Abstract
OBJECTIVES
Insomnia is reported to be more prevalent in minority racial/ethnic groups. Little is known, however, about racial/ethnic differences in changes in insomnia severity over time, particularly among older adults. We examined racial/ethnic differences in trajectories of insomnia severity among middle-aged and older adults.
DESIGN
Data were drawn from five waves of the Health and Retirement Study (2002–2010), a nationally representative longitudinal biennial survey of adults aged >50.
SETTING
Population-based.
PARTICIPANTS
22,252 participants from non-Hispanic white, non-Hispanic black, Hispanic, and other racial/ethnic groups.
INTERVENTION
N/A
MEASUREMENTS
Participants reported the severity of four insomnia symptoms; summed scores ranged from 4 (no insomnia) to 12 (severe insomnia). We assessed change in insomnia across the five waves as a function of race/ethnicity.
RESULTS
Across all participants, insomnia severity scores increased 0.19 points (95% CI=0.14, 0.24; t=7.52; design df=56; p<0.001) over time after adjustment for gender, race/ethnicity, education, and baseline age. After adjusting for the number of accumulated health conditions and BMI, this trend decreased substantially and even changed direction (B=−0.24; 95% CI=−0.29, −0.19; t=−9.22; design df=56; p<0.001). The increasing trajectory was significantly more pronounced in Hispanics compared to non-Hispanic whites, even after adjustment for number of accumulated health conditions, BMI, and number of depressive symptoms.
CONCLUSIONS
Although insomnia severity increases with age—largely due to the accumulation of health conditions—this trend appears more pronounced among Hispanic older adults than in non-Hispanic whites. Further research is needed to determine the reasons for a different insomnia trajectory among Hispanics.
Keywords: disparities, aging, insomnia, chronic health conditions
OBJECTIVE
Health disparities are an area of important public health concern—numerous studies document racial/ethnic differences in the prevalence of chronic health conditions.1–4 These conditions, including heart disease and diabetes among others are prevalent in older adults, and the incidence of their development may differ among racial/ethnic groups as individuals age.5 With the projected growth of the older adult population over the next decade, there is concern that unaddressed disparities may become more pronounced as the population ages. It is important to identify modifiable risk factors that may contribute to these disparities.
Sleep disturbances are strongly associated with chronic health conditions, and there is increasing evidence that racial/ethnic disparities exist in disturbed sleep. Cross-sectional studies report racial/ethnic sleep disparities.6–8 Blacks have reported shorter sleep duration and lower subjective sleep quality than individuals from other racial groups.9,10 A cross-sectional study utilizing data from the National Health and Nutrition Examination Survey by Grandner et al. found non-Hispanic blacks had greater difficulty falling and staying asleep, whereas Hispanics were more likely to snore and gasp compared to non-Hispanic whites.11 It is possible that these racial/ethnic differences in sleep disturbances reflect or contribute to the other well-documented disparities in health, but more research is needed to understand how these two factors develop in different race/ethnicities as individuals age.
The vast majority of studies examining racial/ethnic differences in sleep disturbances are cross-sectional. Surprisingly few studies have examined trajectories of severity of insomnia symptoms as individuals age. There is broad empirical support for age-related changes in sleep. Studies using objective measures (e.g., wrist actigraphy) show declines in sleep quality (e.g., total sleep time and sleep efficiency) with age,12 and epidemiologic studies show age-related increases in self-report of specific sleep complaints (e.g., nighttime and early morning awakenings).13 Circadian rhythms can become dysregulated with age, fragmenting sleep12 and shortening sleep duration.14 Possible contributors include the development of physical health conditions.15 Because these conditions are often chronic, significant co-morbidity can develop as individuals age,16 and multiple risk factors for poor sleep can accumulate over time. Additionally, depressive symptoms are frequently associated with difficulty sleeping and may also impact these trajectories.17
We examined whether insomnia severity increases more rapidly among non-Hispanic blacks, Hispanics, and other racial/ethnic groups, compared to non-Hispanic whites, and whether physical health conditions and depressive symptomatology account for these differences in sleep trajectories. We hypothesized that, compared to non-Hispanic whites, other racial/ethnic groups would exhibit greater increases in insomnia severity, and that the accumulation of physical health conditions and depressive symptoms would explain these disparities with increasing age.
METHODS
Data Source
Data came from the 2002–2010 waves of the Health and Retirement Study (HRS), a nationally representative longitudinal cohort study examining financial, social, and healthcare experiences of older adults.18 The HRS is conducted biannually whereby approximately 20,000 participants are followed and are asked to give responses either through telephone or in-person interviews. Eligibility requirements include being a non-institutionalized adult aged >50 years, and having primary residence in the U.S. HRS oversamples blacks, Hispanics, and residents of Florida; weights account for oversampling. Details about HRS design are provided elsewhere.18 The HRS is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan. Our analyses were based on public-access data and were exempt from human subjects committee review.
