropic medications about their oral health. We aimed to examine the self-reported oral health and access to dental treatment of individuals filing psychotropic medication prescriptions, and to determine whether pharmacy patients would choose to speak with a pharmacist about their oral health if given the option to do so.
Methods
Participants
Participants were recruited through one of six pharmacies from a single pharmacy chain (Bartell Drug Company, Inc.) in Western Washington State. Participating pharmacies were identified by individuals in the pharmacy upper management to reflect both urban and suburban locations among the 63 retail stores that serve individuals of lower socioeconomic status (SES). As the literature has consistently shown an association between mental illness and lower SES,29 it was decided that selecting pharmacies in lower-SES areas might increase the likelihood of identifying and recruiting individuals filling prescriptions for psychotropic medications.
Participants were adults (18 years and over) who came to the participating pharmacies to fill prescriptions for psychotropic medications (e.g., antidepressant, antianxiety, and/or antipsychotic medications). Pharmacists were provided with a study binder that contained a list of such medications in order to facilitate identification of potential participants. Individuals were eligible for participation if they were filling at least one prescription for a psychotropic medication and consented to participate in the study. Although the consent information and surveys were also available in Spanish, Vietnamese, and Russian (the most commonly spoken languages beyond English in the populations served by this pharmacy chain), all surveys were completed in English.
All study protocols and materials were reviewed and approved by the Institutional Review Board (IRB) at the University of Washington.
Procedure
Pharmacists were asked to identify adult patients who were filling at least one prescription for a psychotropic medication. Colored stickers were provided in the study binders to place on the outer packaging of individual patient prescription containers that were being readied for dispensing to facilitate pharmacists approaching eligible adults. When an eligible individual approached the pharmacy counter to purchase his/her prescription, the pharmacist informed the individual of the opportunity to participate in the study, and if interested, handed the participant a paper copy of the survey. At the top of the survey was printed an information statement that gave participants information about the study, their rights as research participants, and contact information for both the Principal Investigator (LJH) and the IRB at the University of Washington.
Each store was given up to 40 surveys to distribute to patients filling prescriptions for psychotropic medications, in batches of 20 each. If a store completed the first 20 surveys, the PI (LJH) offered the lead pharmacist the opportunity to receive another 20 surveys. Four of the six pharmacies opted to receive a second batch of surveys. Pharmacists at the two pharmacies that received only one batch of surveys cited a lack of time and eligible patients as reasons for low recruitment; one of these pharmacies was delayed in beginning recruitment by a month due to staffing issues. The remaining 4 pharmacies reported that they had no difficulty in identifying and surveying patients, although records were not kept regarding how many patients were approached and declined to participate. Therefore, these results represent only those patients who agreed to participate.
Participants completed the anonymous survey either in-store or at home (to be returned at the next visit to the pharmacy), and were instructed not to write any identifying information on the survey. The final question of the survey asked if the participant wished to speak with a pharmacist about his/her oral health. For participants who wished to speak with a pharmacist, the pharmacist reviewed with the participant an information sheet about dry mouth and medications (provided in the study binder)30 and answered any other oral health questions from the participant. Upon completion of the survey and oral health counseling (if requested), participants were each given a bag with a toothbrush and two sample-sized tubes of toothpaste for their participation.
The survey consisted of 13 items related to oral health and use of dental services (see Appendix). Items covered topics such as self-rated oral health, frequency and impact of dry mouth symptoms, how they managed dry mouth symptoms, usual sources of oral health recommendations, number of dental visits in the previous 12 months, reason for last dental visit, and demographic questions. Participants were also asked to indicate on the survey if they wished to speak with a pharmacist about their oral health. The survey was developed and modified by the research team, reviewed and modified by the research team and pharmacy management.
