ABSTRACT
Host cell-free (axenic) culture of Coxiella burnetii in acidified citrate cysteine medium-2 (ACCM-2) has provided important opportunities for investigating the biology of this naturally obligate intracellular pathogen and enabled the development of tools for genetic manipulation. However, ACCM-2 has complex nutrient sources that preclude a detailed study of nutritional factors required for C. burnetii growth. Metabolic reconstruction of C. burnetii predicts that the bacterium cannot synthesize all amino acids and therefore must sequester some from the host. To examine C. burnetii amino acid auxotrophies, we developed a nutritionally defined medium with known amino acid concentrations, termed ACCM-D. Compared to ACCM-2, ACCM-D supported longer logarithmic growth, a more gradual transition to stationary phase, and approximately 5- to 10-fold greater overall replication. Small-cell-variant morphological forms generated in ACCM-D also showed increased viability relative to that generated in ACCM-2. Lack of growth in amino acid-deficient formulations of ACCM-D revealed C. burnetii auxotrophy for 11 amino acids, including arginine. Heterologous expression of Legionella pneumophila argGH in C. burnetii permitted growth in ACCM-D missing arginine and supplemented with citrulline, thereby providing a nonantibiotic means of selection of C. burnetii genetic transformants. Consistent with bioinformatic predictions, the elimination of glucose did not impair C. burnetii replication. Together, these results highlight the advantages of a nutritionally defined medium in investigations of C. burnetii metabolism and the development of genetic tools.
IMPORTANCE Host cell-free growth and genetic manipulation of Coxiella burnetii have revolutionized research of this intracellular bacterial pathogen. Nonetheless, undefined components of growth medium have made studies of C. burnetii physiology difficult and have precluded the development of selectable markers for genetic transformation based on nutritional deficiencies. Here, we describe a medium, containing only amino acids as the sole source of carbon and energy, which supports robust growth and improved viability of C. burnetii. Growth studies confirmed that C. burnetii cannot replicate in medium lacking arginine. However, genetic transformation of the bacterium with constructs containing the last two genes in the L. pneumophila arginine biosynthesis pathway (argGH) allowed growth on defined medium missing arginine but supplemented with the arginine precursor citrulline. Our results advance the field by facilitating studies of C. burnetii metabolism and allowing non-antibiotic-based selection of C. burnetii genetic transformants, an important achievement considering that selectable makers based on antibiotic resistance are limited.
INTRODUCTION
Coxiella burnetii is a wide-ranging bacterial pathogen that causes the zoonosis Q fever (1, 2). Humans are generally infected by inhalation of contaminated aerosols generated by domestic livestock, with sheep, goats, and dairy cattle being the primary animal reservoirs. Traditionally, C. burnetii has been classified as an obligate intracellular pathogen (3). During natural infection, C. burnetii preferentially infects mononuclear phagocytes and traffics to an acidified compartment that resembles a degradative phagolysosome (4). Genomic sequencing of C. burnetii reveals the conservation of many genes and pathways involved in central carbon, amino acid, and lipid metabolism (5, 6). Metabolic reconstruction based on these findings, along with metabolic stimulation of C. burnetii under acidic conditions, provided critical information for the development of an axenic (host cell-free) medium supporting the growth of C. burnetii under microaerobic conditions (7, 8). A second-generation medium, acidified citrate cysteine medium-2 (ACCM-2), supported increased replication and viability (9, 10). Propagation of C. burnetii in ACCM-2 also accelerated the development of genetic tools and allowed cloning of antibiotic-resistant transformants by colony formation (11–13).
Beyond the development of ACCM-2, little work has been conducted on central metabolic processes governing C. burnetii axenic growth. Indeed, the primary carbon and energy sources essential for bacterial replication, including specific amino acids and sugars, remain largely undefined. Early metabolic labeling experiments indicate that C. burnetii transports and incorporates exogenous glutamate and glucose when incubated in an acidic buffer, although glucose is catabolized at very low levels relative to those of glutamate and tricarboxylic acid cycle intermediates, such as succinate and pyruvate (8, 14–17).
Determination of the repertoire of amino acids and carbohydrates required for C. burnetii growth is critical for understanding metabolic constraints encountered during host cell parasitism. However, the elucidation of nutritional pathways utilized by C. burnetii requires a nutritionally defined growth medium. To this end, we developed a defined ACCM (ACCM-D) with known concentrations of amino acids and other nutrients. C. burnetii cultured in ACCM-D exhibited improved growth in liquid and solid media that corresponds to increased viability. In addition, dropout formulations allowed scoring of amino acid auxotrophies and the contribution of glucose to C. burnetii growth.
ACCM-D dropout, along with confirmed arginine auxotrophy in C. burnetii, also presented an opportunity to develop a nonantibiotic method of genetic selection. The use of antibiotic resistance markers in the genetic transformation of C. burnetii, a category B select agent, is restricted to those that confer resistance to antibiotics without clinical relevance, such as chloramphenicol, kanamycin, and ampicillin (13). Acidic conditions similar to those of ACCM-2 and C. burnetii's lysosome-like intracellular niche inhibit the activity of aminoglycoside antibiotics (18). Moreover, a predicted β-lactamase (CBU0807) may neutralize β-lactam antibiotics during C. burnetii transformant selection. Collectively, these reasons might explain why the selection of C. burnetii transformants with ampicillin or kanamycin requires high concentrations of antibiotics and is inefficient (12). The emergence of low-level spontaneous resistance to chloramphenicol has also been encountered (P. Beare, personal observation). Select agent restrictions and natural antibiotic resistance associated with Burkholderia pseudomallei and Burkholderia mallei have prompted the development of nonantibiotic selection methods that exploit metabolic deficiencies or utilize clinically irrelevant resistance determinants (19–21). Nonantibiotic selectable markers have been developed for several other bacterial pathogens (22–24).
Here, we show that heterologous expression of the terminal two genes of the arginine biosynthesis pathway of Legionella pneumophila rescue C. burnetii growth in ACCM-D arginine dropout supplemented with citrulline, a precursor in the arginine biosynthetic pathway. Thus, ACCM-D also enables the isolation of clonal populations using an auxotrophic selectable marker.
MATERIALS AND METHODS
Formulation of ACCM-D.
The components of ACCM-D are listed in Tables 1 and 2. The amino acid concentrations of ACCM-D are based on the concentrations and calculated amino acid compositions of neopeptone, Casamino Acids, and RPMI 1640 cell culture medium (Thermo Fisher Scientific) in ACCM-2 (10). The Becton Dickinson bionutrient technical manual for Bacto neopeptone, a published amino acid analysis of casein (25), and RPMI 1640 product literature (Thermo Fisher Scientific) were used to derive the amino acid compositions (Table 2). An amino acid-free RPMI 1640 powder (1 mg/ml) (United States Biological Life Sciences) was substituted for liquid RPMI 1640. Sodium phosphate and sodium bicarbonate were added to ACCM-D, as these components are absent in amino acid-free RPMI 1640 powder. To generate ACCM-D replete of glucose, a glucose-free, amino acid-free RPMI 1640 powder (1 mg/ml) (United States Biological Life Sciences) was used. Of note, the glucose-free, amino acid-free RPMI 1640 powder contains sodium phosphate, which is not present in the amino acid-free RPMI 1640 powder. Thus, ACCM-D lacking glucose does not require additional sodium phosphate. The final pH of the medium was adjusted to 4.75 using 6 N NaOH and filtered through a 0.22-μm-pore-size filter for sterilization.
TABLE 1.
Composition of ACCM-D
| ACCM-D component | mg/ml | mM |
|---|---|---|
| Citric acid | 2.57 | 13.4 |
| Sodium citrate | 4.74 | 16.1 |
| Potassium phosphate | 0.50 | 3.67 |
| Magnesium chloride | 0.20 | 0.980 |
| Calcium chloride | 0.0132 | 19.7 |
| Sodium chloride | 7.28 | 125.4 |
| Iron sulfate | 0.0028 | 0.010 |
| Sodium phosphate dibasic | 10.0 | 70.4 |
| Sodium bicarbonate | 25.0 | 297.6 |
| Methyl-β-cyclodextrin | 1 | |
| RPMI (−amino acid) powder | 1 | |
| ACCM-D amino acid mix | 3.65 |
TABLE 2.
