Abstract
BACKGROUND/OBJECTIVES
A growing body of research has indicated that night eating could be associated with poor diet quality and negative health outcomes. This study examined the nutritional aspects of night eating, its related factors, and the association between night eating and body weight among Korean adolescents.
SUBJECTS/METHODS
This study analysed the data from a one day 24-hour dietary recall as well as a demographic survey of 1,738 Korean adolescents aged 12 to 18-years-old obtained from the 2010-2012 Korea National Health and Nutrition Examination Survey. 'Night eating' was defined as consuming 25% or more of one's daily energy intake between 21:00 and 06:00. Subjects complying with the preceding condition were classified as 'night eaters', whereas the rest were considered 'non-night eaters'. Logistic regression analysis examined factors related to night eating. Multiple linear regression analyses were used to examine the relationship between night eating and BMI z-scores, whereas multinomial logistic regression analysis was used to examine the relationship between night eating and weight status.
RESULTS
About 21% of Korean adolescents appeared to be night eaters. Night eaters showed increased breakfast skipping (P = 0.001), higher energy intake from snacks (P < 0.001), greater proportion of energy intake from fat (P = 0.029), and lower Dietary Diversity Scores (P = 0.008) than non-night eaters. Male adolescents presented 1.9 times higher odds of being night eaters than females. Adolescents whose both parents were night eaters were 4.4 times as likely to be night eaters as those whose neither parents were. Female adolescents showed a significant relationship between night eating and BMI z-scores (β = 0.28, P = 0.004). However, night eating did not increase odds of being overweight or obese in adolescents.
CONCLUSIONS
Night eating in Korean adolescents was related to undesirable dietary behaviours and low diet quality in general as well as higher BMI z-scores in females. Male gender and parental night eating appeared to be the factors that significantly increased odds of night eating. These results suggest that night eating should be considered when designing nutrition education or intervention programs targeting adolescents.
Keywords: Nutrition survey, eating behavior, obesity, BMI, body weight
INTRODUCTION
Adolescence is characterized by critical changes in several aspects of life. Among these, a rapid growth spurt in both height and weight is one of the most evident physical transformations. These changes, along with modifiable factors, place adolescents at a higher risk category for weight-related health problems [1].
Worldwide the prevalence of obesity and overweight has increased among children and adolescents, becoming an epidemic in both developing and developed nations [2]. South Korea is not exempt from this global trend. From 2008 to 2012, the prevalence of obesity in children and adolescents increased from 11.2% to 14.7% [3]. Some elements associated with higher likelihood of obesity amongst South Korean adolescents are low socio-economic status, dietary patterns, and sitting more than 2 hours per day [4].
Diet is an important modifiable factor influencing weight status. Research has shown associations between changes in Korean adolescents' diet over time and an increased risk of being overweight [5]. Recently, temporal distribution of food consumption has emerged as a possible culprit in the association between diet and weight status. The combination of timing of food intake and specific nutrient profiles has been associated with metabolic abnormalities [6]. For instance, breakfast skipping has been related to obesity in the general population [7,8], and evidence has suggested its link with increased weight gain during the transition from adolescence to adulthood [9].
In particular, food intake during night time has been associated with lower diet quality in children [10], adolescents [11], and adults [12] as well as a higher Body Mass Index (BMI) and greater likelihood of being obese [13,14]. In both South Korea and the United States, night eating has shown a greater prevalence among young adults [15,16,17], and most studies on this topic in South Korea have focused on this population [18,19,20]. To our knowledge, only one study to date has analysed the phenomenon of night eating in adolescents. The study investigated night eating habits in middle school students living in Gyeonggi province and concluded that night food intake predominantly consisted of carbohydrate and fat-rich foods [11]. Nevertheless, until now, no other studies have reported a possible relationship between night eating and body weight in South Korea. Hence, the purpose of the current study was to examine nutritional aspects and factors associated with night eating as well as the relationship of night eating with BMI and weight status among Korean adolescents.
SUBJECTS AND METHODS
Data source and subjects
The data used in this study were obtained from the 2010-2012 Korea National Health and Nutrition Examination Survey (KNHANES V), conducted by Centers for Disease Control and Prevention in Korea. This survey was approved by the Institutional Review Board (IRB) of Centers for Disease Control and Prevention in Korea (IRB approval number: 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C). A final sample of 1,738 subjects was selected from an initial number of 2,193 subjects aged 12-18 years; 424 subjects were excluded because of missing values for major target variables, such as dietary data and anthropometric measures, and 31 subjects were excluded for reporting implausible energy intakes (< 500 or ≥ 5,000 kcal per day). The same exclusion criteria were applied to the analysis of night eating in the general Korean population in order to determine the prevalence of night eating in other age groups for comparative purposes.
Night eating criteria
Investigation of night eating seems to be complicated due to the lack of uniform definitions of both 'night eating' and the related eating disorder termed 'Night Eating Syndrome' (NES) [18]. While night eating is defined as evening hyperphagia, definitions across different studies show diverse description criteria, mainly differing in the definition of night time. Most studies agree that evening hyperphagia refers to intake of at least 25% of one's total daily calories at night [21]. On the other hand, NES has been classically defined as a behavioural eating disorder that also includes morning anorexia and sleep disturbances in addition to evening hyperphagia [19]. The current study focused on night eating rather than NES. Since it was not possible to reliably assess all criteria for the existence of NES among subjects from the available data, evening hyperphagia was used as a measure of night eating.
In this study, 'night eating' was defined as consuming 25% or more of one's total energy intake [15] between 21:00 and 06:00. This time frame was set based on the usual times for evening and morning meals among the subjects to establish a culturally appropriate definition. The subjects complying with the preceding condition were considered 'night eaters', whereas all others, including subjects who had zero caloric intake, were considered 'non-night eaters'. Since the data were obtained from a one day 24-hour recall, the precise delimitation of night time hours was operationalized into two periods in this study from 00:00 to 06:00 and from 21:00 to 23:59 of the same calendar day.
