Abstract
Background
Theoretical domains framework (TDF) provides an integrative model for assessing barriers to behavioral changes in order to suggest interventions for improvement in behavior and ultimately outcomes. However, there are other tools that are used to assess barriers.
Objective
The objective of this study is to determine the degree of concordance between domains and constructs identified in two versions of the TDF including original (2005) and refined version (2012) and independent studies of other tools.
Methods
We searched six databases for articles that studied barriers to health-related behavior changes of health care professionals or the general public. We reviewed quantitative papers published in English which included their questionnaires in the article. A table including the TDF domains of both original and refined versions and related constructs was developed to serve as a reference to describe the barriers assessed in the independent studies; descriptive statistics were used to express the results.
Results
Out of 552 papers retrieved, 50 were eligible to review. The barrier domains explored in these articles belonged to two to eleven domains of the refined TDF. Eighteen articles (36%) used constructs outside of the refined version. The spectrum of barrier constructs of the original TDF was broader and could meet the domains studied in 48 studies (96%). Barriers in domains of “environmental context and resources”, “beliefs about consequences”, and “social influences” were the most frequently explored in 42 (84%), 37 (74%), and 33 (66%) of the 50 articles, respectively.
Conclusion
Both refined and original TDFs cataloged barriers measured by the other studies that did not use TDF as their framework. However, the original version of TDF explored a broader spectrum of barriers than the refined version. From this perspective, the original version of the TDF seems to be a more comprehensive tool for assessing barriers in practice.
Keywords: theoretical domains framework, TDF, practice change, health care quality improvement, barriers
Background
Knowledge translation and quality improvement (QI) efforts aimed at improving processes and outcomes in health care are plagued by many barriers.1–5 Indeed, barriers at the individual, team, organizational, social, economic, and political levels can dramatically reduce the effectiveness of implementation strategies and lead to suboptimal health care outcomes and increased costs.1,2,7,8 Low-quality care is estimated to account for 20%–40% of total health care industry by health care professionals.8
Theoretical domains framework (TDF) has been developed for systematically identifying and assessing barriers to change interventions and is an umbrella of 33 theories of behavior change.3,5,9,10 It is considered a “ coherent theoretical framework of health-professional behaviors” modification, and its use may facilitate practice changes, knowledge translation, and QI based on sound theories.9,11
For performance improvement and professional development, TDF can be helpful at various levels by identifying barriers to practice change and change theories to address these barriers through a systematic approach, as well as in developing theory-informed interventions for clinical performance improvement and for evaluating and detecting effectiveness of these interventions.3,5,9
The original TDF was developed in 2005 with 12 domains and 128 constructs; it has been used in various studies in different disciplines between 2005 and 2012.5 In 2012, its validity was reevaluated, and a refined version of the TDF was proposed with 14 domains and 84 constructs.3 A questionnaire was developed in 2014 to facilitate its adoption as a framework for practice change.12 Several other tools however, which do not make an explicit reference to TDF as their conceptual framework, have also been developed and used for assessing barriers to change in health service research. Thus, a comparison of the barriers assessed in these questionnaires to those included in TDF is important to identify similarities and differences in order to make informed decisions in choosing a tool. Furthermore, although TDF is the single tool that has been built specifically to assess all kind of barriers systematically, it is still new (the original version was developed in 2005 and revised version in 2012). Therefore, it is important to evaluate the experience and knowledge with TDF to inform clinicians of the advantages and strengths, as well as areas that can be improved. The purpose of this study was to review the published literature on barriers to change to identify specific tools created without explicit reference to TDF and to investigate the similarities and differences of the domains and constructs between TDF (original and refined versions) and these tools. To our knowledge, this is the first review of the TDF content which compares the tools used to assess barriers (developed independently of TDF) to the TDF domains to determine if the TDF is comprehensive and addresses all barriers. Therefore, this study provides unique information that is useful for clinicians and researchers to assess barriers before implementing interventions.
Methods
Search methods for identifying studies
Using a combination of possible Medical Subject Heading terms with free text words related to the concepts derived from research question, a detailed search strategy was developed in MEDLINE-OvidSP which can be found in Table S1. This search strategy was validated by comparing the search results to a defined set of four sentinel articles that were selected by a team of two subject experts and met inclusion criteria for our review; all four sentinel studies were found among the retrieved articles. The search strategy was then translated into other databases using the appropriate controlled vocabulary and free text words in order to search appropriate studies.
The following resources were searched in order to identify the studies from the beginning of indexing papers in these databases until April 2014: Ovid MEDLINE: OvidSP, PubMed, CINAHL, PsycINFO (including full text from PsycARTICLES), EBSCO databases: Academic Search Complete, and Google Scholar.
