Abstract
John Brian Christopherson (1868–1955) was one of the first doctors to be recruited to serve in the Sudan under the British colonial rule. During his work in Sudan (1902–1919) he was key in establishing the civilian medical services in Sudan, including establishing Khartoum Civil Hospital (opened in 1909). The present article focuses on the work of Dr Christopherson in Khartoum Civil Hospital in which he introduced tartar emetic for the first time for the treatment of schistosomiasis. To validate this treatment, Christopherson conducted a series of clinical trials and published his findings in leading medical journals. He had to respond to priority claims over this discovery and to deal with skepticism about the safety of this new treatment. The publications of Christopherson covered not only the therapeutic efficacy of the drug but also discussed the epidemiology of the disease, the possible role of mass chemotherapy and also envisioned chemotherapy in school-age children as a possible strategy for future elimination of the disease.
Keywords: Schistosomiasis, Chemotherapy, Sudan, Christopherson, History of tropical medicine
“He will go down medical history as the man who introduced the cure of bilharziasis (schistosomiasis) by intravenous injections of tartar emetic.”
P. Manson-Bahr about JB Christopherson [1]
“ This is probably the most significant contribution to medicine made by a member of the Sudan Medical Service.”
H.C. Squires on the first introduction of schistosomiasis chemotherapy in Sudan [2]
“It is stated by the highest authority that ‘no direct or other means is known by which the schistosomum can be destroyed’. In other words, there is no known cure for bilharziasis.… Let that pass. Now we think there is a cure, and apparently a sure cure-antimony tartrate.”
J. B. Christopherson, quoting Manson’s Textbook on Tropical Diseases [3]
Introduction
John Brian Christopherson (1868–1955) was one of the first British doctors to be recruited to serve in the the Anglo-Egyptian Sudan. When he arrived in the country in 1902, the Sudan medical services were under the control of the army. In 1904 a civilian Sudan Medical Department was established, with a confusion regarding the appointment of the first director between Christopherson and E.S. Crispin. This ended up in Hunter Bey being appointed as the first director in 1905 to be replaced by Christopherson in January 1907 [4]. Christopherson did not show a flair for administration. He held this position for a brief period in which he found himself in conflicts within the department as well as with the high echelons of power in Sudan [5,6]. Eventually, in 1909 he was replaced by M. B. Mathias who became Director General of the health services, in charge of the civil as well as the military health services. Christopherson was then appointed as director of the Khartoum and Omdurman Civil Hospitals (Figure 1). After a very remarkable career in Sudan (Figures 2 and 3) he retired in 1919 and went back to England. He turned to pulmonary medicine, while practicing tropical medicine at the Bilharzia Clinic of the Ministry of Pensions. In 1936 he retired to a small estate in Gloucestershire with his wife. He died at his home in 1955 at the age of 87 [6]. This article focuses on his ground-breaking work in Khartoum Civil Hospital which introduced to the world the first evidence-based therapeutic regimen for treatment of schistosomiasis.
Figure 1.

Khartoum Civil Hospital, established 1909.
Figure 2.
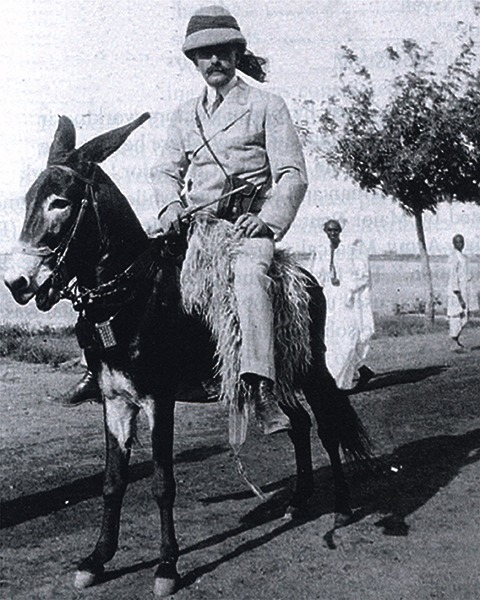
Early years in Sudan: Dr Chistopherson on a donkey, 1906.
Figure 3.
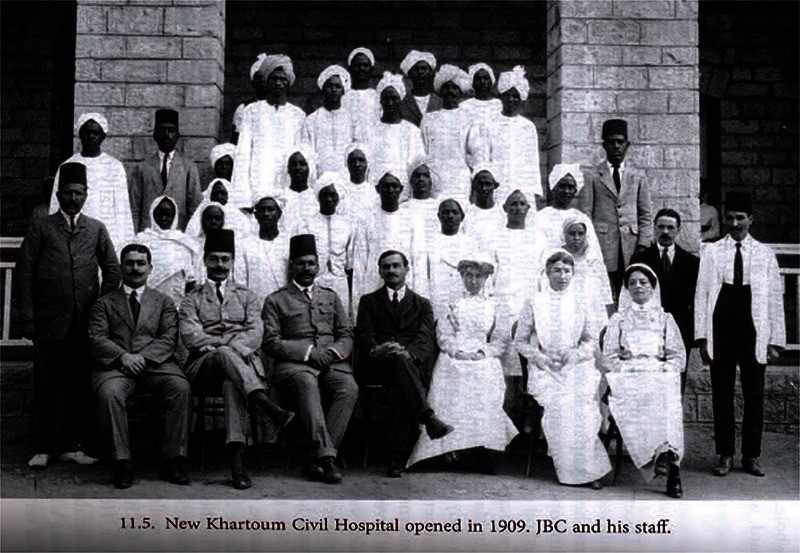
Staff of the Khartoum Civil Hospital. Dr J.B. Christopherson, Director of the hospital sitting in the front row (middle).