General characteristics
This study examined age, sex, household income, parental education level, parental night eating habits, breakfast skipping, stress levels, sleep hours, physical activity level, and recent dieting experience as general characteristics. Level of physical activity was classified according to the frequency and time that subjects performed moderate and/or vigorous physical activity per week. Subjects who did not perform any physical activity were classified as 'inactive', whereas those who performed moderate physical activity for at least 30 minutes a day for 5 or more days and/or vigorous physical activity for at least 20 minutes for 3 or more days were classified as 'active'. The rest of the subjects were considered 'inadequately active'.
Dietary assessment
The dietary data used in this study were collected by a 24-hour recall. Energy intake was classified based on whether it was obtained from a meal or a snack and also whether this meal or snack was consumed at night or during daytime. The percentages of energy obtained during the day from carbohydrates, protein, and fat were calculated.
In order to evaluate overall diet quality, two measures of diet quality were calculated: Mean Adequacy Ratio (MAR) and Dietary Diversity Score (DDS). MAR was obtained by calculating the mean value of the Nutrient Adequacy Ratio (NAR) [22] for each of nine nutrients with a Recommended Nutrient Intake (RNI) value according to the Dietary Reference Intakes for Koreans (KDRIs): protein, vitamin A, thiamin, riboflavin, niacin, vitamin C, calcium, phosphorus, and iron [23]. The NAR for a given nutrient is the ratio of a subject's intake to the current recommended allowance for each sex and age category. The MAR was obtained using the formula by Madden et al. [24] calculating the average NAR, and each NAR was truncated at 1 so that a nutrient with a high NAR would not compensate for those with a low NAR.
DDS was used to measure dietary diversity as described by Kant et al. [25]. DDS included the following five food groups: grains (including starches and excluding cakes, pies, cookies, and pastries), meats (including meat, fish, eggs, and beans), fruits (excluding fruit drinks that are not juices), vegetables, and dairies. For calculation of DDS, 1 point was counted for each food group consumed, excluding foods consumed in less than a minimum amount set for each group [26]. For meat, fruit, and vegetable groups, the minimum reported amount for inclusion in the diversity score was 30 g for all solid foods with a single ingredient and 60 g for all liquids and mixed dishes. For dairy and grain groups, the minimum amount of food included was 15 g for all solids and 30 g for all liquids and mixed dishes. DDS values range from 0 to 5 [25].
Assessment of weight status
BMI was obtained by dividing the weight by the square of the height (kg/m2). BMI z-scores were calculated by using LMS (lambda-mu-sigma) parameters, as described by the World Health Organization [27]. A positive z-score indicates a higher-than-average BMI of other children of the same age and sex, whereas a negative z-score indicates a lower-than-average BMI.
Subjects were considered obese if their BMI was at or above the 95th percentile for their age and sex, and they were classified as overweight if their BMI was at or above the 85th and below the 95th percentiles. Subjects below the 5th percentile of BMI were classified as underweight, whereas those at or above the 5th percentile and below the 85th percentile of BMI were classified as healthy weight. The percentiles were obtained according to the cut-offs presented in the Korean National Growth Charts [28].
Statistical analysis
All statistical analyses were performed using IBM SPSS (PASW Statistics 20; SPSS Inc., Chicago IL, USA). The Complex Samples module was used for analysis. This module incorporates adequate sample weights and takes into account the stratification and clustering used in the KNHANES V design. For analyses, the significance level was set at 0.05.
Continuous variables were presented as mean ± standard error (SE), and categorical variables were given as percentages of the total. The Rao-Scott chi-square test was used to examine associations between categorical variables. ANOVA or t-test was used to compare means. Binomial logistic regression was used to assess factors that could be related to night eating. Dietary intake was compared between night eaters and non-night eaters using ANCOVA, adjusted for age and sex.
Multiple linear regression analysis was performed to assess the relationship between night eating and BMI z-score. These models were controlled for variables that have been found to be important covariates in previous studies: age, sex, total energy intake, stress, and sleeping time [10].
Multinomial logistic regression analysis was conducted in order to evaluate the relationship between night eating and weight status. This model was controlled for confounding variables such as age, sex, and total energy intake [10]. This was carried out in order to have a more simplified model with a minimum of variables that could be related to night eating or weight status.
RESULTS
General characteristics and factors related to night eating
Table 1 shows the prevalence of night eating in the general Korean population. Night eating appeared to be more frequent among adolescents. This age group showed the highest prevalence of night eating as well as the highest mean percentage of night energy intake. About 61% of adolescents ate any amount of food during night time while about 21% consumed more than one quarter of their total energy intake during night time and were therefore classified as night eaters for the purpose of this study.
Table 1. Night eating among Korean population across different age groups.
The data were analysed by Complex Samples module.
1) P-values by Rao-Scott chi square test or ANOVA
2) Night eating status indicates whether energy intake between 9 pm and 6 am was equal to or exceeded 25% of total energy intake or not; night eaters: night energy intake ≥ 25% of total energy intake; non-night eaters: night energy intake < 25% of total energy intake
3) n represents unweighted counts.