Criteria for considering studies
We included all articles reporting studies on barriers to change in health-related behavior with no limitation in terms of research methodology and study design. Participants in the studies were either individuals whose health-related knowledge, beliefs, attitudes, and behaviors were reported or health care professionals whose work-related practices were studied. Only papers published in English were included. Qualitative studies were excluded from the review. We also excluded articles that did not publish their barrier assessment questionnaire or survey, either as supplement or in the contents of the paper.
Data collection, abstraction, and analysis
Selection process of the studies
After controlling for duplicates, the titles and abstracts of all potentially relevant studies were reviewed and evaluated for possible inclusion by two reviewers (MM and HHS) working independently. Both reviewers (MM and HHS) independently agreed on including 88% of the included articles (44 out of 50), before any discussion. Disagreements on the inclusion of other 12% of included papers (six out of 50) deemed relevant by one reviewer (HHS) were resolved by discussion and referring unresolved disagreements to a content expert (JPC) after reviewing full-text paper.
Data abstraction and analysis
A table including domains of TDF and related constructs was developed, and descriptive statistics were used. Definitions of all domains and constructs were generated using TDF (2005 and 2012), professional and regular dictionaries such as American Psychological Association (APA) Dictionary of Psychology, The Cambridge Dictionary of Psychology, Dictionary of Psychology and Allied Health Sciences, Dictionary of Psychological Testing, Assessment and Treatment, Oxford English Dictionary, as well as reliable internet sources, and used as references during data abstraction (Table is available upon request).13–18 We developed our own list of constructs definitions in order to use the most updated resources specially APA Dictionary of Psychology (as the most important references in TDF), last version of which was released in 2015.18 All barriers addressed in the articles were classified with reference to the table, using the constructs and domains definitions. Data abstraction and analyses were conducted by two reviewers (MM and HHS) working independently who are both specialized in behavior modification in health, cognitive medical anthropology, health education and health promotion, and qualitative and quantitative research. Kappa interrater reliability before agreement was 0.86 (P=0.000). Disagreements were resolved through discussion between reviewers and consulting with a third party (JPC) to get to complete agreement.
In this paper, we are defining construct as “a concept specially devised to be part of a theory”, a domain as “an area of interest; a sphere of thought, action or knowledge”, and a theoretical domain as “a group of related theoretical constructs”.5
Results
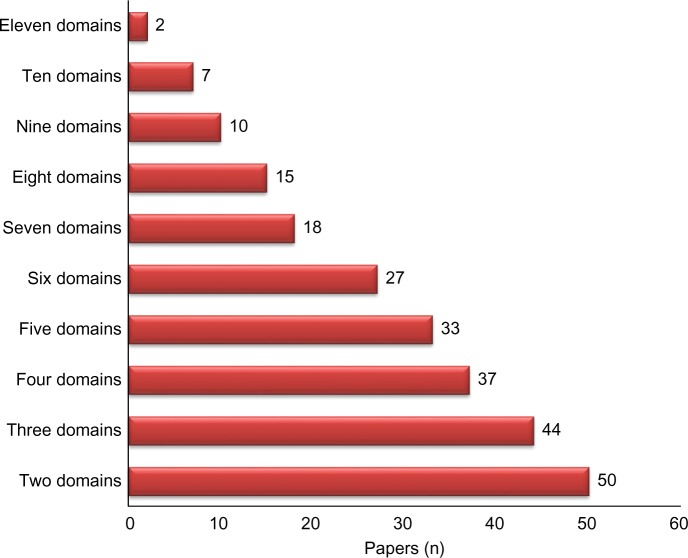
A total of 552 papers were retrieved. After removing duplicates, articles that had been informed by TDF, and articles that were not relevant or did not satisfy our inclusion criteria, 50 papers were selected for final review (Figure 1).2,19–67 In the 50 reviewed articles, 961 items were used for assessing various barriers, on average 19 items per article. Details of items in each questionnaire and for each domain are presented in Table S2.
Figure 1.
Process of identifying publications.
Abbreviation: TDF, theoretical domains framework.