Schistosomiasis in the Sudan before the First World War
The only statistics about the prevalence of schistosomiasis before the first world war are those obtained from schoolchildren [2]. Twenty one percent of Halfa boys were suffering from schistosomiasis and 12 % of the boys in the Gordon Memorial College were infected. At Omdurman, Berber and Suakin schools the prevalence was 3% and in Medani 5%. But the highest prevalence was in the Egyptian army and in the Egyptian pupils that constituted a significant proportion of the students in the Gordon Memorial College. The the pundits of tropical medicine at that time asserted that the schistosomes have found a safe abode by residing in the blood vessels and could not be destroyed in this location without harming the patient. The only treatment available to these cases was palliative management in line with latest edition of Mason’s Tropical diseases which sates [7].
“Our knowledge of the situation occupied by the parasite indicates the futility of attempting radical cure by means of poisonous substances whether introduced by the bladder, by the rectum, or by stomach. As yet we know of no direct, or other, means by which the bilharzia can be destroyed”.
This doctrine was challenged when Christopherson published a paper in The Lancet of 7 September 1918 (Figure 4), with the title:
Figure 4.
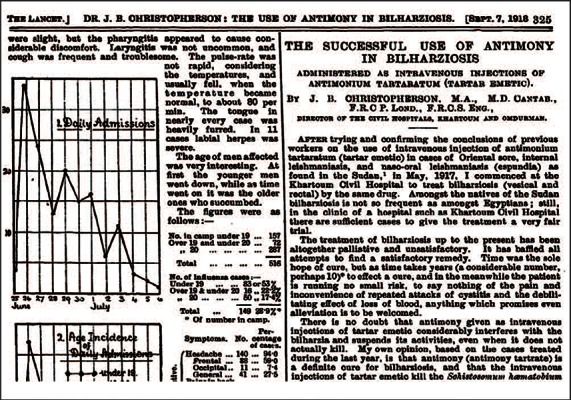
Copy the first paper on treatment of schistosomiasis with tartar emetic.
The Successful Use of Antimony in Bilharziosis: Administered as Intravenous Injections of Antimonium Tartaratum (Tartar Emetic) [8].
In this paper Christopherson presents a series of 13 cases of schistosomiasis treated by intravenous injections of tartar emetic (Figure 5).
Figure 5.

Injection of tartar emetic as reported in the first trial in Khartoum Civil Hospital.
Antimony had been used successfully for kala-azar by Leonard Rogers (1868–1962) and others since 1912 for the treatment of visceral leishmaniasis [9]. Manson-Bahr later wrote that Christopherson’s discovery of antimony as a specific treatment for schistosomiasis came partly by chance. In treating one patient with antimony injections, a man who suffered from both kala-azar and schistosomiasis, Christopherson had noticed not only that the kala-azar was successfully treated but also that the ova of the schistosomiasis parasite were fewer [1]. However, first paper by Christopherson and his subsequent the accounts of the discovery do not indicate that this was an accidental or serendipitous discovery. He states:
“After trying and confirming the conclusions of previous workers on the use of intravenous injection of antimonium tartaratum (tartar emetic) in cases of Oriental sore, internal leishmaniasis, and naso-oral leishmaniasis (espundia) as found in the Sudan in May, 1917, I commenced at the Khartoum Civil Hospital to treat bilharziosis (vesical and rectal) by the same drug…”
“…antimony given in the form of a metallic salt, or as tartar emetic, appears to be a specific cure for leishmaniasis, and there seems to be good reason to believe that it is a specific cure in the case of bilharziosis as well.” [8]
However, it is also clear that he did not conduct a systematic or phased drug discovery research as we understand it today to get to this finding. The medical logic at that time would likely point to antimony as a last resort option for conditions that failed to respond to other less toxic therapies. In an article published in 1916, George Low [9] reviewed the successful use of antimony against African trypanosomiasis and leishmaniasis and then concluded:
“The possibility of the use of antimony intravenously in other diseases, both in the tropics and in temperate regions, should not be lost sight of, in view of the results so far obtained in the diseases in which it has been employed. It might, for example, be given a trial in malaria and in other affections, especially of a protozoal nature.”
Schistosomes are worms, not unicellular protozoan as trypanosomes or Leishmania, but the review by Low does show that intravenous antimony was very much in mind for researchers in tropical medicine at that time. Irrespective of how Christopherson had the first idea of testing tartar emetic against schistosomiasis, it is evident that his work was not limited to testing the therapeutic efficacy of tartar emetic but he went further to set standards for evaluation of a chemotherapeutic agent in a case of schistosomiasis. For example he clearly defines treatment success as parasitological cure (absence of eggs in urine) as opposed to clinical improvement. He also clearly describes a high quality of laboratory tests starting from collection of the sample to microscopic examination (Figure 6):
Figure 6.
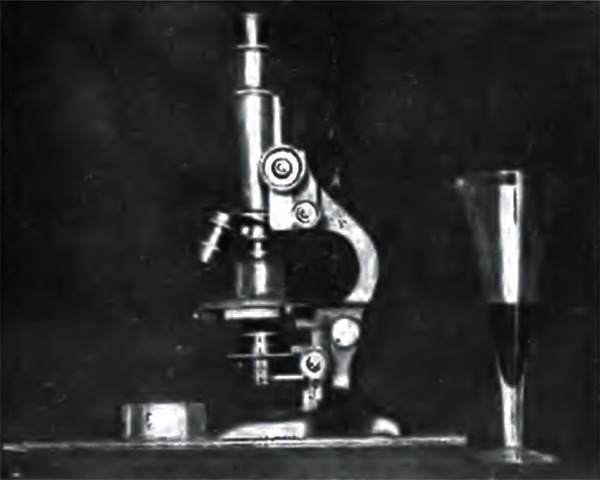
Laboratory equipment used: monocular microscope and sedimentation flask.
“Finally, the microscope is the most valuable guide of all, because ova may continue to be found after other symptoms have cleared up, and after the urine, to ordinary rough tests, has become normal. The urine tested should be passed fresh, that at the end of micturition should be taken, and it should stand for a short time to allow solid particles to settle, or it may be centrifugalised.” [8]
In addition to the 13 cases that he had treated he also quoted Dr. V. S. Hodson, who continued the treatment of bilharzia cases with tartar emetic at Khartoum Civil
Hospital during his absence in 1917, and afterwards independently at Atbara.
