Abstract
Background
Total wrist arthroplasty (TWA) provides the requisite range of motion to accomplish activities of daily living, especially for low-demand patients with bilateral wrist arthritis. However, there are no large epidemiologic studies to evaluate nationwide trends of TWA and wrist fusion (WF).
Questions/Purposes
To analyze data collected from the National Inpatient Sample (NIS) to compare utilization, demographic, and outcome data among patients undergoing TWA versus total WF. We hypothesized that utilization rates of TWA have significantly increased over the prior decade in the United States.
Methods
NIS data from 2001 to 2010 were reviewed. Procedures were identified by ICD-9-CM codes 81.73 (TWA) and 81.25 (WF). Utilization rates, primary treatment diagnoses, patient demographic and medical comorbidity data, and procedure costs were compared between TWA and WF.
Results
There was a decrease in the number of procedures per year for TWA, while the number of WF remained relatively unchanged. There was, however, a transient increase in the frequency of TWA procedures performed from 2005 to 2008, following a decline in 2005. Patients with traumatic arthritis were more likely to receive WF. Rheumatoid patients were more likely to receive TWA. Patients receiving TWA tended to be older, female, be insured by Medicare, have a greater comorbidity burden, and have rheumatologic disease.
Conclusion
WF was performed nearly four times more frequently than TWA. A trend was demonstrated toward a decreasing number of TWA being implanted, and in patients with more underlying comorbidities. TWA was associated with a higher hospitalization charge, which may be expected given the higher implant costs associated with arthroplasty.
Level of Evidence
Level II, prognostic study.
Keywords: arthritis, National Inpatient Sample, total wrist arthroplasty, wrist fusion
Wrist arthritis is commonly thought of as a relatively rare problem.1 2 In the early stages, symptomatic wrist arthritis can be managed nonoperatively using topical and oral medications, splinting, and activity modification. Less invasive, motion-preserving operative techniques including limited wrist fusion (WF), wrist denervation, and arthroscopic debridement may provide temporary relief and preservation of motion in cases unresponsive to conservative treatment. The two major options for the definitive treatment of recalcitrant, advanced wrist arthritis include total wrist arthroplasty (TWA) and total WF.3 4 5 6 Although WF is still considered by many to be the treatment of choice for management of advanced pancarpal wrist arthritis, patients frequently report limitations following fusion, involving activities such as perineal care, screwdriver use, button fastening, hair combing, and jar opening.6 7 8 Therefore, TWA has emerged as an alternative that appears to provide the requisite range of motion to accomplish activities of daily living, especially for low-demand patients with bilateral pancarpal arthritis.9 However, there are no large epidemiologic studies to evaluate nationwide trends of TWA and WF.
The purpose of this study was to analyze data collection from the National Inpatient Sample (NIS) to identify demographic and hospital data, incidence of comorbidities, and procedure-related complications associated with WF versus TWA. As a result of improved quality and design of implants, we hypothesized that the frequency of TWA performed has significantly increased over the prior decade in the United States.
Materials and Methods
We reviewed temporal trends in the utilization of TWA and WF from 2001 through 2010 using the NIS. The NIS database is the largest all-payer database of hospital discharges in the United States.10 The database was developed as a part of the Healthcare Cost and Utilization Project, which is sponsored by the Agency for Healthcare Research and Quality, which falls under the Department of Health and Human Services of the U.S. government. The database consists of approximately 20% stratified sample of U.S. hospitals. Because data in this study were de-identified, this study was exempt from review by the institutional review board. It does not contain clinical and radiographic data.
Inclusion Criteria
To identify the patients, we used the ninth revision of the International Classification of Diseases, clinical modification (ICD-9-CM). The database was searched for procedure codes of 81.73 indicating TWA and 81.25 indicating WF. Patients coded for both procedures were excluded. Individual comorbidity data were assigned using the Agency for Healthcare Research and Quality comorbidity variables, based on ICD-9-CM codes.11 Comorbidities were identified using the following ICD-9 codes: hypertension (401, 402, 403, 404, 405), diabetes mellitus (250), anemia (285), liver disease (571.8), congestive heart failure (428), hypothyroidism (244.9), chronic pulmonary disease (490–492), coagulopathy (286), electrolyte imbalance (276), obesity (278), renal disease (582, 585, 403), and metastatic and nonmetastatic cancer (199.1). Overall comorbidity burden was calculated using the Deyo comorbidity index, an adaptation of the Charlson comorbidity index.12 Both length of stay (LOS) and complication rates and cost were compared between the two treatment groups. The primary diagnoses listed in the database for the procedures evaluated were assessed by ICD codes 715.X3 and 715.X4 for osteoarthritis (OA), 716.9 for unspecified arthropathy, 716.1 for traumatic arthropathy, 733.81 and 733.82 for malunion and nonunion, and 714.0 for rheumatoid arthritis (RA).