Statistical Analyses
Data were entered by hand into a Microsoft Excel spreadsheet, and a random selection of 10% of surveys was checked a second time for accuracy. The data were then imported into PASW Statistics 18.0 (IBM SPSS Software, USA) for analyses. Descriptive analyses examined the distribution of age, gender, race, ethnicity, oral health status, and dental service use of the population. To test differences in self-reported oral health between participants who “never” or “occasionally” experienced dry mouth symptoms (“no dry mouth”) and those who “frequently” or “always” experienced such symptoms (“dry mouth”), independent sample t-tests were used. Chi-square analyses tested between-group differences in reasons for the last dental visit between those with and without dry mouth. In summary, t-tests were used to test between-group differences in means for continuous variables, and Chi Square analyses were used to test between-group differences for categorical variables.
Results
Demographics
One hundred and seventy-eight individuals participated across the 6 pharmacy locations (see Table 1). The sample consisted of 65.9% female participants and had a mean age of 48.2 years (s.d.=14.3; range 19–82 years). Most (91.4%) participants did not consider themselves to be Hispanic or Latino/a, and the majority (87.6%) reported being White/Caucasian. The number of individuals participating in each pharmacy location ranged from 6–33 (mean=23, s.d.=10.8). There were no differences in age, gender, race, ethnicity, or pharmacy locations between those reporting dry mouth or not. Data collection began in June 2014 and was completed in September 2014.
Table 1.
Descriptive statistics by dry mouth frequency
| Dry Mouth (n=44)2 | No Dry Mouth (n=133)2 | p1 | |
|---|---|---|---|
| Age | 47.6 (s.d.=14.2) | 50.0 (s.d.=14.4) | .339 |
|
| |||
| Gender | |||
| Female | 27 (61.4) | 89 (67.4) | .310 |
| Male | 17 (38.6) | 43 (32.6) | |
|
| |||
| Race | |||
| Hispanic/Latino(a) | 4 (88.7) | 11 (6.3) | .528 |
| Not Hispanic/Latino(a) | 39 (22.3) | 121 (69.1) | |
|
| |||
| Ethnicity | |||
| American Indian/Alaska Native | 1 (2.3) | 1 (0.8) | .204 |
| Asian | 0 (0.0) | 5 (3.9) | |
| Native Hawaiian/Other Pacific Islander | 1 (2.3) | 2 (1.6) | |
| Black/African American | 1 (2.3) | 4 (3.1) | |
| White/Caucasian | 36 (83.8) | 113 (89.0) | |
| More than one race | 3 (7.0) | 1 (0.8) | |
| Prefer not to say | 1 (2.3) | 1 (0.8) | |
|
| |||
| Pharmacy locations | |||
| Store #1 (n=29) | 4 (9.0) | 29 (21.8) | .110 |
| Store #2 (n=33) | 7 (15.9) | 32 (24.1) | |
| Store #3 (n=13) | 7 (15.9) | 12 (9.0) | |
| Store #4 (n=23) | 13 (29.5) | 23 (17.3) | |
| Store #5 (n=31) | 9 (20.5) | 31 (23.3) | |
| Store #6 (n=6) | 4 (9.0) | 6 (4.5) | |
T-tests were used for continuous variables, and Chi Square was used for categorical variables.
As not all participants responded to all questions, some response rates do not sum to 100%.
Dry Mouth Symptoms and Impact
The majority of participants (n=117; 66.1%) reported their oral health to be “good” (n=84; 47.5%) or “excellent” (n=33; 18.6%; see Table 2). Nearly one in four participants (n=44, 24.9%) reported experiencing dry mouth symptoms. Participants with dry mouth reported their oral health as significantly worse (p<0.001) and reported more of an impact of dry mouth on their daily lives (p<0.001) than those without dry mouth. A greater percentage of individuals with dry mouth reported asking others about dry mouth than those without dry mouth (37.2% versus 10.4%; p<0.001). While there were no differences in frequency of dental visits within the previous 12 months between those with and without dry mouth (p=.442), a significantly larger proportion of participants with dry mouth reported having seen a dentist most recently for emergent, rather than routine, treatment (35.3% versus 13.0%; p<0.01).
Table 2.