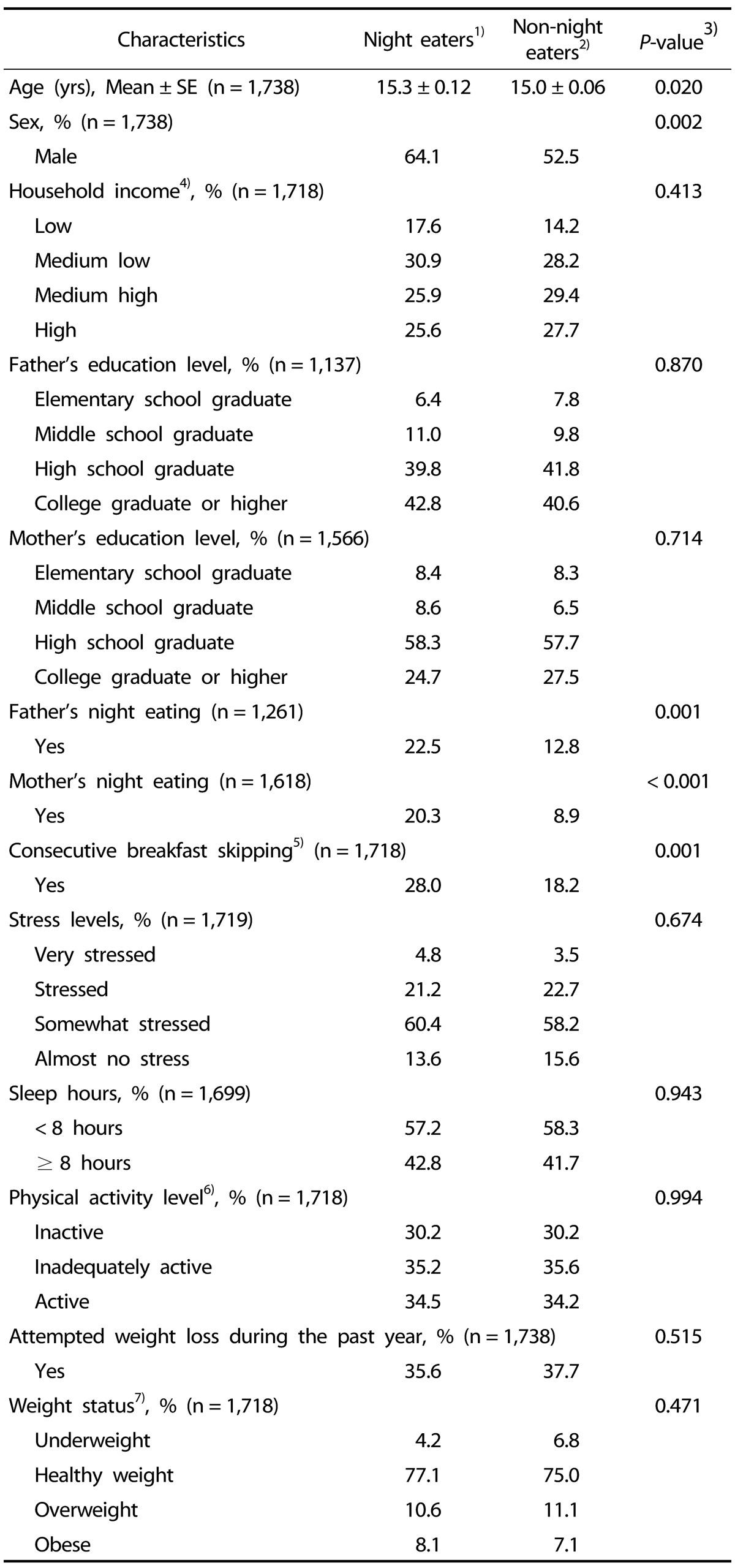
Table 2 presents the characteristics of adolescent night and non-night eaters. Analysis showed significant differences between night and non-night eaters in terms of age, sex, parental night eating, and breakfast skipping. Night eaters exhibited a tendency to be slightly older (15.3-years-old vs. 15.0-years-old). Males predominantly comprised adolescent night eaters, amounting to nearly two thirds. Prevalence of parental night eating was significantly different between night eaters and non-night eaters. Night eaters showed a higher occurrence of consecutive breakfast skipping when compared to non-night eaters (28% vs. 18%, respectively). There was no significant difference between the two groups in terms of socioeconomic status and individual characteristics such as stress level, sleep hours, physical activity, previous attempts to lose weight, and weight status.
Table 2. Characteristics of night eaters and non-night eaters among Korean adolescents.
The data were analysed by Complex Samples module.
1) Night eaters: night energy intake ≥ 25% of total energy intake
2) Non-night eaters: night energy intake < 25% of total energy intake
3) P-values by Rao-Scott chi square test or t-test
4) Average monthly household income based on the minimum cost of living
5) Breakfast skipping was defined as not consuming breakfast during two days in a row (i.e.: the day of the interview, as well as the day before).
6) 'Inactive': no physical activity. 'Active': moderate physical activity for at least 30 minutes a day for five days or more, and/or vigorous physical activity for at least 20 minutes for 3 or more days a week. Remaining subjects: 'Inadequately active'
7) 'Underweight': < 5th BMI percentile. 'Healthy weight': ≥ 5th,, < 85th BMI percentile. 'Overweight': ≥ 85th, < 95th BMI percentile. 'Obese': ≥ 95th BMI percentile
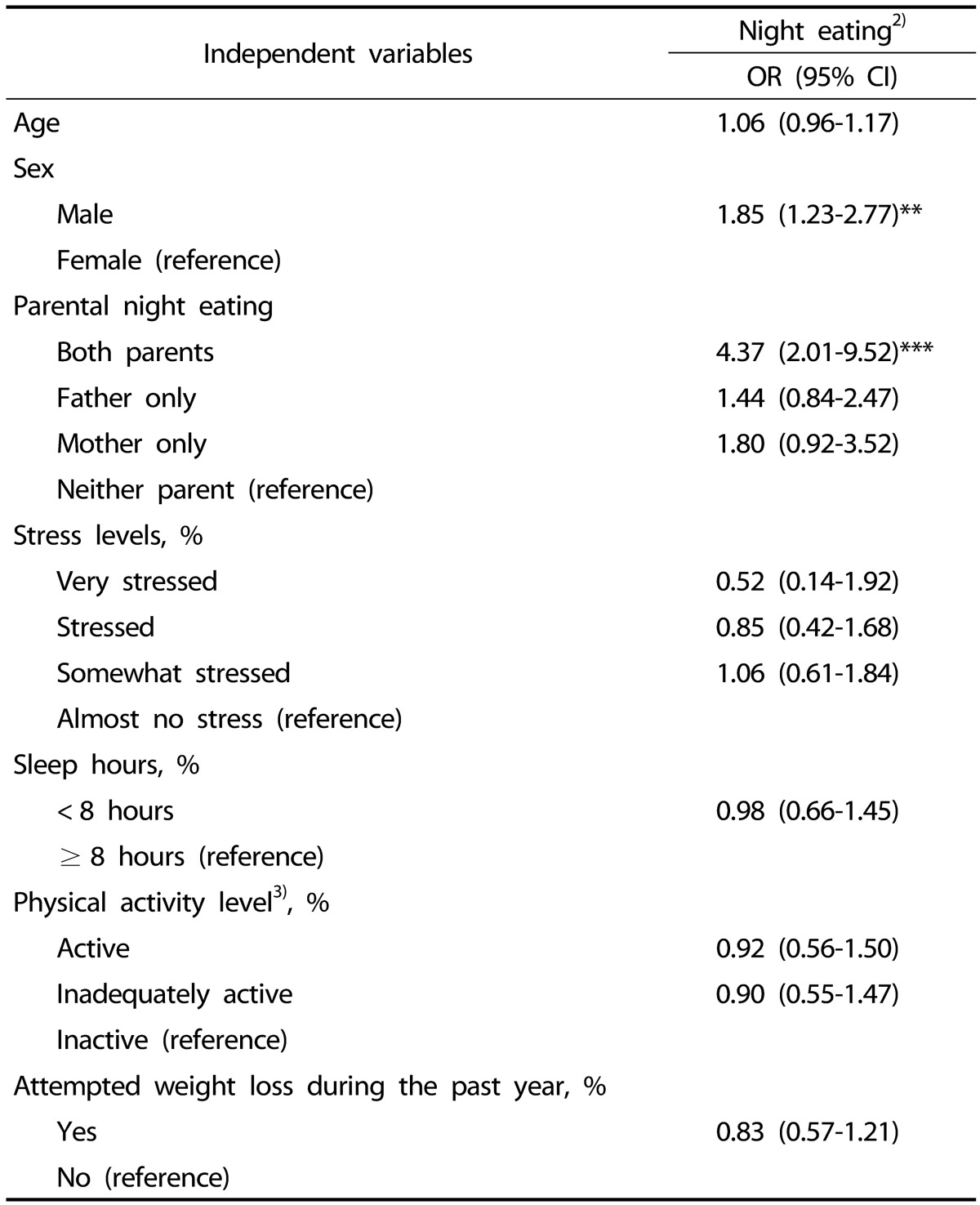
Some of the variables presented in Table 2 were further analysed in order to determine which factors were associated with night eating, as shown in Table 3. The results showed that males had a higher odds of night eating (OR: 1.85, 95% CI: 1.23 - 2.77). Further, having both parents classified as night eaters increased the likelihood of being a night eater (OR: 4.37, 95% CI: 2.01 - 9.52).
Table 3. Factors related to night eating among Korean adolescents1) (n = 1,204).
