Abstract
Purpose
To examine age-varying prevalence rates and health implications of weapon-related violence exposure from adolescence to young adulthood (ages 14–30) using time-varying effect modeling (TVEM).
Methods
Data were from the Add Health study, a longitudinal study of adolescents in the United States (N = 5,103) followed into young adulthood across 4 assessment waves from age 14–30.
Results
Weapon-related violence exposure (WRVE) rates varied with age, peaking during mid-to-late adolescence (ages 16–18). Rates were higher for males (versus females) and African-American youth (versus White) across nearly all ages. Rates were higher for Hispanic youth (versus White) during adolescence. WRVE was positively associated with frequent heavy episodic drinking (HED) and negatively associated with self-reported general health; these associations were significant during adolescence and early adulthood (ages 15–24). WRVE was positively associated with depressive symptoms. This association remained stable over age and was stronger for females from ages 16–21. The association between violence exposure and decreased general physical health was stronger for White versus African-American youth from ages 15–17, with no significant association observed for African-American youth at any age.
Conclusions
Despite its severity, WRVE is prevalent among US youth during adolescence and young adulthood, particularly among males and African-Americans during mid-to-late adolescence. The associations between WRVE and health were stronger during adolescence and differed by sex and race/ethnicity. This information may assist in the timing and targeting of intervention efforts aimed at interrupting the effects of violence exposure on youth behavioral, mental, and physical health.
Keywords: weapon-related violence exposure, adolescent health, heavy episodic drinking, depressive symptoms, age-varying associations
Introduction
Weapon-related violence exposure (WRVE) is common among youth in the United States (US). Between 12%–26% of youth under 18 have experienced WRVE in their lifetimes (1, 2); 6%–8% of adolescents ages 14–17 report WRVE in the past year (3). Rates among young adults are also high; 12% of adults aged 18–27 have been exposed to past-year community violence, including weapon-related violent events such as seeing someone stabbed or shot, being threatened with a knife or gun, and being stabbed or shot themselves (4). WRVE rates vary substantially by sex (higher in males) and race/ethnicity (higher in African-American and Hispanic youth), highlighting the unequal distribution of violent experiences among youth (3, 4).
Much of the research on weapon-related violence has focused on weapon-carrying among youth and less on youth exposure to weapon-related violence (2). Violence exposure is important to understand not only because it has direct links with morbidity and mortality but also because it is associated with myriad behavioral, mental, and physical health problems, including substance use (5, 6), delinquency (7), post-traumatic stress disorder (8), depression and anxiety (9, 10), sexual-risk behavior (6), and poor self-reported health (11). Associations between violence exposure and poor outcomes have been documented in a number of developmental periods, including childhood, adolescence, and young adulthood (6, 8, 11, 12); however, few studies have examined how the manifestations and implications of violence exposures may vary across developmental periods within the same study. A developmental perspective such as this is essential because an individual’s cognitive, emotional, and physical capacities influence how they respond to and to cope with violent events, and these capacities are changing with development (9, 13). Applying a developmental perspective to violence exposure requires that we examine its changing manifestations and its implications across developmental periods; that is, in the context of the changing lives of individuals (9). Doing so will not only help to improve theory and research, but will aid in our ability to match intervention content to the needs of the person and their developmental stage (14).
The current study uses an innovative statistical approach, time-varying effect modeling (TVEM; 15, 16, 17) to examine the age-varying prevalence rates of WRVE (witnessing violence, threat of violence, and violence victimization) and its age-varying associations with three key health outcomes (frequent heavy episodic drinking [HED], depressive symptoms, and general physical health). Using data from a large longitudinal study of US youth followed from adolescence to young adulthood, we apply TVEM to estimate age-varying associations. Because exposure rates and effects of violence differ by sex and race/ethnicity (3, 4, 18–20) we explored these as moderators of age-varying prevalence rates and health implications of WRVE.
Method
Procedures and participants
Data are from the public-use sample of the National Longitudinal Study of Adolescent to Adult Health (Add Health; 21) a sample of adolescents recruited in grades 7 through 12 in the United States (N=6,504). The sample comprised 80 high schools and feeder middle schools stratified with respect to region, urbanicity, school type and size, and ethnicity. Participants completed surveys in 1994–1995 (Wave I), 1995–1996 (Wave II), 2001–2002 (Wave III), and 2007–2008 (Wave IV). Because TVEM can handle unbalanced number and spacing of measurement occasions, we included all available person-waves of data. However, we restricted our analyses to the age range of 14–30 due to data sparseness outside these ages. Our analytic sample included 17,300 person-waves of data across 5,103 adolescents (49% male; 64% non-Hispanic White, 19% non-Hispanic Black or African-American, 12% Hispanic/Latino, 4% Asian, <1% Native American, and <1% other). Of the 5,103 adolescents at Wave 1, 86% (n=4,373), 89% (n=4,556), and 64% (n=3,268) were followed up at Waves II, II, and IV respectively. Data collection was approved by the Public Institutional Review Board at the University of North Carolina.