Participants
Participants were eligible if they participated in ≥1 HRS wave from 2002–2010, were age >50 years, and had complete data on insomnia symptoms and race/ethnicity, yielding 22,252 individuals contributing 68,785 data points. Only 116 participants in our sample were asked about insomnia in 2008 and contributed data to the 2008 analyses. Excluding the 2008 data did not change results appreciably; therefore, we decided to include them in our analyses.
Participants in our sample were followed for an average of 5.57 years (SD=2.79). Of the 22,252 participants in our analyses, 11,107 (49.9%) did not contribute data to at least one of the five HRS waves in our analysis. A total of 4,854 (21.8%) did not contribute data to one wave, 2,291 (10.3%) to two, 2,043 (9.2%) to three, and 1,919 (8.6%) to four. Minority participants in our sample had higher probability of not contributing data compared to non-Hispanic whites (55.7% for minority race/ethnicities vs. 47.9% for non-Hispanic whites; χ2=105.85; df=1; p <0.001). To explore how this impacted our results, we limited main analyses to participants with complete data for at least the 2002 and 2010 waves. Those analyses, for the most part, returned the same pattern of results.
Measures
Insomnia severity
Participants were asked about insomnia symptoms at each wave. Specifically, participants were asked “how often do you have trouble falling asleep--would you say most of the time, sometimes, or rarely or never?” Participants were also asked about “trouble with waking up during the night,” trouble with “waking up too early and not being able to fall asleep again,” and how often they felt “really rested” in the morning. Responses ranged from 1 (“most of the time”) to 3 (“rarely or never”). We summed values from the four items after reverse-coding responses to the first three symptom questions to compute an insomnia score (4=no insomnia, 12=severe insomnia).
Race/ethnicity
Participants self-identified their race (i.e., white/Caucasian, black/African American, American Indian, Alaska Native, Asian, Native Hawaiian, Pacific Islander, other) and ethnicity (Hispanic [Mexican, other, type unknown], or non-Hispanic). We categorized participants as “non-Hispanic white,” “non-Hispanic black,” “Hispanic,” or “other.” If participants indicated they were Hispanic but lacked data on race, we categorized them as Hispanic. If participants did not provide data on race and either indicated they were non-Hispanic or did not provide data on ethnicity, they were excluded from our sample.
Health conditions
At each wave, participants indicated whether they had the following health conditions since last interview: “heart condition,” “stroke,” “memory disease,” “hypertension,” “pain,” “arthritis,” “cancer,” “diabetes” and “incontinence.” In 2010, “memory disease” was removed and replaced with two questions about “Alzheimer’s disease” and “dementia.” We recoded each of those conditions as memory disease. We calculated the number of health conditions each participant reported at each wave. To better capture participant health history, we coded any health conditions endorsed at prior waves as present in subsequent waves, regardless of whether endorsed at those latter waves. Thus, the variable for number of accumulated health conditions reflects the number of health conditions accumulated by each wave.
Other measures
Depressive symptomatology was measured by the 8-item Center for Epidemiologic Studies Depression Scale (CES-D).19 We calculated body mass index (BMI) based on self-reported height and weight at each wave (kg/m2).
Analyses
We first examined demographic and clinical characteristics of participants based on the first wave in which they participated between 2002–2010 and provided data on insomnia symptoms. We also assessed differences in characteristics by race/ethnicity using chi-squared tests weighted for the complex sampling design.
Next, we fit linear regression models with insomnia score as the outcome and time as the predictor, stratified by racial/ethnic groups. Time was calculated by subtracting each survey year by 2002 (the first wave in our study) (i.e., 2010 minus 2002), and dividing by 8. This time variable ranged in values from 0 (2002 wave) to 1 (2010 wave), enabling us to interpret the regression coefficient for time as the change in insomnia score across the entire study period (i.e., 2002–2010). Finally, we fit the same models in the entire sample, and introduced interaction terms for time as a function of racial/ethnic groups to test whether trajectories differed among groups (reference=non-Hispanic whites). Tests for regression coefficients (B) associated with these interaction terms indicated whether the insomnia score increased or decreased at a greater rate from 2002–2010 for each racial/ethnic group compared to non-Hispanic whites.
We fit four regression models. Model 1 adjusted for gender, education, and baseline age. In non-stratified analyses, we also controlled for race/ethnicity. Model 2 adjusted for demographics plus number of accumulated health conditions and BMI. Model 3 controlled for demographics and number of depressive symptoms (allowed to be time-varying). Model 4 adjusted for all covariates.