In the end he acknowledge the help of his staff:
In conclusion, I would thank Dr. Mustafa Izzedin, who has done so much of the work of injecting these cases, and Mr. J. R. Newlove, who has carried out many of the microscopic examinations connected with the urine. [8]
Following this series of cases of hospitalized patients (Figures 7 and 8), Christoherson published a case report in the British Medical Journal describing a case of schistosomiasis successfully treated by Dr Nicola Malouf with tartar emetic as an outpatient in a private clinic [10]. He introduced the case by saying that it demonsterates safety of administering tartar emetic to abulatory patients.
Figure 7.
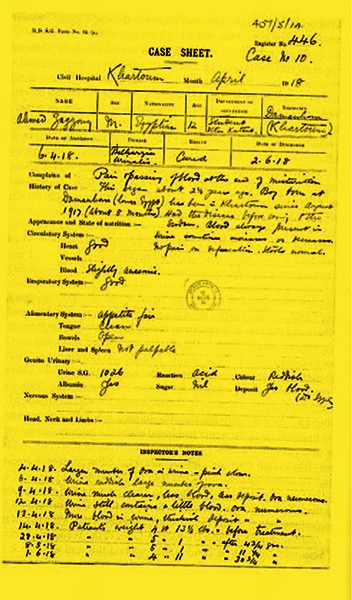
Case record, page 1 (Source Sudan archives at Durham).
Figure 8.
Case record, page 2 (Source Sudan archives at Durham).
Dispute over priority of the discovery
One week after Christopherson’s paper was published The Lancet published the following letter from Dr. J.E.R. McDonagh, a London venereologist claiming priority in using antimony against schistosomiasis. He wrote [11]:
“SIR,-I can fully confirm Dr. J. B. Christopherson’s
results given in his paper in your issue of Sept. 7th. I
began to use antimony in bilharziosis in 1912 (“ Biology and Treatment of Venereal Diseases,” p. 349), and have treated
23 cases with a disappearance of ova in the urine…..”
Christopherson responded to McDonagh in The Lancet on 11 January 1919 [12]:
“Nothing is new in medicine and I dare say that tartar emetic (antimony tartrate) has been used many times for bilharzia, especially in days gone by before tartar emetic fell into disrepute. I have not seen Mr. McDonagh’s book. …My work was original, and has been independent of anyone else’s work and quite spontaneous, and I had never read of, or heard of, or dreamt of any other worker having before tried antimony for bilharzia.”
In fact all that McDonagh wrote in his 1912 book was one sentence at the end of the section on treatment of syphilis with antimony, saying:
“Although not a venereal disease, I should like to mention here that I have had great success in treating cases of bilharzia with intravenous injections of antimony.” [13].
In response to the case report in the British Medical Journal, Major DC Wiley wrote a memorandum about his experience in treating an Egyptian patient in 1916 in the Australian Dermatological Hospital with intravenous tartar emetic [14]. At that time schistosomiasis was ravaging in Egypt with an estimated prevalence of not less than 80 per cent in the agricultural population [15]. It is rather surprising that Wiley did not pursue this finding further. He probably thought that the drug was too toxic:
“Our knowledge of the situation occupied by the parasites in patients suffering from bilharziosis has hitherto acted somewhat as a deterrant in attempting a radical cure of the disease by the introduction of poisonous substances into the general circulation. In consequence treatment has been largely confined to measures tending to mitigate the severity of the symptoms. It is interesting therefore to see in the JOURNAL of December 14 an article by Dr J B Christopherson on the efficacy of intravenous injections of tartar emetic in this disease..” [14].
The experience of the Australian Medical Service (AAMS) was later narrated by Major Athur. Innes:
“…. Major Strong of the Australian Medical Service tells me that he and one or two brother officers had worked with it in 1916, in fairly small doses and at intervals of not less than a week between the injections, but no one felt convinced of the possibility of curing the disease, nor had anyone the courage to adopt the truly heroic dosage which is necessary to affect the bilharzia worm and its ovum.” [16]
Unlike McDonagh, Wiley did not claim priority for discovering a cure for schistosomiasis. Instead, he concluded his memorandum by giving credit to Christopherson for providing evidence. He stated:
“It is unjustifiable to draw conclusions from a single case….... in light of the evidence being brought forward, the facts tend to support the view of the favourable action of tartar emetic in bilharziosis.” [14]
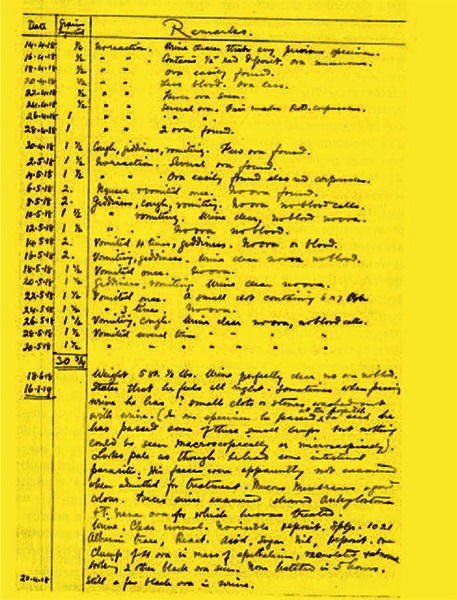
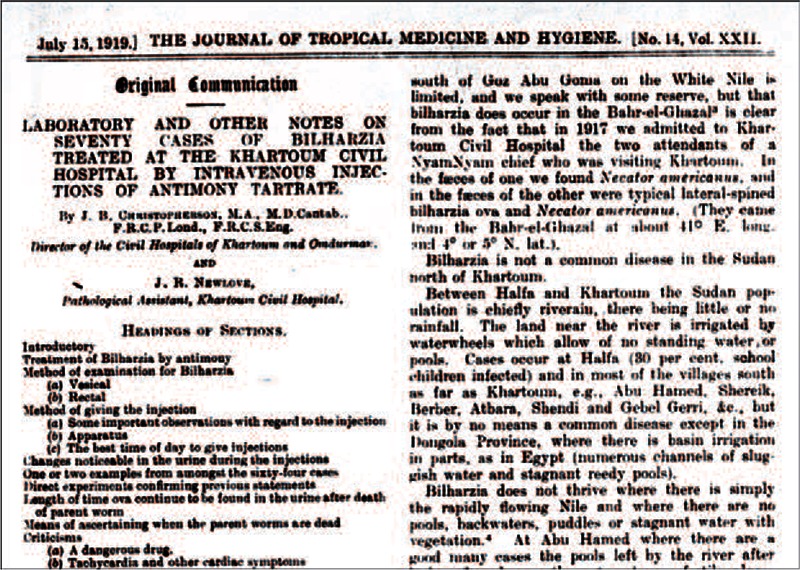
Threat of a setback in the Egyptian Army Military Hospital in Khartoum
