Ibrutinib has been shown to be beneficial for B-cell malignancies with overall response rates of 71% in initial clinical trials for chronic lymphocytic leukemia (CLL), irrespective of high-risk characteristics [Byrd et al. 2013; Parmar et al. 2014]. Ibrutinib, a Bruton’s tyrosine kinase (BTK) inhibitor approved for the treatment of selected leukemias and lymphomas, has been associated with bleeding events [Byrd et al. 2013, 2014; Wang et al. 2013]. Kamel and colleagues illustrated that BTK inhibitors, such as ibrutinib, cause an interruption in collagen-mediated platelet aggregation, and thus increase bleeding risk [Kamel et al. 2015]. Levade and colleagues demonstrated ibrutinib’s effects on adhesion of platelets to von Willebrand factor by the disruption of collagen receptors. It was also shown that removal of the drug, and the generation of new, unaffected platelets provided a decrease in the risk of bleeding [Levade et al. 2014]. While as many as 50% (or half) of patients may experience grade 1 or 2 bleeding on ibrutinib, other studies have revealed more serious bleeding events [Jones et al. 2014]. Wang and colleagues evaluated patients with mantle cell lymphoma being treated with ibrutinib. Approximately 5% of patients were shown to have grade 3 or higher bleeding events; however, the majority of these patients had sustained some sort of trauma [Wang et al. 2013]. Burger and colleagues compared ibrutinib with chlorambucil as initial therapy for patients with CLL. The median treatment duration with ibrutinib was 17.4 months, and major hemorrhage was reported in 4% of these patients [Burger et al. 2015]. Despite a noted disruption in platelet function, ibrutinib has been shown to improve overall platelet counts with the control of the underlying CLL [Farooqui et al. 2012]. Jones and colleagues evaluated the concomitant use of antiplatelet agents and anticoagulants in patients treated with ibrutinib, and the majority of the patients having major bleeding were treated with one of these agents, in addition to the BTK inhibitor [Jones et al. 2014].
Though major bleeding events have been present in patients treated with ibrutinib, the role of vascular remodeling has not previously been described. We present the case of a patient with an unusual bleeding event secondary to a vascular anomaly on ibrutinib for the treatment of CLL. The patient is a 46-year-old man treated for CLL with ibrutinib with no other medical history. He had no prior lines of therapy for his disease. At presentation he had diffuse lymphadenopathy, lymphocytosis with a white blood count of 35,000 mm3, splenomegaly and platelet count of 65,000 mm3. The patient had Rai stage IV CLL at diagnosis which was his indication for treatment. Three months after starting therapy, he experienced a dramatic positive response both in lymph node size and peripheral blood counts. WBC did increase to 55,700 mm3 within a month of treatment but had normalized to 5600 mm3 within 3 months. However, he was admitted to the hospital 3 months after initiating therapy with a severe headache and found to have a subarachnoid hemorrhage on CT and magnetic resonance imaging. Ibrutinib was discontinued upon hospitalization. He was not on any home medications including antiplatelet agents or anticoagulants at the time of this event, nor was any trauma experienced prior to admission. He had no prior history of bleeding diathesis. His prothrombin time (PT), partial thromboplastin time (PTT) and fibrinogen were within normal limits and his platelet count was 99,000 mm3, which was a significant improvement from his pretreatment platelet count of 65,000 mm3. His pretreatment hemoglobin (Hb) was 12.6 g/dl and had normalized to 15.3 g/dl within 3 months of treatment. Hb was stable throughout hospitalization averaging 15 g/dl, as well as platelet count, with no evidence of autoimmune hemolysis. Initial angiography was normal, but 5 days later repeat angiography demonstrated slow filling of an unusual aneurysm arising from the basilar artery demonstrated by the blue arrow in panels A and B of Figure 1. Three days later, a third angiogram was performed which showed spontaneous resolution of the aneurysm. Ibrutinib was held during the patient’s hospitalization and he ultimately recovered. He had no further bleeding episodes. We hypothesize that ibrutinib may interact with the collagen component of vasculature, leading to abnormal remodeling which may be associated with the increased risk of bleeding described with this agent.
Figure 1.