Because analysis of HRS data requires use of survey design and weighting variables to make results nationally representative, we were unable to use traditional mixed model procedures. Using these approaches do not allow us to account for the complex sampling design of the HRS and will result in artificially narrow standard errors. We therefore chose to use methods proposed by Horton et al.20 Each participant had a record for each wave at which they contributed data (i.e., an individual contributing data for 2004 and 2006 waves would have two records). By applying the HRS sampling design variables, we accounted for clustering of each record within individual participants, as well as the clustering, stratification, and weighting from the HRS complex sampling design. Analyses were conducted using Stata version 13 (StataCorp, College Station, TX).
RESULTS
Participant characteristics
Mean age at study entry was 63.96 years (SD=10.47) (Table 1). Half of respondents were women, and most completed high school. The most common health conditions reported at baseline were arthritis (51.8%) and hypertension (47.9%), and the mean CES-D score was 1.51 (SD=1.99). Mean BMI was 27.51 (SD=5.53). Racial/ethnic groups differed by age, gender, education, and baseline health conditions (except for pain and memory disease), CES-D score, and BMI (all p’s<0.02).
Table 1.
Demographic characteristics for HRS participants at study entry, 2002–2010.*
| Total Sample (n=22,252) |
Non Hispanic White (n=16,475) |
Non Hispanic Black (n=3,201) |
Hispanic (n=2,183) |
Other (n=393) |
Comparison of groups | |||
|---|---|---|---|---|---|---|---|---|
| F- statistic |
Design-based degrees of freedom+ |
p-value | ||||||
| Demographics | ||||||||
| Baseline age, Mean (SD) | 63.96 (10.47) | 64.39 (10.17) | 62.77 (12.10) | 61.82 (10.69) | 60.83 (8.51) | 14.70 | 3, 54 | <0.001 |
| Women | 12,806 (53.7) | 9,355 (53.3) | 1,975 (57.2) | 1,252 (53.7) | 224 (53.1) | 3.70 | 2.78, 155.77 | 0.015 |
| Education | 71.05 | 5.15, 288.65 | <0.001 | |||||
| <High school | 6,386 (23.7) | 3,535 (18.5) | 1,395 (39.7) | 1,337 (56.3) | 119 (27.2) | |||
| GED/High school diploma | 10,586 (48.4) | 8,511 (51.1) | 1,319 (42.4) | 623 (31.0) | 133 (36.3) | |||
| Some/completed college | 3,452 (18.2) | 2,870 (19.7) | 332 (12.7) | 154 (8.3) | 96 (25.1) | |||
| Graduate degree | 1,828 (9.7) | 1,559 (10.7) | 155 (5.1) | 69 (4.5) | 45 (11.4) | |||
| Health Conditions | ||||||||
| Heart condition | 5,138 (20.7) | 4,047 (21.5) | 672 (19.5) | 346 (15.0) | 73 (16.1) | 11.92 | 2.37, 132.96 | <0.001 |
| Stroke | 1,574 (5.9) | 1,126 (5.7) | 304 (8.9) | 119 (4.8) | 25 (4.2) | 12.40 | 2.79, 156.09 | <0.001 |
| Hypertension | 11,435 (47.9) | 8,012 (46.1) | 2,133 (64.2) | 1,101 (46.6) | 189 (46.1) | 56.86 | 2.92, 163.68 | <0.001 |
| Pain | 6,849 (30.7) | 5,031 (30.5) | 929 (29.9) | 770 (33.9) | 119 (32.2) | 2.05 | 2.78, 155.44 | 0.114 |
| Arthritis | 12,439 (51.8) | 9,311 (52.2) | 1,880 (54.9) | 1,082 (46.3) | 166 (40.1) | 9.45 | 2.92, 163.52 | <0.001 |
| Cancer | 2,745 (11.2) | 2,234 (12.0) | 305 (9.0) | 173 (6.9) | 33 (5.7) | 20.64 | 2.86, 160.22 | <0.001 |
| Diabetes | 3,807 (15.3) | 2,366 (13.5) | 839 (24.9) | 533 (22.4) | 69 (16.4) | 64.67 | 2.72, 152.48 | <0.001 |
| Incontinence | 4,116 (16.7) | 3,284 (17.7) | 490 (13.6) | 292 (12.2) | 50 (9.6) | 22.37 | 2.74, 153.41 | <0.001 |
| Memory disease | 562 (1.8) | 386 (1.7) | 96 (2.0) | 65 (2.3) | 15 (2.7) | 2.29 | 2.80, 156.61 | 0.085 |
| CES-D§score, Mean (SD) | 1.51 (1.99) | 1.39 (1.83) | 2.00 (2.65) | 2.15 (2.65) | 1.77 (1.96) | 37.85 | 3, 54 | <0.001 |
| BMI, Mean (SD) | 27.51 (5.53) | 27.26 (5.18) | 29.21 (7.80) | 28.24 (5.97) | 26.88 (5.07) | 68.15 | 3, 54 | <0.001 |
Note: All percentages and means are weighted to account for unequal probability of selection into study. Bolded p-values are statistically significant, and account for the complex sampling design of HRS.
Data are presented as number (percentage) unless otherwise specified.