Measures
All study measures were assessed during in-home interviews at each wave.
WRVE over the past year included (i) witnessing weapon-related violence (“You saw someone shoot or stab another person”, 8.6% of occasions), (ii) threat of weapon-related violence (“Someone pulled a knife or gun on you”; 9.3% of occasions), and (iii) weapon-related violence victimization (“Someone shot, cut, or stabbed you”, 3.7% of occasions). WRVEs were highly interrelated at each wave (α=.57–.82) as in previous research (22, 23). Thus, we combined exposures into a WRVE composite ranging from 0 to 3 (M=0.22, SD=0.60).
Frequent heavy episodic drinking (HED) was assessed using the item “During the past 12 months, on how many days did you drink five or more drinks in a row?” at waves 1–3 and “… five or more (if male) or four or more (if female) drinks in a row?” at wave 4. As in previous research (24), we considered HED to be frequent if it occurred at least twice a month. Frequent HED was reported on 17.8% of occasions.
Depressive symptoms during the past week were assessed using 8 items from the Center for Epidemiological Studies Depression Scale (CES-D; 25). A sample item is “You felt sad”; responses included 0=never or rarely, 1=sometimes, 2=a lot of the time, 3=most or all of the time (α=.78–.81 across waves).
General physical health was assessed using the item: “In general, how is your health?” Responses included excellent, very good, good, fair, or poor. Consistent with previous research (11), we dichotomized the responses and coded 1= good or better (excellent, very good, or good health, =1) and 0=fair or poor health. Physical health was good in this sample, reflecting the developmental period; good or better health was reported on 93.3% of occasions.
Covariates included the following, in addition to sex and race/ethnicity. Family disadvantage before age 18 was coded at each of the four waves following methods of Add Health investigators (26). Family disadvantage was indicated if (i) the parent reported that family income fell below $16,000 at wave 1 (less than or equal to poverty level in 1994), and (ii) family welfare receipt before age 18 was reported from either family information (waves 1–2) or participant retrospective report (waves 3–4); 30% of respondents experienced family disadvantage. Violence perpetration was assessed using two items at each of the four waves. Respondents were asked whether they “pulled a knife or gun on someone” or “shot or stabbed someone” in the past year; a score of 1 was assigned if either was reported (0 if neither). Violence perpetration was reported on 3.8% of occasions.
Statistical Analyses
The TVEM SAS Macro (36) was used for all analyses. TVEM is a direct extension of multiple regression allowing intercept and slope coefficients to be estimated as non-parametric functions of continuous age (17, 24). These functions are non-parametric because TVEM, in contrast to multiple regression and multilevel modeling, requires no constraints on the shapes of the intercept and slope functions across age. Instead, shapes are estimated from the available data with the only assumption that changes with time happen in a smooth way. These models used a P-spline approach to split complex functions into numerous segments, each of which is estimated with a polynomial model. All models used “sandwich” error estimation to adjust for the clustering of observations within adolescents (27). Additional technical details of TVEM can be found elsewhere (15).
Analyses proceeded in three steps. First, we estimated age-varying levels of WRVE by sex and race/ethnicity using intercept-only Poisson TVEM. Separate models tested for the age-varying association between sex (including all racial/ethnic groups) and race/ethnicity (including only White, African-American, and Hispanic). Significance by sex and race/ethnicity was evaluated by generating group-specific functions from model estimates and declaring significance only where the confidence intervals of these did not overlap. This approach is more conservative than testing the significance of a difference between two groups (28) and was used to control Type I error. We followed these models by testing sex and racial/ethnic differences for each of the three exposure types (using logistic TVEM for each dichotomous exposure) only where significant differences in the composite were found.
Second, we tested age-varying associations between the WRVE composite and each of the three health outcomes (HED, depressive symptoms, and general physical health). Binary HED and physical health outcomes were modeled using logistic TVEM; the continuous normal depressive symptom score was modeled using normal TVEM. These models included sex, race/ethnicity, low income, and violence perpetration as covariates.