Oral health outcomes by frequency of dry mouth
| Dry Mouth (n=44)2 | No Dry Mouth (n=133)2 | p1 | |
|---|---|---|---|
| Self-reported oral health (N=177) | |||
| Excellent | 0 (0.0) | 33 (24.8) | .000* |
| Good | 12 (27.3) | 72 (54.1) | |
| Fair | 19 (43.2) | 19 (14.3) | |
| Poor | 11 (25.0) | 8 (6.0) | |
| I don’t know | 2 (4.5) | 1 (0.8) | |
|
| |||
| Impact of dry mouth (N=134) | |||
| Extremely | 1 (2.3) | 1 (1.1) | .000* |
| Quite a bit | 18 (41.9) | 0 (0.0) | |
| A little | 20 (46.5) | 43 (47.3) | |
| Not at all | 4 (9.3) | 47 (51.6) | |
|
| |||
| Asked others about dry mouth | |||
| Yes | 16 (37.2) | 10 (10.4) | .000* |
| No | 27 (62.8) | 86 (89.6) | |
|
| |||
| Dental visits in the last 12 months (mean (s.d.)) | |||
| 1.6 (1.6) | 1.8 (1.6) | .442 | |
|
| |||
| Reason for visits | |||
| Routine/scheduled | 22 (64.7) | 100 (87.0) | .003* |
| Emergency | 12 (35.3) | 15 (13.0) | |
|
| |||
| Oral Health Recommendations (number of “yes” responses) | |||
| Dentist | 30 (68.2) | 110 (82.7) | .036* |
| Hygienist | 8 (18.2) | 64 (48.1) | .000* |
| Dental Assistant | 5 (11.4) | 21 (15.8) | .327 |
| Physician | 6 (13.6) | 8 (6.0) | .100 |
| Nurse | 1 (2.3) | 1 (0.8) | .436 |
| Pharmacist | 4 (9.0) | 7 (5.3) | .279 |
| Therapist/Counselor | 1 (2.3) | 0 (0.0) | .249 |
| Psychologist/Psychiatrist | 1 (2.3) | 0 (0.0) | .249 |
| Friends or family | 8 (18.2) | 16 (12.0) | .214 |
|
| |||
| Methods tried to manage dry mouth (number of “yes” responses) | |||
| My mouth never feels dry | 0 (0.0) | 5 (3.8) | .358 |
| Chewing gum | 15 (34.1) | 23 (17.3) | .056 |
| Drinking water | 39 (88.6) | 80 (60.2) | .002* |
| Soda or pop | 6 (13.6) | 11 (0.8) | .497 |
| Juice | 7 (15.9) | 10 (7.5) | .227 |
| Candy | 5 (11.4) | 10 (7.5) | .624 |
| Mouthwash | 12 (27.3) | 11 (8.3) | .005* |
T-tests were used for continuous variables, and Chi Square was used for categorical variables.
As not all participants responded to all questions, some response rates do not sum to 100%.
Oral Health Resources
Participants identified individuals whom they sought out for recommendations about their oral health (see Table 2). Compared to those with dry mouth, participants without dry mouth were significantly more likely to ask a dentist (82.7% versus 68.2%; p=.036) or a hygienist (48.1% versus 18.2%; p<0.001) for advice about oral health. There were no other differences in sources of oral health recommendations (e.g., physicians, counselors) between those with and without dry mouth.
Methods Tried to Manage Dry Mouth
Participants were asked to indicate all the methods they had used to manage dry mouth symptoms (see Table 2). Compared to participants without dry mouth, a greater proportion of those with dry mouth had tried drinking water (88.6% versus 60.2%; p<.01) and using mouthwash (27.3% versus 8.3%; p<.01) to manage dry mouth symptoms. No other differences were found across methods for managing dry mouth between those with and without dry mouth.