The degrees of freedom for analyses involving categorical variables are fractional due to adjustment for clustering and stratification in design-based analyses.
Center for Epidemiologic Studies Depression Scale
Racial/ethnic disparities in insomnia severity trajectories
Across all participants, the mean insomnia score increased modestly by 0.19 points (95% CI=0.14, 0.24; t=7.52; design df=56; p<0.001) between 2002 and 2010 after controlling for baseline age, race/ethnicity, gender, and education (Model 1). In stratified analyses, we also found statistically significant increases for non-Hispanic whites, non-Hispanic blacks, and Hispanics, whereas a statistically significant increase was not observed for other race (Table 2, Model 1). Among the racial/ethnic groups, there was a statistically significant interaction effect of time and the dummy variable for Hispanic vs. non-Hispanic white ethnicity (interaction B=0.39; 95% CI= 0.19, 0.60; t=3.82; design df=56; p<0.001), indicating that Hispanics experienced a greater increase in insomnia severity over time compared to non-Hispanic whites. In sum, we found a statistically significant increase in insomnia severity over time which was disproportionately more pronounced among Hispanics compared to non-Hispanic whites.
Table 2.
Trajectories of insomnia severity stratified by racial/ethnic groups, HRS, 2002–2010.
| Model 1 Adjusted for baseline age, gender, and education |
Model 2 Adjusted for Model 1 + number of accumulated health conditions* and BMI |
Model 3 Adjusted for Model 1 + CES-D− Score |
Model 4 Adjusted for variables in all models |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | t | p-value | B | 95% CI | t | p-value | B | 95% CI | t | p-value | B | 95% CI | t | p-value | |
| Full Score§ | ||||||||||||||||
| Non-Hispanic White | 0.16 | 0.11, 0.22 | 5.76 | <0.001 | −0.25 | −0.31, −0.19 | −8.36 | <0.001 | 0.22 | 0.17, 0.26 | 8.79 | <0.001 | −0.03 | −0.09, 0.02 | −1.29 | 0.204 |
| Non-Hispanic Black | 0.23 | 0.10, 0.35 | 3.63 | 0.001 | −0.22 | −0.34, −0.11 | −3.95 | <0.001 | 0.31 | 0.21, 0.40 | 6.44 | <0.001 | 0.05 | −0.06, 0.15 | 0.93 | 0.358 |
| Hispanic | 0.51║ | 0.31, 0.71 | 5.04 | <0.001 | −0.09║ | −0.31, 0.14 | −0.76 | 0.450 | 0.52║ | 0.30, 0.74 | 4.77 | <0.001 | 0.15║ | −0.09, 0.39 | 1.26 | 0.214 |
| Other | 0.23 | −0.06, 0.52 | 1.62 | 0.112 | −0.28 | −0.59, 0.03 | −1.83 | 0.073 | 0.34 | 0.13, 0.55 | 3.31 | 0.002 | 0.03 | −0.20, 0.26 | 0.24 | 0.814 |
Note: All beta coefficients account for the complex sampling procedures of the HRS, and are weighted to make results nationally representative. The design-based degrees of freedom ranged from 50–56. Bolded p-values are statistically significant.
Corresponds to the sum of health conditions for each participant at each wave. Health conditions include: heart condition, stroke, high blood pressure, pain, arthritis, cancer, diabetes, incontinence, and memory problem.
Center for Epidemiologic Studies Depression Scale
All results correspond to beta coefficients of the change in insomnia score across the years within each racial/ethnic group from linear regressions.
Statistically significant (p<0.05) difference in trajectories of the insomnia score or specific sleep problem compared to non-Hispanic whites
Mediation by physical health conditions and depressive symptomatology
Across all participants, after adjusting for multiple accumulated health conditions and BMI, the association between insomnia severity and time decreased substantially and changed direction (B=−0.24; 95% CI=−0.29, −0.19; t=−9.22; design df=56; p<0.001) (Model 2), suggesting that the observed worsening in insomnia severity was attributable to the accumulation of health conditions. A significant positive association existed after adjusting only for demographic characteristics and depressive symptoms (B=0.24; 95% CI=0.20, 0.29; t=11.42; design df=56; p<0.001) (Model 3). There was no statistically significant association after adjustment for all variables (Model 4).