Third, we tested whether these age-varying WRVE associations with health outcomes were moderated by sex and race/ethnicity by testing Sex × WRVE and Race/Ethnicity × WRVE interactions in separate models. We evaluated significance of moderation by generating group-specific functions from model estimates and declaring significance only where confidence intervals did not overlap. Models testing moderation by sex controlled for race/ethnicity (all race/ethnicity groups included), family disadvantage, and violence perpetration. Models testing moderation by race/ethnicity controlled for sex, family disadvantage, and violence perpetration and included only youth in White, African-American, and Hispanic groups.
Results
Figure 1 shows the age-varying WRVE count (Panel A) and prevalences of each WRVE type (Panels B, C, and D) by sex. The bolded curves represent the age-varying WRVE levels; the dashed lines represent 95% confidence intervals. Males were exposed to significantly more violence at all ages. Each exposure type was more prevalent in males than females at nearly all ages. Peak rates of witnessing violence (males: 14.58%, age 17.1; females: 9.57%, age 15.6), threat of violence (males: 19.62%, age 17.6; females: 6.53%, age 16.4), and violence victimization (males: 7.64%, age 16.7; females: 3.48%, age 15.6) occurred during adolescence. Exposure rates declined during the transition into young adulthood, rising somewhat after age 25.
Figure 1.
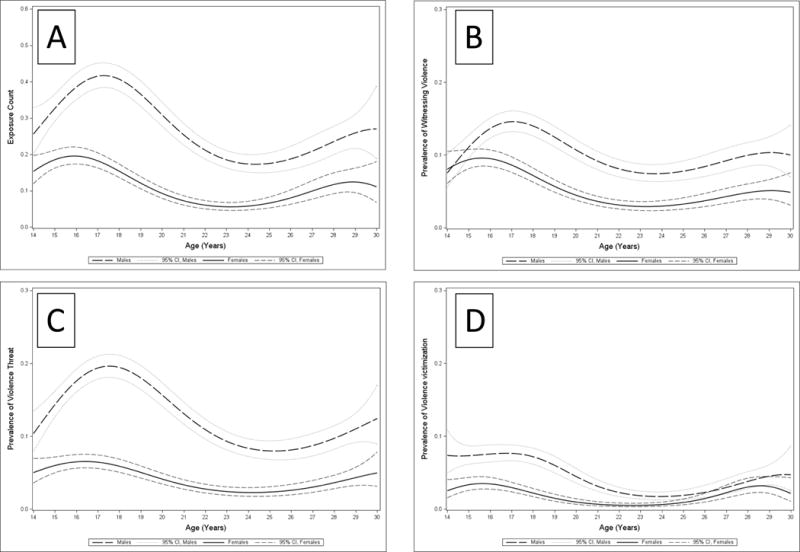
Age-varying level of weapon-related violence exposure composite (Panel A), and prevalences of witnessing weapon-related violence (Panel B), weapon-related violence threat (Panel C), and weapon-related violence victimization (Panel D), by sex.
Figure 2 shows the age-varying WRVE count (Panel A) and prevalences of WRVE types (Panels B, C, and D) by race/ethnicity. African-Americans were exposed to more violence than White youth at nearly all ages; Hispanic youth were exposed to more violence than White youth from ages 15–24. Panels B, C, and D explore rates of WRVE types by race/ethnicity. African-Americans were significantly more likely than White youth to witness violence across all ages, and were more likely to be threatened by violence from ages 15–30. From ages 15–21 and 27–30, African-Americans were significantly more likely to be victimized than White youth. Compared to White youth, Hispanic youth were significantly more likely to witness violence at all ages, be threatened by violence from ages 15–22, and slightly more likely to be victimized by violence from ages 16–17. Hispanic youth were significantly less likely than African-American youth to witness violence from ages 20–24 but these groups did not differ significantly in their rates of violence threat or victimization at any age. Peak rates of witnessing violence (African-American: 21.26%, age 17.1; White: 7.40%, age 15.8; Hispanic: 19.85%, age 16.4), threat of violence (African-American: 18.23%, age 17.7; White: 10.37%, age 17.1; Hispanic: 17.99%, age 17.2), and violence victimization (African-American: 8.84%, age 17.2; White: 4.50%, age 15.3; Hispanic: 7.14%, age 16.1) were seen during adolescence.
Figure 2.