Statistical Analysis
Statistical analysis was performed using R foundation for statistical computing, (Vienna, Austria). Differences in patient and hospital characteristics were determined using chi-square tests for categorical variables and t-test for continuous variables. Linear regression modeling was used to determine the association between procedures and year. All data undergoing statistical analysis were original data from the database and not based upon extrapolated values.
Results
There were 199 TWA and 738 WF cases found in the NIS database during this 10-year period. This was extrapolated to a national 10-year incidence corresponding to ∼995 TWA cases and 3,960 WF procedures nationwide. The calculated nationwide numbers of WF and TWA in each year are shown in Fig. 1. Over the 10-year duration reviewed, there was a decrease in the frequency (number of procedures per year) for TWA (p = 0.04), while the number of WF remained relatively constant (p = 0.13). There was, however, a transient increase in the frequency of TWA procedures observed from 2005 to 2008, following a decline in 2005, where the percentage of TWA increased from 10% in 2005 to 20% in 2006 and 2007, and 24% in 2008 (percentage of total procedures). Finally, in 2010, there was a drop in both procedures (Fig. 1).
Fig. 1.
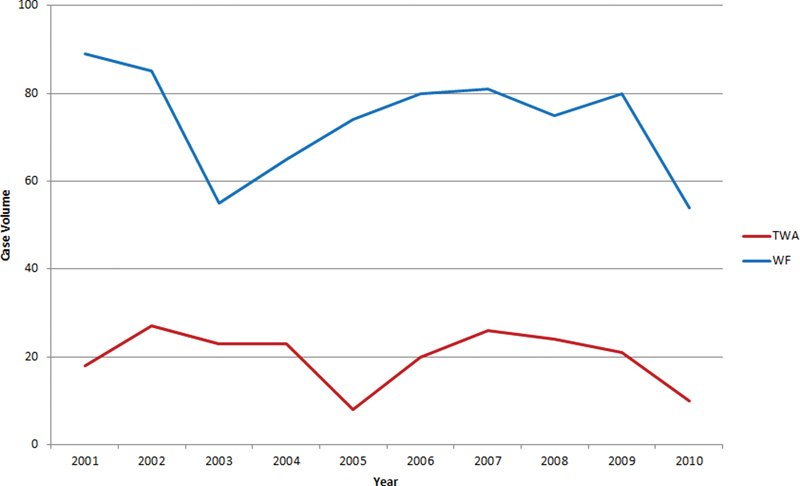
National trends of volume of total wrist arthroplasty and total wrist fusion from 2001 to 2010.
Demographic Characteristics
Mean age of the patients who underwent TWA was 58.3 years versus 52 years in patients who underwent WF (p < 0.001). Fig. 2 shows a comparison of mean age of patients in both groups during the study period. Of note, the mean age of the patients undergoing WF increased from 50 to 54 years (p < 0.05), while the age of TWA patients was unchanged. Of patients, 73% were female in the TWA group, as compared with 43% of patients in the WF group (p < 0.001). Analysis of ethnicity revealed that whites comprised 82% of the TWA and 77% of all fusions, African Americans 9% of the TWA and 12% of all fusions, and Hispanics 7% of the TWA and 8% of all fusions. The rate of whites receiving TWA was not significantly different than that of nonwhites. According to the 2010 census data, the racial categories in the United States include 72.4% whites, 12.6% African Americans, 16.4% Hispanics, and 4.8% Asian.13
Fig. 2.
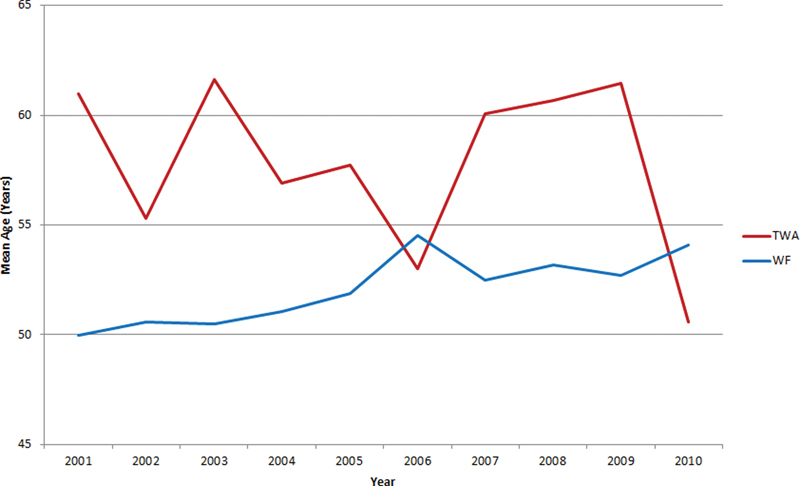
Comparison of mean age of patients in total wrist arthroplasty and total wrist fusion groups.