Amino acid composition of ACCM-D
| Amino acid | Molecular mass (kDa) | mg/ml | mM |
|---|---|---|---|
| l-Alanine | 89.09 | 0.112 | 1.26 |
| l-Arginine monohydrochloride | 210.66 | 0.158 | 0.750 |
| l-Asparagine | 132.12 | 0.088 | 0.666 |
| l-Aspartic acid | 133.10 | 0.072 | 0.541 |
| l-Cysteine hydrochloride monohydrate | 175.63 | 0.274 | 1.56 |
| l-Glutamine | 146.00 | 0.356 | 2.44 |
| l-Glutamic acid potassium salt monohydrate | 203.23 | 0.672 | 3.31 |
| Glycine | 75.07 | 0.088 | 1.17 |
| l-Histidine | 155.15 | 0.055 | 0.354 |
| l-Isoleucine | 131.17 | 0.112 | 0.854 |
| l-Leucine | 131.17 | 0.231 | 1.76 |
| l-Lysine monohydrochloride | 182.65 | 0.261 | 1.43 |
| l-Methionine | 149.21 | 0.068 | 0.455 |
| l-Phenylalanine | 165.19 | 0.104 | 0.630 |
| l-Proline | 115.13 | 0.348 | 3.02 |
| l-Serine | 105.09 | 0.177 | 1.68 |
| l-Threonine | 119.12 | 0.122 | 1.02 |
| l-Tryptophan | 204.23 | 0.050 | 0.245 |
| l-Tyrosine | 181.19 | 0.109 | 0.602 |
| l-Valine | 117.15 | 0.161 | 1.37 |
Bacterial strains and mammalian cells.
The C. burnetii Nine Mile phase II (clone 4, RSA439) strain was used in this study and grown microaerobically in either ACCM-2, ACCM-D, or ACCM-D lacking glucose, as previously described (10). Escherichia coli Stellar (BD Clontech) and PIR1 (Thermo Fisher Scientific) cells were used for recombinant DNA procedures and cultivated in Luria-Bertani (LB) broth. E. coli transformants were selected on LB agar plates containing kanamycin (50 μg/ml) or chloramphenicol (10 μg/ml). African green monkey kidney (Vero) cells (CCL-81; ATCC) were maintained in RPMI 1640 medium containing 10% fetal bovine serum (FBS) at 37°C and 5% CO2.
CFU, infectious FFU, and qPCR assays.
A modified soft-agarose overlay on ACCM agarose plates was used to enumerate CFU, as previously described (10). ACCM agarose plates were made using a 2× solution of ACCM-2, ACCM-D, or ACCM-D lacking glucose and inoculated using an overlay spot titration protocol. Briefly, 10-fold serial dilutions of bacterial cultures were made in 1× ACCM-2, ACCM-D, or ACCM-D lacking glucose. Fifty microliters of molten 0.5% agarose was added to 200 μl of each dilution, mixed, and then 50 μl of the suspension was spotted onto a single ACCM-2, ACCM-D, or ACCM-D lacking glucose agarose plate. The plates were left undisturbed for 1 min to allow the agarose to solidify and were incubated microaerobically for 7 to 10 days to allow the development of visible colonies. The total number of colonies from the lowest dilution showing visible growth was counted using a dissecting microscope at 4× magnification, and the CFU per milliliter were calculated using the dilution factor. To quantify the ability of axenically grown C. burnetii to infect host cells, focus-forming unit (FFU) assays were conducted using Vero cells, as previously described (26). C. burnetii replication in ACCM-2, ACCM-D, or ACCM-D lacking glucose was measured by quantitative PCR (qPCR) of genome equivalents (GE) using a probe specific to dotA, as previously described (4, 7).
Construction of pJB-CAT::argGH and pMiniTn7T-CAT::argGH expression vectors.
The argGH genes were amplified from L. pneumophilia JR32 genomic DNA (gDNA) by PCR using AccuPrime Pfx (Thermo Fischer Scientific) and the primers Arg-pJB-F (5′-CTTCATGAAGGAGGCTGCAGATGAAAAAGGTTATTAAAAAAATCGCATTAG-3′) and ArgGH-pJB-R (5′-GCATGCCTCAGTCGACTTAGCCTCCTTTTAATAATTCATTCAGTG-3′). The argGH PCR product was cloned by In-Fusion (BD Clontech) into pJB-CAT (10, 13) digested with PstI and SalI to create pJB-CAT::argGH. To construct pMiniTn7T-CAT::argGH, the argGH genes were amplified with the primers Arg-miniTn7-F (5′-TGAAGGAGGGAATTCATGAAAAAGGTTATTAAAAAAATCGCATTAG-3′) and ArgGH-miniTn7-R (5′-GCTTCTCGAGGAATTCTTAGCCTCCTTTTAATAATTCATTCAGTG-3′). The CBU1169 promoter was amplified from C. burnetii gDNA using the primers P1169-miniTn7-F (5′-TTACTCAATGGAATTCATGGCTTCGTTTCGCAGCGAAC-3′) and P1169-ArgAux-R (5′-GAATTCCCTCCTTCATGAAGGATTAATGTC-3′). The CBU1169 promoter and argGH PCR products were cloned by In-Fusion (BD Clontech) into pMiniTn7T-CAT (13) digested with EcoRI to create pMiniTn7T-CAT::argGH.
Transformation and selection.
C. burnetii was genetically transformed with 10 μg of pJB-CAT::argGH or with 10 to 20 μg of pMiniTn7T-CAT::argGH and 10 μg of pTnS2::1169P-tnsABCD, as previously described (11). The electroporation mixture (150 μl) was transferred to a T-25 tissue culture flask containing 6 ml of ACCM-D lacking arginine and supplemented with 0.75 mM citrulline and 1% FBS. FBS is used in the first round of selection to prevent sticking of hydrophobic avirulent phase II C. burnetii to the bottom of the flask, which improves transformation efficiency (12). Cultures were incubated for 7 days, and then 1 ml was transferred to a T-25 flask containing 6 ml of ACCM-D lacking arginine and supplemented with 0.75 mM citrulline. Cultures were grown for 7 days, and 50 μl was transferred to a new T-25 flask containing 6 ml of ACCM-D lacking arginine and supplemented with 0.75 mM citrulline, and grown for an additional 7 days. C. burnetii argGH genetic transformants were pelleted by centrifugation for 15 min at 16,000 × g, washed two times with phosphate-buffered saline (1 mM KH2PO4, 155 mM NaCl, 3 mM Na2HPO4 [pH 7.2]), resuspended in 500 μl of amino acid-free cell freezing medium (10% dimethyl sulfoxide, 10 mg/ml methyl-β-cyclodextrin, 1 mg/ml amino acid-free RPMI 1640 powder), and stored at −80°C.
TEM.
T-150 tissue culture flasks containing 50 ml of ACCM-2 or ACCM-D were inoculated with 1 × 106 GE/ml of C. burnetii. Bacteria were incubated microaerobically for 21 days and then processed for transmission electron microscopy (TEM) analysis, as previously described (7).
RESULTS
ACCM-D is a nutritionally defined medium.
ACCM-2 is a complex growth medium for C. burnetii containing both defined and undefined nutrient sources. A defined medium is needed for controlled metabolic studies of C. burnetii and to exploit natural metabolic deficiencies for nutrition-based selection of genetic transformants. Casamino Acids and neopeptone are undefined components within ACCM-2 that provide peptides, amino acids, and other micronutrients. RPMI 1640 supplies the medium with specific amino acids, glucose, vitamins, phosphate, and inorganic salts. To generate a defined medium, comparable amounts of individual amino acids contributed by Casamino Acids and neopeptone in ACCM-2 were added to the defined medium (Table 2). To allow easy manipulation of individual amino acids, an amino acid-free RPMI 1640 powder replaced the liquid RPMI 1640 present in ACCM-2. Sodium phosphate and sodium bicarbonate were also added to the defined medium to account for the loss of these ingredients present in the liquid form of RPMI (Table 1). We termed the new defined medium ACCM-D (see Materials and Methods).