At the time Christopherson started his tials in Khartoum Civil Hospital, the Egyptian Army Military Hospital in Khartoum (Figure 9) was providing medical care for the Egyptian soldiers who were mainly recruited Egyptian peasants with haigh prevalence of schistosomiasis. It was logical that the Army physicians in this hospital were highly interested in the work of Christopherson on schistosomiasis. In 27 th June 1918 they started to treat cases of schistosomiasis with tartar emetic injections [17]. After enrollment of twenty six patients in the treatment trial, one patient who completed treatment with tartar emetic died. The patient was an Egyptian soldier who presented with hematuria and urine examination showed Schistosoma haematobium eggs. He was started with the standard gradually increased dose of tartar emetic beginning with 1/2 grain to 2 grains, which was then given every second day. After reaching a total dose of 33 g his urine examination was free of schitosome eggs. The 1918 Inflenza Pandemic made its first appearance in the Sudan in the Egyptian Army Military Hospital (EAMH). Patients in the bilharzia ward started to come down with very high temperatures. Three days after first detection of the epidemic in the ward the patient developed high fever for four days and then deteriorated rapidly and died. An autopsy was performed on the patient about 12 hours after his death. The autopy findings were published in the Journal of Tropical Medicine and Hygiene [17]. The authors are Robert Archibald, Pathologist at the Wellcome Laboratories in Khartoum and Major Arthur Innes who was the patient’s attending physician. The paper describes the pathological changes in the different organs and in the end made a surprisingly definitive conclusion that the death was due to antimony toxicity and not due other causes:
“In the case recorded in this paper there can be little doubt that the pathological changes in the organs were attributed to the action of tartar emetic, and were not sequels of bilharzia, influenza or a previous malarial infection. The treatment carried out appeared intensive and ended in a sudden and unexpected fatal result.” [17]
Figure 9.
The Military Hospital, Egyptian Army, Khartoum.
Fearing the toxic effect of antimony in other cases, the treatment was discontinued. Of the series of 26 cases treated in the period from June 27th, 1918 to August 10th, 1918, 14 were discharged with the urine free of blood and ova, 11 were still infected but were discharged on account of the influenza epidemic, after receiving doses of tartar emetic varying from 3 grains to 23 grains [16].
The conclusions in the autopy paper were clearly not balanced. The patient had influenza and very high temperature for 4 days before his death but it seems that the autopy report was influenced by concerns over the use tartar emetic in unprecedented dose schedules.
Christopherson was concerned that the paper by Archibald and Innes [17] could discredit his work to establish tartar emetic as a treatment for schistosomiasis. He believed that the cause of death of this case was clearly influenza, probably with some aggravated conditions like previous malaria snd parasitic infections. He wrote a paper in the same journal criticizing the post-mortum paper staring from its suggestive title [18]. Christopherson went through the post-mortum report point after point and explained why he thought antimony toxicity was not the cause of death in this particular patient. In this paper Christopherson shows the depth of his clinical analytic skills and his wide scope of knowledge of medical sciences at that time. He admitted that tartar emetic could be highly toxic and has to be used with caution but he asseted that there was no evidence that it was the cause of death of that particular patient. In conclusing he quoted an epitaph in Latin:
“‘post hoc’ is not necessarily ‘propter hoc’ and I am unable to follow the facts of this particular case as furnishing adequate grounds for the warning administered by the authors” [18].
It seems that Christopherson was able to convince the physcians in EAMH that the death of this patient was due to influenza and not to tartar emetic as suggested by the autopy paper. Treatment with antimony was resumed in the EAMH before publication of his response, but publication of his reponse was necessary to address the readers of the journal. In addition, as the influenza epidemic continued the phsicians in the military hospital saw other patients not under antimaony treatment develop high fever and die in a similar fashion. Major Innes, who co-authored the autopy paper later wrote:
“we not unnaturally associated the high temperatures which laid low patient after patient with our vigorous pushing of the tartar emetic; having seen patients not infested with bilharzia become ill and some die, we again attempted the antimony tartrate.” [16]
A second series of 36 cases was started and an account of all the cases treated in the Military Hospital were published in a paper by Innes in the British Medical Journal [16]. Now Innes is singing praise for tatar emetic and the new regimen treatment recommended by Christopherson for schistosomiasis. He starts his presentation by stating:
“TARTAR EMETIC, as advised by J. B. Christopherson,’ must be accepted as a positive cure of bilharzial infection. I knew many of the cases on which his recommendation was based, and had commenced the treatment in the Egyptian Military Hospital, Khartoum, where the opportunities of proving or disproving its efficiency are many among the fellaheen recruits of the Egyptian army.”
He ends by asserting his “faith” in tartar emetic as a treatment for builharzia.
