Abstract
Statins are competitive inhibitors of HMG-CoA reductase, the rate-limiting enzyme of cholesterol synthesis. Statins reduce plasma cholesterol levels, but whether this is actually caused by inhibition of de novo cholesterol synthesis has not been clearly established. Using three different statins, we investigated the effects on cholesterol metabolism in mice in detail. Surprisingly, direct measurement of whole body cholesterol synthesis revealed that cholesterol synthesis was robustly increased in statin-treated mice. Measurement of organ-specific cholesterol synthesis demonstrated that the liver is predominantly responsible for the increase in cholesterol synthesis. Excess synthesized cholesterol did not accumulate in the plasma, as plasma cholesterol decreased. However, statin treatment led to an increase in cholesterol removal via the feces. Interestingly, enhanced cholesterol excretion in response to rosuvastatin and lovastatin treatment was mainly mediated via biliary cholesterol secretion, whereas atorvastatin mainly stimulated cholesterol removal via the transintestinal cholesterol excretion pathway. Moreover, we show that plasma cholesterol precursor levels do not reflect cholesterol synthesis rates during statin treatment in mice. In conclusion, cholesterol synthesis is paradoxically increased upon statin treatment in mice. However, statins potently stimulate the excretion of cholesterol from the body, which sheds new light on possible mechanisms underlying the cholesterol-lowering effects of statins.
Keywords: cholesterol/absorption, cholesterol/biosynthesis, liver, intestine, biliary cholesterol, transintestinal cholesterol excretion
Statins represent the most commonly used class of drugs to treat and prevent cardiovascular diseases worldwide and supposedly work by decreasing cholesterol synthesis (1–3). In vitro statins act indeed as competitive inhibitors of HMG-CoA reductase (HMGCR), the rate-limiting enzyme of cholesterol synthesis. When statins are bound to HMGCR, they block the access of the natural substrate HMG-CoA to the catalytic site and thereby interfere with cholesterol synthesis (4). As a result, the cholesterol content in the membrane of the endoplasmic reticulum decreases, causing activation of the SREBF chaperone (SCAP), which then transports sterol regulatory element-binding protein 2 (SREBP2) to the Golgi apparatus (5, 6). In the Golgi apparatus, SREBP2 is activated via several cleavages and translocates to the nucleus (7). In the nucleus, the active SREBP2 can bind to the sterol regulatory element (SRE-1) of, among others, the LDL receptor (LDLR) promoter and thereby induce expression of the LDLR (8–10). An increased number of LDLRs on the cell membrane leads to decreased plasma LDL cholesterol levels explaining partly how LDL lowering is achieved upon statin treatment. This scenario seems a plausible sequel to reduced cholesterol synthesis; however, there is surprisingly scarce in vivo data available confirming that statins actually do reduce cholesterol synthesis rates. Cholesterol synthesis in vivo is mainly estimated via surrogate biomarkers (e.g., intermediates of cholesterol synthesis). The concentration of mevalonic acid, squalene, cholestenol, lathosterol, and desmosterol has indeed been shown to decrease in statin-treated patients (11, 12). More direct measurements of cholesterol synthesis yielded controversial results. Sterol balance measurements in humans treated with pravastatin showed slight decreases in cholesterol synthesis (13–15). In contrast, Goldberg et al. (16) found that cholesterol synthesis rates were unaltered in lovastatin-treated patients. Kallien et al. (17) measured cholesterol synthesis in human subjects treated with pravastatin or placebo in a direct way using 13C-acetate, which is incorporated into the cholesterol molecule during cholesterol synthesis. They reported that cholesterol synthesis was even increased in pravastatin-treated individuals compared with controls. Furthermore, increased hepatic Hmgcr mRNA and enzyme activity levels have been observed in biopsies of humans and in various animal models treated with statins (18–24). Combined, these data challenge the current dogma that decreased cholesterol synthesis underlies the reduction of plasma cholesterol levels achieved by statin treatment. To address this challenge, we assessed the effects of statin treatment in detail using a mouse model. In order to study the effects of statins on cholesterol metabolism in detail, we selected three different statins based on differences in their pharmacokinetic properties. Rosuvastatin is a hydrophilic statin that makes it more hepatoselective compared with atorvastatin and lovastatin, which are lipophilic (25). Atorvastatin and rosuvastatin have a longer half-life compared with lovastatin, and next to that, lovastatin is a prodrug (i.e., it needs to be activated in the enterohepatic circulation to become active) (25, 26). In our study, statin treatment led to a slight decrease in plasma cholesterol levels. Paradoxically, cholesterol synthesis rates were robustly increased upon statin treatment in sharp contrast with what would be expected upon HMGCR inhibition.
MATERIALS AND METHODS
Animals and treatments
Male C57BL/6J mice were purchased from Charles River (L’Arbressie Cedex, France) and housed under standard conditions with ad libitum access to food and water, under a 12 h light/12 h dark cycle in a temperature-controlled environment. Mice were fed a standard rodent chow diet (RMH-B; AB-Diets, Woerden, The Netherlands), containing 0.023% cholesterol, with or without the supplementation of 0.01% rosuvastatin (Crestor; AstraZeneca, Zoetermeer, The Netherlands), 0.05% atorvastatin (Lipitor; Pfizer, Freiburg, Germany), or 0.2% lovastatin (1 A Pharma, Oberhaching, Germany) for 2 weeks (n = 7 per group). These doses were chosen based on previous publications for use in mice without any toxic side effects (27–30). The institutional ethical committee for animal experiments of the University of Groningen approved all experimental procedures.
Experimental procedures
After 5 days of statin treatment, mice were injected intravenously with D5-cholesterol and orally gavaged with D7-cholesterol; blood spots were taken from the tail vein at 0, 3, 6, 12, 24, 48, 72, 92, 120, 144, 168, and 192 h after administration of the stably labeled isotopes, to measure the absorption of cholesterol (31). To assess cholesterol synthesis, 2% 13C-acetate was added to the drinking water ad libitum from day 12 on for 72 h. The 13C-acetate addition started at 9 AM, and bloodspots were taken at time points 0, 24, 31, 48, 55, and 72 h. Feces were collected during 24 h prior to termination. At the end of the experiment, bile cannulations were performed, and bile was collected continuously for 30 min as described by Brufau and Groen (31). Mice were terminated under anesthesia by cardiac puncture, and consecutively, the liver and the small intestine were excised. After excision, the liver was weighed and snap frozen in liquid N2. After the small intestine was excised, it was flushed with PBS containing protease inhibitors (Complete, Roche Diagnostics) and frozen in liquid N2. In a separate experiment, cholesterol synthesis was measured specifically in liver and small intestine, by injecting mice with 99% deuterium oxide (23.3 mg/g; ip) after 2 weeks of statin treatment. Mice were terminated by cardiac puncture 60 min after injection; liver and small intestine were excised as described above. Organ-specific cholesterol synthesis in deuterium water-injected mice was analyzed with the use of the method described by Previs et al. (32). The number of incorporated hydrogen atoms per newly synthesized cholesterol molecule (n) was calculated as described (32) based on M+1 and M+2 isotopomer ratios as measured by GC/MS. It was found that 23 hydrogen atoms per newly synthesized cholesterol molecule were derived from water or water-exchangeable sources, which is in accordance with results obtained by others (32). Following lipid extraction from tissues, cholesteryl esters were hydrolyzed, and cholesterol was subsequently derivatized to cholesteryl acetate. Samples were then analyzed by isotope ratio mass spectroscopy (IRMS) (Delta V Advantage IRMS, Thermo Scientific) to measure the abundance of deuterated hydrogen atoms in the cholesterol molecules, and synthesis rates were calculated as described (32).