Requests for Oral Health Counseling from Pharmacists
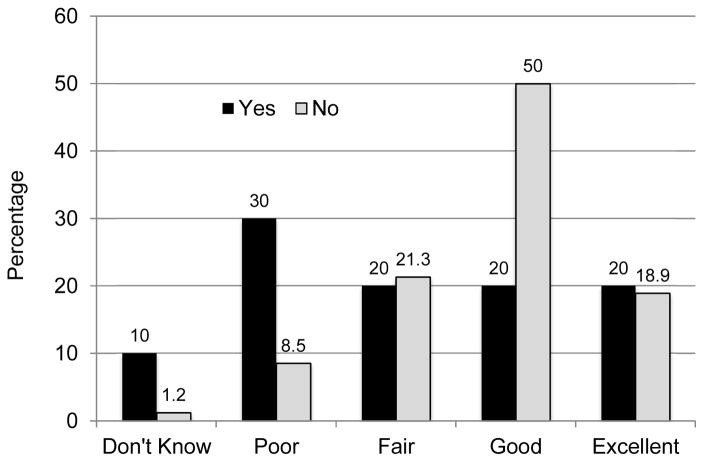
A small percentage (5.6%) requested to speak with pharmacists about oral health; they reported significantly poorer oral health than those who opted not to speak with a pharmacist (p<0.05; see Figure 1). Those with dry mouth were more likely to report their oral health as “poor”, while those without dry mouth were more likely to rate their oral health as “good.” While there was a trend for a greater proportion of participants requesting an oral health consult to also report dry mouth compared to those not requesting a consult (11.9% versus 3.8%; p=.063), this difference was not statistically significant.
Figure 1.
Self-reported oral health by request for a pharmacy oral health consult
Discussion
To our knowledge, this is the first study to assess oral health and dental attendance in patients at increased risk for oral disease in a pharmacy setting. In the current study, a significant proportion of patients in pharmacies filling prescriptions for psychotropic medications reported experiencing dry mouth “always” or “frequently,” as well as having poor oral health. The prevalence of dry mouth in the current study (24.9%) is slightly higher than in dental patient samples (19.6%).31 Consistent with our hypotheses, participants with dry mouth reported poorer oral health and were more likely to have sought recent emergency dental care than those without dry mouth, although there were no differences in frequency of dental care between the groups. Locker and colleagues noted an association between poor oral health-related quality of life and dry mouth in a sample of medically compromised elderly adults.32 Thomson and colleagues found use of antidepressants was linked with a significantly higher odds ratio (4.7) of having dry mouth in a sample of 32-year-old adults, and have noted that increased used of multiple medications such as antidepressants in older adults is associated with greater incidence of dry mouth.33–34
Some results of this study point to a potential lack of access to routine dental treatment for individuals taking psychotropic medications with oral health impacts. Participants reporting dry mouth were more likely to have seen a dentist most recently for emergent, rather than routine care, and were less likely to have spoken to a dentist or hygienist about their oral health than individuals without dry mouth. As participants with dry mouth reported poorer oral health overall, it could be expected that they would be more likely to speak with dental staff about their oral health, but non-significant trends in the current data suggested that they were more likely to speak with a physician or pharmacist about their oral health than individuals without dry mouth.
Consistent with these data, a small number (5.8%) of participants requested an oral health consult with a pharmacist. What is notable about this small subsample of participants is that they reported significantly poorer oral health than those who did not wish to speak with a pharmacist. This suggests that for individuals with poor oral health and potential lack of access to regular dental care, pharmacists are appropriate sources of oral health recommendations. Asahina and colleagues noted that patients were less likely to ask pharmacists about oral health recommendations if they also “had an incorrect understanding about health products”.35
While the literature is limited in patients’ attitudes toward receiving oral health recommendations from pharmacists, current data and those from Asahina suggest that the onus is on pharmacists to initiate conversations with patients at risk for oral disease, rather than focusing interventions at the patient level.35 Pharmacists in community pharmacies are considerably more accessible than dentists; individuals do not need an appointment or referral to approach a pharmacist with questions about medications or health conditions, including oral health. As noted previously, pharmacists and pharmacy technicians are willing to provide such counseling to patients, but feel their oral health training is lacking.24–26 In the current study, pharmacists cited the usefulness of the following factors as helping to facilitate their participation in the study: 1) a study binder that contained the study protocol, contact information for the PI, and a list of psychotropic medications; 2) stickers to affix to eligible individual prescription packages for more rapid identification of potential participants; and 3) a fact sheet regarding oral health that pharmacists were asked to use in their oral health consultations with participants who requested a consult.