“…. we feel that the faith that is in us relative to the value of tartar emetic in billiarzial infections is justified by the results we have given, for these results are not based on naked-eye bservations or beliefs, but on the non-partisan findings of the microscope.” [16]
More series of cases from Khartoum Civil Hospital
In 14 June, 1919 Christopherson published another article in The Lancet, citing additional 30 cases successfully treated in Khatoum Civil Hospital. He described in more detail the experience of Khartoum Civil Hospital in the management of these cases. [3]
“The cases which have formed the basis of this paper have been under the care of Dr. Ferid Masoud, medical officer at the Khartoum Civil Hospital, who has done for me many of the injections and in other ways assisted me, and I have especially to thank Mr. J. R. Newlove, pathological assistant at the hospital, who made the daily microscopical and other examinations of the urines with so much skill and enthusiasm, and who devoted so much of his time to the work” [3].
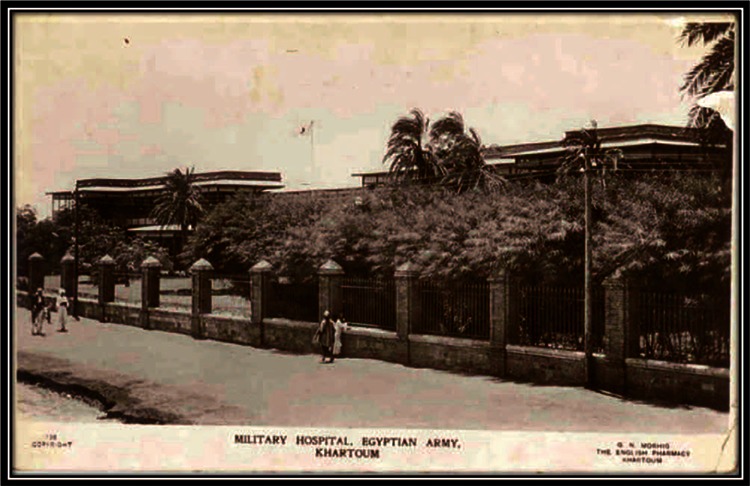
Not only a therapeutic artisan
The largest series of cases were included in a paper co-authored by his assistant Newlove, published in 15 July, 1919 in the Journal of Tropical Medicine and Hygiene with the title: Laboratory and Other Notes on Seventy Cases of Bilharzia Treated at the Khartoum Civil Hospital by Intravenous Injections of Antimony Tartrate [19]. This paper (Figure 10) reports the successful treatment of a larger series of seventy cases, including forty cases treated as out-patients. In this paper Christopherson demonsterates that he was more than a’therapeutic artisan ‘. His thoughts extended beyond the patient to the community and to how to prevent and eliminate the disease.
Figure 10.
The second and main paper on treatment of schistosomiasis with tartar emetic in Khartoum.
The paper starts with an introduction that reviews the epidemiology of schistosomiasis which was endemic in all provinces of the Sudan except the Red Sea Province. This is the best reference to date on the distribuition of schistosomiasis in the Sudan at that time. They describe the different types of foci of schistosomiasis transmission in the country including “ the newly acquired Province of Darfur”. The epidemiological data was based on patient records and reports of health workers and results of surveys on school children when these were available. For example they mention that 30% of school children in Halfa are infected. They also describe the different types of snail habitats in the endemic foci in gravitation irrigation schemes with stagnant waters and vegetation in the northern provinces and rain water pools (foulas) and seasonal streams (khours) in the western Sudan. Population movements from Egypt to Sudan are considered as the main factor for the spread of schistosomiasis.
All cases have been followed up to completion of the treatment but some were available for extended follow-up to two years. They give the methods used in for diagnosis and treatment in great detail to the extent of giving the brand and magnification lenses of the microscope used. The parasitological tests described esured great sensitivity with sedimentation of urine and followed by hatching test. Negative stools results were followed by concentration test to detect light infections. For drug administration they describe apparatus for preparing the antimony tartrate solution and the syringes. A decription of the gradual increase of dosage is highlighted in detail. A detailed description of the side-effects and signs of toxicity is given.
One of the remarkable sides of this paper is that it gives some highly insightful opinions about the epidemiology of schistosomiasis and proposes operational details for elimination of the disease in Sudan and Egypt. Looking back to how the schistosomiasis control starategies have evolved over the time, one cannot help but admire Christopherson for having put forwards these ideas. He was more than a mere “therapeutic artisan”, his concern was not limted to treating the patient but he ventured beyond that to show concern for the cummnity and the economic impact of the disease. In this respect the most notable points are:
(1) Screening school children to determine the prevalence of the disease in the community, this approach is still being recommended.
“The surest method for ascertaining the presence or absence and the incidence of bilharzia in any locality is the systematic examination of urine of all boys at the Government schools, which exist all over the Sudan. Children are most liable to infection.”
(2) He puts forwards a rationale for mass chemotherapy as a strategy for elimination of schistosomiasis which he gives under the heading “ the prophylactic action of antimony treatment”:
“We think the greatet value of this tratement is in its prophylactic action, for it is clear that if the treatment is adopted on a large scale and ova which is evacuated are sterile, there is an excellent chance are of stamping out this disease in the Sudan and Egypt by cutting off the source of infection and so breaking the chain in the cycle of development at a very important point.”
(3) He identifies school children as a target for chemotherapy since they are the main reservoir of infection in the community:
“We know that it is chiefly the the school children who are infected, and who are therefore, chiefly responsible for propagation of the disease…”
(4) He proposes annual mass treatment and this is what is recommended today to treat re-infections.
“If the schools in the affected out-stations were taken each once a year –each boy’s urine and faeces examined-a bilharzia index kept, and the boys suffering from the disease given a course of treatment, it seems to us that each year would mark a great step forwards towards the eradication of the disease from the Sudan.”
(5) He warns about the economic impact of the disease and makes suggestion for limiting the spread of the disease.
One need hardly point out the danger and disadvantages –economically and physically –of having a disease like bilharzia so wide spread, and spreading, in the Sudan.