* P < 0.05, ** P < 0.01, *** P < 0.001
The data were analysed by Complex Samples module.
1) Result of multiple logistic regression analysis
2) Night eating: Night energy intake ≥ 25% of total energy intake
3) 'Inactive': no physical activity. 'Active': moderate physical activity for at least 30 minutes a day for five days or more, and/or vigorous physical activity for at least 20 minutes for 3 or more days a week. Remaining subjects: 'Inadequately active'
Nutritional aspects of night eating
The differences in terms of dietary intake and quality between night eaters and non-night eaters are presented in Table 4. Compared with non-night eaters, night eaters presented not only higher energy intakes at night as expected but also lower energy intakes during the day and higher consumption of energy derived from snacks during both day and night time. The mean percentage of energy from fat was significantly higher in night eaters. When measuring overall diet quality, MAR showed no significant difference between night eaters and non-night eaters, whereas DDS was lower among night eaters.
Table 4. Dietary intake by night eating in Korean adolescents aged 12-18 years old.
The data were analysed by Complex Samples module.
1) Night eaters: Night energy intake ≥ 25% of total energy intake
2) Non-night eaters: Night energy intake < 25% of total energy intake
3) P-values by ANCOVA, adjusted for age and sex
4) Mean Adequacy Ratio; Mean value of the Nutrient Adequacy Ratio.
5) Dietary Diversity Score; Expressed in a scale of 0-5.
Night eating and body weight
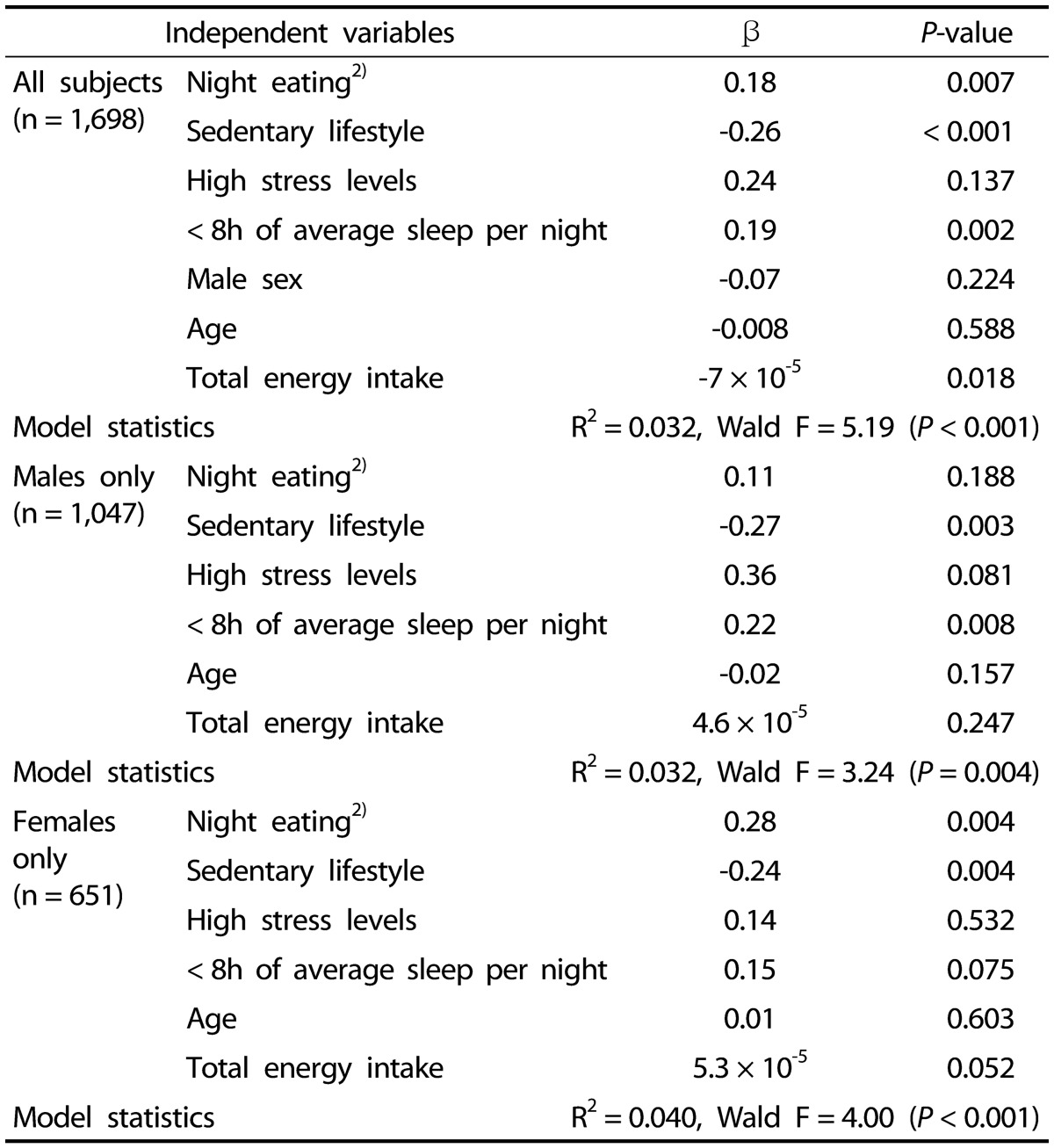
The association of night eating with BMI z-scores was assessed in a linear regression model (Table 5). Analysis showed a significant association between night eating and BMI z-score in all subjects (β = 0.18, P = 0.007). This association appeared to be significant only among female subjects after stratifying for sex (β = 0.28, P = 0.004).
Table 5. Relation of night eating to BMI z-score in Korean adolescents aged 12-18 years old1).
The data were analysed by Complex Samples module.
1) Result of multiple linear regression analyses for the whole sample and the stratified samples according to sex
2) Night eating: Night energy intake ≥ 25% of total energy intake
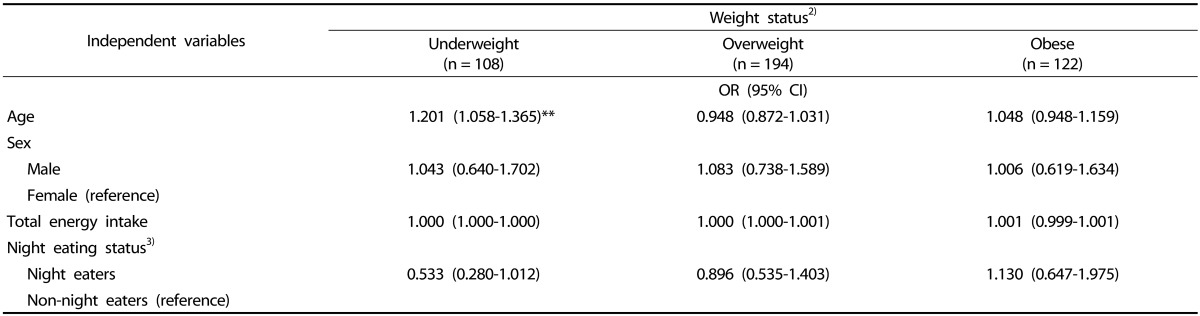