The current study showed pharmacists were willing to engage patients in oral health discussions if given appropriate information to provide to patients. Interventions with practicing pharmacists should aim to increase both oral health knowledge and self-efficacy in providing oral health recommendations through. Interprofessional education activities between dental and pharmacy students provide excellent opportunities both for pharmacy students to gain knowledge of oral health issues and for dental students to engage with pharmacists as members of the oral healthcare team.36
Limitations
There are a number of limitations to this study that should be taken into consideration when interpreting these results. Specifically, reliance on self-reports of oral health and dry mouth without a clinical assessment by a dental provider provides limited information on a patient’s oral health status. Self-reported oral health does not always correlate with clinical findings, particularly when people are asked to self-report on current periodontal disease and dental decay.37 Agreement between self-reports and clinical findings of dry mouth is often weak.38 Therefore, estimates of dental disease and dry mouth in this sample may not be accurate. It will be important to repeat a similar study with a clinical examination to confirm participants’ self-perceptions. Further, as records were not kept regarding the number of participants who where approached and did not participate were not kept. Therefore, the results of this study are limited to those individuals who agreed to participate, and the ability to generalize these results to the larger population is limited. We were not able to follow up with participants to determine whether oral health counseling with pharmacists resulted in any type of behavior change with regard to management of dry mouth and/or overall oral health. Future studies will examine such behavior change through longitudinal means. Finally, the generalizability of the findings is limited by the study’s location in Western Washington State in a single retail pharmacy chain. However, the participating pharmacy locations were located in both urban and suburban locations, which helps increase generalizability. Future studies will include pharmacies across a larger geographic area and collect data regarding the exact prescriptions being filled by participants.
Conclusions
Nearly one in four patients in this pharmacy sample reported having dry mouth, and those with dry mouth reported significantly worse oral health and were significantly more likely to have recently sought emergency dental treatment than patients without dry mouth. While a small number of participants requested an oral health consult with a pharmacist, those who opted for such a consult reported significantly poorer oral health than those who did not request a consult. The results of this study suggest that pharmacy-based oral health interventions are feasible, but that such interventions may best be initiated by the pharmacists rather than patients.
Key Points.
Background
Individuals with mental illness are often at an increased risk for developing oral health problems.
As healthcare providers, pharmacists have been enlisted to provide access to health care resources for underserved populations.
There has been increasing interest in pharmacists providing oral health recommendations in recent years, both from pharmacists and the public health sector.
Findings
One third of patients filling prescriptions for psychotropic medications in participating community pharmacies reported their oral health was ‘fair’ or ‘poor’.
Participants with dry mouth reported poorer oral health and were more likely to have sought recent emergency dental care than those without dry mouth, although there were no differences in frequency of dental care between the groups.
While a small number of participants requested an oral health consult with a pharmacist, those who opted for such a consult reported significantly poorer oral health than those who did not request a consult.
Acknowledgments
This study was funded by National Institutes of Health/National Institute of Dental and Craniofacial Research (NIH/NIDCR) Grant 5K23DE019202-05. Material support was provided by the Bartell Drug Company in the form of the time and assistance of pharmacists in 6 store locations.
The authors would like to thank Billy Chow, RPh, Vice President of Pharmacy Operations and Clinical Programs for the Bartell Drug Company, Inc., the pharmacists and pharmacy assistants at the participating Bartell locations, and the study participants. This study was supported by NIH/NIDCR Grant 5K23DE019202-05.