It is undoubtedly becoming more widely spread and more common, and, as cultivation and population increase, it will go on increasing. Nothing at all is done at the present time by the Sudan Government to keep it and other parasitic diseases in hand. Treatment is left to the discretion of individual doctors practicing. The medical department can do nothing ; it has not the means.
Notes and statitics should be carefully kept and filed. Much valuable information would thereby accrue. The doctor should go from place to place and have at his disposal a mobile laboratory.
But such measures as those outlined above will be useless if steps were not also taken to prevent bilharzia infection pouring in from Egypt as it does now, yearly, monthly, daily and for the this end the Egyptian Army medical authorities will doubtless like to cooperate. Every Egyptian soldier before coming to the Sudan should be examined for biharzia, and if found should have a course of treatment and should be cured.
Much could be done through the schools, and, in point of fact, in the Sudan, where the school authorities, much to their credit have so much influence, we are inclined to think that, working through the schools, in a few years it should be possible to eradicate bilharzia and other parasitic diseases, both by direct measures and by educational means.”
Scepticism is followed by world wide recognition
By the time of retirement of Christoperson the treatment of schistosomiasis had been independently tested and validated by leading experts in tropical medicine. Idividual cases and series of cases were treated in London [20–23] and South Africa [24]. The availability of a large number of cases of schistosomiasis in Egypt allowed the pysicians there to test modifications of the dosage, giving lower doses in children and women and increasing the intervals between the doses and the success with these dose variations was reported [25].
“Since June, 1919, injections of antimony tartrate in accordance with Dr. Christopherson’s observations have been the routine treatment for bilharziasis at the Church Missionary Society’s Hospital, Old Cairo, and we are now injecting from fifty to seventy cases a day; both, urinary and rectal bilharziasis are being treated, but the former in a much larger proportion… Our patients, most of them farm labourers, are unwilling to prolong their stay in hospital unduly. On –the other hand, it appears that a much smaller and more gradual administration of antimony is equally effective. Quite small doses spread over a considerably longer period appear to cure the disease, the main point being the cumulative effect of about 20 grains of the drug.”
Christopherson wrote an editorial article for the British Medical Journal on the treatmet of these cases in Egypt [26]:
“The cases were all voluntary, and, since the completion of this series of 1,000 cases in August, 1920, another 1,000 have been done in five months. The C.M.S. Hospital, Old Cairo, is by no means the only hospital in Cairo where large numbers of bilharzia cases are coming for treatment; the Kasr-el-Aini Hospital, if my information is correct, has treated about 1,600 cases of bilharzia by the intravenous method during twelve montlhs, and other hospitals and practitioners in Cairo are similarly treating numbers of patients, though naturally on a smaller scale; also the Government hospitals in the provinces, some of which have a still larger number of cases to their credit even than the Kasr-el-Aini, and other hospitals, are carrying out the treatment. The great number treated is striking, but bilharziasis is so deeply rooted and prevalent in Egypt that, in my judgement hospital treatmnent alone, even on this large scale, will take a long time to make an impression on it as a national disease; the sources of reinfection, too, are many. It should be remembered, however, that each case, when cured by antimony tartrate, ceases to convey infection, owing to the fact that the ova deposited in the bladder and rectum are also killed by the remedy, in other words, the patient ceases to be a “carrier.”
Christopherson became the world expert in treatment of schistosomiasis. He was selected to write about treatment of schistosomiasis in The Lancet under the section of “Modern Technique in Treatment, Series of Special Articles, contributed by invitation, on the Treatment of Medical and Surgical Conditions” [27].
Mc Donagh continued to write claims for priority in discovering a cure for bilharzia without giving more details about the cases [28,29] and Christopherson did not miss a chance to respond to these claims [30,31]. The world has accepted the treatment of schistosomiasis with tartar emetic.
The treatment of bilharzia with antimony was published in Medical Notes of the British Parliament [32].
“The Treatnent of bilharziasis.-Mr. Doyle asked, on May 12th, whether the Miinister for Pensions was aware that Dr. Christopherson’s antimony treatment was now accepted as a certain cure for bilharziasis; that the Australian Government, after segregating all returned officers infected in Egypt, had completely stamped it out by this method of treatment; that there are still a number of men in this country who were infected during the Soutlh African war, and were still sufferers, but who were debarred from treatment by the Ministry because they had not served (in many cases because of this disease) in the recent war; and if there were any reason why an exception should not be made in favour of these men so that they might receive treatment? Mr. Macpherson sympathized with the suggestion, and said he was communicating with the War Secretary about it.”
The place of mass chemotherapy in schistosomiasis control
The legacy of Christopherson is not limited to his introduction of tartar emetic as a chemotherapeutic agent against schistosomiasis but also his pioneering ideas about the epidemiology of the disease and the possible role of mass chemotherapy and other measures in elimination of the disease. In 1919 and following publication of the the work of Chrestopherson, the first mass treatment intervention using intravenous tartar emetic was implemented in Egypt [15] and in Japan the cases of schistosomiasis detected in epidemiological surveys were treated with sodium tartar emetic (Stibnal) after 1921 [33]. Following this a number of national programmes started controlling schistosomiasis using treatment and/or snail control, often combined with provision of health education messages [34]. In Sudan there were limited attempts to implement mass treatment with intravenous antimony as a control strategy for schistosomiasis. Squires [2] described an early programe in Berber area where a series of dispensaries were organized at intervals of fifty miles. Medical assistants carried out diagnosis and treatment of cases of schistosomiasis with tartar emetic with high expertise and success. This program did produce a local impact on the prevalence of the disease with very few mishaps due to the treatment. Yet, as Christopherson had predicted, the great expansion of agricultuaral projects in Sudan was accompanied by devastating spread of schistosomiasis in the country. By 1947 the prevalence of schistosomiasis was more than 50% in many parts in Gezira. The global startegies adopted used two main high –impact approaches: first is morbidity control by chemotherapy as introduced and advocated by Christopherson and the second tool is transmission control by destruction of the snail intermediate host. These tools were supplemented by health education and other measures. Schistosomiasis control strategies have evolved as a function of the availability of new tools. In Sudan, as in other endemic countries, there was a great emphasis on targeting transmission through snail control by chemical, physical and biological methods and little attention was given to developing or deploying antischistosomal drugs. It was soon realized that in many instances snail control was not efficient and not cost-effective and some projects based on snail control have failed. Eventually WHO shifted its emphasis from from snail control back to chemotherapy with the availability of safer medicines such as niridazole, metrifonate, oxamniquine and praziquantel. Moreover, with the advent of single-dose oral administration (e.g. of oxamniquine or praziquantel), the cost effectiveness and feasibility of large-scale preventive chemotherapy have favoured mass chemotherapy as the main tool for schistosomiasis elimination today. In 1985 WHO recommended mass chemotherapy and morbidity control as the main approach in countries like Sudan [35]. Chistopherson would have been gratified to know that his prediction for chemotherapy to be a potent tool for eventual eradication of chistosomiasis have been realized. The WHO strategy for 2012–2020, aimed at the ultimate eradication of the disease, recommend that countries to deploy mass chemotherapy in endemic reas like should Sudan, with emphasis on school-age children [36].