A multinomial logistic regression explored the relationship between night eating and weight status. This model did not identify a significant relationship between night eating and overweight/obesity (Table 6).
Table 6. Relation of night eating to weight status in Korean adolescents aged 12-18 years old1).
* P < 0.05, ** P < 0.01, *** P < 0.001
The data were analysed by Complex Samples module.
1) Result of multinomial logistic regression model. Reference category: healthy weight (n = 1,294). Model statistics: Nagelkerke R2 = 0.023 Wald F = 1.704 (P = 0.061)
2) 'Underweight': < 5th BMI percentile. 'Healthy weight': ≥ 5th,, < 85th BMI percentile. 'Overweight': ≥ 85th, < 95th BMI percentile. 'Obese': ≥ 95th BMI percentile
3) Night eating status indicates whether energy intake between 9 pm and 6 am exceeded 25% of total energy intake or not.; night eaters: night energy intake ≥ 25% of total energy intake; non-night eaters: night energy intake < 25% of total energy intake
DISCUSSION
The results of the present study classified around 21% of Korean adolescents as night eaters, who were defined as subjects consuming 25% or more of their daily energy intake at night. Adolescents showed a significantly higher prevalence of night eating compared to other age groups. On the other hand, children and elders appeared to have a lower prevalence of night eating. These results are in accordance with a recent survey performed in Gyeonggi province, the most populous province in Korea, that identified over 60% of middle school students as eating during night time more than once a week [11]. Other studies in Korea indicated that night eating and snacking were more frequent in younger adults [20,21]. These results indicate that night eating predominantly affects younger populations.
Analysis of night eating in adolescents found some significant differences between night eaters and non-night eaters in terms of sex and parental night eating. According to our results, males presented 85% higher odds of night eating, representing 64% of adolescent night eaters. Previous research showed inconsistent results when exploring sex distribution in night eating. Studies in Korean and international populations have suggested a positive association between males and night eating syndrome or nocturnal snacking [16,17,29]. In contrast, other studies have not showed differences in distribution of night eating between sexes [11,30].