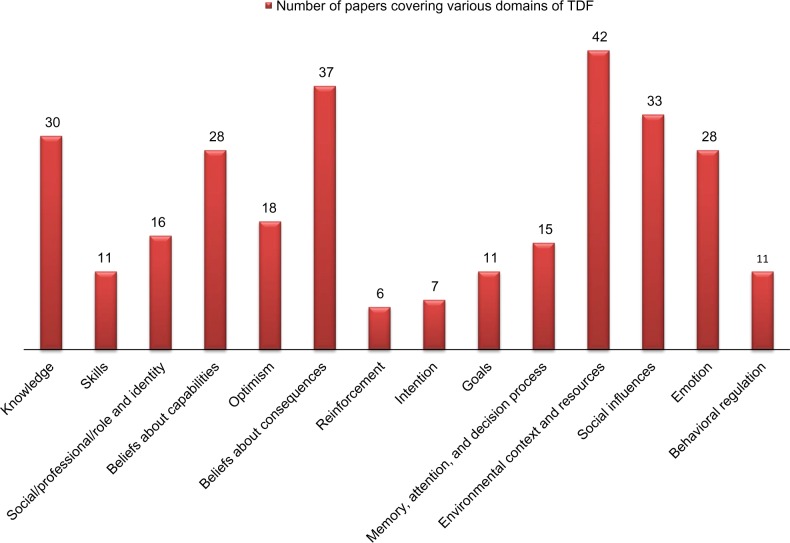
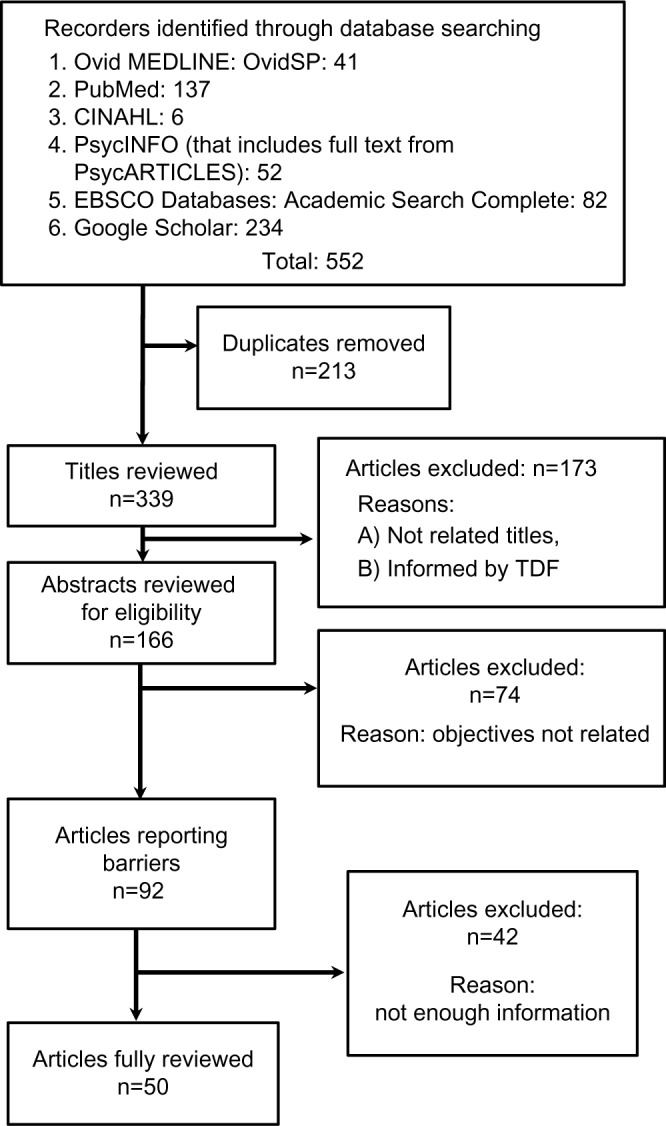
On average, the 50 articles focused on six domains (95% confidence interval: 5.1–6.6) of the refined TDF, and they covered at least two domains; 37 papers (74%) covered four domains and 27 papers (54%) covered six domains. Only two papers (4%) covered up to eleven domains (Figure 2). Domains of “environmental context and resources”, “beliefs about consequences”, and “social influences” were the three domains of refined TDF assessed most frequently in the reviewed studies, so that 42, 37, and 33 out of 50 papers (84%, 74%, and 66%, respectively) had assessed barriers in these domains (Figure 3). “Reinforcement” and “intention”, on the other hand, were the domains of the refined TDF that were the least assessed in the studies; “reinforcement” was studied in only six articles (12%) and “intention” in seven (14%) (Figure 3).
Figure 2.
Number of domains of theoretical domains framework covered by reviewed papers (N=50).
Figure 3.
Frequency of papers covering various domains of TDF (N=50).
Abbreviation: TDF, theoretical domains framework.