C. burnetii growth and viability are improved in ACCM-D.
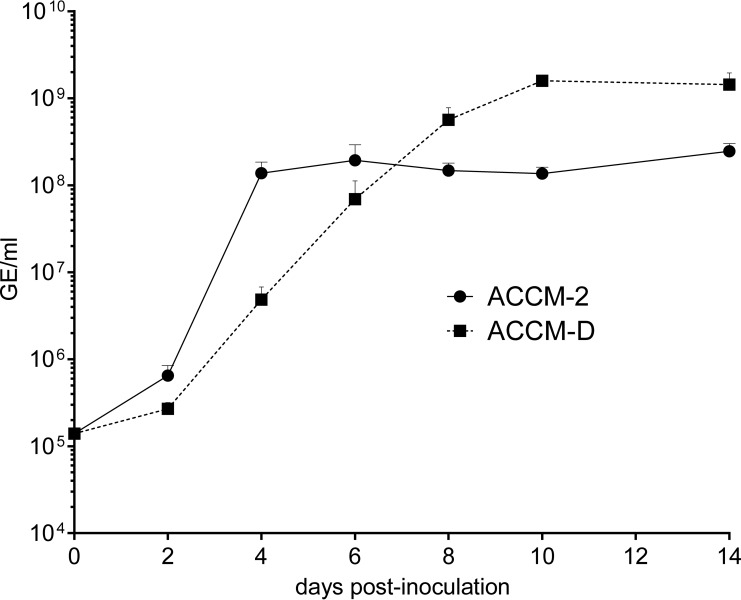
To compare C. burnetii growth in ACCM-D and ACCM-2, we measured bacterial replication in medium over 14 days (Fig. 1). At 10 and 14 days postinoculation (dpi), C. burnetii cultured in ACCM-D replicated approximately 5- to 10-fold more than bacteria cultured in ACCM-2. In addition, bacteria exhibited logarithmic-growth kinetics for approximately 6 days when cultured in ACCM-D, compared to the 2 to 3 days of logarithmic growth in ACCM-2. The growth cycle kinetics of C. burnetii cultured in ACCM-D were similar to those of bacteria cultivated in Vero cells (26).
FIG 1.
ACCM-D supports enhanced growth of C. burnetii. Growth of C. burnetii in ACCM-D and ACCM-2 was assessed using qPCR to quantitate genome equivalents (GE) during a 14-day incubation. C. burnetii displayed a longer logarithmic-growth phase in ACCM-D than that in ACCM-2. The results are expressed as the means of the results from three independent experiments, and the error bars indicate the standard deviations.
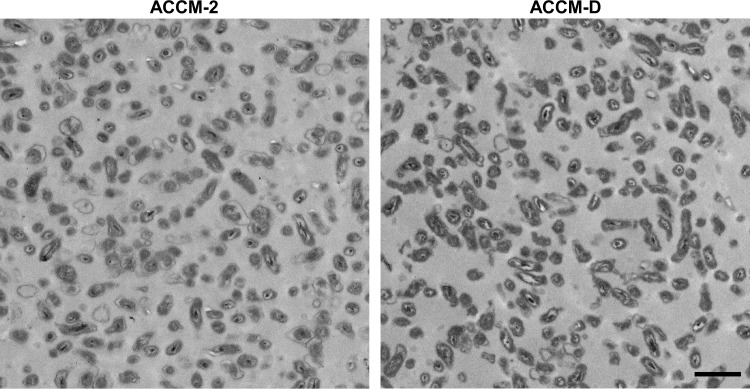
An unusual attribute of Coxiella is the ability to remain in stationary phase for weeks with a negligible loss in viability (9), which correlates with differentiation to the stable small-cell variant (SCV) developmental form (27, 28). However, for unknown reasons, the viability of stationary-phase SCV propagated in ACCM-2, as measured by the GE/FFU ratio, is substantially less than that of host cell-propagated SCV (9), in which GE/FFU ratios approach 6 (29). ACCM-D supported morphological differentiation to the SCV developmental form (Fig. 2). To examine the ability of ACCM-D to support SCV viability, FFU and CFU were enumerated after growth of C. burnetii to stationary phase (14 dpi) in ACCM-D and ACCM-2. C. burnetii grown in ACCM-D exhibited a mean ± standard deviation (SD) GE/FFU ratio of 6.02 ± 3.28, compared to a mean ± SD ratio of 38.77 ± 10.81 for bacteria grown in ACCM-2. The GE/CFU ratio of C. burnetii cultured in ACCM-D was also significantly lower than that of bacteria cultured in ACCM-2 (Table 3). Additionally, C. burnetii colonies that developed on ACCM-D agarose plates were visually larger than those grown on ACCM-2 (data not shown). Collectively, the similar growth cycle kinetics and SCV viability of C. burnetii propagated in ACCM-D and Vero cells suggests that ACCM-D more closely mimics the nutritional conditions encountered by C. burnetii in the mammalian host cell.
FIG 2.
ACCM-D supports morphological transition to the SCV. Transmission electron micrographs showing characteristic small-cell-variant morphology (e.g., condensed chromatin) after growth of C. burnetii in ACCM-2 and ACCM-D for 21 days. Scale bar, 1 μm.
TABLE 3.
Comparison of yield and viability of C. burnetii grown in ACCM-2, ACCM-D, or ACCM-D (−glucose) for 14 daysa
| Medium | GE/ml | FFU/ml | CFU/ml | GE/FFU | GE/CFU |
|---|---|---|---|---|---|
| ACCM-2 | 2.46 × 108 | 6.24 × 106 | 8.75 × 106 | 38.77 ± 10.81 | 18.90 ± 3.21 |
| ACCM-D | 1.44 × 109 | 2.57 × 108 | 4.63 × 108 | 6.02 ± 3.28b | 3.13 ± 3.24b |
| ACCM-D (−glucose) | 1.18 × 109 | 3.00 × 108 | 5.67 × 108 | 3.92 ± 1.05b | 2.42 ± 1.49b |
GE, genome equivalents; FFU, focus-forming units. The results represent the mean of the results from three independent experiments (for GE/ml, FFU/ml, and CFU/ml) or the mean ± standard deviation of the results from three independent experiments (for GE/FFU and GE/CFU).
Statistical difference compared to ACCM-2 determined by one-way analysis of variance (ANOVA) (P < 0.005).
Culture in ACCM-D confirms amino acid auxotrophies.