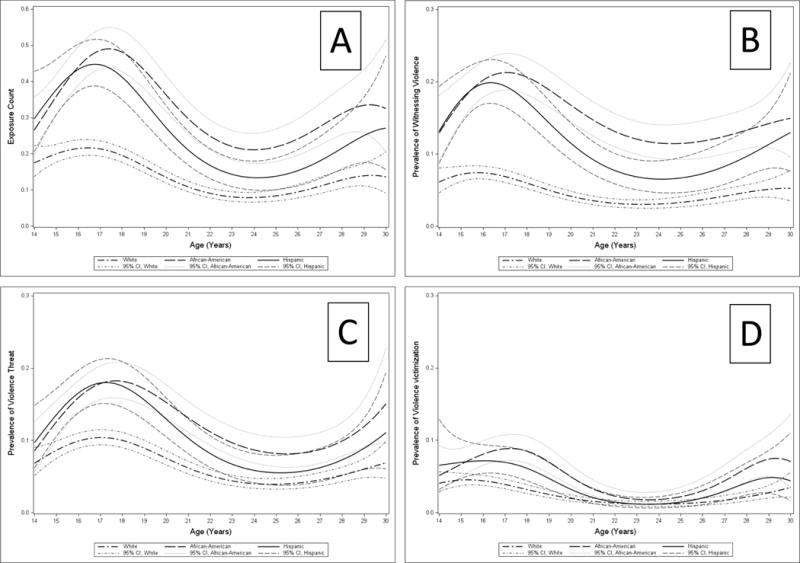
Age-varying level of weapon-related violence exposure composite (Panel A), and prevalences of witnessing weapon-related violence (Panel B), weapon-related violence threat (Panel C), and weapon-related violence victimization (Panel D), by race/ethnicity.
Figure 3 shows age-varying associations between the WRVE composite and frequent HED (Panel A), depressive symptoms (Panel B), and general physical health (Panel C). The association for HED is positive and significant until approximately age 24. The maximum effect size was observed at age 14.0 (OR=1.91); it declined steadily with age. For depressive symptoms, the association was significant at all ages and was strongest at age 14.0 (β=0.25), declining through adolescence until approximately age 17, thereafter remaining fairly constant. WRVE was associated with lower odds of good physical health from ages 15–24, but was not associated outside these ages. The association was strongest at age 20.9 (OR=0.61).
Figure 3.
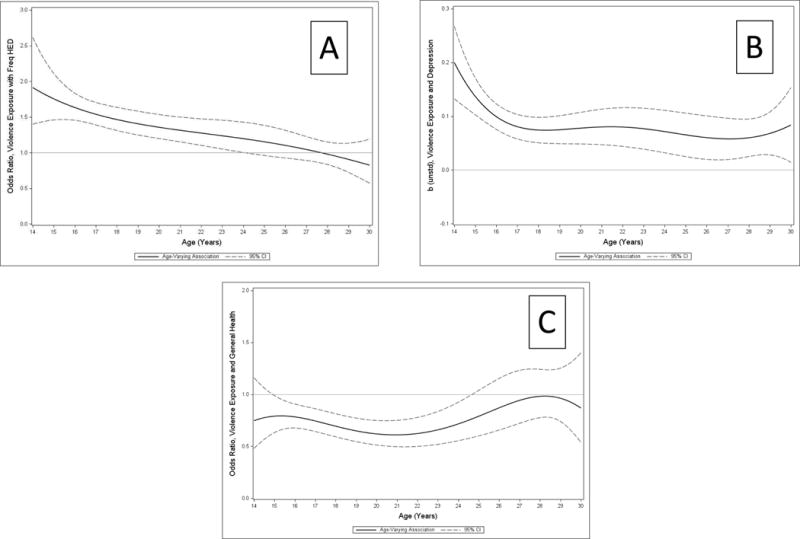
Age-varying associations between weapon-related violence exposure composite and frequent HED (Panel A), depressive symptoms (Panel B), and general physical health (Panel C), full sample. b(unstd) = unstandardized regression coefficient.
Figure 4 shows the age-varying association between WRVE and depressive symptoms by sex and reveals a significant difference from late adolescence to early adulthood. From ages 16–21, the association between WRVE and depressive symptoms becomes significantly stronger for females. We found no evidence for sex differences in age-varying associations between WRVE and frequent HED or physical health.
Figure 4.