Analysis of cholesterol fluxes
After extraction of fecal neutral sterols and biliary cholesterol, the determination of the concentrations was carried out by GC (HP 6890 series, Hewlett Packard) and GC/MS (5975C inert XL EI/CI MSD and 7890A GC system, Agilent Technologies) as described previously (31, 33). Fractional absorption and transintestinal cholesterol excretion (TICE) were calculated according to previously published protocols (31, 33). Fecal bile salts were measured from the acid sterol fraction of the feces after extraction of neutral sterols, by GC as detailed elsewhere (34).
Mass isotopomer distribution analysis of cholesterol synthesis using the 13C-acetate method
Fractional cholesterol synthesis was determined by mass isotopomer distribution analysis (MIDA) using 13C-acetate (Isotec, Miamisburg, OH) as labeled precursor according to the method originally published by Neese et al. (35). The incorporation of 13C into newly synthesized cholesterol molecules was quantified by GC/MS (5975C inert XL EI/CI MSD and 7890A GC system, Agilent Technologies). Using these data, cholesterol synthesis was calculated as detailed elsewhere (33). Briefly, cholesterol was extracted from blood spots, taken at the time points indicated above, using 1 ml 95% ethanol-acetone (1:1, v/v) and trimethylsilylated using N,O-bis-(trimethyl)trifluoroacetamide (BSTFA) with 1% trimethylchlorosilane (TMCS) overnight at room temperature. Cholesterol label enrichment was determined by capillary GC on an Agilent gas chromatograph (7890A; Amstelveen, The Netherlands) connected to an Agilent mass spectrometer (5975C). Isotope ratios were determined in the selected ion monitoring mode on m/z 458 (M+0) to 465 (M+7) and corrected for the fractional distribution due to natural abundance of 13C by multiple linear regression as described by Lee et al. (36) to obtain excess fractional distribution of mass isotopomers. M+1 and M+3 were used in MIDA calculations to determine the fraction of newly synthesized cholesterol. Precursor pool enrichment was estimated from the ratios of M+1 and M+3 based on theoretical multinomial curves. Next, from a curve in which M+1 and M+3 are plotted against precursor pool enrichment, mass-isotopomer distributions of the newly synthesized cholesterol can be estimated (M+1new and M+3new). The ratio of the measured fractional distribution of cholesterol and the estimated fractional distribution in the newly synthesized cholesterol gives the fractional contribution of newly synthesized in the cholesterol pool (fnew).
Plasma and hepatic lipid analysis
Plasma cholesterol was measured using an enzymatic kit (DiaSys Diagnostic Systems, Holzheim, Germany), and the same assay was used to measure hepatic cholesterol after extraction of cholesterol from liver homogenates according to the method of Bligh and Dyer (37). Separation of the lipoproteins was performed with fast-protein liquid chromatography (FPLC) using a Superose 6 10/300 GL column (GE Healthcare, Uppsala, Sweden) as described (38). Triglycerides in the lipoprotein fractions were measured using a commercially available kit (Roche Diagnostics, Mannheim, Germany).
Targeted quantitative proteomics
Targeted proteomics was used to quantify HMGCR in homogenized liver tissue via the isotopically labeled peptide standard FLSDAEIIQLVNAK (containing 13C-labeled lysine), derived from synthetic protein concatamers (QconCAT) (PolyQuant GmbH, Germany). Briefly, homogenized tissues (50 μg protein) were mixed with 3.22 fmol of QconCAT per 1 μg of total protein. In-gel tryptic digestion (1:100 g/g sequencing grade modified trypsin V5111, Promega) was performed after reduction with 10 mM dithiothreitol and alkylation with 55 mM iodoacetamide proteins, followed by solid phase extraction (SPE C18-Aq 50 mg/1 ml, Gracepure) for sample cleanup. The peptide was targeted and analyzed by a triple quadrupole mass spectrometer equipped with a nano-electrospray ion source (TSQ Vantage, Thermo Scientific). The chromatographic separation of the peptides was performed by liquid chromatography on a nano-UHPLC system (Ultimate UHPLC focused, Dionex) using a nanocolumn (Acclaim PepMap100 C18, 75 µm × 500 mm 2 µm, 100 Å) with a linear gradient from 3% to 60% v/v acetonitrile plus 0.1% v/v formic acid in 110 min at a flowrate of 200 nl/min. The MS traces were manually curated using the Skyline software (39) prior to integration of the peak areas for quantification. The sum of all transition peak areas for the endogenous peptide and isotopically labeled QconCAT-peptide standard was used to calculate the ratio between the endogenous and standard peptides. The concentrations of the endogenous peptides were calculated from the known concentration of the standard and expressed in femtomoles per microgram of total protein.
Analysis of hepatic HMG levels
Liver samples were homogenized in PBS and sonicated to a 15 (w/w %) liver homogenate. To allow quantification of HMG, an internal standard of 0.05 mg/ml 4-phenyl-butyric acid was added to 1.5 ml homogenate and centrifuged at 20,800 g for 5 min at 4°C (Eppendorf Centrifuge 5417R), and the supernatant was collected. One hundred microliters of ethoxim was added to the samples and subsequently incubated at 60°C. Approximately 150 μl of 12N HCl and approximately 10 mg of NaCl were added to the samples. Organic acids were extracted by adding 4 ml of a mixture of ether and ethylacetate (1:1), vortexed for 3 min, and centrifuged for 10 min at 3,500 g (Megafuge 1.0, Heraeus Sepatech). The supernatant was collected, and the extraction was repeated once more. The supernatant was evaporated at 50°C under a stream of nitrogen. The dried samples were derivatized by adding 100 µl BSTFA:TMCS:pyridine (5:0.06:1) and heated for 30 min at 60°C. Concentrations of HMG were further analyzed using GC/MS (Finigan Trace GC/MS, ThermoQuest) as previously described (40).
Analysis of lathosterol, desmosterol, and lanosterol in plasma
To allow quantification of lathosterol, desmosterol, and lanosterol in plasma, 100 µl internal standards of D6-β-sitosterol (22.8 µM) and 100 µl D4-lathosterol (3.8 µM) were added to empty tubes and evaporated at 40°C under a stream of nitrogen. Subsequently, the samples were added to the tubes and extraction was performed as described previously (41). After extraction, lathosterol, desmosterol, and lanosterol concentrations were further analyzed using GC/MS (Agilent 5973N) as described previously (33).
Analysis of gene expressions
RNA isolation, cDNA synthesis, and real-time quantitative PCR were used to analyze gene expression and were performed as described previously (42).
Statistics
Statistical analysis was performed using the Kruskal-Wallis H test followed by Conover post hoc comparisons in Brightstat (43). Values are presented as XY plots and Tukey box plots. P values <0.05 were considered statistically significant.
RESULTS
Statins decrease plasma cholesterol in mice
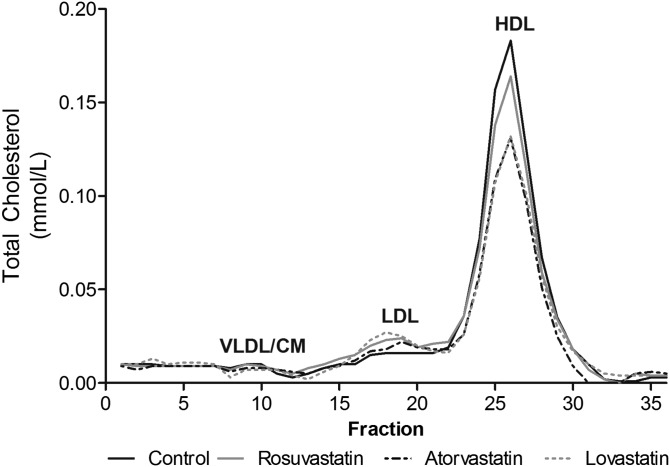
Two weeks of treatment of mice with rosuvastatin, atorvastatin, or lovastatin was well tolerated, only changes in body weight (BW), liver weight, and mass fecal output were observed in lovastatin-treated mice (Table 1). Plasma total cholesterol decreased in atorvastatin- and lovastatin-treated mice mainly attributable to decreases in HDL as indicated by FPLC profiles (Fig. 1). Furthermore, hepatic total cholesterol content was somewhat increased in lovastatin-treated mice only (Table 1).