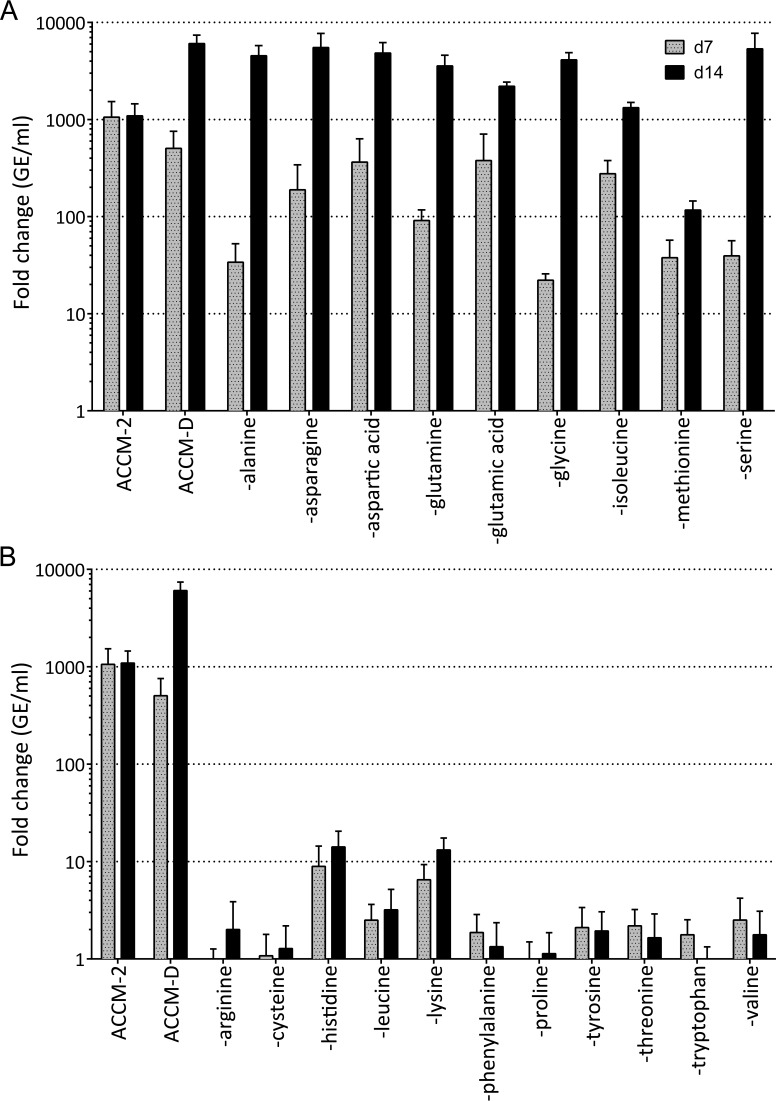
ACCM-D afforded the opportunity to examine C. burnetii amino acid auxotrophies. To score auxotrophies, C. burnetii replication was measured in ACCM-D deficient in each amino acid. Replication was assessed at 7 and 14 dpi in ACCM-2, ACCM-D, or ACCM-D lacking an individual amino acid. C. burnetii was designated auxotrophic or prototrophic for a specific amino acid when replication was <20-fold or >1,000-fold, respectively, over the 14-day incubation period. By these criteria, C. burnetii was judged to be prototrophic for alanine, asparagine, aspartic acid, glutamine, glutamic acid, glycine, isoleucine, and serine (Fig. 3A). Intermediate growth of C. burnetii (100-fold) in ACCM-D lacking methionine was observed (Fig. 3A). Auxotrophy was scored for arginine, cysteine, histidine, leucine, lysine, phenylalanine, proline, tyrosine, threonine, tryptophan, and valine (Fig. 3B). These results are consistent with bioinformatic predictions of amino acid biosynthesis pathways encoded by the C. burnetii Nine Mile RSA493 reference strain genome, with the exception of growth in media lacking methionine and isoleucine (5, 6).
FIG 3.
Growth behavior in ACCM-D confirms C. burnetii amino acid auxotrophies. Amino acid prototrophies (A) and auxotrophies (B) of C. burnetii are indicated by growth characteristics in ACCM-D. Individual amino acids were omitted to generate ACCM-D amino acid dropout media. Media were inoculated with C. burnetii, and the fold change in bacterial replication was determined by qPCR to quantitate genome equivalents (GE) at 7 days (d7) and 14 days (d14) postinoculation. The results are expressed as the means of the results from three independent experiments, and the error bars indicate the standard deviations. Auxotrophy was scored as a fold change in GE/ml of <20 by 14 days postinoculation, while prototrophy was scored as a fold change in GE/ml of >1,000. A partial dependence on methionine was observed.
Arginine auxotrophy can be complemented with terminal L. pneumophila arginine biosynthesis genes and citrulline supplementation.
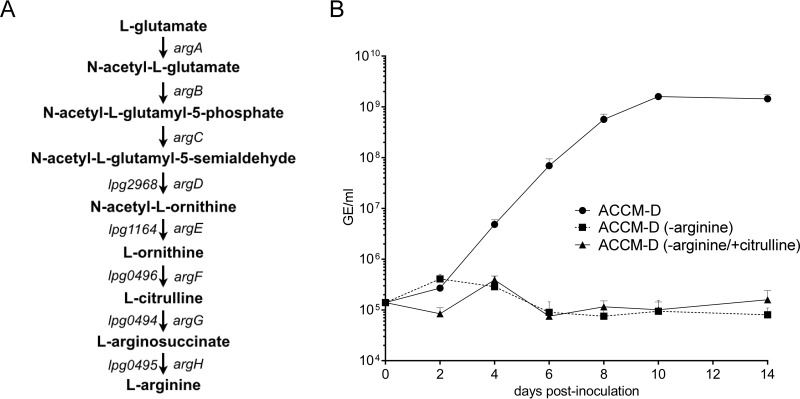
The restricted use of antibiotics for C. burnetii genetic selection prompted us to determine if we could exploit the intrinsic arginine auxotrophy of the organism to create a nonantibiotic method of genetic selection. The components of the bacterial arginine biosynthetic pathway required for the conversion of glutamate into arginine are typically encoded by argABCDEFGH (Fig. 4A) (30, 31). C. burnetii lacks all arg genes, rendering it an arginine auxotroph. L. pneumophila, a close relative of C. burnetii, contains the argDEFGH genes, which complete the terminal steps of arginine biosynthesis (Fig. 4A) (32). C. burnetii encodes an arginine/ornithine-type transporter (ArtPIQM) (5, 6, 33), which likely compensates for the absence of arginine biosynthetic genes. The ArtPIQM system is composed of two transmembrane transport proteins (ArtQ and ArtM), an ATP-binding ATPase (ArtP), and a periplasm-localized arginine/ornithine binding protein (ArtI), which facilitate in a coordinated manner the transport of arginine and ornithine across the inner membrane (34). Although it is unknown if C. burnetii ArtI can also bind and transport citrulline, a Pasteurella haemolytica ArtI homolog called LapT is competitively inhibited by citrulline, suggesting that the substrate specificity of ArtI might also include this arginine precursor (35).
FIG 4.
Citrulline does not complement C. burnetii growth in ACCM-D lacking arginine. (A) Schematic of the arginine biosynthesis pathway. L. pneumophila contains argDEFGH with argG (lpg0494, argininosuccinate synthase), argH (lpg0495, argininosuccinate lyase), and argF (lpg0496, ornithine carbamoyltransferase) arranged in a predicted operon (32). (B) Growth of C. burnetii in ACCM-D, ACCM-D minus arginine, or ACCM-D minus arginine and supplemented with citrulline was assessed using qPCR to quantitate genome equivalents (GE) during a 14-day incubation. The results are expressed as the means of the results from three independent experiments, and the error bars indicate the standard deviations.
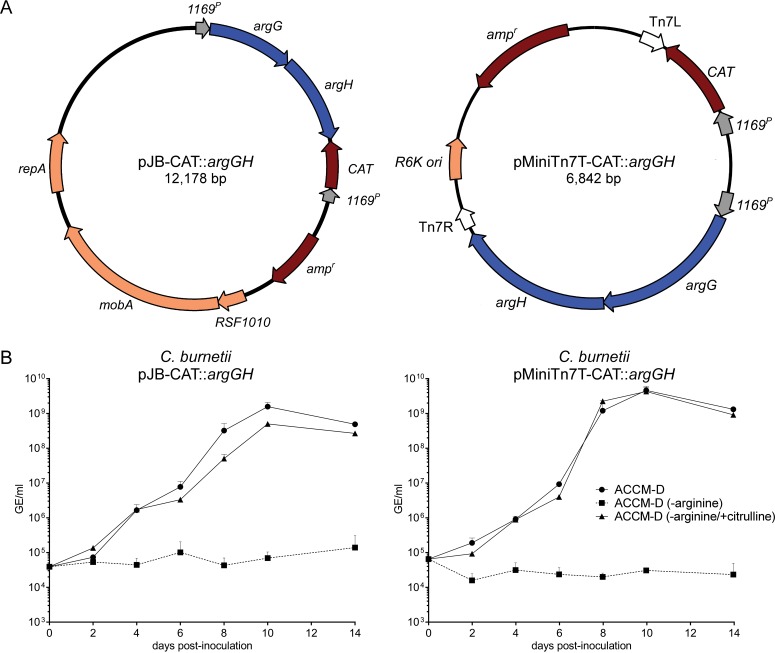
In L. pneumophila, ArgG (argininosuccinate synthase) and ArgH (argininosuccinate lyase) convert citrulline into arginine (Fig. 4A). To investigate if L. pneumophila argGH can complement the intrinsic arginine auxotrophy of C. burnetii, we first examined C. burnetii growth in arginine-deficient ACCM-D supplemented with citrulline. Consistent with the lack of arginine biosynthesis enzymes, wild-type C. burnetii did not grow in this medium (Fig. 4B). L. pneumophila argGH genes were then cloned under the control of the CBU1169 promoter into two C. burnetii expression vectors: pJB-CAT for multicopy-plasmid expression, and pMiniTn7T-CAT for single-copy-chromosome expression (13) (Fig. 5A). Growth of C. burnetii expressing argGH in single or multiple copies was restored when citrulline was added to arginine-deficient ACCM-D (Fig. 5B). Collectively, these data demonstrate that argGH is a selectable genetic marker when used in conjunction with ACCM-D lacking arginine and supplemented with citrulline.