The refined version of TDF excluded barriers cited in 18 articles (36%) of papers, while the original TDF excluded only barriers cited in two articles (4%). The excluded barriers in 18 articles were mostly related to the removal of domains or constructs from the original version of TDF in the process of creating refined version in 2012 (“characteristics of the innovation/nature of behavior itself ”, “intrinsic motivation”, “attitudes”, “competitive concerns/conflicting demands”, “perceived severity and perceived susceptibility”, and “past experiences”). However, the excluded barriers in the two papers assessed barriers that were outside of domains of both versions of TDF. These barriers focused on “involvement/engagement”, “importance of the desired change”, “preferences”, and “expectations” that we did not find obvious fit with any TDF domains.
Discussion
A coherent theoretical framework of health-professional behaviors is useful to facilitate a systematic approach for identifying barriers and planning interventions aimed at practice change for QI.9,11,68 Our finding that the barrier domains in the refined and original versions of TDF were satisfactory for covering 64% and 96% of barriers in the reviewed articles confirms the comprehensiveness of TDF, especially the original version, as a framework for assessing barriers to behavior modification and explaining practice changes.10 Indeed, between 2005 and 2012, various health care research teams in different countries (Australia, UK, Denmark, and Canada) have applied TDF to inform practice; its usefulness has been confirmed in various health care systems.3,12
Our findings are consistent with those of Francis et al who reported that out of 133 papers from 83 scientific journals indexed in the Scopus database that cited TDF, 21 studies used TDF as an overarching framework for their work.10 Francis et al concluded that TDF-related publications in 13 journals and its application in six countries implied a substantial coverage and interdisciplinary impact. They also highlighted its usefulness as a diagnostic tool to identify mediators of practice improvement and barriers to the implementation of evidence-based practice and QI which is confirmed by French et al.9,10
The TDF domain most often cited in the 50 articles reviewed was “environmental context and resources” in 42 papers (84%). This may imply that environmental context is an important source of barriers or that “environmental context and resources” encompasses numerous types of barriers.69
“Reinforcement” and “intention”, on the other hand, were the least studied, assessed in only six (12%) and seven (14%) of all reviewed articles, respectively. This may reflect a perceived lack of significance of these domains for knowledge users and decision makers. These results were not expected in context of extensive literature supporting the importance of barriers related to “reward-punishment system”, “readiness to change”, and “stages of change”, which are related to these two domains for influencing practice change.70–73
Our finding that barriers in some of the reviewed articles were not cataloged by TDF is interesting and supported by literature. Thirty-six percent of the articles had barriers not captured in the refined TDF and 4% in the original version of TDF. Barriers in the cited 36% tried to assess “characteristics of the innovation/nature of behavior itself ”, “intrinsic motivation”, “attitudes”, and “competitive concerns/conflicting demands”, which had been covered in the original TDF either as a domain (“nature of behavior/characteristics of innovation”) or as constructs under other domains (“intrinsic motivation”, for instance, was covered under the domain “motivation and goals”, “attitudes” was covered under “beliefs about consequences” domain, and “conflict—competing demands, conflicting roles” was covered under the domain “social influences”). Furthermore, “perceived severity” and “perceived susceptibility” had been covered in the original TDF under the domain “beliefs about consequences” as “perceived risk/threat”. The structure of the original TDF and its changes are described briefly in Table S3.3,5 Our finding that the original TDF with a broader range of constructs was more comprehensive than the refined version and compatible with the researchers’ needs is supported by other researchers.12 In the process of developing and validating a user-friendly questionnaire based on TDF, Huijg et al concluded that the original (2005) version of TDF with 12 domains and 128 constructs is more applicable for assessing barriers in practice, while they partially supported the refined TDF.12 In addition, authors of a recent study that has tried to use refined TDF in QI have used the original TDF for informing their interview and focus group questions, implying more practicality for the original version of TDF.74
There were also a few barriers (“involvement/engagement”, “importance of the desired change”, “preferences”, “expectations”) identified in two articles (4%) that could not be found in any TDF versions. Besides a possible shift in behavior change theories over time, another reason for this discrepancy may lie on the difference in definitions of some constructs as we developed our own definition list with the last edition of APA dictionary (2015).5,18 A possible misclassification due to varying scopes of subjective definitions may also be considered; for instance, other researchers may have classified “engagement/involvement” into the construct “team working” that was part of the “social influences” domain in the original TDF; however, any decision to classify constructs in one category or another is subject to critics, given the numerous assumptions in the absence of clear operational definitions.