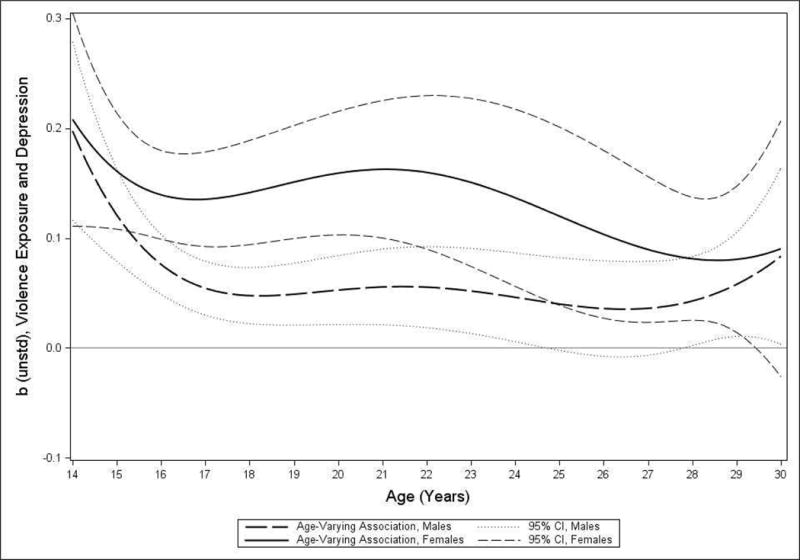
Age-varying association between weapon-related violence exposure composite and depressive symptoms by sex. b(unstd) = unstandardized regression coefficient.
Figure 5 shows that the WRVE association with general health was significant for White versus African-American youth between ages 15–17. The WRVE association with physical health was significant for White youth from ages 14 to approximately 24, whereas this association was never significant for African-Americans. We found no other significant differences in WRVE associations by ethnicity.
Figure 5.
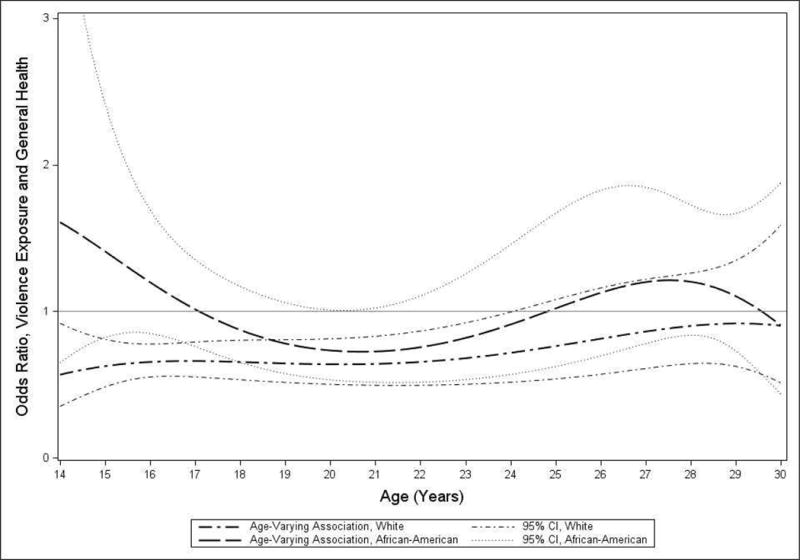
Age-varying associations weapon-related violence exposure composite and general physical health by race/ethnicity (African-American versus White).
Discussion
We used TVEM to understand the age-varying prevalence and health implications of past-year WRVE in a large longitudinal study of youth from ages 14–30. Examining these questions in a longitudinal study provides confidence that our results more closely reflect developmental patterns compared to studies examining age differences in a repeat cross-sectional design. WRVE rates were highest during mid-to-late adolescence (ages 16–18) for all exposure types. Consistent with national statistics (3), our results show that males and minority (African-American and Hispanic) youth experience higher rates of WRVE than females and White youth, and these differences persist across adolescence and young adulthood. Despite their severity, WRVE rates were high; for example, approximately 20% of African-American and Hispanic youth witnessed weapon-related violence during late adolescence. WRVE rates were lower during early adulthood (ages 20–25) for nearly all demographic subgroups and all exposure types, but increased from ages 25–30. Although this increase may align with previous research suggesting that violence exposure rates in young adulthood appear comparable to rates in adolescence (29), this finding was unanticipated with regard to WRVE and warrants continued investigation.