FIG 5.
Genetic transformation with pJB-CAT::argGH or pMiniTn7T-CAT::argGH complements C. burnetii arginine auxotrophy in ACCM-D lacking arginine but supplemented with citrulline. (A) Plasmid maps of pJB-CAT::argGH and pMiniTn7T-CAT::argGH containing argGH from L. pneumophila. (B) Growth of C. burnetii transformed with pJB-CAT::argGH or pMiniTn7T-CAT::argGH in ACCM-D, ACCM-D minus arginine, or ACCM-D minus arginine and supplemented with citrulline. Growth was quantified using qPCR to determine genome equivalents (GE) during a 14-day incubation. The results are expressed as the means of the results from three independent experiments, and the error bars indicate the standard deviations.
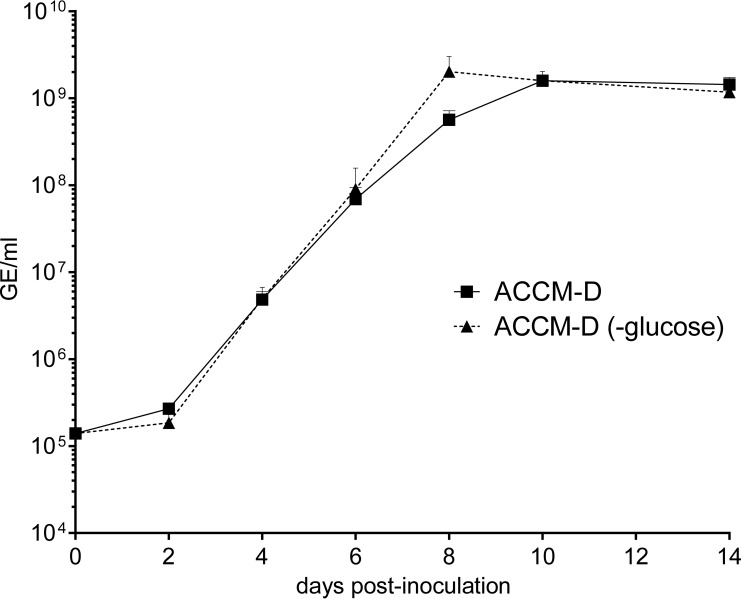
Glucose is not required for C. burnetii growth.
The importance of exogenous glucose in central carbon metabolism of C. burnetii is unresolved (8, 15, 36). ACCM-D contains RPMI 1640 cell culture medium that contains glucose at a concentration of approximately 1.39 mM. Thus, to generate ACCM-D lacking glucose, an amino acid-free, glucose-free RPMI 1640 powder was substituted. Bacteria grown in ACCM-D and ACCM-D lacking glucose replicated comparably, indicating that glucose is not required for axenic growth (Fig. 6 and Table 3). This result demonstrates that Coxiella can be propagated in medium containing only inorganic salts, vitamins, and amino acids.
FIG 6.
C. burnetii does not require glucose for growth in ACCM-D. Growth of C. burnetii in ACCM-D lacking glucose was assessed using qPCR to quantify genome equivalents (GE) during a 14-day incubation in ACCM-D and ACCM-D lacking glucose. The results are expressed as the means of the results from three independent experiments, and the error bars indicate the standard deviations.
DISCUSSION
In the current study, we describe the development of ACCM-D, a nutritionally defined medium that supports increased replication of C. burnetii compared to that in previous generations of ACCM (7, 9, 10). The yield of C. burnetii grown in ACCM-D is approximately 5- to 10-fold greater than that achieved with ACCM-2. Interestingly, the logarithmic-growth rate is lower in ACCM-D and resembles that of host cell-grown organisms (26). Furthermore, ACCM-D supports morphological transition to the SCV developmental form, which displays increased viability over SCV generated in ACCM-2 as assessed by infectivity for Vero cells and colony formation on agarose plates. ACCM-D offers a significant improvement over current C. burnetii axenic culture media in terms of bacterial yield and viability and the ability to precisely define medium components for metabolic studies.
The study of C. burnetii central metabolic processes using intracellular culture methods or complex media, such as ACCM-2, is difficult. Consequently, knowledge of C. burnetii catabolic and anabolic potential is predominantly based on metabolic reconstruction using the genome sequence of the Nine Mile RSA493 reference strain (5, 6). The development of nutritionally defined ACCM-D now allows the omission of individual amino acids and other nutrients to assess their contributions to C. burnetii metabolism, replication, and progression through the developmental cycle. Indeed, growth studies using ACCM-D lacking specific amino acids validate predicted C. burnetii auxotrophies for arginine, cysteine, histidine, leucine, lysine, phenylalanine, proline, threonine, tyrosine, tryptophan, and valine (5). C. burnetii grew in the absence of isoleucine and, to a lesser degree, methionine, despite predicted auxotrophy for these amino acids. Growth in the absence of isoleucine suggests that C. burnetii may operate an alternative isoleucine biosynthesis pathway similar to that of other bacteria (37–39). The citramalate-dependent pathway utilizes citramalate synthase (CimA) to synthesize isoleucine from pyruvate and acetyl-coenzyme A (CoA) (39). Although C. burnetii leuA (cbu0520) shares homology to cimA, genes encoding the enzymes required to complete the remaining steps in the pathway are not readily identifiable, leaving the question of the potential mechanism of C. burnetii isoleucine biosynthesis unresolved. The reason why ACCM-D lacking methionine supports moderate growth of C. burnetii is also unclear. In E. coli, the conversion of aspartate to methionine involves the activities of MetA and MetB, which are absent in C. burnetii. However, C. burnetii might use one of several alternative pathways for methionine biosynthesis, as it contains several met genes (40). A predicted methionine-specific ABC transporter (CBU0107 to CBU0109) likely compensates for an inability to synthesize sufficient levels of methionine (41, 42).
Optimal axenic growth and viability of C. burnetii in ACCM-D do not require exogenous glucose. The organism appears to be capable of transporting glucose via a glucose proton symporter (CBU0265), and the sugar is metabolized at low levels in acidic buffers (8, 15). However, C. burnetii is missing a classical hexokinase for the generation of glucose-6-phosphate that can be degraded for anabolic and catabolic purposes by glycolysis. C. burnetii also lacks a UhpT-like transporter for glucose-6-phosphate and is devoid of a glucose-specific phosphotransferase system capable of phosphorylating glucose at the expense of phosphoenolpyruvate (5, 6). An alternative route to glucose-6-phosphate by C. burnetii may involve a transphosphorylation reaction between carbamoyl phosphate and glucose, catalyzed by a predicted membrane-bound glucose-6-phosphatase (CBU1267) (36, 43). Although glucose is unnecessary for axenic growth, a recent transcriptome study suggests that glucose is an important carbon source during intracellular growth (44). Lysosomes contain a glucose transporter and accumulate glycogen, which is broken down to glucose by lysosomal acid α-glucosidase (45, 46). Thus, the C. burnetii phagolysosome-like replication vacuole may contain ample glucose. Substantial differences in carbon metabolism have been documented for bacterial pathogens during axenic and intracellular growth (47); however, defining the significance of glucose during intracellular growth of C. burnetii will require additional experimentation.