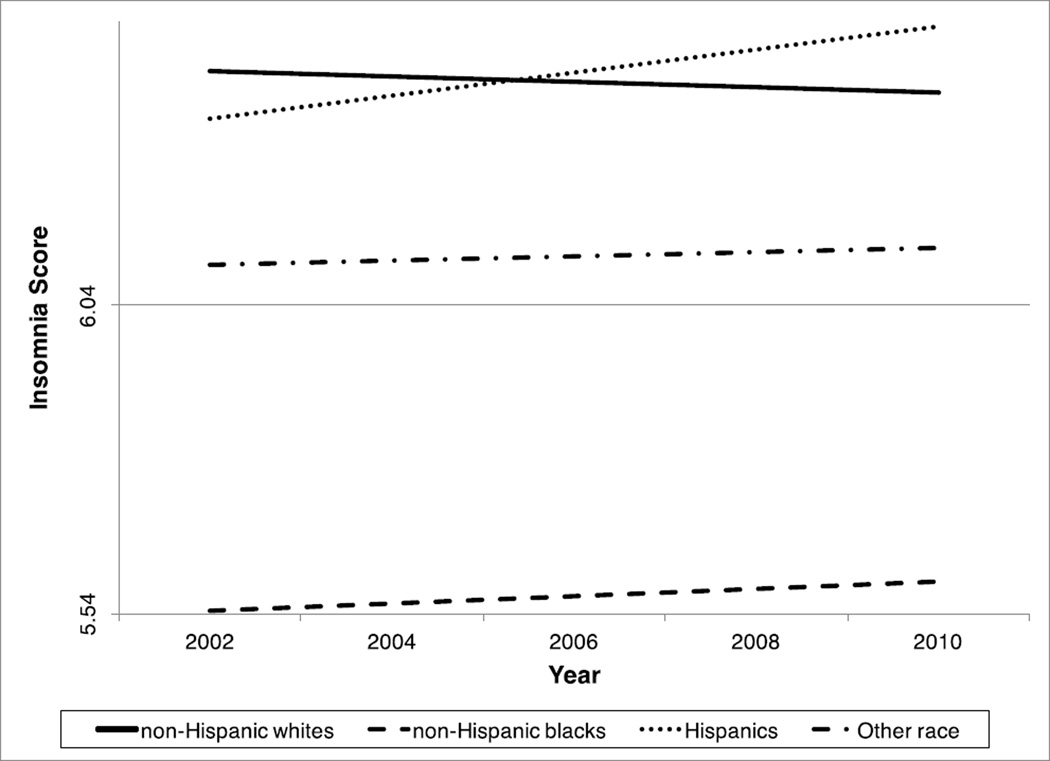
Within individual race/ethnicities, after adjusting for accumulated health conditions and BMI, the regression coefficient for non-Hispanic whites, blacks, and the other racial group again decreased substantially and changed direction. The coefficients were significant for non-Hispanic whites and blacks, and the coefficient for other racial group became marginally significant (Model 2, Table 2). The regression coefficient for Hispanics declined, but became non-significant. Associations in Model 3 were similar to Model 1 except that the regression coefficient for the other racial group became significant, indicating that increases in insomnia scores within each racial/ethnic group were independent of changes in depressive symptomatology. After controlling for all variables (Model 4), the regression coefficients all became non-significant (see Figure 1). In all models, there remained a statistically significant interaction between time and the dummy variable for Hispanic vs. non-Hispanic whites (interaction B=0.29; 95% CI=0.09, 0.48; t=2.88; design df=56; p=0.006 for Model 2; interaction B=0.33; 95% CI=0.09, 0.57; t=2.79; design df=56; p=0.007 for Model 3; and interaction B=0.25; 95% CI=0.02, 0.49; t=2.15; design df=56; p=0.036 for Model 4), indicating that Hispanics still saw significantly greater increases in insomnia severity even after controlling for all variables.
Figure 1.
Trajectories of insomnia severity from 2002–2010 adjusted for variables in Model 4.
Note: Insomnia Score ranges from values of 4 to 12. Trajectories are adjusted for age at baseline, gender, education, number of accumulated health conditions, BMI, and CES-D score.
Overall, these analyses indicate that increases in insomnia severity over time may be due to the accumulation of health conditions and BMI. However, even after taking these variables into account, Hispanics continued to have a disproportionately greater increase in insomnia severity than non-Hispanic whites.
Further analyses
We repeated analyses stratifying by 0, 1, 2, and 3+ accumulated health conditions to investigate why the insomnia score decreased over time after adjustment for accumulated health conditions. We re-estimated Model 1, but restricted analyses to individuals with the same number of accumulated health conditions (i.e., only 0, 1, 2, or 3+). When stratified by the number of health conditions in the full sample, the insomnia score showed no statistically significant change in the first stratum (0 health conditions), whereas it showed a declining trend within the 1, 2, and 3+ health conditions strata (although not as strongly as in the unstratified Model 2) (Table 3). By race/ethnicity group, Hispanics showed a statistically significant increase in the insomnia score for the “no health conditions” stratum, but no statistically significant change in insomnia for the other three strata. Among non-Hispanic whites, no statistically significant change in the insomnia score was observed for the no health conditions stratum, but a statistically significant declining trend in insomnia severity was observed for the other three strata. These findings suggest that accumulation of health conditions may disproportionately affect the sleep of Hispanics compared to non-Hispanics (particularly non-Hispanic whites).