Recognition of Chistopherson and his work.
It is sad that the pioneering work of Christopherson in Khartoum did not get the recognition it deserves. In a touching letter written to Christopherson in 1927, Dr Hassan Zaki, an Egyptian medical assistant worked with him wrote (Figures 11 and 12):
Figure 11.
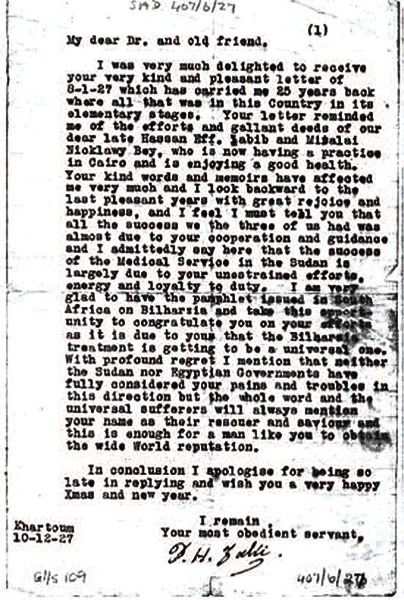
copy of letter from Hassan Zaki.
Figure 12.

Staff of staff the first Khartoum Civil Hospital, 1905. Dr J B Christopherson (seated in front, second from left) Hassan Zeki on JBC’s left.
“My dear Dr. and old friend, I was very much delighted to receive your very kind and pleasant letter of 8-1-27 which has carried me 25 years back where all that was in this country was in its elementary stages. Your kind words and memoirs have affected me very much and I look backward to the last pleasant years with great rejoice and happiness, and I feel I must tell you that all the success we the three had was almost [all] due to your cooperation and guidance and I admittedly say here that the success of the Medical Service in the Sudan is largely due to your unrestrained effort, energy and loyalty to duty… With profound regret I mention that neither the Sudan nor Egyptian Governments have fully considered your pains and troubles in this direction but the whole world and the universal sufferers will always mention your name as their rescuer and saviour and this is enough for a man like you to obtain the wide World reputation……
H. Zaki.”
In 1923, Professor George Wherry of Cambridge University nominated Chrisopherson for the Nobel Prize for Medicine. In 1924, Sir Ronald Ross put Christopherson’s name forward for Fellowship of the Royal Society (FRS) but neither the Nobel Prize nor the FRS materialied [5]. In 2003 Symposium on the chemotherapy of scshistosomiasis was held in the buildings of old Chistophersons’s Khartoum Civil Hospital (now Sudan Medical Specialization Borad ). A memorial paque for Chistopherson was unveiled by H.E. the British Ambassaror in Khartoum. Perhaps the most valuable recognition of the the achievement of Christopherson is a book published by his great niece, Ann Crichton-Harris [6]. She was born in Britain in 1936 but now lives in Canada. Her book (Figure 13) is entitled “ Poison in small measure: Dr. Christopherson and the cure for Bilharzia”. She did an extensive research for eight years that culminated in this book. Also, in preparation for writing this book she took a number of courses at the University of Toronto in History of Medicine and Medical Anthropology. The book is a valuable asset to the literature on the history of tropical medicine in particularly the early history of the modern medical services in Sudan. The most striking feature in this book is the accuracy of the information and the eye for detail that are not compromised by the fact that this is a niece writing about her great uncle.
Figure 13.
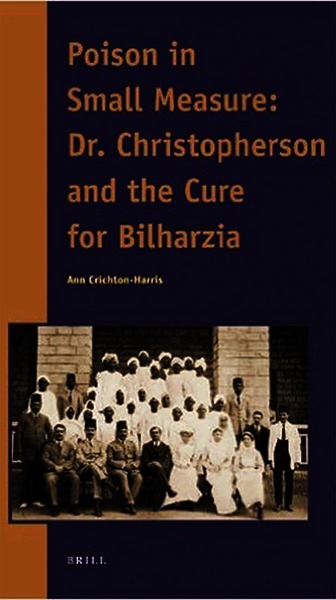
Cover of the book by Ann Crichton-Harris “Poison in Small Measure: Dr Christopherson and the Cure for Bilharzia”.
Acknowledgements
The origin of Figures 2, 3 and 11 is Ms. Ann Crichton-Harris. Some of the illustrations were taken from her articles or her biography of Christopherson. The source of the Figures 6, 7 and 10 is the Sudan Archives, University of Durham.