We also found that there is a need for more clarification about assigning items into the domain of “emotion”. For instance, when a person is saying “I am scared of side effects of medication” or when a practitioner is saying “I fear that this approach may lead to more issues in complex patients”, should these be categorized in the domain of emotion (construct of fear) or are they making references to the consequences, or both? This confirms Wilkinson et al’s finding that more clarification regarding operationalization of TDF would streamline its application.75
Findings of this study should be considered in light of several limitations that may affect some of our results. Non-English papers and qualitative researches were excluded. We also eliminated the articles that did not include their questionnaires in the publication. In addition, the findings are based on the questionnaires developed by the authors of the reviewed articles, and not empirical data. Furthermore, we added the term guidelines in the search strategy since we were aiming to include articles studying barriers to health-related behavior of public people, as well as barriers to clinical practice of health care professionals. Therefore, we may have missed some papers. Like original TDF itself, some constructs were defined using general resources, although we have tried to keep these as low as possible. Finally, we did not assess the quality of the original studies. We do not think, however, that these limitations invalidate our conclusions.
Conclusion
Both refined and original versions of TDF covered well barriers measured by the studies that did not make references to TDF. This result reinforces the idea that TDF is a coherent theoretical framework for measuring barriers to improve or change health-related behaviors among public people or health care professionals. In practice, however, the original version of TDF showed a broader scope of barrier constructs that better fit the researchers’ comprehensive needs. More research may need to see if our findings are supported.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
Author contributions
MM contributed to the conception and design of the study, and the acquisition, analysis, and interpretation of data. HHS contributed to acquisition, analysis, and interpretation of data. NK and JPC contributed to conception and design of the study. All authors contributed toward drafting and critically revising the paper, read and approved the final manuscript, and agree to be accountable for all aspects of the work. This project was not supported by any funding.
References
- 1.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 2.Larson E. A tool to assess barriers to adherence to hand hygiene guideline. Am J Infect Control. 2004;32(1):48–51. doi: 10.1016/j.ajic.2003.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lugtenberg M, Zegers-van Schaick JM, Westert GP, Burgers JS. Why don’t physicians adhere to guideline recommendations in practice? An analysis of barriers among Dutch general practitioners. Implement Sci. 2009;4:54. doi: 10.1186/1748-5908-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33. doi: 10.1136/qshc.2004.011155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabana MD, Rushton JL, Rush AJ. Implementing practice guidelines for depression: applying a new framework to an old problem. Gen Hosp Psychiatry. 2002;24(1):35–42. doi: 10.1016/s0163-8343(01)00169-4. [DOI] [PubMed] [Google Scholar]
- 7.Della Penna R, Martel H, Neuwirth EB, et al. Rapid spread of complex change: a case study in inpatient palliative care. BMC Health Serv Res. 2009;9:245. doi: 10.1186/1472-6963-9-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sollecito WA, Johnson J. McLaughlin and KalCuzny’s Continuous Quality Improvement in Health Care. 4th ed. Burlington, MA: Jones and Bartlett Learning; 2013. The global evolution of continuous quality improvement: from Japanese manufacturing to global health services. [Google Scholar]
- 9.French SD, Green SE, O’Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7(1):38. doi: 10.1186/1748-5908-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Francis JJ, O’Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci. 2012;7:35. doi: 10.1186/1748-5908-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sudsawad P. Knowledge Translation: Introduction to Models, Strategies, and Measures. The National Center for the Dissemination of Disability Research; 2007. [Accessed February 5, 2016]. Available from: http://www.ncddr.org/kt/products/ktintro/ktintro.pdf. [Google Scholar]