Associations between WRVE and health outcomes revealed intriguing patterns across age. Associations with frequent HED and depressive symptoms were strongest at the earliest ages (14–15) whereas the association with general physical health was strongest in early adulthood (age 20). The strength of WRVE associations with frequent HED and depressive symptoms at age 14 may partly reflect selection effects, as broader contextual or individual risk factors such as poverty or pre-existing behavior problems might explain the co-occurrence of weapon-related violence, frequent HED, depressive symptoms at such early ages. However, the fact that these associations were present even after adjusting our models for sex, race/ethnicity, family disadvantage, and violence perpetration gives us confidence that these associations may reflect WRVE effects on health. Our findings also showed that the WRVE association with depressive symptoms remained significant from ages 14–30, whereas WRVE associations with frequent HED and general health showed a “fade out”, becoming nonsignificant by approximately age 24. For frequent HED, this fade out may occur partly as a function of heavy alcohol use becoming more normative during the early 20s. For general health, it is not entirely clear why this was observed; it may reflect changing determinants of general perceived health during young adulthood, including more proximal day-to-day factors like income, diet, exercise, and stress.
We found that WRVE was more strongly associated with depressive symptoms for females than males during late adolescence and early adulthood (approximately ages 16–21). The stronger association between WRVE and depressive symptoms among females during adolescence and early adulthood likely reflects a heightened general vulnerability for depression among females (30), combined with intensifying socialization pressures during adolescence and young adulthood that may exacerbate this vulnerability (31). We found a small but significant difference in the WRVE association with general health for White versus African-American youth during middle adolescence (ages 15–17). The WRVE association with physical health was significant for White youth from ages 14–24, but was not significant at any age for African-American youth. Although reduced effects of violence exposure among African-American youth have been reported in previous research (7); the current study shows that these reduced effects may be present across adolescence and young adulthood. One potential explanation for this reduced association between WRVE and health may include desensitization, whereby youth who are exposed to high levels of violence become less reactive to its effects (32, 33). Another potential explanation may include differences in cultural practices that may protect against violence exposure effects. One example is racial socialization, a practice in which parents teach youth about their racial/ethnic heritage and promote youths’ cultural pride (34); racial socialization has been shown to be protective against community violence exposure effects for African-American youth (35).
Our findings may have implications for the timing of intervention. Overall, WRVE associations with health outcomes appeared most pronounced during adolescence, reinforcing the idea of this developmental period as an important window of opportunity for prevention. For example, our finding that an association between violence exposure and frequent HED is already present at age 14 suggests that interventions targeting violence exposure during this time could have impacts on the prevention of alcoholism, given the known association between early-onset drinking and adult dependence (36). Our findings showing age-varying moderation of WRVE associations highlight the importance of considering demographic factors in addition to developmental stage during intervention planning. Interventions targeting links between violence exposure and physical health may be especially important for White youth during middle adolescence (ages 15–17), and interventions targeting links between violence exposure and depressive symptoms may be especially important for females during late adolescence and early adulthood.
This study has several limitations. First, because WRVE and health outcomes were assessed contemporaneously, we cannot make inferences about directionality, an important limitation given previous research showing bidirectional associations between violence exposure and some outcomes (37). However, previous research in Add Health has shown predictive effects of WRVE on health outcomes (4, 38), giving us some confidence in our interpretations. Second, given our focus on WRVE, the violence composite we used was less broad than those used in other studies. However, we note that research on polyvictimization has shown that youth experiencing WRVE are substantially more likely to be experiencing other types of violence exposure (2), suggesting that WRVE may function as a proxy for other violence exposure types. Third, because our main goal was to examine the age-varying health implications of WRVE, our selection of health indicators was limited to a smaller set than may be ideal. Future research might also include outcomes such as PTSD, anxiety disorders, injury, illness, and stress-influenced biomarkers such as metabolic syndrome and systemic inflammation. Fourth, we were unable to explore the context of WRVEs, such as the identity of the perpetrator (stranger, friend, significant other) or the setting in which these events occurred, as this information was unavailable in Add Health. Fifth, the unequal spacing of measurement points, with waves 1–2 being closer in time than waves 3–4, created a higher density of observations and lower attrition rates in the adolescent years, which may have resulted in tighter confidence intervals and increased statistical power at these ages relative to later ages. Future research examining these associations with denser sampling of waves in young adulthood is needed. Sixth, due data sparsity before age 14, we were unable to examine WRVE associations at younger ages, such as early adolescence (i.e., ages 10–13) when the impact of exposures may be particularly strong given evidence for increased biological sensitivity to social environment (39). Future studies testing for age-varying WRVE associations among children and younger adolescents are needed.