Knowledge of C. burnetii amino acid auxotrophies exhibited during culture in ACCM-D provided an opportunity to develop a nonantibiotic method for genetic selection. C. burnetii lacks genes responsible for arginine biosynthesis, consistent with its observed arginine auxotrophy, but it does encode a predicted arginine/ornithine-type transporter (ArtPIQM). L. pneumophila is an arginine auxotroph that has retained argDEFGH, genes that are responsible for the terminal steps of arginine biosynthesis (32). C. burnetii expression of L. pneumophila argGH, along with citrulline transport, possibly mediated by the ArtPIQM, allows growth of C. burnetii in ACCM-D lacking arginine and supplemented with citrulline.
Interestingly, C. burnetii encodes a predicted arginine repressor (ArgR, CBU0480) upstream of the artPIQM arginine transporter operon. In the presence of arginine, ArgR inhibits the transcription of arginine (ARG)-box-containing genes and acts as a coactivator for the transcription of other genes (48–50). The expression of L. pneumophila argR is regulated by the stationary-phase sigma factor RpoS (51), and a L. pneumophila argR mutant exhibits impaired growth in amoebae (32). The L. pneumophila ArgR regulon encodes proteins with diverse functions that include type IV secretion system effectors, amino acid and nucleotide metabolism, transport and binding, detoxification, and stress adaptation (32). Although L. pneumophila argR is required for growth in amoebae, it is not required for growth in THP-1 human macrophages, underscoring the effect that altered nutritional niches have on the activation of distinct regulatory responses (32). As with L. pneumophila, we predict that arginine availability regulates physiologic processes beyond arginine acquisition in C. burnetii. ACCM-D will enable future studies examining ArgR transcriptional regulation by C. burnetii.
There are additional possibilities for auxotrophic selectable markers based on the intrinsic C. burnetii amino acid biosynthetic deficiencies identified in this study. For example, a nearly complete lysine biosynthesis pathway is present in C. burnetii, but the enzyme diaminopimelic acid decarboxylase (LysA) that converts meso-2,6-diaminopimelate into lysine is missing. However, meso-2,6-diaminopimelate is a component of C. burnetii peptidoglycan (52), indicating that C. burnetii can synthesize this lysine intermediate. These data suggest that C. burnetii lysine auxotrophy can be complemented via heterologous expression of lysA in ACCM-D replete of lysine. Indeed, a similar approach was used to complement lysine auxotrophy in Mycobacterium bovis BCG (53, 54).
Exploitation of host amino acid metabolism by intracellular bacteria is an emerging paradigm (55, 56). There is prominent overlap between the amino acid auxotrophies of C. burnetii, L. pneumophila, and other intracellular bacteria and the essential amino acids of the mammalian host cell (57, 58). L. pneumophila replicates intracellularly within an endoplasmic reticulum-derived vacuole and can utilize amino acids as its main source of carbon and energy (59–64). To generate a sufficient supply of amino acids to support growth, L. pneumophila promotes proteasomal degradation of polyubiquitinated proteins surrounding the pathogen vacuole (65) and relies upon the host cell amino acid transporter solute carrier (SLC) protein SLC1A5 (66). SLC proteins are responsible for shuttling nutrients across plasma, lysosome, and other organelle membranes (67). Endolysosomal compartments that fuse with the C. burnetii-containing vacuole contain numerous SLC proteins (4, 68, 69). It is logical to hypothesize that, like Legionella, C. burnetii hijacks host cell peptide or amino acid transport to acquire amino acids needed for growth. Moreover, the C. burnetii vacuole shows robust engagement with autophagosomes predicted to deliver proteins destined for degradation to amino acids by lysosomal proteases (70–72).
The metabolic interlock between pathogen and host has spurred interest in studying nutritional virulence associated with intracellular bacteria (47, 58, 73, 74). The exploitation of host cell amino acid pools by C. burnetii remains an unexplored area of investigation that will be facilitated by the tools and findings presented here. ACCM-D now enables an assessment of C. burnetii nutritional requirements that promote its intracellular parasitic lifestyle, and it provides an alternative method of genetic selection based on amino acid auxotrophies.
ACKNOWLEDGMENTS
We thank Charles Larson for critical review of the manuscript, Anita Mora and Austin Athman for graphic support, Bryan Hansen for transmission electron microscopy, and Howard Shuman for sharing the CFU enumeration protocol.
This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
REFERENCES
- 1.Williams JC. 1991. Infectivity, virulence, and pathogenicity of Coxiella burnetii for various hosts, p 21–71. In Williams JC, Thompson HA (ed), Q fever: the biology of Coxiella burnetii. CRC Press, Inc., Boca Raton, FL. [Google Scholar]
- 2.Maurin M, Raoult D. 1999. Q fever. Clin Microbiol Rev 12:518–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Schaik EJ, Chen C, Mertens K, Weber MM, Samuel JE. 2013. Molecular pathogenesis of the obligate intracellular bacterium Coxiella burnetii. Nat Rev Microbiol 11:561–573. doi: 10.1038/nrmicro3049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howe D, Shannon JG, Winfree S, Dorward DW, Heinzen RA. 2010. Coxiella burnetii phase I and II variants replicate with similar kinetics in degradative phagolysosome-like compartments of human macrophages. Infect Immun 78:3465–3474. doi: 10.1128/IAI.00406-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seshadri R, Paulsen IT, Eisen JA, Read TD, Nelson KE, Nelson WC, Ward NL, Tettelin H, Davidsen TM, Beanan MJ, Deboy RT, Daugherty SC, Brinkac LM, Madupu R, Dodson RJ, Khouri HM, Lee KH, Carty HA, Scanlan D, Heinzen RA, Thompson HA, Samuel JE, Fraser CM, Heidelberg JF. 2003. Complete genome sequence of the Q-fever pathogen Coxiella burnetii. Proc Natl Acad Sci U S A 100:5455–5460. doi: 10.1073/pnas.0931379100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beare PA, Unsworth N, Andoh M, Voth DE, Omsland A, Gilk SD, Williams KP, Sobral BW, Kupko JJ III, Porcella SF, Samuel JE, Heinzen RA. 2009. Comparative genomics reveal extensive transposon-mediated genomic plasticity and diversity among potential effector proteins within the genus Coxiella. Infect Immun 77:642–656. doi: 10.1128/IAI.01141-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omsland A, Cockrell DC, Howe D, Fischer ER, Virtaneva K, Sturdevant DE, Porcella SF, Heinzen RA. 2009. Host cell-free growth of the Q fever bacterium Coxiella burnetii. Proc Natl Acad Sci U S A 106:4430–4434. doi: 10.1073/pnas.0812074106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hackstadt T, Williams JC. 1981. Biochemical stratagem for obligate parasitism of eukaryotic cells by Coxiella burnetii. Proc Natl Acad Sci U S A 78:3240–3244. doi: 10.1073/pnas.78.5.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandoz KM, Sturdevant DE, Hansen B, Heinzen RA. 2014. Developmental transitions of Coxiella burnetii grown in axenic media. J Microbiol Methods 96:104–110. doi: 10.1016/j.mimet.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Omsland A, Beare PA, Hill J, Cockrell DC, Howe D, Hansen B, Samuel JE, Heinzen RA. 2011. Isolation from animal tissue and genetic transformation of Coxiella burnetii are facilitated by an improved axenic growth medium. Appl Environ Microbiol 77:3720–3725. doi: 10.1128/AEM.02826-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beare PA, Larson CL, Gilk SD, Heinzen RA. 2012. Two systems for targeted gene deletion in Coxiella burnetii. Appl Environ Microbiol 78:4580–4589. doi: 10.1128/AEM.00881-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beare PA, Heinzen RA. 2014. Gene inactivation in Coxiella burnetii. Methods Mol Biol 1197:329–345. doi: 10.1007/978-1-4939-1261-2_19. [DOI] [PubMed] [Google Scholar]