- 12.Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci. 2014;9:11. doi: 10.1186/1748-5908-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.VandenBos G. APA Dictionary of Psychology. Washington, DC: American Psychological Association (APA); 2007. [Google Scholar]
- 14.Matsumoto D. The Cambridge Dictionary of Psychology. New York, NY: Cambridge University Press; 2009. [Google Scholar]
- 15.Stuart-Hamilton I. Dictionary of Psychological Testing, Assessment and Treatment. 2nd ed. London, UK: Jessica Kingsley Publishers; 2007. [Google Scholar]
- 16.Roeckelein J. Elsevier’s Dictionary of Psychological Theories. Amsterdam: Elsevier; 2006. [Google Scholar]
- 17.Bhatia M. Dictionary of Psychology and Allied Health Sciences. New Delhi: New Age International (P) Ltd., Publishers; 2009. [Google Scholar]
- 18.VandenBos GR. APA Dictionary of Psychology. 2nd ed. Washington, DC: American Psychological Association (APA); 2015. [Google Scholar]
- 19.Mollem ED, Snoek FJ, Heine RJ. Assessment of perceived barriers in self-care of insulin-requiring diabetic patients. Patient Educ Couns. 1996;29(3):277–281. doi: 10.1016/s0738-3991(96)00926-3. [DOI] [PubMed] [Google Scholar]
- 20.Young M, Read J, Barker-Collo S, Harrison R. Evaluating and overcoming barriers to taking abuse histories. Prof Psychol Res Pract. 2001;32(4):407–414. [Google Scholar]
- 21.O’Carroll RE, Foster C, McGeechan G, Sandford K, Ferguson E. The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol. 2011;30(2):236–245. doi: 10.1037/a0022379. [DOI] [PubMed] [Google Scholar]
- 22.Heinowitz AE, Brown KR, Langsam LC, et al. Identifying perceived personal barriers to public policy advocacy within psychology. Prof Psychol Res Pract. 2012;43(4):372–378. [Google Scholar]
- 23.Sudom K, Zamorski M, Garber B. Stigma and barriers to mental health care in deployed Canadian forces personnel. Mil Psychol. 2012;24(4):414–431. [Google Scholar]
- 24.Pidano AE, Kimmelblatt CA, Neace WP. Behavioral health in the pediatric primary care setting: needs, barriers, and implications for psychologists. Psychol Serv. 2011;8(3):151–165. [Google Scholar]
- 25.Ouimette P, Vogt D, Wade M, et al. Perceived barriers to care among veterans health administration patients with posttraumatic stress disorder. Psychol Serv. 2011;8(3):212–223. [Google Scholar]
- 26.Gordon AJ, Kavanagh G, Krumm M, et al. Facilitators and barriers in implementing buprenorphine in the Veterans Health Administration. Psychol Addict Behav. 2011;25(2):215–224. doi: 10.1037/a0022776. [DOI] [PubMed] [Google Scholar]
- 27.Perepletchikova F, Hilt LM, Chereji E, Kazdin AE. Barriers to implementing treatment integrity procedures: survey of treatment outcome researchers. J Consult Clin Psychol. 2009;77(2):212–218. doi: 10.1037/a0015232. [DOI] [PubMed] [Google Scholar]
- 28.Vincent N, Lewycky S, Finnegan H. Barriers to engagement in sleep restriction and stimulus control in chronic insomnia. J Consult Clin Psychol. 2008;76(5):820–828. doi: 10.1037/0022-006X.76.5.820. [DOI] [PubMed] [Google Scholar]
- 29.Mansfield AK, Addis ME, Courtenay W. Measurement of men’s help seeking: development and evaluation of the barriers to help seeking scale. Psychol Men Masc. 2005;6(2):95–108. [Google Scholar]
- 30.Martin DJ, Brooks RA, Ortiz DJ, Veniegas RC. Perceived employment barriers and their relation to workforce-entry intent among people with HIV/AIDS. J Occup Health Psychol. 2003;8(3):181–194. doi: 10.1037/1076-8998.8.3.181. [DOI] [PubMed] [Google Scholar]
- 31.Catz SL, Kelly JA, Bogart LM, Benotsch EG, Mcauliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19(2):124–133. [PubMed] [Google Scholar]
- 32.de Vos ML, van der Veer SN, Graafmans WC, et al. Implementing quality indicators in intensive care units: exploring barriers to and facilitators of behaviour change. Implement Sci. 2010;5:52. doi: 10.1186/1748-5908-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mills E, Wilson K, Rachlis B, et al. Barriers to participation in HIV drug trials: a systematic review. Lancet Infect Dis. 2006;6(1):32–38. doi: 10.1016/S1473-3099(05)70324-8. [DOI] [PubMed] [Google Scholar]
- 34.Bryar RM, Closs SJ, Baum G, et al. The Yorkshire BARRIERS project: diagnostic analysis of barriers to research utilisation. Int J Nurs Stud. 2003;40(1):73–84. doi: 10.1016/s0020-7489(02)00039-1. [DOI] [PubMed] [Google Scholar]
- 35.Tucker CM, Rice KG, Desmond FF, Hou W, Kaye LB, Smith TM. The youth form of the Motivators of and Barriers to Health-Smart Behaviors Inventory. Psychol Assess. 2012;24(2):490–502. doi: 10.1037/a0026262. [DOI] [PubMed] [Google Scholar]