Table 3.
Trajectories of insomnia severity across racial/ethnic groups stratified by number of health conditions from 2002 to 2010, Health and Retirement Study.
| Model 1 restricted to those with no health conditions* Adjusted for baseline age, gender, race and education |
Model 1 restricted to those with 1 condition* Adjusted for baseline age, gender, race and education |
Model 1 restricted to those with 2 conditions* Adjusted for baseline age, gender, race and education |
Model 1 restricted to those with 3+ conditions* Adjusted for baseline age, gender, race and education |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | t | p-value | B | 95% CI | t | p-value | B | 95% CI | t | p-value | B | 95% CI | t | p-value | |
| Full Score− | ||||||||||||||||
| All Races | −0.07 | −0.23, 0.10 | −0.82 | 0.413 | −0.16 | −0.26, −0.06 | −3.09 | 0.003 | −0.14 | −0.23, −0.05 | −2.99 | 0.004 | −0.15 | −0.22, −0.08 | −4.21 | <0.001 |
| Racial/ethnic Groups§ | ||||||||||||||||
| Non-Hispanic White | −0.13 | −0.30, 0.04 | −1.50 | 0.140 | −0.16 | −0.28, −0.04 | −2.68 | 0.010 | −0.18 | −0.28, −0.07 | −3.30 | 0.002 | −0.17 | −0.25, −0.09 | −4.17 | <0.001 |
| Non-Hispanic Black | 0.25 | −0.18, 0.67 | 1.17 | 0.249 | −0.25 | −0.53, 0.03 | −1.77 | 0.082 | −0.16 | −0.44, 0.13 | −1.10 | 0.275 | −0.09 | −0.28, 0.09 | −1.05 | 0.299 |
| Hispanic | 0.56 | 0.09, 1.02 | 2.43 | 0.020 | −0.20 | −0.60, 0.21 | −0.96 | 0.341 | 0.30 | −0.13, 0.73 | 1.42 | 0.162 | −0.01 | −0.29, 0.27 | −0.08 | 0.934 |
| Other | −0.28 | −0.98, 0.41 | −0.82 | 0.415 | 0.13 | −1.03, 1.29 | 0.23 | 0.820 | −0.09 | −0.79, 0.60 | −0.28 | 0.783 | −0.33 | −0.85, 0.20 | −1.26 | 0.215 |
Note: All beta coefficients account for the complex sampling procedures of the HRS, and are weighted to make results nationally representative. The design-based degrees of freedom ranged from 33–56. Bolded p-values are statistically significant.
Corresponds to the sum of health conditions for each participant at each wave. Health conditions include: heart condition, stroke, high blood pressure, pain, arthritis, cancer, diabetes, incontinence, and memory problem.
All results correspond to beta coefficient estimates of the change in the insomnia score across the years within each racial/ethnic group from linear regressions.
Estimates for analyses stratified by race/ethnic groups do not adjust for race/ethnicity.
Furthermore, we assessed whether results concerning the accumulation of health conditions would have changed if we accounted for the presence or absence of specific health conditions at each wave rather than the accumulation of health conditions. We repeated analyses for Model 2, but instead of controlling for the accumulation of health conditions, we entered into the model variables for each health condition at each wave. For the overall sample, the coefficient for time was not statistically significant (B=−0.01; 95% CI=−0.06, 0.04; t=−0.33; design df=56; p=0.745). In the context of findings from our main analyses showing a substantial drop and change in direction of the beta coefficients when adjusting for accumulating health conditions, these sensitivity analyses suggest that accumulation of health conditions and their interactions may be a significant contributor to worsening insomnia as individuals age.
In the Hispanic group, we also investigated whether the trends observed differed by immigration status, national origin, or access to health coverage. None of these analyses yielded statistically significant differences in observed trajectories.
CONCLUSIONS
We investigated whether racial/ethnic disparities in age-related changes in insomnia severity exist among middle-aged and older adults, and whether differences in physical health conditions and depression can explain these disparities. We found reports of insomnia severity increased with age across all racial/ethnic groups, but Hispanics exhibited greater increases in insomnia severity compared to non-Hispanic whites. After adjusting for accumulated health conditions, insomnia severity substantially declined and reversed directions, except among Hispanics who saw no change. This suggests increases in insomnia severity among non-Hispanics may be due to accumulation of chronic health conditions with age, while Hispanics may see increases even after adjusting for these conditions.
This study extends prior research in several ways. First, while prior studies have focused on sleep disparities between blacks and whites,7–9 we included Hispanics. We found Hispanics reported lower sleep quality than non-Hispanics. It is possible this is due to snoring and gasping during the night, which was found to be more prevalent in Hispanics compared to non-Hispanics in the Grandner et al. study.11 The mechanism for the disproportionate increase in insomnia severity in Hispanics remains unclear. While we found worsening insomnia among Hispanics did not differ by immigration status, national origin, or health coverage, it is possible different acculturation levels played a role in the worsening of insomnia severity. Future studies can assess sleep disturbances in Hispanics who live near a greater number of family members, who feel more welcomed in the U.S., and who have greater involvement in their local community/neighborhoods. Studies on acculturation among Hispanics using validated measures are needed. Given that Hispanics were younger at baseline relative to other racial/ethnic groups, future studies need to examine other factors related to the impact of workforce participation on associations observed in this study.