In this study, night eating was associated with parental night eating habits, in agreement with a study involving 6-year-old German children in which risk of night eating was seven times higher in children with mothers who reported night eating themselves [14]. There is evidence that food preferences and selection are strongly influenced by parental choices, and this could not only determine their children's weight status but also the efficacies of weight control interventions [31]. Parental diets appear to be an important factor for adolescents' night eating. This could be related to the fact that evening meals are usually consumed at home, as middle and high school students spend most of their daytime at schools.
Subjects who consumed more than 25% of their daily energy intake at night in the present study had a lower energy intake during daytime as well as a higher prevalence of consecutive breakfast skipping. Morning anorexia, in the form of breakfast skipping, is one of the key features of NES [32]. Although the present research did not focus on NES, it has been proposed that sub-syndrome cases lacking all of the diagnostic criteria for NES should be taken into account due to possible long-term metabolic consequences [33]. It has been suggested that food consumption times have moved to later hours of the day in recent years [34]. With the advent of modern life, schedules and habits have been changing gradually. Variations in daily rhythms due to the use of artificial lighting [35] have also allowed activities and food intake to occur during night hours, which may have a detrimental effect on human metabolic health [36]. Previous reports have stated that delayed eating behaviours were accompanied by a delayed physical activity pattern [37], indicating a possible overall alteration of the circadian biological clock. Although night eaters appear to have delayed eating times, sleep hours and physical activity were not significantly different between night eaters and non-night eaters in this study.
According to our results, night eating appeared to be associated with higher intake of both full meals and snacks during night hours. However, night eating was also found to be associated with a significant increase in energy obtained from snacks. This pattern indicates a possible point of intervention for night eating. Night snacking has been associated with psychological distress [29] and could be related to eating disorder symptoms [38]. Therefore, approaches that target night time snacking and possibly related psychological disturbances may help resolve the root causes of night eating.
In this study, night eating was also associated with lower diet quality, presenting a lower DDS among those with high night energy intake. These results are in accordance with findings in the literature, indicating that evening chronotypes show a tendency to consume less healthy diets. This tendency has been explained by the inclination of individuals with delayed eating patterns to select high carbohydrate and palatable foods during late eating occasions [10].
The present study identified a relationship between night eating and BMI z-cores. A higher energy intake during night time has previously been associated with higher BMI z-scores and higher risk of being overweight or obese [12,13]. Further, behavioural control of evening and night time habits might support weight loss or prevent weight gain beyond usual dieting strategies [39]. In the present study, the mean energy intake from fat was higher among subjects who consumed at least 25% of their calorie intake at night, whereas the percentage of calories obtained from carbohydrates was lower in this group. Previous studies have suggested that fat intake at night is related to higher BMI, body fat percentage, and waist circumference [40], whereas other studies blame a higher carbohydrate intake for this relationship [10].
It is not clear which mechanisms mediate the relationship between night eating and weight. Night time snacking has been found to change metabolism in an acute manner, as it increases the risk of obesity by elevating total LDL cholesterol and reducing whole body fat oxidation without affecting daily energy expenditure [41]. It has been argued that reduced sleep time and sleep disorders may play roles in night time food intake by making people susceptible to greater caloric intake [42]. Lack of sleep among Korean adolescents could play a role in night eating tendency. Around three quarters of Korean adolescents from a nationally representative sample reported that they did not get enough sleep [43], and lack of sleep has been strongly associated with a greater risk of being overweight and obese in this age group [44]. Nevertheless, this relationship seemed to be mediated by disordered eating rather than sleep disorders, as sleep deficits were not related to weight gain or obesity but instead to night eating [45]. Further, calorie intake after 8:00 pm has been associated with an increased risk of obesity, independently of sleep timing and duration [12]. Some studies have indicated that the disturbance of circadian rhythms might produce metabolic alterations that, when combined with behavioural changes (such as eating at night as a consequence of exposure to artificial lighting for example), could promote obesity [44,46].
In the present study, the relationship between night eating and BMI z-score remained significant only for females after stratification for sex. A study in middle-aged subjects found that only women who were already obese showed higher weight gain 6 years after initial assessment of night eating [47]. Female adolescents have shown a tendency to develop a delayed chronotype earlier than young males [48]. This difference may be attributable to distinct endocrine factors between sexes.
In this study, night eating did not appear to increase the risk for being overweight or obese, despite its association with BMI z-score in adolescents. This indicates that the association with BMI z-scores was within normal weight levels. This disparity could be explained by the age of the sample examined in this study. Age seems to moderate the relationship between night eating and BMI. In other words, weight gain may only occur after longer periods of engaging in the behaviour of night eating, thus causing a small or no relationship in younger samples [49]. Identifying whether adolescents' dietary behaviours shape their future eating habits in adulthood or influence metabolism permanently could help explain how the effect of night eating is different across age groups.
The findings presented in this study can be used as a foundation for future research on the topic of night eating. This research area seems to be constantly growing worldwide as well as in recent years in South Korea, as indicated by the publication of studies that explored night eating and snacking, especially those focused on university students [11,16,17,19,20]. Our results seem to indicate the importance of incorporating a temporal dimension to diet planning and weight control programs, especially those targeted at adolescent girls. The inclusion of parents also seems to be important for children's lifestyle changes.
This study has some limitations. As data were obtained from the KNHANES, a cross-sectional study, the associations do not necessarily imply the existence of a causal relationship. This study might be confounded by a lack of data on important variables, such as psychological factors related to night eating or comorbidity with other eating disorders. Further, the fact that dietary data were derived from a one day 24-hour dietary recall limits the ability to measure usual intake and determine if night eating is a habitual behaviour. On the other hand, one of the strengths of the present study is that, to the best knowledge of the authors, this is the first study to evaluate the relationship between night eating and weight in Korean adolescents and one of the few at an international level.