Conclusions
Our results identify mid-to-late adolescence as a period of high vulnerability for WRVE; during this period, exposure rates appear highest and associations with health outcomes appear strongest. Significant differences by sex and race/ethnicity in age-varying WRVE associations with health markers suggest that vulnerability may shift differentially with age across demographic groups. As suggested by Coyle and DiClemente (14), this type of information may enhance intervention effectiveness by providing details informative for the tailoring (by sex or race/ethnicity), timing (within specific age windows), and targeting (by focusing on specific health outcomes) of interventions aimed at buffering the toxic effects of WRVE.
Implications and Contribution.
This study investigated weapon-related violence exposure (WRVE) across adolescence and young adulthood. WRVE was highest during adolescence and differed by sex and race/ethnicity. WRVE age-varying associations were stronger with depressive symptoms for females and with physical health for White versus African-American youth.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. Preparation of this article was supported by awards T32 DA017629 (PI: Collins), P50 DA010075 (PI: Collins) and P50 DA039838 (PI: Collins). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. The authors would like to thank Amanda Applegate for her comments on a previous draft of this manuscript. Portions of this work were presented at the 2015 Society for Prevention Research annual meeting in Washington, D.C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure: All authors declare that they have no conflicts of interest.
References
- 1.Finkelhor D, Shattuck A, Turner H, et al. A revised inventory of adverse childhood experiences. Child Abuse Neglect. 2015;48:13–21. doi: 10.1016/j.chiabu.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell KJ, Hamby SL, Turner HA, et al. Weapon involvement in the victimization of children. Pediatrics. 2015;136:10–17. doi: 10.1542/peds.2014-3966. [DOI] [PubMed] [Google Scholar]
- 3.Kann L, Kinchen S, Shanklin S, et al. Youth risk behavior surveillance — United States, 2013. Morbidity and Mortality Weekly Report. 2014;63 [PubMed] [Google Scholar]
- 4.Voisin DR, Chen P, Fullilove R, et al. Community violence exposure and sexual behaviors in a nationally representative sample of young adults: The effects of race/ethnicity and gender. J Soc Serv Res. 2015;41:295–306. doi: 10.1080/01488376.2014.987941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zinzow HM, Ruggiero KJ, Hanson RF, et al. Witnessed community and parental violence in relation to substance use and delinquency in a national sample of adolescents. J Trauma Stress. 2009;22:525–533. doi: 10.1002/jts.20469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brady SS. Lifetime community violence exposure and health risk behavior among young adults in college. J Adolescent Health. 2006;39:610–613. doi: 10.1016/j.jadohealth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Fowler PJ, Tompsett CJ, Braciszewski JM, et al. Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol. 2009;21:227–259. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- 8.Margolin G, Vickerman KA. Posttraumatic stress in children and adolescents exposed to family violence: I. Overview and issues. Couple Family Psychol. 2011;1:63–73. [Google Scholar]
- 9.Margolin G, Gordis EB. The effects of family and community violence on children. Annu Rev Psychol. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- 10.Slopen N, Fitzmaurice GM, Williams DR, et al. Common patterns of violence experiences and depression and anxiety among adolescents. Soc Psych Psych Epid. 2012;47:1591–1605. doi: 10.1007/s00127-011-0466-5. [DOI] [PubMed] [Google Scholar]
- 11.Boynton-Jarrett R, Ryan LM, Berkman LF, et al. Cumulative violence exposure and self-rated health: Longitudinal study of adolescents in the United States. Pediatrics. 2008;122:961–970. doi: 10.1542/peds.2007-3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: A systematic review. Pediatrics. 2006;117:e278–e290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- 13.Finkelhor D. Developmental victimology. In: Davis RC, Luirigio AJ, Herman S, editors. Victims of crime. Thousand Oaks, CA: Sage; 2007. pp. 9–34. [Google Scholar]