Comorbidities
Overall comorbidity burden calculated by Deyo comorbidity index was greater for patient undergoing TWA (TWA: 0.97; WF: 0.54; p < 0.001).
Underling Diagnoses
Based on the available coding system, RA was the most common underlying diagnosis for patients receiving TWA (51% of the TWA cases), followed by OA (34%) and unspecified arthropathy (6%). In the WF group, OA was the most common underlying diagnosis (33% of cases), followed by RA (16%), traumatic arthropathy (12%), and malunion (12%). Statistical analysis showed that patients with malunion or traumatic arthritis were more likely to receive WF by percentage (malunion: 12 vs. 3%, p < 0.001; traumatic: 12 vs. 3%, p < 0.001). Patients with RA were more likely to receive TWA (RA: 51 vs. 16%, p < 0.001). The extrapolated total number of patients who underwent WF in each diagnostic group separately, and overall, outnumbered those who underwent TWA (995 TWA vs. 3,960 WF).
Length of Stay and Cost
Average LOS was a little over 2 days for both TWA and WF. Linear regression modeling showed that for WF, LOS increased from 1.7 in 2001 to 2.9 in 2010, but this trend did not reach statistical significance (p = 0.1; Fig. 3). As seen in Fig. 4, the cost of both procedures has risen over the last 10 years, with TWA being generally more expensive than WF. TWA was associated with a higher hospitalization charge ($34,055 vs. $27,079, p < 0.01), although both TWA and WF underwent a steady increase in hospitalization charge (Fig. 4).
Fig. 3.

Trends of length of stay for total wrist arthroplasty and wrist fusion from 2001 to 2010.
Fig. 4.
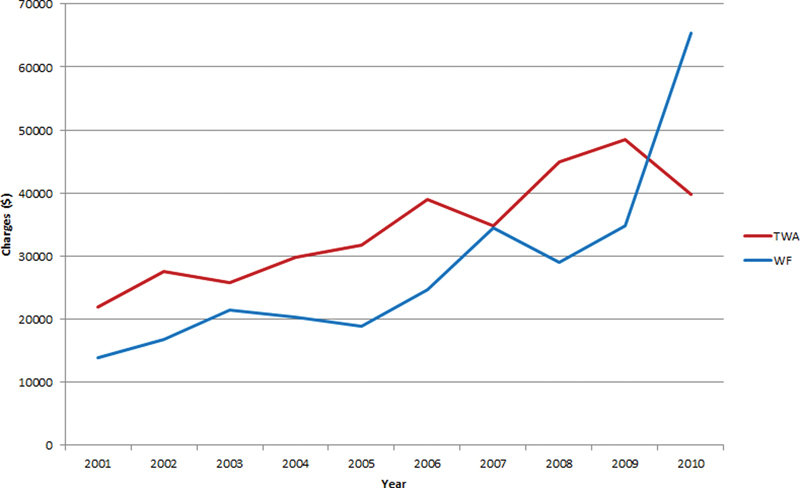
Cost of hospitalization for TWA and WF.
Complications
Total complication rate was 10% for WF and 7% for TWA (p = 0.0033). However, these complications were not stratified as being either major or minor. Patients receiving WF had a higher percentage of perioperative device–related complications (6 vs. 3%, p < 0.001) and respiratory complications (0.54 vs. 0%, p < 0.05).
Discussion
WF and TWA are two common procedures for treatment of severe end-stage wrist arthritis nonresponsive to conservative management. Although WF is often still considered the treatment of choice for the management of pancarpal arthritis, some fourth-generation TWA implants have shown good midterm survival with low failure rates.14 15 16 17 18 Yet, poor results have also been demonstrated.19 20 However, there has been no large epidemiologic study to evaluate nationwide trends of WF and TWA. To the best of our knowledge, the present study is the first report of national utilization of TWA and WF for treatment of advanced wrist arthritis.