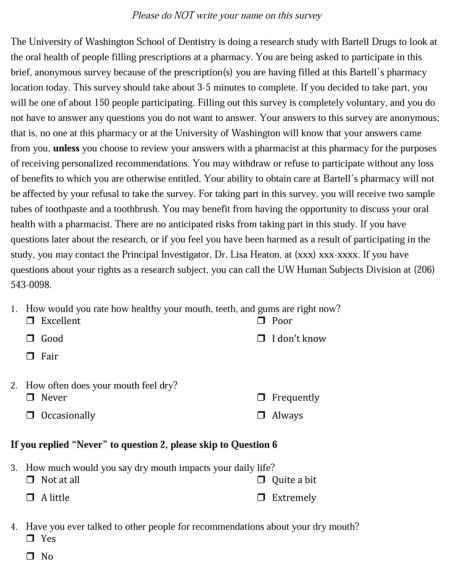
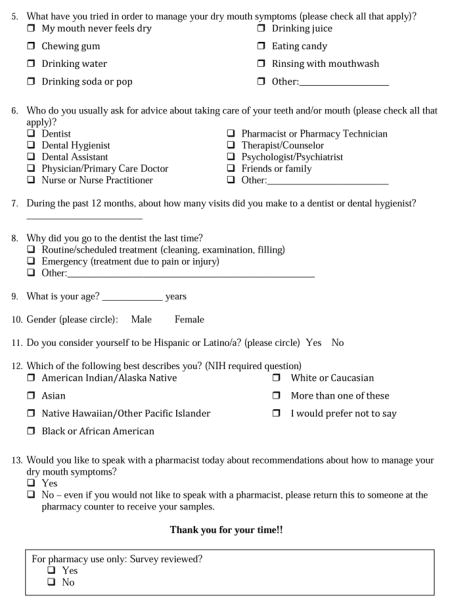
Appendix: Oral Health Survey
Footnotes
The data presented in this paper were presented at the 2015 annual meeting of the International Association for Dental Research (Boston, MA).
The authors confirm that they do not have any conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lisa J. Heaton, Clinical Assistant Professor, Department of Oral Health Sciences, University of Washington School of Dentistry.
Kimberly Swigart, Past: Clinical Programs Manager, Bartell Drug Company; Seattle, Washington; Current: Pharmacy Manager, Union Center Pharmacy; Seattle, Washington.
Gavin McNelis, Past: Undergraduate Student, University of Washington; Current: Volunteer, University of Washington School of Dentistry.
Peter Milgrom, Professor, Department of Oral Health Sciences, University of Washington School of Dentistry.
Donald F. Downing, Clinical Professor, Department of Pharmacy, University of Washington School of Pharmacy.
References
- 1.Heaton LJ, Mancl LA, Grembowski D, et al. Unmet dental need in community-dwelling adults with mental illness: results from the 2007 Medical Expenditure Panel Survey. J Am Dent Assoc. 2013;144(3):e16–23. doi: 10.14219/jada.archive.2013.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matevosyan NR. Oral health of adults with serious mental illnesses: a review. Community Ment Health J. 2010;46(6):553–62. doi: 10.1007/s10597-009-9280-x. [DOI] [PubMed] [Google Scholar]
- 3.Velasco E, Bullón P. Periodontal status and treatment needs among Spanish hospitalized psychiatric patients. Spec Care Dentist. 1999;19(6):254–8. doi: 10.1111/j.1754-4505.1999.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 4.Kisely S, Quek LH, Pais J, et al. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. 2011;199(3):187–93. doi: 10.1192/bjp.bp.110.081695. [DOI] [PubMed] [Google Scholar]
- 5.Kisely S, Baghaie H, Lalloo R, et al. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med. 2015;77(1):83–92. doi: 10.1097/PSY.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 6.Morales-Chávez MC, Rueda-Delgado YM, Peña-Orozco DA. Prevalence of bucco-dental pathologies in patients with psychiatric disorders. J Clin Exp Dent. 2014;6(1):e7–e11. doi: 10.4317/jced.51147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fratto G, Manzon L. Use of psychotropic drugs and associated dental diseases. Int J Psychiatry Med. 2014;48(3):185–97. doi: 10.2190/PM.48.3.d. [DOI] [PubMed] [Google Scholar]