In conclusion, around 21% of Korean adolescents consumed more than one quarter of their energy intake during night hours. Night eating in Korean adolescents was accompanied by delayed eating behaviour, increased breakfast skipping, and lower diet quality, as evidenced by higher energy intake from snacks, higher energy intake from fat, and lower dietary diversity. Parental night eating and being male appeared to be factors that significantly increased odds of night eating. Although male adolescents had a higher odds of night eating, only female adolescents showed a significant positive relationship between night eating and BMI z-scores. Nevertheless, night eating did not appear to increase the risk of being overweight or obese among adolescents.
Footnotes
This work was supported by the Korean Government Scholarship Program (KGSP) Research Scholarship.
References
- 1.Laurson KR, Lee JA, Eisenmann JC. The cumulative impact of physical activity, sleep duration, and television time on adolescent obesity: 2011 Youth Risk Behavior Survey. J Phys Act Health. 2015;12:355–360. doi: 10.1123/jpah.2013-0402. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 3.Statistics Korea. The obesity rates of children and adolescents [Internet] Daejeon: Statistics Korea; 2015. [cited 2015 April 15]. Available from: http://www.index.go.kr. [Google Scholar]
- 4.Kim HS, Park J, Ma Y, Ham OK. Factors influencing health-related quality of life of overweight and obese children in South Korea. J Sch Nurs. 2013;29:361–369. doi: 10.1177/1059840513475363. [DOI] [PubMed] [Google Scholar]
- 5.Song Y, Park MJ, Paik HY, Joung H. Secular trends in dietary patterns and obesity-related risk factors in Korean adolescents aged 10-19 years. Int J Obes (Lond) 2010;34:48–56. doi: 10.1038/ijo.2009.203. [DOI] [PubMed] [Google Scholar]
- 6.Almoosawi S, Prynne CJ, Hardy R, Stephen AM. Time-of-day and nutrient composition of eating occasions: prospective association with the metabolic syndrome in the 1946 British birth cohort. Int J Obes (Lond) 2013;37:725–731. doi: 10.1038/ijo.2012.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang CJ, Hu HT, Fan YC, Liao YM, Tsai PS. Associations of breakfast skipping with obesity and health-related quality of life: evidence from a national survey in Taiwan. Int J Obes (Lond) 2010;34:720–725. doi: 10.1038/ijo.2009.285. [DOI] [PubMed] [Google Scholar]
- 8.Deshmukh-Taskar P, Nicklas TA, Radcliffe JD, O'Neil CE, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999-2006. Public Health Nutr. 2013;16:2073–2082. doi: 10.1017/S1368980012004296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR. Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health. 2006;39:842–849. doi: 10.1016/j.jadohealth.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Gallant A, Lundgren J, Drapeau V. Nutritional aspects of late eating and night eating. Curr Obes Rep. 2014;3:101–107. doi: 10.1007/s13679-013-0081-8. [DOI] [PubMed] [Google Scholar]
- 11.Cho YJ, Kim MH, Kim MH, Choi MK. Night eating habits of middle school students in Gyeonggi. J Korean Soc Food Sci Nutr. 2014;43:300–308. [Google Scholar]
- 12.Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring) 2011;19:1374–1381. doi: 10.1038/oby.2011.100. [DOI] [PubMed] [Google Scholar]
- 13.Huang Y. Night eating in Hong Kong adolescents: prevalence and associations with dinner habits, bedtime and weight status [master's thesis] Hong Kong: The University of Hong Kong; 2014. [Google Scholar]
- 14.Lamerz A, Kuepper-Nybelen J, Bruning N, Wehle C, Trost-Brinkhues G, Brenner H, Hebebrand J, Herpertz-Dahlmann B. Prevalence of obesity, binge eating, and night eating in a cross-sectional field survey of 6-year-old children and their parents in a German urban population. J Child Psychol Psychiatry. 2005;46:385–393. doi: 10.1111/j.1469-7610.2004.00363.x. [DOI] [PubMed] [Google Scholar]
- 15.Striegel-Moore RH, Franko DL, Thompson D, Affenito S, Kraemer HC. Night eating: prevalence and demographic correlates. Obesity (Silver Spring) 2006;14:139–147. doi: 10.1038/oby.2006.17. [DOI] [PubMed] [Google Scholar]
- 16.Suh Y, Lee EK, Chung YJ. Comparison of nutritional status by energy level of night snack in Korean adults: using the data from 2005 Korean National Health and Nutrition Examination Survey. Korean J Nutr. 2012;45:479–488. [Google Scholar]
- 17.Jung HJ, Park KH, Cho YG, Cho JJ, Paek YJ, Song HJ, Byun JS. Night eating tendency and related health risk factors. Korean J Obes. 2006;15:98–105. [Google Scholar]
- 18.Hong SH, Yeon JY, Bae YJ. Relationship among night eating and nutrient intakes status in university students. J East Asian Soc Diet Life. 2013;23:297–310. [Google Scholar]
- 19.Joung HS, Koo NS. The dietary and Late-night eating behavior according to residence type of university students in Daejeon. Korean J Hum Ecol. 2014;23:721–732. [Google Scholar]
- 20.Jun YS, Choi MK, Bae YJ. Night eating and nutrient intake status according to residence type in university students. J Korean Soc Food Sci Nutr. 2015;44:216–225. [Google Scholar]
- 21.Striegel-Moore RH, Franko DL, May A, Ach E, Thompson D, Hook JM. Should night eating syndrome be included in the DSM? Int J Eat Disord. 2006;39:544–549. doi: 10.1002/eat.20302. [DOI] [PubMed] [Google Scholar]
- 22.Energy and Protein Requirements. Report of a joint FAO/WHO/UNU expert consultation. World Health Organ Tech Rep Ser. 1985;724:1–206. [PubMed] [Google Scholar]
- 23.The Korean Nutrition Society. Dietary Reference Intakes for Koreans. Seoul: The Korean Nutrition Society; 2010. [Google Scholar]