Second, we examined trajectories of racial/ethnic disparities in insomnia severity. Most research on sleep disparities has been cross sectional. While several studies have examined the natural history of insomnia in various populations,21 little prior work has focused on racial/ethnic disparities in insomnia longitudinally.
Finally, we examined how the accumulation of health conditions might drive trajectories of insomnia severity among middle-aged and older adults, and racial/ethnic disparities in these trajectories. Our analyses suggest accumulated health conditions may disproportionately impact trajectories of insomnia severity among Hispanics compared to non-Hispanics.
Although we found health conditions are associated with insomnia symptoms, the direction of causality remains unclear. It is likely that the association is reciprocal, such that health conditions contribute to insomnia and insomnia is in turn a risk factor for future health conditions. While insomnia may exacerbate health conditions, it may also simply be a marker of these conditions. If insomnia does in fact exacerbate health conditions, it will be important to prevent or treat insomnia to minimize the severity of these conditions.
Contrary to past findings showing a greater prevalence of insomnia symptoms in non-Hispanic blacks compared to whites,7–9 we did not observe disparities in insomnia scores over time in these groups. One explanation is that while a greater proportion of non-Hispanic blacks have insomnia symptoms than whites, the trajectories of those symptoms may be similar across these groups.
Given the large body of literature showing an association between depression and insomnia,21 it is surprising that adjusting for depression did not alter the trajectory of insomnia severity. This may be because we controlled for number of depressive symptoms, not for the diagnosis of major depression. More research should examine how fluctuations in depressive symptoms influence insomnia trajectories and the differences across racial/ethnic groups with regard to these trajectories.
We used data on middle-aged and older adults; therefore, we can only generalize findings to individuals in the later life course. Insomnia severity trajectories may differ in younger age groups. Studies show that sleep patterns change from early childhood through adolescence,22 perhaps due to hormonal changes during puberty.23 Further research on how sleep patterns change over the entire life course may inform future efforts to improve sleep quality in later life.
As the U.S. Hispanic population grows,24 it will be important to address preventable health disparities experienced by this ethnic group. Hispanics are less likely to use health services than non-Hispanics,25 and consequently their sleep conditions may be untreated. Improvements in access to care and screening for sleep problems may minimize the burden of insomnia in this population, and in turn, control healthcare costs. Future studies should examine the influence of access to sleep treatments on health outcomes among Hispanics in greater detail.
This study has limitations. First, sleep disturbances and health conditions were self-reported. There is some evidence regarding racial/ethnic differences in self-reports of somatic and psychiatric symptoms.26 Second, participants were not asked about the diagnosis of sleep apnea, which has a higher prevalence in minority populations.27 While we adjusted for BMI, a proxy for sleep apnea, this was based on self-reported weight and not all individuals with apnea are obese. Also, the HRS did not inquire about aspects of sleep difficulties beyond the insomnia symptoms (e.g., next day drowsiness or napping during the day)—further investigation of these factors is warranted. Third, although sleep duration is likely to be correlated with insomnia measures, it was not assessed by the HRS and could be considered a potential confounder. Fourth, the insomnia symptom measures in this study were not derived from established insomnia instruments; future studies should replicate our findings using well known measures such as the Insomnia Severity Index.28 Because the HRS did not obtain diagnoses of clinical levels of insomnia, our findings concerning insomnia symptom trajectories will not necessarily extend to differences in the course of diagnosed insomnia. Fifth, some participants did not participate in all waves, possibly resulting in selection bias. The proportion with complete data differed across racial ethnic groups (with minority participants more likely to have missing data). However, Hispanics still showed a greater increase in insomnia severity compared to other groups when we limited analyses to those who, at a minimum, had complete data available for 2002 and 2010. Finally, we assumed health conditions were chronic and persisted after first report. However, in sensitivity analyses where we relaxed the assumption of chronicity of health conditions, we found that controlling for transitory comorbidity still yielded attenuated and reversed beta coefficients for time.
Overall, we found that the development of insomnia symptoms with increasing age may have different trajectories across racial/ethnic groups. Our findings highlight the importance of detecting and screening for sleep problems among minority racial/ethnic groups—particularly in Hispanics—in mid- and later-life. If corroborated, our findings also underscore the need to better understand the reasons for racial/ethnic differences in insomnia trajectories and to determine the effect that treating insomnia will have on health outcomes and quality of life.