- 13.Beare PA. 2012. Genetic manipulation of Coxiella burnetii. Adv Exp Med Biol 984:249–271. doi: 10.1007/978-94-007-4315-1_13. [DOI] [PubMed] [Google Scholar]
- 14.Omsland A, Cockrell DC, Fischer ER, Heinzen RA. 2008. Sustained axenic metabolic activity by the obligate intracellular bacterium Coxiella burnetii. J Bacteriol 190:3203–3212. doi: 10.1128/JB.01911-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hackstadt T, Williams JC. 1981. Stability of the adenosine 5′-triphosphate pool in Coxiella burnetii: influence of pH and substrate. J Bacteriol 148:419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hackstadt T, Williams JC. 1983. pH dependence of the Coxiella burnetii glutamate transport system. J Bacteriol 154:598–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hackstadt T. 1983. Estimation of the cytoplasmic pH of Coxiella burnetii and effect of substrate oxidation on proton motive force. J Bacteriol 154:591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mingeot-Leclercq MP, Glupczynski Y, Tulkens PM. 1999. Aminoglycosides: activity and resistance. Antimicrob Agents Chemother 43:727–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schweizer HP, Peacock SJ. 2008. Antimicrobial drug-selection markers for Burkholderia pseudomallei and B. mallei. Emerg Infect Dis 14:1689–1692. doi: 10.3201/eid1411.080431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zajdowicz SL, Jones-Carson J, Vazquez-Torres A, Jobling MG, Gill RE, Holmes RK. 2011. Alanine racemase mutants of Burkholderia pseudomallei and Burkholderia mallei and use of alanine racemase as a non-antibiotic-based selectable marker. PLoS One 6:e21523. doi: 10.1371/journal.pone.0021523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norris MH, Kang Y, Lu D, Wilcox BA, Hoang TT. 2009. Glyphosate resistance as a novel select-agent-compliant, non-antibiotic-selectable marker in chromosomal mutagenesis of the essential genes asd and dapB of Burkholderia pseudomallei. Appl Environ Microbiol 75:6062–6075. doi: 10.1128/AEM.00820-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mignon C, Sodoyer R, Werle B. 2015. Antibiotic-free selection in biotherapeutics: now and forever. Pathogens 4:157–181. doi: 10.3390/pathogens4020157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanchez-Romero JM, Diaz-Orejas R, De Lorenzo V. 1998. Resistance to tellurite as a selection marker for genetic manipulations of Pseudomonas strains. Appl Environ Microbiol 64:4040–4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herrero M, de Lorenzo V, Timmis KN. 1990. Transposon vectors containing non-antibiotic resistance selection markers for cloning and stable chromosomal insertion of foreign genes in Gram-negative bacteria. J Bacteriol 172:6557–6567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sales MG, de Freitas O, Zucoloto S, Okano N, Padovan GJ, dos Santos JE, Greene LJ. 1995. Casein, hydrolyzed casein, and amino acids that simulate casein produce the same extent of mucosal adaptation to massive bowel resection in adult rats. Am J Clin Nutr 62:87–92. [DOI] [PubMed] [Google Scholar]
- 26.Coleman SA, Fischer ER, Howe D, Mead DJ, Heinzen RA. 2004. Temporal analysis of Coxiella burnetii morphological differentiation. J Bacteriol 186:7344–7352. doi: 10.1128/JB.186.21.7344-7352.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCaul TF, Hackstadt T, Williams JC. 1981. Ultrastructural and biological aspects of Coxiella burnetii under physical disruptions, p 267–280. In Burgdorfer W, Anacker RL (ed), Rickettsiae and rickettsial diseases. Academic Press, New York, NY. [Google Scholar]
- 28.McCaul TF, Williams JC. 1981. Developmental cycle of Coxiella burnetii: structure and morphogenesis of vegetative and sporogenic differentiations. J Bacteriol 147:1063–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cockrell DC, Beare PA, Fischer ER, Howe D, Heinzen RA. 2008. A method for purifying obligate intracellular Coxiella burnetii that employs digitonin lysis of host cells. J Microbiol Methods 72:321–325. doi: 10.1016/j.mimet.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cunin R, Glansdorff N, Pierard A, Stalon V. 1986. Biosynthesis and metabolism of arginine in bacteria. Microbiol Rev 50:314–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu SE, Soule JD, Gross DC. 2003. Characterization of the argA gene required for arginine biosynthesis and syringomycin production by Pseudomonas syringae pv. syringae. Appl Environ Microbiol 69:7273–7280. doi: 10.1128/AEM.69.12.7273-7280.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hovel-Miner G, Faucher SP, Charpentier X, Shuman HA. 2010. ArgR-regulated genes are derepressed in the Legionella-containing vacuole. J Bacteriol 192:4504–4516. doi: 10.1128/JB.00465-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ren Q, Chen K, Paulsen IT. 2007. TransportDB: a comprehensive database resource for cytoplasmic membrane transport systems and outer membrane channels. Nucleic Acids Res 35:D274–D279. doi: 10.1093/nar/gkl925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caldara M, Minh PN, Bostoen S, Massant J, Charlier D. 2007. ArgR-dependent repression of arginine and histidine transport genes in Escherichia coli K-12. J Mol Biol 373:251–267. doi: 10.1016/j.jmb.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 35.Caskey LS, Lamphear JG, Highlander SK. 1996. Binding-protein-dependent arginine transport in Pasteurella haemolytica. Microbiology 142:1739–1747. doi: 10.1099/13500872-142-7-1739. [DOI] [PubMed] [Google Scholar]
- 36.Omsland A, Heinzen RA. 2011. Life on the outside: the rescue of Coxiella burnetii from its host cell. Annu Rev Microbiol 65:111–128. doi: 10.1146/annurev-micro-090110-102927. [DOI] [PubMed] [Google Scholar]
- 37.Risso C, Van Dien SJ, Orloff A, Lovley DR, Coppi MV. 2008. Elucidation of an alternate isoleucine biosynthesis pathway in Geobacter sulfurreducens. J Bacteriol 190:2266–2274. doi: 10.1128/JB.01841-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu B, Zhang B, Feng X, Rubens JR, Huang R, Hicks LM, Pakrasi HB, Tang YJ. 2010. Alternative isoleucine synthesis pathway in cyanobacterial species. Microbiology 156:596–602. doi: 10.1099/mic.0.031799-0. [DOI] [PubMed] [Google Scholar]
- 39.Xu H, Zhang Y, Guo X, Ren S, Staempfli AA, Chiao J, Jiang W, Zhao G. 2004. Isoleucine biosynthesis in Leptospira interrogans serotype lai strain 56601 proceeds via a threonine-independent pathway. J Bacteriol 186:5400–5409. doi: 10.1128/JB.186.16.5400-5409.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferla MP, Patrick WM. 2014. Bacterial methionine biosynthesis. Microbiology 160:1571–1584. doi: 10.1099/mic.0.077826-0. [DOI] [PubMed] [Google Scholar]