- 8.deVries MW, Peeters F. Dental caries with longterm use of antidepressants. Lancet. 1995;346(8990):1640. doi: 10.1016/s0140-6736(95)91980-5. [DOI] [PubMed] [Google Scholar]
- 9.Peeters FP, deVries MW, Vissink A. Risks for oral health with the use of antidepressants. Gen Hosp Psychiatry. 1998;20(3):150–4. doi: 10.1016/s0163-8343(98)00017-6. [DOI] [PubMed] [Google Scholar]
- 10.Lalloo R, Kisely S, Amarasinghe H, et al. Oral health of patients on psychotropic medications: a study of outpatients in Queensland. Australas Psychiatry. 2013;21(4):338–42. doi: 10.1177/1039856213486308. [DOI] [PubMed] [Google Scholar]
- 11.Janardhanan T, Cohen CI, Kim S, Rizvi BF. Dental care and associated factors among older adults with schizophrenia. J Am Dent Assoc. 2011;142(1):57–65. doi: 10.14219/jada.archive.2011.0029. [DOI] [PubMed] [Google Scholar]
- 12.Kilbourne AM, McCarthy JF, Post EP, et al. Access to and satisfaction with care comparing patients with and without serious mental illness. Int J Psychiatry Med. 2006;36(4):383–99. doi: 10.2190/04XR-3107-4004-4670. [DOI] [PubMed] [Google Scholar]
- 13.Goyette D, Disco ME, Leal S, Schwed DH. The pharmacist as a primary care provider for the medically underserved. J Am Pharm Assoc (2003) 2003;43(5 Suppl 1):S52–3. doi: 10.1331/154434503322612483. [DOI] [PubMed] [Google Scholar]
- 14.McClatchy TP. Walk-in clinics bring affordable, on-demand health care to the masses. [Accessed June 10, 2015];Naples Daily News website. http://www.naplesnews.com/news/health/walkin-clinics-bring-affordable-ondemand-health-care-to-the-masses_58069148.
- 15.Murphy PA, Frazee SG, Cantlin JP, et al. Pharmacy provision of influenza vaccinations in medically underserved communities. J Am Pharm Assoc (2003) 2012;52(1):67–70. doi: 10.1331/JAPhA.2012.10070. [DOI] [PubMed] [Google Scholar]
- 16.Landau SC, Tapias MP, McGhee BT. Birth control within reach: a national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception. 2006;74(6):463–70. doi: 10.1016/j.contraception.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 17.McIntosh J, Tsikitas L, Dennis A. Low-income women’s access to contraception after health care reform in Massachusetts. J Am Pharm Assoc (2003) 2012;52(3):349–57. doi: 10.1331/JAPhA.2012.11033. [DOI] [PubMed] [Google Scholar]
- 18.American Pharmacists Association. [Accessed June 10, 2015];Dentists, Pharmacists Raise Awareness of Medication-Induced Dry Mouth. http://www.pharmacist.com/dentists-pharmacists-raise-awareness-medication-induced-dry-mouth.