Acknowledgments
Sources of Funding: This work was supported by the National Institutes of Health. Drs. Kaufmann and Spira were supported by the National Institute on Aging (CNK: F31AG044052, APS: K01AG033195). Dr. Kaufmann currently receives funding from the National Institute of Mental Health (T32MH019934). Drs. Hock and Chen-Edinboro were supported by the National Institute of Mental Health (RSH: T32MH093310, LC-E: T32MH014592). Dr. Thorpe was supported by the National Institute on Minority Health and Health Disparities (P60MD000214). Dr. Canham was supported by the National Institute on Drug Abuse (T32DA007292).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Previous Presentation: This study was presented at the 27th Annual Meeting of the Associated Professional Sleep Societies in Baltimore, Maryland, June 3rd, 2013.
Conflicts of Interest: All authors report no conflicts of interest.
References
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 3.McBean AM, Li S, Gilbertson DT, Collins AJ. Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: whites, blacks, hispanics, and asians. Diabetes Care. 2004;27(10):2317–2324. doi: 10.2337/diacare.27.10.2317. [DOI] [PubMed] [Google Scholar]
- 4.Manseau M, Case BG. Racial-Ethnic Disparities in Outpatient Mental Health Visits to U.S. Physicians, 1993–2008. Psychiatr Serv. 2013;65(1):59–67. doi: 10.1176/appi.ps.201200528. [DOI] [PubMed] [Google Scholar]
- 5.Taylor MG. Timing, Accumulation, and the Black/White Disability Gap in Later Life A Test of Weathering. Research on Aging. 2008 [Google Scholar]
- 6.Gamaldo AA, McNeely JM, Shah MT, Evans MK, Zonderman AB. Racial Differences in Self-Reports of Short Sleep Duration in an Urban-Dwelling Environment. J Gerontol B Psychol Sci Soc Sci. 2013 Nov; doi: 10.1093/geronb/gbt117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008;70(4):410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. doi: 10.5665/sleep.3508. doi:10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grandner MA, Petrov MER, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. doi: 10.5664/jcsm.2990. 905A–905D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y-L, Liu R-Y, Wang Q-S, Van Someren EJW, Xu H, Zhou J-N. Age-associated difference in circadian sleep-wake and rest-activity rhythms. Physiol Behav. 2002;76(4–5):597–603. doi: 10.1016/s0031-9384(02)00733-3. [DOI] [PubMed] [Google Scholar]
- 13.Soldatos CR, Allaert FA, Ohta T, Dikeos DG. How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med. 2005;6(1):5–13. doi: 10.1016/j.sleep.2004.10.006. doi:10.1016/j.sleep.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Morris M, Lack L, Barrett J. The effect of sleep/wake state on nocturnal melatonin excretion. J Pineal Res. 1990;9(2):133–138. doi: 10.1111/j.1600-079x.1990.tb00701.x. [DOI] [PubMed] [Google Scholar]
- 15.Costa e Silva JA. Sleep disorders in psychiatry. Metab Clin Exp. 2006;55(10 Suppl 2):S40–S44. doi: 10.1016/j.metabol.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Yancik R, Ershler W, Satariano W, Hazzard W, Cohen HJ, Ferrucci L. Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci. 2007;62(3):275–280. doi: 10.1093/gerona/62.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buysse DJ. Insomnia depression aging Assessing sleep and mood interactions in older adults. Geriatrics. 2004;59(2) 47–51-quiz52. [PubMed] [Google Scholar]
- 18.Hauser R. Survey design and methodology in the Health and Retirement Study and the Wisconsin Longitudinal Study. Population and Development Review. 2004 [Google Scholar]
- 19.Steffick D, editor. [Accessed June 14, 2012];Documentation of Affective Functioning Measures in the Health and Retirement Study. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf.
- 20.Horton NJ, Fitzmaurice GM. Regression analysis of multiple source and multiple informant data from complex survey samples. Stat Med. 2004;23(18):2911–2933. doi: 10.1002/sim.1879. [DOI] [PubMed] [Google Scholar]
- 21.Suh S, Yang H-C, Fairholme CP, Kim H, Manber R, Shin C. Who is at risk for having persistent insomnia symptoms? A longitudinal study in the general population in Korea. Sleep Med. 2014;15(2):180–186. doi: 10.1016/j.sleep.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 22.Laberge L, Petit D, Simard C, Vitaro F, Tremblay RE, Montplaisir J. Development of sleep patterns in early adolescence. J Sleep Res. 2001;10(1):59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 23.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 24.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. U.S. Department of Commerce; 2011. pp. 1–16. [Google Scholar]
- 25.Barrio C, Palinkas LA, Yamada A-M, et al. Unmet needs for mental health services for latino older adults: perspectives from consumers, family members, advocates, and service providers. Community Ment Health J. 2008;44(1):57–74. doi: 10.1007/s10597-007-9112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341(18):1329–1335. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 27.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]