References
- 1.Manson-Bahr P, John B. Christopherson. Nature 1955; 175:377–378. [DOI] [PubMed] [Google Scholar]
- 2.Squires HC. The Sudan Medical Service. An experiment in social medicine. Ulster Med J 1959; 28:83. [Google Scholar]
- 3.Christopherson JB. Antimony tartrate for bilharziasis: a specific cure. Lancet 1919; 14:1021–23. [Google Scholar]
- 4.Daly MW. Empire on the Nile: The Anglo-Egyptian Sudan, 1898-1934. London: Cambridge University Press, 2003. [Google Scholar]
- 5.Crichton-Harris A. Undercurrents on the Nile: the life of Dr. John B. Christopherson, 1868-1955. J Med Biogr 2006; 14:8–16. [DOI] [PubMed] [Google Scholar]
- 6.Crichton-Harris A. Poison in Small Measure: Dr. Christopherson and the Cure for Bilharzia. p1–428. The Netherlands: Brill NY Leiden, 2009. [Google Scholar]
- 7.Manson P. Tropical diseases: a manual of the diseases of warm climate. Page 615, Baltimore: Williams & Wilkins Co, 1898. Book digitized by Google and uploaded to the Internet Archive by user tpb at: https://archive.org/details/tropicaldisease00unkngoog [Google Scholar]
- 8.Christopherson JB. The successful use of Antimony in Bilharziosis administered as intravenous injections of antimonium tartaratum (tartar emetic). Lancet 1918; 192:325–27. [Google Scholar]
- 9.Low GC. The history of the use of intravenous injections of tartar emetic (Antimonium tartaratum) in tropical medicine. Trans R Soc Trop Med Hyg 1916; 10:37–42. [Google Scholar]
- 10.Christopherson JB. Intravenous injections of Antimonium Tartarum in Bilharziosis. BMJ 1918; 652–653. [DOI] [PMC free article] [PubMed]
- 11.McDonagh JER. Letter to Editor. Lancet 1918; 371.
- 12.Christopherson JB. Letter to the Editor. Lancet, 11 January 1919; 79. [Google Scholar]
- 13.McDonagh JER. Venereal Diseases: Their Clinical Aspect and Treatment. p 214 London: Heineman, 1920. https://archive.org/stream/venerealdiseases00mcdouoft#page/214/mode/2up [Google Scholar]
- 14.Wiley CJ. The treatment of Bilharziosis by intravenous injections of tartar emetic. BMJ 1918; 716–717.
- 15.Day H. The outpatient treatment of bilharziasis, with analysis of 1000 cases. Lancet 1921; 525–529.
- 16.Innes A. Treatment of bilharzial infection by tatar emetic. BMJ 1919; 340–41. [DOI] [PMC free article] [PubMed]
- 17.Archibald RG and Innes A. Clinical and pathological notes on a fatal case of bilharzia treated by tartar emetic. J Trop Med Hyg, 1 April 1919; 53–54.
- 18.Christopherson JB. The cure of bilharzia disease by the intravenous ijections of antimonu tartrate. J Trop Med Hyg, 16 June 1919; 113–114. [DOI] [PMC free article] [PubMed]
- 19.Christopherson JB and Newlove JR. Laboratory and Other Notes on Seventy Cases of Bilharzia Treated at the Khartoum Civil Hospital by Intravenous Injections of Antimony Tartrate. J Trop Med Hyg, 15 July 1919; 139.
- 20.Low GC. A case of bilharzial disease treated by intravenous injections of antimonium tartarum. J Trop Med Hyg, 15 May 1919; 93–94.
- 21.Low GC, Newham HBG. Bilharziasis treated by intravenous injections of antimonium tartarum. J Trop Med Hyg, 1 December 1919, 216–220.
- 22.Low GC, Newham HBG. A series of cases of Bilharziasis treated by intravenous injections of antimonium tartarum. Lancet, 11 October 1919; 633–636.
- 23.Taylor F. Intravenous injections of antimonium tartarum (tartar emetic) in Bilharziasis. Lancet, 9 August 1919; 246–247.
- 24.Cawston FG. A case of biharziasis in Natal treated by tartar emetic. Lancet, November 1919; 873–874.
- 25.Lasbrey FO, Coleman RB. Notes on one thousand cases of bilharzia treated by antimony tartrate. BMJ, 26 February 1921; 299–301. [DOI] [PMC free article] [PubMed]
- 26.Christopherson JB. Bilharzia disease in Egypt. BMJ, 2 April 1921; 491–492. [DOI] [PMC free article] [PubMed]
- 27.Christopherson JB. Modern Technique in Treatment. A Series of Special Articles, contributed by invitation, on the Treatment of Medical and Surgical Conditions. LXXII. The Treatment Of Bilharzia Disease. Lancet; 24:1071–72. [Google Scholar]
- 28.McDonagh JER. The treatment of bilhaziasis with antimony. J Trop Med Hyg 1923; 26:119. [Google Scholar]
- 29.McDonagh JER. Letter to the Editor. Lancet, 31 May 1924; p1130.
- 30.Christopherson JB. The treatment of bilhaziasis with antimony. J Trop Med Hyg 1923; 26:211. [Google Scholar]
- 31.Christopherson JB. Letter to the Editor. Lancet, 7 June 1924; p1184.
- 32.Medical Notes in Parliament. Treatment of bilharziasis. BMJ, 21 May 1921; p753.
- 33.Tanaka H, Tsuji M. From discovery to eradication of schistosomiasis in Japan: 1847-1996. Int J Parasitol 997; 27:1465–1480. [DOI] [PubMed] [Google Scholar]
- 34.Jordan P. From katayama to the Dakhla Oasis: the beginning of epidemiology and control of bilharzia. Acta Trop 2000; 77:9–40. [DOI] [PubMed] [Google Scholar]
- 35.Control of Scistosomiasis. Report of a WHO Expert Committee. World Health Organization. Technical Report Series. 728 World Health Organization, Geneva: 1985. [Google Scholar]
- 36.World Health Organization: Schistosomiasis progress report 2001–2011 and strategic plan 2012–2020 Ref: ISBN 978 92 4 150317 4. Avaialble at: http://www.who.int/schistosomiasis/resources/en/