TABLE 1.
Basal parameters and plasma and hepatic total cholesterol after 2 weeks of statin treatment
| Control | Rosuvastatin | Atorvastatin | Lovastatin | |
| BW (g) | 26.9 (25.5–28.4) | 26.7 (26.1–27.1) | 25.6 (24.7–26.1) | 24.4 (23.5–25.1)a |
| Food intake (g/day) | 4.3 (3.7–5.0) | 4.3 (3.6–4.8) | 5.4 (4.4–6.5) | 4.1 (3.7–4.6) |
| Fecal output (g/day) | 0.77 (0.73–0.83) | 0.85 (0.81–0.85) | 0.79 (0.65–0.89) | 0.60 (0.52–0.75)a |
| Liver weight (% of BW) | 4.6 (3.6–5.0) | 4.9 (4.6–5.0) | 4.4 (4.4–4.9) | 5.1 (5.0–5.6)a |
| Plasma total cholesterol (mM) | 2.32 (2.03–2.49) | 2.00 (1.86–2.26) | 1.72 (1.38–1.93)a | 1.81 (1.64–1.95)a |
| Hepatic total cholesterol (nmol/mg protein) | 29.7 (28.1–31.0) | 29.2 (26.9–31.2) | 31.5 (28.3–34.0) | 38.5 (34.8–41.0)a |
Values are expressed as median with the interquartile range.
P < 0.05 versus control.
Fig. 1.
Lipoprotein profile in plasma analyzed by FPLC. Total cholesterol concentrations were measured in FPLC fractions of 0.5 ml. Data are presented from pool of n = 7 mice per group.
Statins paradoxically increase cholesterol synthesis, primarily in the liver
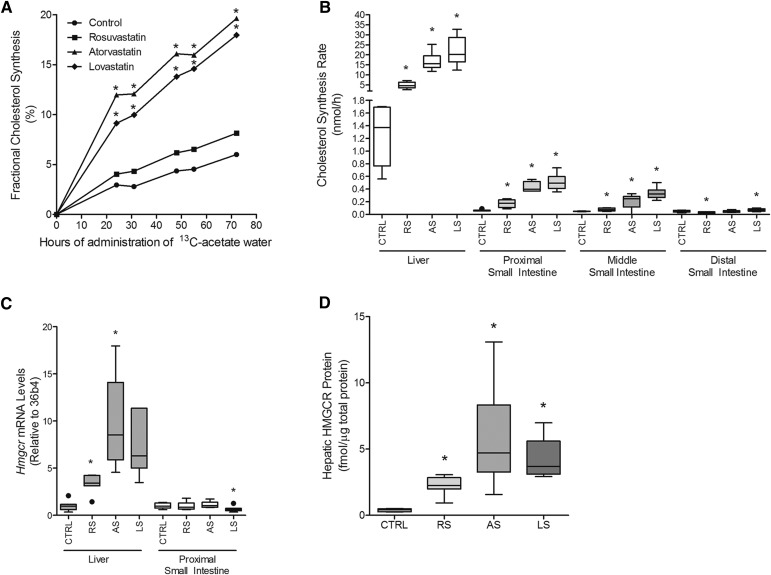
Because statins are supposedly effective by inhibiting HMGCR, we next evaluated the impact of statin administration on cholesterol synthesis. To assess in vivo cholesterol synthesis rates in response to statins, 13C-acetate was added to the drinking water of the mice. Remarkably, and in apparent contrast with the expectation of statins inhibiting HMGCR activity, treatment with atorvastatin and lovastatin led to a robust increase in measured cholesterol synthesis rates (Fig. 2A). These data reflect cholesterol synthesis during a period of 3 days. To investigate the contribution of the liver or small intestine, organ-specific cholesterol synthesis in these organs was determined using deuterated water. Also, certain limitations associated with the use of labeled acetate as a precursor to measure cholesterol synthesis have been reported, likely related to differences in cell entry of acetate or its conversion into acetyl-CoA between different cells and organs (44). Labeled water equilibrates with body water within minutes and therefore does not have this potential drawback. Therefore, cholesterol synthesis measured using D2O served not only as an organ-specific assessment for this parameter, but also as a validation of the results obtained with 13C-acetate. The data obtained using D2O confirmed that statin treatment strongly enhances cholesterol synthesis. A strong induction was observed in the liver, whereas only a modest increase was observed in the proximal, middle, and distal parts of the small intestine (Fig. 2B). Increased hepatic cholesterol synthesis thus appears to be responsible for a major part of the increase in cholesterol synthesis found with the 13C-acetate method. In keeping with this finding, no increase in gene expression of Hmgcr in the small intestine was detected in contrast to the liver, further indicating that statins induced hepatic cholesterol synthesis more strongly than intestinal cholesterol synthesis (Fig. 2C). Because HMGCR is subject to extensive regulation at the protein level, hepatic protein levels of this enzyme were measured as well. Indicative of posttranscriptional regulation as a mechanism counteracting inhibition of HMGCR by statins, hepatic protein levels showed a stronger induction as mRNA levels. On average, HMGCR protein levels were 6-, 15-, and 11-fold higher in mice treated with rosuvastatin, atorvastatin, and lovastatin, respectively, compared with controls (Fig. 2D).
Fig. 2.
Cholesterol synthesis is increased in statin-treated mice. A: Statin treatment leads to increased total body cholesterol synthesis measured by the incorporation of 13C-acetate into the cholesterol molecule over a period of 72 h. B: Hepatic cholesterol synthesis is highly increased after statin treatment, compared with the proximal, middle, and distal parts of the small intestine using deuterium water. C: mRNA levels of Hmgcr in the liver are increased, however, not in the small intestine. D: Hepatic HMGCR protein concentrations were increased after statin treatment. n = 6–7 animals per group. * P < 0.05 compared with control. AS, atorvastatin; CTRL, control; LS, lovastatin; RS, rosuvastatin.