- 36.Tu VP, Husson F, Sutan A, Ha DT, Valentin D. For me the taste of soy is not a barrier to its consumption. And how about you? Appetite. 2012;58(3):914–921. doi: 10.1016/j.appet.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 37.Collet J-P, Kissoon N, Skippen P, et al. Engaging pediatric intensive care unit (PICU) clinical staff to lead practice improvement: the PICU participatory action research project (PICU-PAR) Implement Sci. 2014;9:6. doi: 10.1186/1748-5908-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seid M, Opipari-Arrigan L, Gelhard LR, Varni JW, Driscoll K. Barriers to care questionnaire: reliability, validity, and responsiveness to change among parents of children with asthma. Acad Pediatr. 2009;9(2):106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Cahill NE, Murch L, Cook D, Heyland DK. Barriers to feeding critically ill patients: a multicenter survey of critical care nurses. J Crit Care. 2012;27(6):727–734. doi: 10.1016/j.jcrc.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 40.Welsh EM, Jeffery RW, Levy RL, et al. Measuring perceived barriers to healthful eating in obese, treatment-seeking adults. J Nutr Educ Behav. 2012;44(6):507–512. doi: 10.1016/j.jneb.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Venner KL, Greenfield BL, Vicuña B, Muñoz R, Bhatt S, O’Keefe V. “I’m not one of them”: barriers to help-seeking among American Indians with alcohol dependence. Cultur Divers Ethnic Minor Psychol. 2012;18(4):352–362. doi: 10.1037/a0029757. [DOI] [PubMed] [Google Scholar]
- 42.Timen A, Hulscher MEJL, Rust L, et al. Barriers to implementing infection prevention and control guidelines during crises: experiences of health care professionals. Am J Infect Control. 2010;38(9):726–733. doi: 10.1016/j.ajic.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams MT, Domanico J, Marques L, Leblanc NJ, Turkheimer E. Barriers to treatment among African Americans with obsessive-compulsive disorder. J Anxiety Disord. 2012;26(4):555–563. doi: 10.1016/j.janxdis.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simon SL, Duncan CL, Janicke DM, Wagner MH. Barriers to treatment of paediatric obstructive sleep apnoea: development of the adherence barriers to continuous positive airway pressure (CPAP) questionnaire. Sleep Med. 2012;13(2):172–177. doi: 10.1016/j.sleep.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 45.Aiken AM, Gold MA, Parker AM. Changes in young women’s awareness, attitudes, and perceived barriers to using emergency contraception. J Pediatr Adolesc Gynecol. 2005;18(1):25–32. doi: 10.1016/j.jpag.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 46.Park E, Song M. Communication barriers perceived by older patients and nurses. Int J Nurs Stud. 2005;42(2):159–166. doi: 10.1016/j.ijnurstu.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 47.Chou P-L, Rau K-M, Lin C-C. Development and psychometric testing of a short version of the Barriers Questionnaire-Taiwan form for cancer patients. Int J Nurs Stud. 2011;48(9):1071–1079. doi: 10.1016/j.ijnurstu.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 48.Passik SD, Kirsh KL, Donaghy K, et al. Patient-related barriers to fatigue communication: initial validation of the fatigue management barriers questionnaire. J Pain Symptom Manage. 2002;24(5):481–493. doi: 10.1016/s0885-3924(02)00518-3. [DOI] [PubMed] [Google Scholar]
- 49.Thompson JL, Davis SM, Gittelsohn J, et al. Patterns of physical activity among American Indian children: an assessment of barriers and support. J Community Health. 2001;26(6):423–445. doi: 10.1023/a:1012507323784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cigularov K, Chen PY, Thurber BW, Stallones L. What prevents adolescents from seeking help after a suicide education program? Suicide Life Threat Behav. 2008;38(1):74–86. doi: 10.1521/suli.2008.38.1.74. [DOI] [PubMed] [Google Scholar]
- 51.Cranney M, Barton S, Walley T. Addressing barriers to change: an RCT of practice-based education to improve the management of hypertension in the elderly. Br J Gen Pract. 1999;49(444):522–526. [PMC free article] [PubMed] [Google Scholar]
- 52.Letizia M, Creech S, Norton E, Shanahan M, Hedges L. Barriers to caregiver administration of pain medication in hospice care. J Pain Symptom Manage. 2004;27(2):114–124. doi: 10.1016/j.jpainsymman.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 53.Chan WK, Kong H, Wai K, Sum R, Lau KO. Barriers to the implementation of physical education (PE) assessment in Hong Kong. Int J Learn. 2006;13(4):165–170. [Google Scholar]
- 54.McKenna HP, Ashton S, Keeney S. Barriers to evidence-based practice in primary care. J Adv Nurs. 2004;45(2):178–189. doi: 10.1046/j.1365-2648.2003.02879.x. [DOI] [PubMed] [Google Scholar]