- 14.Coyle KK, DiClemente RJ. Time-varying risk behaviors among adolescents: Implications for enhancing the effectiveness of sexual risk reduction interventions. J Adolescent Health. 2014;55:465–466. doi: 10.1016/j.jadohealth.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Tan X, Shiyko MP, Li R, et al. A time-varying effect model for intensive longitudinal data. Psychol Methods. 2012;17:61–77. doi: 10.1037/a0025814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shiyko M, Lanza S, Tan X, et al. Using the time-varying effect model (TVEM) to examine dynamic associations between negative affect and self confidence on smoking urges: Differences between successful quitters and relapsers. Prev Sci. 2012;13:288–299. doi: 10.1007/s11121-011-0264-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vasilenko SA, Lanza ST. Predictors of multiple sexual partners from adolescence through young adulthood. J Adolescent Health. 2014;55:491–497. doi: 10.1016/j.jadohealth.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buka SL, Stichick TL, Birdthistle I, et al. Youth exposure to violence: Prevalence, risks, and consequences. Am J Orthopsychiat. 2001;71:298–310. doi: 10.1037/0002-9432.71.3.298. [DOI] [PubMed] [Google Scholar]
- 19.Moore CG, Probst JC, Tompkins M, et al. The prevalence of violent disagreements in US families: Effects of residence, race/ethnicity, and parental stress. Pediatrics. 2007;119:S68–S76. doi: 10.1542/peds.2006-2089K. [DOI] [PubMed] [Google Scholar]
- 20.Crouch JL, Hanson RF, Saunders BE, et al. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. J Community Psychol. 2000;28:625–641. [Google Scholar]
- 21.Harris KM. The Add Health Study: Design and accomplishments. Chapel Hill, NC: Carolina Population Center, University of North Carolina, Chapel Hill; 2013. [Google Scholar]
- 22.Finkelhor D, Turner HA, Shattuck A, et al. Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatr. 2013;167:614–621. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- 23.Finkelhor D, Turner H, Ormrod R, et al. Children’s exposure to violence: A comprehensive national survey. Washington, D.C.: U.S Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; 2009. [Google Scholar]
- 24.Evans-Polce RJ, Vasilenko SA, Lanza ST. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: Ages 14 to 32. Addict Behav. 2015;41:218–222. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 26.Lee H, Harris KM, Gordon-Larsen P. Life course perspectives on the links between poverty and obesity during the transition to young adulthood. Popul Res Policy Rev. 2009;28:505–532. doi: 10.1007/s11113-008-9115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986:13–22. [Google Scholar]
- 28.Schenker N, Gentleman JF. On judging the significance of differences by examining the overlap between confidence intervals. Am Stat. 2001;55:182–186. [Google Scholar]
- 29.Scarpa A. Community violence exposure in young adults. Trauma Violence Abuse. 2003;4:210–227. doi: 10.1177/1524838003004003002. [DOI] [PubMed] [Google Scholar]
- 30.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- 31.Nolen-Hoeksema S. Gender differences in depression. Curr Dir Psychol Sci. 2001;10:173–176. [Google Scholar]
- 32.Mrug S, Loosier PS, Windle M. Violence exposure across multiple contexts: Individual and joint effects on adjustment. Am J Orthopsychiat. 2008;78:70–84. doi: 10.1037/0002-9432.78.1.70. [DOI] [PubMed] [Google Scholar]
- 33.Gaylord-Harden NK, Cunningham JA, Zelencik B. Effects of exposure to community violence on internalizing symptoms: Does desensitization to violence occur in African American youth? J Abnorm Child Psych. 2011;39:711–719. doi: 10.1007/s10802-011-9510-x. [DOI] [PubMed] [Google Scholar]
- 34.Hughes D, Rodriguez J, Smith EP, et al. Parents’ ethnic-racial socialization practices: A review of research and directions for future study. Dev Psychol. 2006;42:747–770. doi: 10.1037/0012-1649.42.5.747. [DOI] [PubMed] [Google Scholar]
- 35.Henry JS, Lambert SF, Smith Bynum M. The protective role of maternal racial socialization for African American adolescents exposed to community violence. J Fam Psychol. 2015;29:548–557. doi: 10.1037/fam0000135. [DOI] [PubMed] [Google Scholar]
- 36.Zucker RA. Anticipating problem alcohol use developmentally from childhood into middle adulthood: What have we learned? Addiction. 2008;103:100–108. doi: 10.1111/j.1360-0443.2008.02179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mrug S, Windle M. Bidirectional influences of violence exposure and adjustment in early adolescence: Externalizing behaviors and school connectedness. J Abnorm Child Psych. 2009;37:611–623. doi: 10.1007/s10802-009-9304-6. [DOI] [PubMed] [Google Scholar]
- 38.Turanovic JJ, Pratt TC. Longitudinal effects of violent victimization during adolescence on adverse outcomes in adulthood: A focus on prosocial attachments. J Pediatr. 2015;166:1062–1069.e1061. doi: 10.1016/j.jpeds.2014.12.059. [DOI] [PubMed] [Google Scholar]
- 39.Crone EA, Dahl RE. Understanding adolescence as a period of social-affective engagement and goal flexibility. Nat Rev Neurosci. 2012;13:636–650. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]