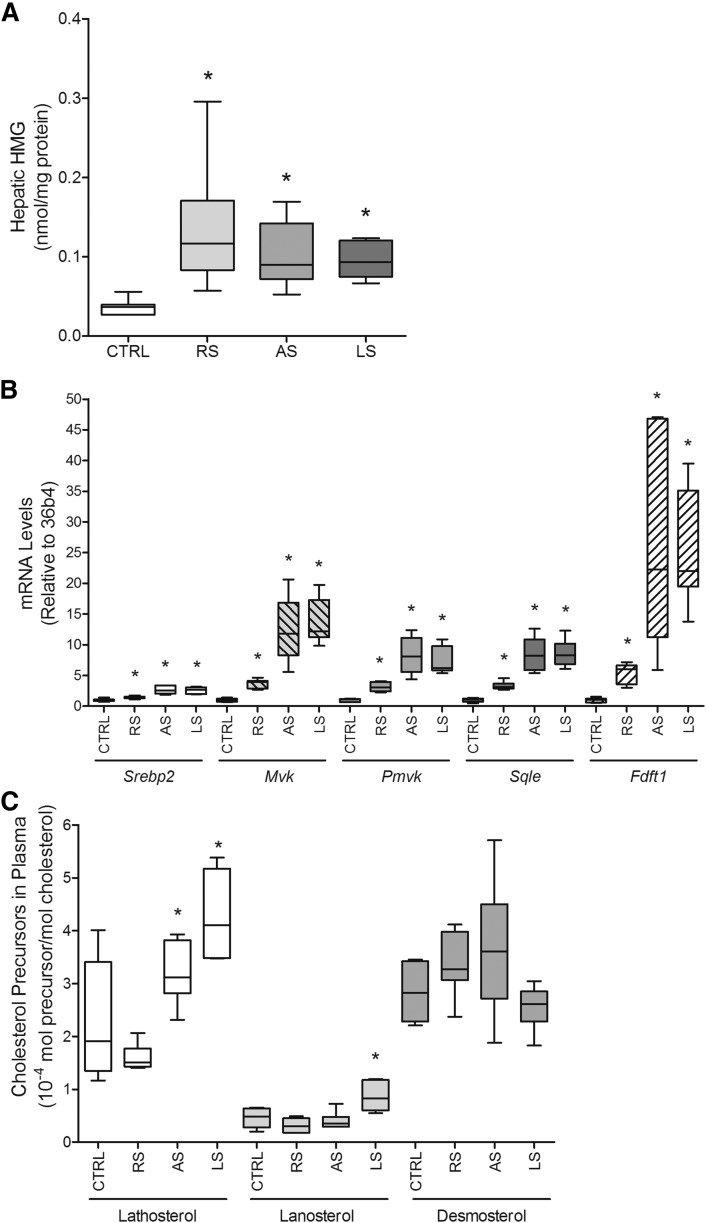
Statin treatment results in accumulation of HMG
Apparently, an inhibitor of HMGCR is able to increase cholesterol synthesis, and this led to the hypothesis of whether an accumulation of the natural substrate of HMGCR could outcompete the binding of statins to HMGCR. We did not succeed in measuring HMG-CoA; instead, concentrations of HMG, a degradation product of HMG-CoA, were analyzed. Hepatic HMG levels were indeed increased in statin-treated mice (Fig. 3A), suggesting that there is an accumulation of the natural substrate for HMGCR that may counteract the inhibitory action of the statins to a certain degree and thereby contribute to the observed increase in cholesterol synthesis. Next, the effects of statins on the cholesterol synthesis pathway downstream of HMGCR were investigated. Statin treatment led to an increased expression of the regulator of cholesterol synthesis Srebf2/Srebp2 in the liver (Fig. 3B). Subsequently, gene expression levels of other enzymes in the cholesterol synthesis pathway, which are target genes of SREBP2, were analyzed (45). Statin treatment strongly induced gene expression of the cholesterol synthesis enzymes Mvk (mevalonate kinase), Pmvk (phosphomevalonate kinase), Fdft1/Sqs (farnesyl-diphosphate farnesyltransferase 1), and Sqle (squalene epoxidase) (Fig. 3B).
Fig. 3.
Plasma cholesterol precursor concentrations do not reflect cholesterol synthesis in mice. A: Hepatic HMG levels are increased upon statin treatment. B: Statin treatment increases gene expression of the regulator of cholesterol synthesis Srebp2 and of enzymes acting downstream in the cholesterol synthesis pathway. C: Minor changes in the concentrations of the cholesterol synthesis precursors lathosterol, lanosterol, and desmosterol were observed upon statin treatment. n = 7 animals per group. * P < 0.05 compared with control.
Intermediates of cholesterol synthesis do not reflect synthesis rates in statin-treated mice
Intermediates of cholesterol synthesis are often used to estimate cholesterol synthesis, and these data indicate that a decrease in cholesterol synthesis by statins can be monitored by a reduction in the plasma levels of precursors of cholesterol synthesis. The concentrations of the cholesterol synthesis precursors lathosterol, lanosterol, and desmosterol were analyzed in plasma to determine whether these are indeed suitable as surrogate biomarkers for cholesterol synthesis. Lathosterol measurements showed a slight increase atorvastatin- and lovastatin-treated mice. A minor increase in lanosterol levels was observed only in lovastatin-treated mice. No differences in desmosterol concentrations could be detected in any of the groups (Fig. 3C). Altogether, none of these markers accurately reflected cholesterol synthesis rates in the presence of statins.
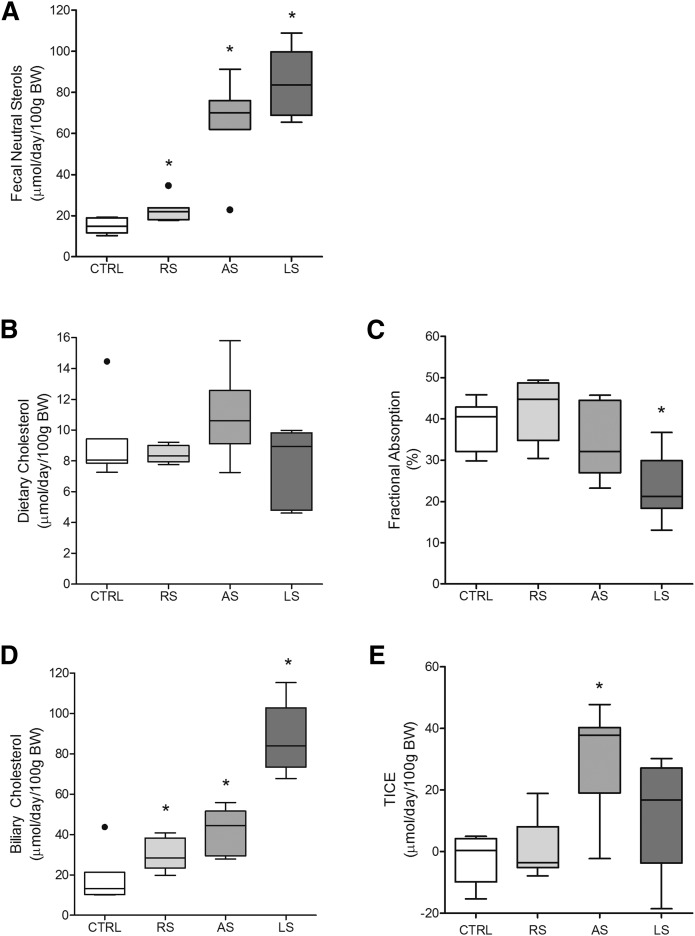
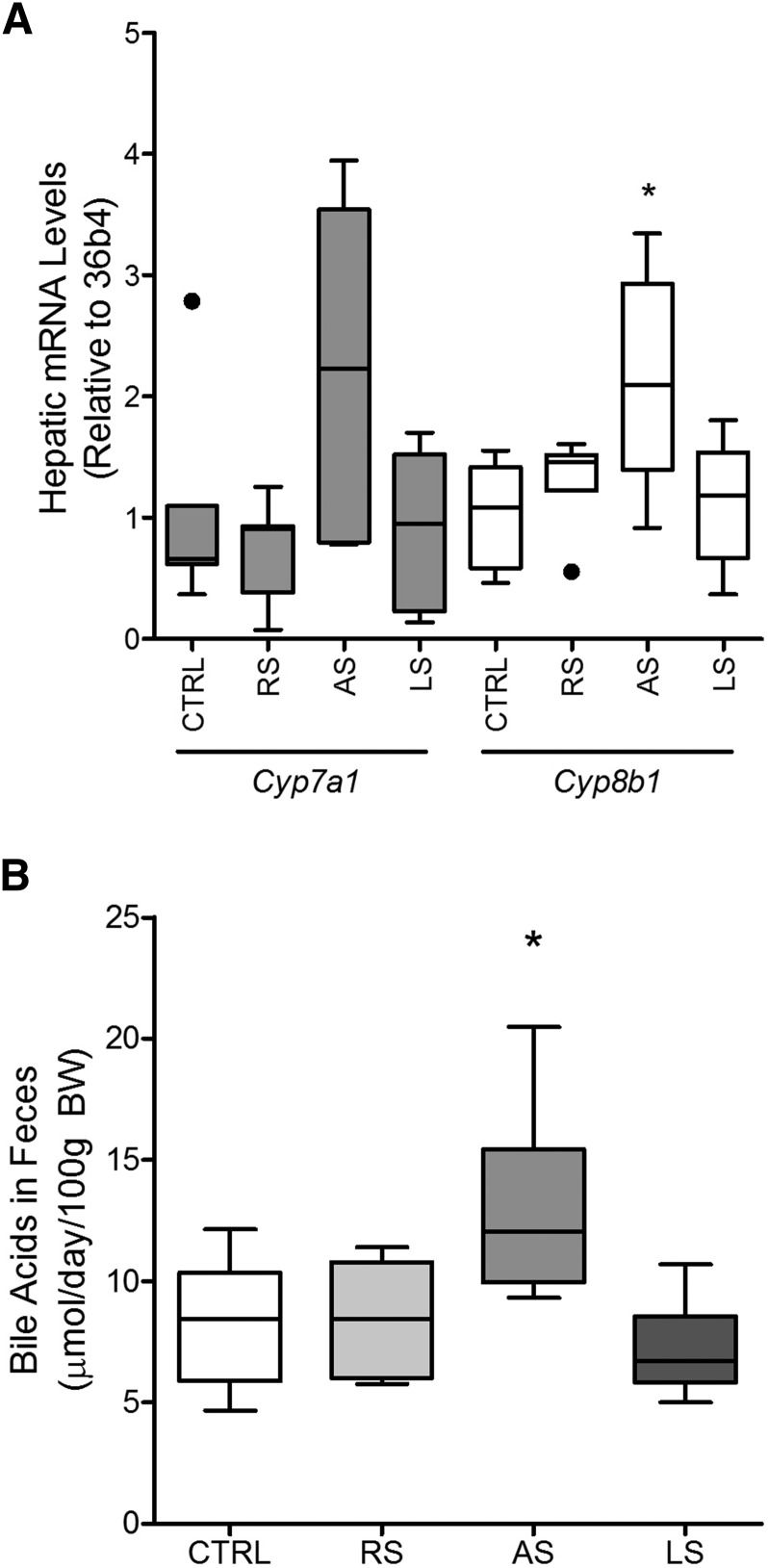
Fecal cholesterol excretion is increased in statin-treated mice
To investigate via which pathway the flux of cholesterol from the plasma is mediated, we analyzed gene expressions of Srebp2 target genes, which mediate cholesterol influx and efflux transport. The LDLR is a transporter that mediates import of cholesterol into the cell, and the heterodimer of ABCG5 and ABCG8 regulates cholesterol export. In the liver, statin treatment increased Ldlr expression, which suggests enhanced hepatic uptake of cholesterol from the plasma (Table 2), as well as Abcg5 and Abcg8 expression, suggesting increased transport of cholesterol from the liver into the bile (Table 2). Similarly, these transporters are also expressed in the small intestine where LDLR can mediate the influx of cholesterol from the basolateral side of the enterocytes, while the ABGC5/ABCG8 heterodimer facilitates efflux toward the intestinal lumen. In contrast to the liver, no increase in gene expression levels of any of these transporters was detected in the small intestine (Table 2). The results described above show that statins enhance cholesterol synthesis but do not increase plasma cholesterol levels or to a major extent hepatic cholesterol content. We therefore hypothesized that the newly synthesized cholesterol is quickly eliminated from the body and thus assessed the effect of statins on fecal neutral sterol excretion. Indeed, fecal neutral sterol excretion was increased in the statin-treated mice (Fig. 4A). Fecal cholesterol can originate from three different pathways: i) unabsorbed cholesterol from the diet, ii) biliary cholesterol secretion, or iii) TICE (46). In addition, absorption of cholesterol in the small intestine is also an important determinant of the cholesterol balance. The intake of