- 19.Cohen LA. Enhancing pharmacists’ role as oral health advisors. J Am Pharm Assoc. 2013;53(3):316–21. doi: 10.1331/JAPhA.2013.12017. [DOI] [PubMed] [Google Scholar]
- 20.Cohen LA, Bonito AJ, Akin DR, et al. Role of pharmacists in consulting with the underserved regarding toothache pain. J Am Pharm Assoc (2003) 2009;49(1):38–42. doi: 10.1331/JAPhA.2009.07149. [DOI] [PubMed] [Google Scholar]
- 21.Bawazir OA. Knowledge and attitudes of pharmacists regarding oral healthcare and oral hygiene products in Riyadh, Saudi Arabia. J Int Oral Health. 2014;6(6):10–3. [PMC free article] [PubMed] [Google Scholar]
- 22.Buxcey AJ, Morgaine KC, Meldrum AM, Cullinan MP. An exploratory study of the acceptability of delivering oral health information in community pharmacies. N Z Dent J. 2012;108(1):19–24. [PubMed] [Google Scholar]
- 23.Maunder PE, Landes DP. An evaluation of the role played by community pharmacies in oral healthcare situated in a primary care trust in the north of England. Br Dent J. 2005;199(4):219–23. doi: 10.1038/sj.bdj.4812614. [DOI] [PubMed] [Google Scholar]
- 24.Heaton LJ, Downing DF, Milgrom P. Pharmacists’ confidence and additional training needed in oral health recommendations. J Dent Res. 2012;91(Spec Iss B):3025. ( www.iadr.org) [Google Scholar]
- 25.Mann RS, Marcenes W, Gillam DG. Is there a role for community pharmacists in promoting oral health? Br Dent J. 2015;218(5):E10. doi: 10.1038/sj.bdj.2015.172. [DOI] [PubMed] [Google Scholar]
- 26.Priya S, Madan Kumar PD, Ramachandran S. Knowledge and attitudes of pharmacists regarding oral health care and oral hygiene products in Chennai city. Indian J Dent Res. 2008;19(2):104–8. doi: 10.4103/0970-9290.40462. [DOI] [PubMed] [Google Scholar]
- 27.Steel BJ, Wharton C. Pharmacy counter assistants and oral health promotion: an exploratory study. Br Dent J. 2011;211(9):E19. doi: 10.1038/sj.bdj.2011.938. [DOI] [PubMed] [Google Scholar]
- 28.Rajiah K, Ving CJ. An assessment of pharmacy students’ knowledge, attitude, and practice toward oral health: An exploratory study. J Int Soc Prev Community Dent. 2014;4(Suppl 1):S56–62. doi: 10.4103/2231-0762.144601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75(1):3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 30.Carr A. Diseases and Conditions – Dry Mouth. [Accessed June 10, 2015];The Mayo Clinic website. http://www.mayoclinic.org/diseases-conditions/dry-mouth/expert-answers/dry-mouth/faq-20058424?reDate=10062015.
- 31.Villa A, Abati S. Risk factors and symptoms associated with xerostomia: a cross-sectional study. Aust Dent J. 2011;56(3):290–5. doi: 10.1111/j.1834-7819.2011.01347.x. [DOI] [PubMed] [Google Scholar]
- 32.Locker D, Matear D, Stephens M, Jokovic A. Oral health-related quality of life of a population of medically compromised elderly people. Community Dent Health. 2002;19(2):90–7. [PubMed] [Google Scholar]
- 33.Thomson W, Poulton R, Broadbent JM, Al-Kubaisy S. Xerostomia and medications among 32-year-olds. Acta Odontol Scand. 2006;64(4):249–54. doi: 10.1080/00016350600633243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomson WM. Dry mouth and older people. Aust Dent J. 2015;60(Suppl 1):54–63. doi: 10.1111/adj.12284. [DOI] [PubMed] [Google Scholar]
- 35.Asahina Y, Hori S, Sawada Y. Understanding of definition and safety of oral health products among patients, physicians and pharmacists. Yakugaku Zasshi. 2010;130(7):961–9. doi: 10.1248/yakushi.130.961. [DOI] [PubMed] [Google Scholar]
- 36.Wamsley M, Staves J, Kroon L, et al. The impact of an interprofessional standardized patient exercise on attitudes toward working in interprofessional teams. J Interprof Care. 2012;26(1):28–35. doi: 10.3109/13561820.2011.628425. [DOI] [PubMed] [Google Scholar]
- 37.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62(2):122–8. doi: 10.1111/j.1752-7325.2002.tb03432.x. [DOI] [PubMed] [Google Scholar]
- 38.Hay EM, Thomas E, Pal B, et al. Weak association between subjective symptoms or and objective testing for dry eyes and dry mouth: results from a population based study. Ann Rheum Dis. 1998;57(1):20–4. doi: 10.1136/ard.57.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]