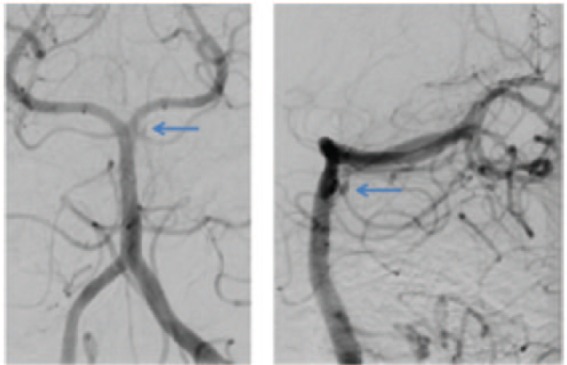
Angiogram performed on day 8 of hospitalization demonstrating unusual aneurysm. The blue arrow in panels A and B indicates location of this abnormal aneurysm from different views. This aneurysm was not present on initial angiography and was absent during angiography 3 days later for a planned intervention.
Some researchers have used this known disruption in collagen structure and function as a beneficial side effect of ibrutinib. Dubovsky and colleagues described using the drug to deliberately interrupt collagen’s role in forming the fibrotic tissue changes that contribute to chronic graft-versus-host disease [Dubovsky et al. 2014]. The aforementioned patient likely did not have bleeding that was secondary to disrupted platelet aggregation, but rather, we hypothesize that ibrutinib may have caused some intermittent disruption or remodeling of the collagen fibers comprising his vasculature. This intermittent nature of disruption could explain his lack of initial aneurysm at presentation, spontaneous aneurysm formation, and its subsequent resolution with removal of the drug. The package insert for ibrutinib quotes a 6% grade 3 or higher bleeding risk in patients treated with ibrutinib, with this risk increased in patients on other anticoagulants or antiplatelet therapy (ibrutinib package insert, Pharmacyclics, Sunnyvale, CA, 2013). As the mechanism for bleeding events secondary to ibrutinib is not completely understood, this case illustrates that abnormal vascular remodeling leading to aberrations in normal vasculature could be a component of these hemorrhagic events in addition to disruption in platelet aggregation.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Eric Wiedower, Department of Hematology/Oncology, The West Clinic/University of Tennessee Health Science Center, 2699 Tangbourne Drive, Memphis, TN 38119, USA.
Felicia Hare, Department of Internal Medicine, The University of Tennessee Health Science Center, Memphis, TN, USA.
Adam Arthur, Semmes-Murphy Neurologic and Spine Institute, The University of Tennessee Health Science Center, Memphis, TN, USA.
Jason Chandler, Department of Hematology/Oncology, The West Clinic, The University of Tennessee Health Science Center, Memphis, TN, USA.
Michael G. Martin, Department of Hematology/Oncology, The West Clinic, The University of Tennessee Health Science Center, Memphis, TN, USA
References
- Burger J., Tedeschi A., Barr P., Robak T., Owen C., Ghia P., et al. (2015) Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med 373: 2425–2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd J., Brown J., O’Brien S., Barrientos J., Kay N., Reddy N., et al. (2014) Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med 371: 213–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd J., Furman R., Coutre S., Flinn I., Burger J., Blum K., et al. (2013) Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med 369: 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubovsky J., Flynn R., Du J., Harrington B., Zhong Y., Kaffenberger B., et al. (2014) Ibrutinib treatment ameliorates murine chronic graft-versus-host disease. J Clin Invest 124: 4867–4876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooqui M., Lozier J., Valdez J., Saba N., Wells A., Soto S., et al. (2012, November) Ibrutinib (PCI 32765) rapidly improves platelet counts in chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) patients and has minimal effects on platelet aggregation. Blood 120: abstract 1789. [Google Scholar]
- Jones J., Hillmen P., Coutre S., Tam C., Furman R., Barr P., et al. (2014) Pattern of use of anticoagulation and/or antiplatelet agents in patients with chronic lymphocytic leukemia (CLL) treated with single-agent ibrutinib therapy. Blood 124: 1990–1990. [Google Scholar]
- Kamel S., Horton L., Ysebaert L., Levade M., Burbury K., Tan S., et al. (2015) Ibrutinib inhibits collagen-mediated but not ADP-mediated platelet aggregation. Leukemia 29: 783–787. [DOI] [PubMed] [Google Scholar]
- Levade M., David E., Garcia C., Laurent P., Cadot S., Michallet A., et al. (2014) Ibrutinib treatment affects collagen and Von Willebrand factor-dependent platelet functions. Blood 124: 3991–3995. [DOI] [PubMed] [Google Scholar]
- Parmar S., Patel K., Pinilla-Ibarz J. (2014) Ibrutinib (Imbruvica): a novel targeted therapy for chronic lymphocytic leukemia. Pharm Ther 39: 483–519. [PMC free article] [PubMed] [Google Scholar]
- Wang M., Rule S., Martin P., Goy A., Auer R., Kahl B., et al. (2013) Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med 369: 507–516. [DOI] [PMC free article] [PubMed] [Google Scholar]