cholesterol via the diet was the same in all groups (Fig. 4B), and fractional cholesterol absorption was decreased only in lovastatin-treated mice (Fig. 4C). The dietary cholesterol and fractional absorption alone are not sufficient to explain the increase in fecal neutral sterols. However, biliary cholesterol was increased upon statin treatment, and this was most pronounced in the lovastatin-treated group (Fig. 4D). By subtracting nonabsorbed cholesterol of dietary and biliary origin from the fecal neutral sterols, the contribution of TICE can be estimated. Interestingly, statin treatment led to increased TICE only in atorvastatin-treated mice (Fig. 4E). These results show that the increased fecal neutral sterol excretion is mainly due to increased excretion of cholesterol via the hepatobiliary route upon administration of rosuvastatin and lovastatin, while atorvastatin leads to a substantial increase in TICE. Bile salt synthesis is a major pathway of cholesterol catabolism. Therefore, the effects of statin treatment on hepatic mRNA expression of the key genes in bile salt synthesis were measured. Hepatic expression of cytochrome P450, family 7, subfamily a, polypeptide 1 (Cyp7a1) was somewhat higher in the animals treated with atorvastatin but was unaffected in mice receiving rosuvastatin or lovastatin (Fig. 5A). Cytochrome P450, family 8, subfamily b, polypeptide 1 (Cyp8b1) was significantly increased in atorvastatin mice only (Fig. 5A). Under steady-state conditions, fecal bile salt excretion reflects bile salt synthesis. Indicative of increased bile salt synthesis, fecal bile salts were increased in mice treated with atorvastatin, whereas no differences were observed in mice receiving the other statins (Fig. 5B). The increase in fecal bile salt secretion in atorvastatin-treated mice could be entirely attributed to cholate-derived bile salt species (data not shown). Increased cholesterol catabolism due to increased bile salt synthesis therefore likely underlies the increased cholesterol synthesis observed in atorvastatin-treated mice to some extent. However, bile salt synthesis does not appear to be affected in mice treated with rosuvastatin or lovastatin and therefore cannot explain increased cholesterol synthesis in those mice.
TABLE 2.
Gene expression levels in liver and proximal small intestine
| Control | Rosuvastatin | Atorvastatin | Lovastatin | |
| Liver | ||||
| Abcg5 | 1.0 (0.6–1.6) | 1.5 (1.3–1.7) | 2.9 (1.9–3.6)a | 4.2 (3.0–5.0)a |
| Abcg8 | 1.0 (0.5–1.5) | 1.5 (1.3–1.7) | 2.9 (1.9–3.8)a | 3.6 (2.6–4.4)a |
| Ldlr | 1.0 (0.8–1.2) | 1.3 (1.2–1.4)a | 2.1 (1.5–2.7)a | 1.9 (1.5–2.4)a |
| Proximal small intestine | ||||
| Abcg5 | 1.0 (0.4–1.7) | 0.7 (0.2–0.9) | 0.9 (0.7–1.0) | 0.3 (0.2–0.5)a |
| Abcg8 | 1.0 (0.5–1.8) | 0.9 (0.1–1.3) | 1.0 (0.8–1.2) | 0.4 (0.2–0.5) |
| Ldlr | 1.0 (0.7–1.2) | 0.6 (0.5–0.8)a | 0.8 (0.5–1.1) | 0.4 (0.3–0.5)a |
Results were normalized to 36b4 mRNA levels and to the values of the control group. Values are expressed as median with the interquartile range.
P < 0.05 vs. control.
Fig. 4.
Atorvastatin and lovastatin treatment increases fecal neutral sterol excretion. A: After 2 weeks of statin treatment, fecal neutral sterols are increased. The increase of fecal neutral sterols could not be explained by changes in dietary cholesterol (B) or fractional cholesterol absorption (C) but is largely due to the contribution of biliary cholesterol (D) and slightly to TICE (E). n = 7 animals per group. * P < 0.05 compared with control.
Fig. 5.
Increased fecal bile acids in atorvastatin-treated mice. A: Hepatic gene expression levels of Cyp7a1 and Cyp8b1. Cyp7a1 is increased in mice treated with atorvastatin. B: Biliary bile acids in feces are increased in atorvastatin-treated mice. n = 7 animals per group. * P < 0.05 compared with control.
DISCUSSION
This study demonstrates that treatment of mice with statins paradoxically increases cholesterol synthesis. These findings are surprising considering the fact that statins inhibit HMGCR, the rate-limiting enzyme of cholesterol synthesis. The three statins used in this study induced different effects. Atorvastatin and lovastatin strongly increased cholesterol synthesis, whereas only a slight effect of rosuvastatin was observed. Surprisingly, the effect on plasma cholesterol was the opposite. Despite increasing cholesterol synthesis, atorvastatin and lovastatin modestly decreased levels of plasma cholesterol, confirming earlier studies. The reduced efficacy of statins in rodents compared with humans has been explained by the fact that statins primarily control levels of LDL cholesterol, which is compared with HDL a minor component in plasma lipoproteins of mice (47).