- 24.Madden JP, Goodman SJ, Guthrie HA. Validity of the 24-hr. recall. Analysis of data obtained from elderly subjects. J Am Diet Assoc. 1976;68:143–147. [PubMed] [Google Scholar]
- 25.Kant AK, Block G, Schatzkin A, Ziegler RG, Nestle M. Dietary diversity in the US population, NHANES II, 1976-1980. J Am Diet Assoc. 1991;91:1526–1531. [PubMed] [Google Scholar]
- 26.Kant AK, Schatzkin A, Ziegler RG. Dietary diversity and subsequent cause-specific mortality in the NHANES I epidemiologic follow-up study. J Am Coll Nutr. 1995;14:233–238. doi: 10.1080/07315724.1995.10718501. [DOI] [PubMed] [Google Scholar]
- 27.Preedy VR. Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease. New York (NY): Springer-Verlag; 2012. [Google Scholar]
- 28.Korea Centers for Disease Control and Prevention; Korean Pediatrics Society. 2007 Korea Growth Charts. Cheongwon: Korea Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 29.Colles SL, Dixon JB, O'Brien PE. Night eating syndrome and nocturnal snacking: association with obesity, binge eating and psychological distress. Int J Obes (Lond) 2007;31:1722–1730. doi: 10.1038/sj.ijo.0803664. [DOI] [PubMed] [Google Scholar]
- 30.Ochiai H, Shirasawa T, Ohtsu T, Nishimura R, Morimoto A, Hoshino H, Tajima N. Eating behaviors and overweight among adolescents: a population-based survey in Japan. J Obes. 2013;2013:717942. doi: 10.1155/2013/717942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klesges RC, Stein RJ, Eck LH, Isbell TR, Klesges LM. Parental influence on food selection in young children and its relationships to childhood obesity. Am J Clin Nutr. 1991;53:859–864. doi: 10.1093/ajcn/53.4.859. [DOI] [PubMed] [Google Scholar]
- 32.Allison KC, Lundgren JD, O'Reardon JP, Geliebter A, Gluck ME, Vinai P, Mitchell JE, Schenck CH, Howell MJ, Crow SJ, Engel S, Latzer Y, Tzischinsky O, Mahowald MW, Stunkard AJ. Proposed diagnostic criteria for night eating syndrome. Int J Eat Disord. 2010;43:241–247. doi: 10.1002/eat.20693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Zwaan M, Roerig DB, Crosby RD, Karaz S, Mitchell JE. Nighttime eating: a descriptive study. Int J Eat Disord. 2006;39:224–232. doi: 10.1002/eat.20246. [DOI] [PubMed] [Google Scholar]
- 34.Almoosawi S, Winter J, Prynne CJ, Hardy R, Stephen AM. Daily profiles of energy and nutrient intakes: are eating profiles changing over time? Eur J Clin Nutr. 2012;66:678–686. doi: 10.1038/ejcn.2011.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.LeGates TA, Fernandez DC, Hattar S. Light as a central modulator of circadian rhythms, sleep and affect. Nat Rev Neurosci. 2014;15:443–454. doi: 10.1038/nrn3743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wyse CA, Biello SM, Gill JM. The bright-nights and dim-days of the urban photoperiod: implications for circadian rhythmicity, metabolism and obesity. Ann Med. 2014;46:253–263. doi: 10.3109/07853890.2014.913422. [DOI] [PubMed] [Google Scholar]
- 37.Gallant AR, Mathieu ME, Lundgren JD, Allison K, Tremblay A, O'Loughlin J, Drapeau V. Daily physical activity patterns of children with delayed eating behaviors. J Biol Rhythms. 2013;28:332–338. doi: 10.1177/0748730413499857. [DOI] [PubMed] [Google Scholar]
- 38.Striegel-Moore RH, Rosselli F, Wilson GT, Perrin N, Harvey K, DeBar L. Nocturnal eating: association with binge eating, obesity, and psychological distress. Int J Eat Disord. 2010;43:520–526. doi: 10.1002/eat.20735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Allison KC, Goel N, Ahima RS. Delayed timing of eating: impact on weight and metabolism. Curr Obes Rep. 2014;3:91–100. doi: 10.1007/s13679-013-0084-5. [DOI] [PubMed] [Google Scholar]
- 40.Dattilo M, Crispim CA, Zimberg IZ, Tufik S, de Mello MT. Meal distribution across the day and its relationship with body composition. Biol Rhythm Res. 2010;42:119–129. [Google Scholar]
- 41.Hibi M, Masumoto A, Naito Y, Kiuchi K, Yoshimoto Y, Matsumoto M, Katashima M, Oka J, Ikemoto S. Nighttime snacking reduces whole body fat oxidation and increases LDL cholesterol in healthy young women. Am J Physiol Regul Integr Comp Physiol. 2013;304:R94–R101. doi: 10.1152/ajpregu.00115.2012. [DOI] [PubMed] [Google Scholar]
- 42.Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36:981–990. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korea Centers for Disease Control and Prevention. 2007 Statistics on Adolescent Health-related Behavior in South Korea. Cheongwon: Korea Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 44.Park S. Association between short sleep duration and obesity among South korean adolescents. West J Nurs Res. 2011;33:207–223. doi: 10.1177/0193945910371317. [DOI] [PubMed] [Google Scholar]
- 45.Yeh SS, Brown RF. Disordered eating partly mediates the relationship between poor sleep quality and high body mass index. Eat Behav. 2014;15:291–297. doi: 10.1016/j.eatbeh.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 46.Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring) 2009;17:2100–2102. doi: 10.1038/oby.2009.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Andersen GS, Stunkard AJ, Sørensen TI, Petersen L, Heitmann BL. Night eating and weight change in middle-aged men and women. Int J Obes Relat Metab Disord. 2004;28:1338–1343. doi: 10.1038/sj.ijo.0802731. [DOI] [PubMed] [Google Scholar]
- 48.Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, Merrow M. A marker for the end of adolescence. Curr Biol. 2004;14:R1038–R1039. doi: 10.1016/j.cub.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 49.Meule A, Allison KC, Brähler E, de Zwaan M. The association between night eating and body mass depends on age. Eat Behav. 2014;15:683–685. doi: 10.1016/j.eatbeh.2014.10.003. [DOI] [PubMed] [Google Scholar]