- 41.Merlin C, Gardiner G, Durand S, Masters M. 2002. The Escherichia coli metD locus encodes an ABC transporter which includes Abc (MetN), YaeE (MetI), and YaeC (MetQ). J Bacteriol 184:5513–5517. doi: 10.1128/JB.184.19.5513-5517.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gál J, Szvetnik A, Schnell R, Kálmán M. 2002. The metD d-methionine transporter locus of Escherichia coli is an ABC transporter gene cluster. J Bacteriol 184:4930–4932. doi: 10.1128/JB.184.17.4930-4932.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paretsky D, Consigli RA, Downs CM. 1962. Studies on the physiology of rickettsiae. III. Glucose phosphorylation and hexokinase activity in Coxiella burnetii. J Bacteriol 83:538–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kuley R, Bossers-deVries R, Smith HE, Smits MA, Roest HI, Bossers A. 2015. Major differential gene regulation in Coxiella burnetii between in vivo and in vitro cultivation models. BMC Genomics 16:953. doi: 10.1186/s12864-015-2143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mancini GM, Beerens CE, Verheijen FW. 1990. Glucose transport in lysosomal membrane vesicles. Kinetic demonstration of a carrier for neutral hexoses. J Biol Chem 265:12380–12387. [PubMed] [Google Scholar]
- 46.Zirin J, Nieuwenhuis J, Perrimon N. 2013. Role of autophagy in glycogen breakdown and its relevance to chloroquine myopathy. PLoS Biol 11:e1001708. doi: 10.1371/journal.pbio.1001708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eisenreich W, Dandekar T, Heesemann J, Goebel W. 2010. Carbon metabolism of intracellular bacterial pathogens and possible links to virulence. Nat Rev Microbiol 8:401–412. doi: 10.1038/nrmicro2351. [DOI] [PubMed] [Google Scholar]
- 48.Maas WK. 1994. The arginine repressor of Escherichia coli. Microbiol Rev 58:631–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caldara M, Charlier D, Cunin R. 2006. The arginine regulon of Escherichia coli: whole-system transcriptome analysis discovers new genes and provides an integrated view of arginine regulation. Microbiology 152:3343–3354. doi: 10.1099/mic.0.29088-0. [DOI] [PubMed] [Google Scholar]
- 50.Kiupakis AK, Reitzer L. 2002. ArgR-independent induction and ArgR-dependent superinduction of the astCADBE operon in Escherichia coli. J Bacteriol 184:2940–2950. doi: 10.1128/JB.184.11.2940-2950.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hovel-Miner G, Pampou S, Faucher SP, Clarke M, Morozova I, Morozov P, Russo JJ, Shuman HA, Kalachikov S. 2009. SigmaS controls multiple pathways associated with intracellular multiplication of Legionella pneumophila. J Bacteriol 191:2461–2473. doi: 10.1128/JB.01578-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Amano K, Williams JC. 1984. Sensitivity of Coxiella burnetii peptidoglycan to lysozyme hydrolysis and correlation of sacculus rigidity with peptidoglycan-associated proteins. J Bacteriol 160:989–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nascimento IP, Dias WO, Quintilio W, Hsu T, Jacobs WR Jr, Leite LC. 2009. Construction of an unmarked recombinant BCG expressing a pertussis antigen by auxotrophic complementation: protection against Bordetella pertussis challenge in neonates. Vaccine 27:7346–7351. doi: 10.1016/j.vaccine.2009.09.043. [DOI] [PubMed] [Google Scholar]
- 54.Saubi N, Gea-Mallorqui E, Ferrer P, Hurtado C, Sánchez-Úbeda S, Eto Y, Gatell JM, Hanke T, Joseph J. 2014. Engineering new mycobacterial vaccine design for HIV-TB pediatric vaccine vectored by lysine auxotroph of BCG. Mol Ther Methods Clin Dev 1:14017. doi: 10.1038/mtm.2014.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Popp J, Noster J, Busch K, Kehl A, Zur Hellen G, Hensel M. 2015. Role of host cell-derived amino acids in nutrition of intracellular Salmonella enterica. Infect Immun 83:4466–4475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brissac T, Ziveri J, Ramond E, Tros F, Kock S, Dupuis M, Brillet M, Barel M, Peyriga L, Cahoreau E, Charbit A. 2015. Gluconeogenesis, an essential metabolic pathway for pathogenic Francisella. Mol Microbiol 98:518–534. doi: 10.1111/mmi.13139. [DOI] [PubMed] [Google Scholar]
- 57.Young VR. 1994. Adult amino acid requirements: the case for a major revision in current recommendations. J Nutr 124:1517S–1523S. [DOI] [PubMed] [Google Scholar]
- 58.Abu Kwaik Y, Bumann D. 2013. Microbial quest for food in vivo: ‘nutritional virulence’ as an emerging paradigm. Cell Microbiol 15:882–890. doi: 10.1111/cmi.12138. [DOI] [PubMed] [Google Scholar]
- 59.Molofsky AB, Swanson MS. 2004. Differentiate to thrive: lessons from the Legionella pneumophila life cycle. Mol Microbiol 53:29–40. doi: 10.1111/j.1365-2958.2004.04129.x. [DOI] [PubMed] [Google Scholar]
- 60.Warren WJ, Miller RD. 1979. Growth of Legionnaires disease bacterium (Legionella pneumophila) in chemically defined medium. J Clin Microbiol 10:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.George JR, Pine L, Reeves MW, Harrell WK. 1980. Amino acid requirements of Legionella pneumophila. J Clin Microbiol 11:286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tesh MJ, Miller RD. 1981. Amino acid requirements for Legionella pneumophila growth. J Clin Microbiol 13:865–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ristroph JD, Hedlund KW, Gowda S. 1981. Chemically defined medium for Legionella pneumophila growth. J Clin Microbiol 13:115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pine L, George JR, Reeves MW, Harrell WK. 1979. Development of a chemically defined liquid medium for growth of Legionella pneumophila. J Clin Microbiol 9:615–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Price CT, Al-Quadan T, Santic M, Rosenshine I, Abu Kwaik Y. 2011. Host proteasomal degradation generates amino acids essential for intracellular bacterial growth. Science 334:1553–1557. doi: 10.1126/science.1212868. [DOI] [PubMed] [Google Scholar]
- 66.Wieland H, Ullrich S, Lang F, Neumeister B. 2005. Intracellular multiplication of Legionella pneumophila depends on host cell amino acid transporter SLC1A5. Mol Microbiol 55:1528–1537. doi: 10.1111/j.1365-2958.2005.04490.x. [DOI] [PubMed] [Google Scholar]
- 67.Hediger MA, Clémençon B, Burrier RE, Bruford EA. 2013. The ABCs of membrane transporters in health and disease (SLC series): introduction. Mol Aspects Med 34:95–107. doi: 10.1016/j.mam.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schröder BA, Wrocklage C, Hasilik A, Saftig P. 2010. The proteome of lysosomes. Proteomics 10:4053–4076. doi: 10.1002/pmic.201000196. [DOI] [PubMed] [Google Scholar]
- 69.Taylor PM. 2014. Role of amino acid transporters in amino acid sensing. Am J Clin Nutr 99:223S–230S. doi: 10.3945/ajcn.113.070086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Newton HJ, Kohler LJ, McDonough JA, Temoche-Diaz M, Crabill E, Hartland EL, Roy CR. 2014. A screen of Coxiella burnetii mutants reveals important roles for Dot/Icm effectors and host autophagy in vacuole biogenesis. PLoS Pathog 10:e1004286. doi: 10.1371/journal.ppat.1004286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Winchell CG, Graham JG, Kurten RC, Voth DE. 2014. Coxiella burnetii type IV secretion-dependent recruitment of macrophage autophagosomes. Infect Immun 82:2229–2238. doi: 10.1128/IAI.01236-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Romano PS, Gutierrez MG, Berón W, Rabinovitch M, Colombo MI. 2007. The autophagic pathway is actively modulated by phase II Coxiella burnetii to efficiently replicate in the host cell. Cell Microbiol 9:891–909. doi: 10.1111/j.1462-5822.2006.00838.x. [DOI] [PubMed] [Google Scholar]
- 73.Abu Kwaik Y. 2015. Nutrition-based evolution of intracellular pathogens. Environ Microbiol Rep 7:2–3. doi: 10.1111/1758-2229.12236. [DOI] [PubMed] [Google Scholar]
- 74.Zhang YJ, Rubin EJ. 2013. Feast or famine: the host-pathogen battle over amino acids. Cell Microbiol 15:1079–1087. doi: 10.1111/cmi.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]