The inhibition of cholesterol synthesis by statins has been described in numerous cell culture studies (19, 48). Assuming that this effect can be translated to in vivo conditions, cholesterol synthesis is rarely measured in experiments in humans or rodent models. Yet, compared with the in vitro experiments in cultured cells, the in vivo situation is more complex because due to the longer term more system adaptation can be expected. It is well known that statins strongly induce expression of Hmgcr via a SREBP2-mediated pathway (21). Although in our experiments statins were dosed via the diet at high levels, in principle fasting during the light period could lead to a decrease in statin concentration inducing a short relief of inhibition leading to an overshoot of synthesis. An overshoot of cholesterol synthesis upon statin withdrawal has been shown in rats (20, 49). To investigate whether such a phenomenon occurred during our experiments, we have monitored cholesterol synthesis for up to 72 h. Surprisingly, synthesis rates were lowest during the light phase indicating that fasting did not induce overshoots in synthesis. In contrast, apart from the well-known circadian rhythm in cholesterol synthesis (50), rates were remarkably constant. Measurements of organ-specific cholesterol synthesis in this study revealed that hepatic cholesterol synthesis was profoundly increased in statin-treated animals following the extent of overexpression of the enzyme. Intestinal synthesis was increased much less. These results are in accordance with the study of Chuang et al. (51) who have measured an increase in acute cholesterol synthesis in BALB/c mice treated with simvastatin. Interestingly, Freeman et al. (52) showed that lovastatin reduced HMGCR activity in human intestinal biopsies. Administration of compounds that inhibit in vivo processes usually induce adaptive homeostatic reactions. It is, however, difficult to predict to what extend such compensatory reactions of a system could be counterbalanced by adjustment of the dose of the inhibitor. Because statins are competitive inhibitors, a compensatory increase in the amount of HMGCR protein or accumulation of the endogenous substrate, HMG-CoA, could impact the competition balance and cholesterol synthesis rates. HMG-CoA protein levels were up to 15-fold higher in statin-treated mice. We have not succeeded in measuring hepatic levels of HMG-CoA. As a proxy of increased HMG-CoA, we have measured the concentration of the breakdown product HMG, which was indeed increased. Those data suggest that the competition hypothesis may be valid. The increased cholesterol synthesis was not reflected by increased cholesterol in plasma or in the liver indicating that steroid produced in excess is possibly removed by reverse cholesterol transport. Indeed, statin treatment stimulated fecal neutral sterol excretion. The increase in fecal neutral sterol excretion could not be explained by changes in dietary cholesterol intake or fractional cholesterol absorption. Calculation of cholesterol fluxes revealed that the increase in neutral sterols after statin treatment is primarily caused via induction of biliary cholesterol secretion. This is in accordance with data from studies in statin-treated rats that similarly found an increased secretion of cholesterol into the bile (23, 53). Interestingly, the increase in neutral sterols observed in atorvastatin-treated mice was also due to an increase in TICE. No significant induction of TICE in lovastatin-treated mice was observed in our study, in contrast to a previous study from Le May et al. (30) who did observe stimulated TICE in lovastatin-treated mice. We have no explanation for this discrepancy.
Cholesterol synthesis is rarely measured directly; in most cases, synthesis is estimated from surrogate markers such as intermediates of the cholesterol synthesis pathway. The plasma concentrations of these intermediates, such as lathosterol, lanosterol, or desmosterol, are generally accepted as suitable surrogate markers for cholesterol synthesis (11, 12). It is mostly not appreciated that the validity of the use of these surrogate markers depends on constancy of the ratios of activities of the involved enzymes. Statins not only lead to induction of HMGCR but via the Srebp2 pathway also induce expression of the other enzymes in the pathway. Increased activity of these enzymes will invalidate the use of the concentration of their substrates or products as a marker of the rate of cholesterol synthesis. Indeed we saw little change in the plasma concentration of lathosterol, desmosterol, and lanosterol at the increased rates of cholesterol synthesis measured in this study. Clearly, these surrogate markers should be used with great caution as biomarkers of cholesterol synthesis in patients treated with statins.
This research contributes to a better understanding of the mechanism of action of one of the most prescribed drugs in the world. Translation of the results to humans will require in-depth estimation of cholesterol synthesis in humans, which is difficult to accomplish because of ethical reasons. It should be noted that there are certain species differences in cholesterol metabolism upon statin treatment. For instance, in line with data reported previously, we found increased biliary cholesterol secretion in statin-treated mice. However, a reduction of biliary cholesterol secretion and saturation index has been observed in humans treated with pravastatin (17, 24) or lovastatin (54). In addition, statin use was associated with a reduction in the risk of gallstone disease (55), supporting decreased rather than increased biliary cholesterol secretion rates. The effect of statins on TICE has not been assessed in humans. Augmented fecal bile salt excretion, a surrogate of synthesis, has been reported in atorvastatin-treated mice (29). We also observed increased fecal excretion of bile salts in mice treated with atorvastatin but found no change with other statins. In humans, lovastatin treatment was associated with a decrease in bile salt synthesis (54). The effects on biliary secretion may indicate inhibition of hepatic cholesterol synthesis in humans. However, the few early studies in statin-treated humans that applied direct methods to measure cholesterol synthesis and failed to prove a reduced cholesterol synthesis (16) or even pointed toward increased cholesterol synthesis (17) indicate that whole body cholesterol synthesis may also be augmented in humans. If increased cholesterol synthesis after statin treatment is also the case in humans, then it would be important to investigate whether this would also lead to enhanced fecal excretion of neutral sterols or if the newly synthesized cholesterol undergoes a different fate.
In summary, this study reveals a paradoxical increase in hepatic cholesterol synthesis in mice treated with the HMGCR inhibitors rosuvastatin, atorvastatin, and lovastatin. However, statin-treated mice do have reduced plasma cholesterol levels. This can likely be explained by increased fecal neutral sterol excretion, which is mainly attributed to an increase in the biliary cholesterol flux in rosuvastatin- and lovastatin-treated mice. After atorvastatin treatment, TICE also contributes to fecal neutral sterol excretion. In addition, this study is also the first to question the clinical usefulness of cholesterol precursor levels in plasma as surrogate biomarkers for cholesterol synthesis.
Acknowledgments
Theo Boer, Albert Gerding, Renze Boverhof, and Rick Havinga are kindly acknowledged for expert technical assistance.
Footnotes
Abbreviations:
- BW
- body weight
- Cyp7a1
- cytochrome P450, family 7, subfamily a, polypeptide 1
- Cyp8b1
- cytochrome P450, family 8, subfamily b, polypeptide 1
- FPLC
- fast-protein liquid chromatography
- HMGCR
- HMG-CoA reductase
- LDLR
- LDL receptor
- SREBF2/SREBP2
- sterol regulatory element-binding protein 2
- TICE
- transintestinal cholesterol excretion
This work was supported in part by Foundation LeDucq (Transatlantic Network, 2009-2014), the Netherlands Cardiovascular Research Initiative (CVON2011-2016; Genius), and the European Union (Transcard Grants FP7-305707 and FP7-603091-2). J. A. Kuivenhoven is an Established Investigator of the Netherlands Heart Foundation (2015T068).