- 55.Chiu Ya-Wen, Weng Yi-Hao, Lo Heng-Lien, Hsu Chih-Cheng, Ya-Hui Shih KK. Comparison of evidence-based practice between physicians and nurses: a national survey of regional hospitals in Taiwan. J Contin Educ Health Prof. 2010;30(2):132–138. doi: 10.1002/chp.20070. [DOI] [PubMed] [Google Scholar]
- 56.Morinaga K, Ohtsubo Y, Yamauchi K, Shimada Y. Doctors’ traits perceived by Japanese nurses as communication barriers: a questionnaire survey. Int J Nurs Stud. 2008;45(5):740–749. doi: 10.1016/j.ijnurstu.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 57.Simm Alanna, Li Linda, Geddes Lynne, Brooks Diana, Alisson Hoens DR. Impact of a behavioral-based intervention on inspiratory muscle training prescription by a multidisciplinary team. J Contin Educ Health Prof. 2012;32(2):116–125. doi: 10.1002/chp.21134. [DOI] [PubMed] [Google Scholar]
- 58.Lee C, Ory MG, Yoon J, Forjuoh SN. Neighborhood walking among overweight and obese adults: age variations in barriers and motivators. J Community Health. 2013;38(1):12–22. doi: 10.1007/s10900-012-9592-6. [DOI] [PubMed] [Google Scholar]
- 59.Gunnarsdottir S, Donovan HS, Serlin RC, Voge C, Ward S. Patient-related barriers to pain management: the Barriers Questionnaire II (BQ-II) Pain. 2002;99(3):385–396. doi: 10.1016/S0304-3959(02)00243-9. [DOI] [PubMed] [Google Scholar]
- 60.Dobkin PL, de Civita M, Bernatsky S, Filipski M, Sita A, Baron M. Preliminary validity of the barriers to treatment adherence questionnaire in fibromyalgia: combining quantitative and focus group data. Psychol Rep. 2009;105(2):447–460. doi: 10.2466/PR0.105.2.447-460. [DOI] [PubMed] [Google Scholar]
- 61.Bearse JL, McMinn MR, Seegobin W, Free K. Barriers to psychologists seeking mental health care. Prof Psychol Res Pract. 2013;44(3):150–157. [Google Scholar]
- 62.Turconi G, Celsa M, Rezzani C, Biino G, Sartirana MA, Roggi C. Reliability of a dietary questionnaire on food habits, eating behaviour and nutritional knowledge of adolescents. Eur J Clin Nutr. 2003;57(6):753–763. doi: 10.1038/sj.ejcn.1601607. [DOI] [PubMed] [Google Scholar]
- 63.CCN Critical Care Nutrition: barriers questionnaire. 2013. [Accessed May 1, 2014]. Available from: http://www.criticalcarenutrition.com/index.php?option=com_content&view=article&id=171%3Ains-barriers-questionnaire&catid=16%3Anewsroom&Itemid=1.
- 64.McCluskey A, Lovarini M. Providing education on evidence-based practice improved knowledge but did not change behaviour: a before and after study. BMC Med Educ. 2005;5:40. doi: 10.1186/1472-6920-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gravel K, Légaré F, Graham I. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci. 2006;1:16. doi: 10.1186/1748-5908-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Salbach NM, Jaglal SB, Korner-bitensky N, Rappolt S, Davis D. Practitioner and organizational barriers to evidence-based practice of physical therapists for people with stroke. Phys Ther. 2007;87(10):1284–1303. doi: 10.2522/ptj.20070040. [DOI] [PubMed] [Google Scholar]
- 67.Stichler JF, Fields W, Kim SC, Brown CE. Faculty knowledge, attitudes, and perceived barriers to teaching evidence-based nursing. J Prof Nurs. 2011;27(2):92–100. doi: 10.1016/j.profnurs.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 68.Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(8 Suppl 2):II2–II45. [PubMed] [Google Scholar]
- 69.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Di Noia J, Prochaska JO. Dietary stages of change and decisional balance: a meta-analytic review. Am J Health Behav. 2010;34(5):618–632. doi: 10.5993/ajhb.34.5.11. [DOI] [PubMed] [Google Scholar]
- 71.Norcross JC, Krebs PM, Prochaska JO. Stages of change. J Clin Psychol. 2011;67(2):143–154. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- 72.Lam CS, Wiley AH, Siu A, Emmett J. Assessing readiness to work from a stages of change perspective: implications for return to work. Work. 2010;37(3):321–329. doi: 10.3233/WOR-2010-1085. [DOI] [PubMed] [Google Scholar]
- 73.Redding CA, Rossi JS, Rossi SR, Velicer WF, Prochaska JO. Health behavior models. Int Electron J Health Educ. 2000;3(Special Issue):180–193. [Google Scholar]
- 74.Steinmo SH, Michie S, Fuller C, Stanley S, Stapleton C, Stone SP. Bridging the gap between pragmatic intervention design and theory: using behavioural science tools to modify an existing quality improvement programme to implement “Sepsis Six”. Implement Sci. 2016;11:14. doi: 10.1186/s13012-016-0376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilkinson S, Thomas S, Phillips CJ, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc. 2015;8:139–146. doi: 10.2147/JMDH.S78458. [DOI] [PMC free article] [PubMed] [Google Scholar]