REFERENCES
- 1.McKenney J. M. 2003. Pharmacologic characteristics of statins. Clin. Cardiol. 26 (Suppl. 3): 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schachter M. 2005. Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundam. Clin. Pharmacol. 19: 117–125. [DOI] [PubMed] [Google Scholar]
- 3.Vaughan C. J., and Gotto A. M. Jr. 2004. Update on statins: 2003. Circulation. 110: 886–892. [DOI] [PubMed] [Google Scholar]
- 4.Istvan E. S. 2002. Structural mechanism for statin inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase. Am. Heart J. 144 (Suppl.): S27–S32. [DOI] [PubMed] [Google Scholar]
- 5.Nohturfft A., DeBose-Boyd R. A., Scheek S., Goldstein J. L., and Brown M. S.. 1999. Sterols regulate cycling of SREBP cleavage-activating protein (SCAP) between endoplasmic reticulum and Golgi. Proc. Natl. Acad. Sci. USA. 96: 11235–11240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakai J., and Rawson R. B.. 2001. The sterol regulatory element-binding protein pathway: control of lipid homeostasis through regulated intracellular transport. Curr. Opin. Lipidol. 12: 261–266. [DOI] [PubMed] [Google Scholar]
- 7.Brown M. S., and Goldstein J. L.. 1999. A proteolytic pathway that controls the cholesterol content of membranes, cells, and blood. Proc. Natl. Acad. Sci. USA. 96: 11041–11048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith J. R., Osborne T. F., Goldstein J. L., and Brown M. S.. 1990. Identification of nucleotides responsible for enhancer activity of sterol regulatory element in low density lipoprotein receptor gene. J. Biol. Chem. 265: 2306–2310. [PubMed] [Google Scholar]
- 9.Briggs M. R., Yokoyama C., Wang X., Brown M. S., and Goldstein J. L.. 1993. Nuclear protein that binds sterol regulatory element of low density lipoprotein receptor promoter. I. Identification of the protein and delineation of its target nucleotide sequence. J. Biol. Chem. 268: 14490–14496. [PubMed] [Google Scholar]
- 10.Wang X., Briggs M. R., Hua X., Yokoyama C., Goldstein J. L., and Brown M. S.. 1993. Nuclear protein that binds sterol regulatory element of low density lipoprotein receptor promoter. II. Purification and characterization. J. Biol. Chem. 268: 14497–14504. [PubMed] [Google Scholar]
- 11.Naoumova R. P., Marais A. D., Mountney J., Firth J. C., Rendell N. B., Taylor G. W., and Thompson G. R.. 1996. Plasma mevalonic acid, an index of cholesterol synthesis in vivo, and responsiveness to HMG-CoA reductase inhibitors in familial hypercholesterolaemia. Atherosclerosis. 119: 203–213. [DOI] [PubMed] [Google Scholar]
- 12.Miettinen T. A., and Gylling H.. 2003. Synthesis and absorption markers of cholesterol in serum and lipoproteins during a large dose of statin treatment. Eur. J. Clin. Invest. 33: 976–982. [DOI] [PubMed] [Google Scholar]
- 13.Vanhanen H., Kesaniemi Y. A., and Miettinen T. A.. 1992. Pravastatin lowers serum cholesterol, cholesterol-precursor sterols, fecal steroids, and cholesterol absorption in man. Metabolism. 41: 588–595. [DOI] [PubMed] [Google Scholar]
- 14.Vanhanen H. T., and Miettinen T. A.. 1995. Cholesterol absorption and synthesis during pravastatin, gemfibrozil and their combination. Atherosclerosis. 115: 135–146. [DOI] [PubMed] [Google Scholar]
- 15.Gylling H., and Miettinen T. A.. 1996. Effects of inhibiting cholesterol absorption and synthesis on cholesterol and lipoprotein metabolism in hypercholesterolemic non-insulin-dependent diabetic men. J. Lipid Res. 37: 1776–1785. [PubMed] [Google Scholar]
- 16.Goldberg I. J., Holleran S., Ramakrishnan R., Adams M., Palmer R. H., Dell R. B., and Goodman D. S.. 1990. Lack of effect of lovastatin therapy on the parameters of whole-body cholesterol metabolism. J. Clin. Invest. 86: 801–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kallien G., Lange K., Stange E. F., and Scheibner J.. 1999. The pravastatin-induced decrease of biliary cholesterol secretion is not directly related to an inhibition of cholesterol synthesis in humans. Hepatology. 30: 14–20. [DOI] [PubMed] [Google Scholar]
- 18.Morand O. H., Aebi J. D., Dehmlow H., Ji Y. H., Gains N., Lengsfeld H., and Himber J.. 1997. Ro 48–8.071, a new 2,3-oxidosqualene:lanosterol cyclase inhibitor lowering plasma cholesterol in hamsters, squirrel monkeys, and minipigs: comparison to simvastatin. J. Lipid Res. 38: 373–390. [PubMed] [Google Scholar]
- 19.Bergstrom J. D., Bostedor R. G., Rew D. J., Geissler W. M., Wright S. D., and Chao Y. S.. 1998. Hepatic responses to inhibition of 3-hydroxy-3-methylglutaryl-CoA reductase: a comparison of atorvastatin and simvastatin. Biochim. Biophys. Acta. 1389: 213–221. [DOI] [PubMed] [Google Scholar]
- 20.Fujioka T., Nara F., Tsujita Y., Fukushige J., Fukami M., and Kuroda M.. 1995. The mechanism of lack of hypocholesterolemic effects of pravastatin sodium, a 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, in rats. Biochim. Biophys. Acta. 1254: 7–12. [DOI] [PubMed] [Google Scholar]
- 21.Roglans N., Verd J. C., Peris C., Alegret M., Vazquez M., Adzet T., Diaz C., Hernandez G., Laguna J. C., and Sanchez R. M.. 2002. High doses of atorvastatin and simvastatin induce key enzymes involved in VLDL production. Lipids. 37: 445–454. [DOI] [PubMed] [Google Scholar]
- 22.Verd J. C., Peris C., Alegret M., Diaz C., Hernandez G., Vazquez M., Adzet T., Laguna J. C., and Sanchez R. M.. 1999. Different effect of simvastatin and atorvastatin on key enzymes involved in VLDL synthesis and catabolism in high fat/cholesterol fed rabbits. Br. J. Pharmacol. 127: 1479–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamauchi S., Linscheer W. G., and Beach D. H.. 1991. Increase in serum and bile cholesterol and HMG-CoA reductase by lovastatin in rats. Am. J. Physiol. 260: G625–G630. [DOI] [PubMed] [Google Scholar]
- 24.Reihnér E., Rudling M., Stahlberg D., Berglund L., Ewerth S., Björkhem I., Einarsson K., and Angelin B.. 1990. Influence of pravastatin, a specific inhibitor of HMG-CoA reductase, on hepatic metabolism of cholesterol. N. Engl. J. Med. 323: 224–228. [DOI] [PubMed] [Google Scholar]
- 25.Gazzerro P., Proto M. C., Gangemi G., Malfitano A. M., Ciaglia E., Pisanti S., Santoro A., Laezza C., and Bifulco M.. 2012. Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharmacol. Rev. 64: 102–146. [DOI] [PubMed] [Google Scholar]
- 26.Pasha M. K., Muzeeb S., Basha S. J., Shashikumar D., Mullangi R., and Srinivas N. R.. 2006. Analysis of five HMG-CoA reductase inhibitors–atorvastatin, lovastatin, pravastatin, rosuvastatin and simvastatin: pharmacological, pharmacokinetic and analytical overview and development of a new method for use in pharmaceutical formulations analysis and in vitro metabolism studies. Biomed. Chromatogr. 20: 282–293. [DOI] [PubMed] [Google Scholar]
- 27.Neto-Ferreira R., Rocha V. N., Souza-Mello V., Mandarim-de-Lacerda C. A., and de Carvalho J. J.. 2013. Pleiotropic effects of rosuvastatin on the glucose metabolism and the subcutaneous and visceral adipose tissue behavior in C57Bl/6 mice. Diabetol. Metab. Syndr. 5: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marchesi M., Parolini C., Caligari S., Gilio D., Manzini S., Busnelli M., Cinquanta P., Camera M., Brambilla M., Sirtori C. R., et al. 2011. Rosuvastatin does not affect human apolipoprotein A-I expression in genetically modified mice: a clue to the disputed effect of statins on HDL. Br. J. Pharmacol. 164: 1460–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parker R. A., Garcia R., Ryan C. S., Liu X., Shipkova P., Livanov V., Patel P., and Ho S. P.. 2013. Bile acid and sterol metabolism with combined HMG-CoA reductase and PCSK9 suppression. J. Lipid Res. 54: 2400–2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Le May C., Berger J. M., Lespine A., Pillot B., Prieur X., Letessier E., Hussain M. M., Collet X., Cariou B., and Costet P.. 2013. Transintestinal cholesterol excretion is an active metabolic process modulated by PCSK9 and statin involving ABCB1. Arterioscler. Thromb. Vasc. Biol. 33: 1484–1493. [DOI] [PubMed] [Google Scholar]
- 31.Brufau G., and Groen A. K.. 2011. Characterization of whole body cholesterol fluxes in the mouse. Curr. Protoc. Mouse Biol. 1: 413–427. [DOI] [PubMed] [Google Scholar]
- 32.Previs S. F., Mahsut A., Kulick A., Dunn K., Andrews-Kelly G., Johnson C., Bhat G., Herath K., Miller P. L., Wang S. P., et al. 2011. Quantifying cholesterol synthesis in vivo using (2)H(2)O: enabling back-to-back studies in the same subject. J. Lipid Res. 52: 1420–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Veen J. N., van Dijk T. H., Vrins C. L., van Meer H., Havinga R., Bijsterveld K., Tietge U. J., Groen A. K., and Kuipers F.. 2009. Activation of the liver X receptor stimulates trans-intestinal excretion of plasma cholesterol. J. Biol. Chem. 284: 19211–19219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Out C., Patankar J. V., Doktorova M., Boesjes M., Bos T., de Boer S., Havinga R., Wolters H., Boverhof R., van Dijk T. H., et al. 2015. Gut microbiota inhibit Asbt-dependent intestinal bile acid reabsorption via Gata4. J. Hepatol. 63: 697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neese R. A., Faix D., Kletke C., Wu K., Wang A. C., Shackleton C. H., and Hellerstein M. K.. 1993. Measurement of endogenous synthesis of plasma cholesterol in rats and humans using MIDA. Am. J. Physiol. 264: E136–E147. [DOI] [PubMed] [Google Scholar]
- 36.Lee W. N., Byerley L. O., Bergner E. A., and Edmond J.. 1991. Mass isotopomer analysis: theoretical and practical considerations. Biol. Mass Spectrom. 20: 451–458. [DOI] [PubMed] [Google Scholar]
- 37.Bligh E. G., and Dyer W. J.. 1959. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 37: 911–917. [DOI] [PubMed] [Google Scholar]
- 38.Voshol P. J., Havinga R., Wolters H., Ottenhoff R., Princen H. M., Oude Elferink R. P., Groen A. K., and Kuipers F.. 1998. Reduced plasma cholesterol and increased fecal sterol loss in multidrug resistance gene 2 P-glycoprotein-deficient mice. Gastroenterology. 114: 1024–1034. [DOI] [PubMed] [Google Scholar]
- 39.MacLean B., Tomazela D. M., Shulman N., Chambers M., Finney G. L., Frewen B., Kern R., Tabb D. L., Liebler D. C., and MacCoss M. J.. 2010. Skyline: an open source document editor for creating and analyzing targeted proteomics experiments. Bioinformatics. 26: 966–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gates S. C., and Sweeley C. C.. 1978. Quantitative metabolic profiling based on gas chromatography. Clin. Chem. 24: 1663–1673. [PubMed] [Google Scholar]
- 41.Windler E., Zyriax B. C., Kuipers F., Linseisen J., and Boeing H.. 2009. Association of plasma phytosterol concentrations with incident coronary heart disease: data from the CORA study, a case-control study of coronary artery disease in women. Atherosclerosis. 203: 284–290. [DOI] [PubMed] [Google Scholar]
- 42.Plösch T., Bloks V. W., Baller J. F., Havinga R., Verkade H. J., Jansen P. L., and Kuipers F.. 2002. Mdr P-glycoproteins are not essential for biliary excretion of the hydrophobic heme precursor protoporphyrin in a griseofulvin-induced mouse model of erythropoietic protoporphyria. Hepatology. 35: 299–306. [DOI] [PubMed] [Google Scholar]
- 43.Stricker D. 2008. BrightStat.com: free statistics online. Comput. Methods Programs Biomed. 92: 135–143. [DOI] [PubMed] [Google Scholar]
- 44.Andersen J. M., and Dietschy J. M.. 1979. Absolute rates of cholesterol synthesis in extrahepatic tissues measured with 3H-labeled water and 14C-labeled substrates. J. Lipid Res. 20: 740–752. [PubMed] [Google Scholar]
- 45.Horton J. D., Shah N. A., Warrington J. A., Anderson N. N., Park S. W., Brown M. S., and Goldstein J. L.. 2003. Combined analysis of oligonucleotide microarray data from transgenic and knockout mice identifies direct SREBP target genes. Proc. Natl. Acad. Sci. USA. 100: 12027–12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brufau G., Groen A. K., and Kuipers F.. 2011. Reverse cholesterol transport revisited: contribution of biliary versus intestinal cholesterol excretion. Arterioscler. Thromb. Vasc. Biol. 31: 1726–1733. [DOI] [PubMed] [Google Scholar]
- 47.Cholesterol Treatment Trialists’ (CTT) Collaboration. 2010. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 376: 1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Funatsu T., Suzuki K., Goto M., Arai Y., Kakuta H., Tanaka H., Yasuda S., Ida M., Nishijima S., and Miyata K.. 2001. Prolonged inhibition of cholesterol synthesis by atorvastatin inhibits apo B-100 and triglyceride secretion from HepG2 cells. Atherosclerosis. 157: 107–115. [DOI] [PubMed] [Google Scholar]
- 49.Bilhartz L. E., Spady D. K., and Dietschy J. M.. 1989. Inappropriate hepatic cholesterol synthesis expands the cellular pool of sterol available for recruitment by bile acids in the rat. J. Clin. Invest. 84: 1181–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Edwards P. A., Muroya H., and Gould R. G.. 1972. In vivo demonstration of the circadian rhythm of cholesterol biosynthesis in the liver and intestine of the rat. J. Lipid Res. 13: 396–401. [PubMed] [Google Scholar]
- 51.Chuang J. C., Valasek M. A., Lopez A. M., Posey K. S., Repa J. J., and Turley S. D.. 2014. Sustained and selective suppression of intestinal cholesterol synthesis by Ro 48–8071, an inhibitor of 2,3-oxidosqualene:lanosterol cyclase, in the BALB/c mouse. Biochem. Pharmacol. 88: 351–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Freeman M. L., Prigge W. F., Hunninghake D. B., Duane W. C., and Gebhard R. L.. 1988. Intestinal HMG-CoA reductase activity is low in hypercholesterolemic patients and is further decreased with lovastatin therapy. J. Lipid Res. 29: 839–845. [PubMed] [Google Scholar]
- 53.Linscheer W. G., Atreyee B., Uma K. M., John W., Sandor N., and Jyotirmoy N.. 1995. Lovastatin induces synthesis of cholesterol, which acts as a secretagogue of biliary phospholipids in rats. Am. J. Physiol. 268: G242–G250. [DOI] [PubMed] [Google Scholar]
- 54.Hanson D. S., and Duane W. C.. 1994. Effects of lovastatin and chenodiol on bile acid synthesis, bile lipid composition, and biliary lipid secretion in healthy human subjects. J. Lipid Res. 35: 1462–1468. [PubMed] [Google Scholar]
- 55.Bodmer M., Brauchli Y. B., Krahenbuhl S., Jick S. S., and Meier C. R.. 2009. Statin use and risk of gallstone disease followed by cholecystectomy. J. Am. Med. Assoc. 302: 2001–2007. [DOI] [PubMed] [Google Scholar]