Despite improvement in design and kinematics of newer generation TWA systems, and the potential for preservation of motion, WF was still performed about four times more frequently. Close analysis of the overall trend showed an initial surge in the early 2000s, followed by a decline in 2005. We assume that this decrease may be partly explained by the withdrawal of the Biax prosthesis (Depuy Orthopaedics) in 2004, which was one of the few FDA-approved wrist implants at the time. The Biax TWA was introduced in 1983 and its production was discontinued in 2004 without having developed a follow-up model.21 Overall, the 10-year trend was that of decreasing numbers of TWA being implanted. This may be related to the advent of biologic disease–modifying drugs for RA, which have decreased the rate of progression to painful, end-stage arthritis.22 As these medications effectively prevent disease progression, fewer patients are expected to require reconstruction of the radiocarpal joint compared with previous decades. In addition, there are several alternative reconstruction options for the rheumatoid wrist that can potentially decrease the number of TWA procedures performed. However, limited WF are appropriate in patients with early collapse patterns of the wrist and in those with destruction limited to only a portion of the radiocarpal joints.23 Another theory is that since training to perform TWA is not standard in most hand fellowship programs, surgeons will avoid procedures that are outside their training or comfort level. A final explanation may be a trend toward TWA procedures being done on an outpatient basis, thus decreasing the number of procedures being represented in the NIS database, which only accounts for inpatient surgery. Indeed, younger and healthier non-RA patients are more likely to be treated on an outpatient basis.
We are not sure as to why numbers of both procedures dropped in 2010. Since the data were retrieved in mid-2013, we would expect that all 2010 cases had been reported. A possible explanation is more procedures done in an outpatient setting, and thus a lesser number of procedures is represented, but that still would not explain the sudden drop.
Based on this study, the most common joint disorder resulting in TWA was RA (51%), followed by OA and unspecified arthropathy. The most common diagnosis resulting in WF was OA, followed by RA, traumatic arthropathy, and malunion. The present study indicates that RA patients are more likely to receive TWA than WF. Traditionally, the ideal candidates for TWA have been RA patients who comparatively lead a less active lifestyle. In a recent systemic review summarizing the results of eight articles published in the past 5 years, RA was the indication for surgery in 42% of the cases that provided the primary patient diagnosis.20 Furthermore, several other studies have described RA as an indication for TWA but have found variable outcomes.19 24 Additionally, two other studies found no difference in revision rates between the different diagnostic etiologies.16 25 These studies include data on the use of fourth-generation TWA prostheses. Our cohort includes the years from 2001 to 2010, and although NIS does not indicate the generation of TWA prosthesis used, we speculate that before 2010, use of these newer implants was more limited. Likewise, with the advent of new implant technology, TWA is increasingly offered as a treatment option to patients with posttraumatic arthritis and OA if they are able to maintain certain activity restrictions.26 Currently, fourth-generation implants are available in the market. Fourth-generation designs have been proposed in an attempt to solve the complications with previous models, mainly loosening of the distal component. Fourth-generation implants are mainly uncemented with porous titanium surfaces to allow for osseous integration. Although fourth-generation implants have shown promise, additional long-term outcome studies as well as prospective randomized trials are needed to compare TWA with WF in the management of pancarpal arthritis.
This study has several limitations that need to be recognized. The NIS database accounts for inpatient surgery only, while today many patients undergo both of these procedures on an outpatient basis. These patients were not accounted for in this database review, potentially underestimating the number of procedures performed. In addition, morbidities occurring after discharge are not captured. Thus, the findings of this study are limited to the acute perioperative period, and may underestimate the actual complication rates. Another limitation is that we were only able to report the incidence (new cases in a given time period) of TWA or WF. The prevalence (all existing cases) of TWA or WF remains unknown. While many of the results of this study are expected, namely, TWA is done more often in RA patients and that there is a very low rate of significant perioperative medical complications, it is still important to quantify this for physicians and patients. Also, the data are limited by the coding done by the hospitals, and may have had inaccuracies.
In conclusion, our analysis of this national inpatient database registry from 2001 to 2010 demonstrates that the rate of WF remains essentially constant, while the rate of TWA is on a gentle downward trend. This applies for patients undergoing inpatients surgery only, and cannot be generalized to all cases. In addition, the cost of both procedures has risen over the last 10 years, with TWA being generally more expensive than WF.
Ethical Review Committee
The study does not involve patient data and did not require ethical committee as the data used were de-identified.
Conflict of Interest None.
Note
The study was performed entirely at NYU Hospital for Joint Diseases, New York.
References
- 1.Buckwalter J A Saltzman C Brown T The impact of osteoarthritis: implications for research Clin Orthop Relat Res 2004(427, Suppl):S6–S15. [DOI] [PubMed] [Google Scholar]
- 2.Watson H K, Ballet F L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 3.Graham T J. Philadelphia, PA: Saunders; 2009. Total wrist arthrodesis and total wrist arthroplasty; pp. 90–105. [Google Scholar]
- 4.Nydick J A, Watt J F, Garcia M J, Williams B D, Hess A V. Clinical outcomes of arthrodesis and arthroplasty for the treatment of posttraumatic wrist arthritis. J Hand Surg Am. 2013;38(5):899–903. doi: 10.1016/j.jhsa.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Cavaliere C M, Chung K C. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg. 2008;122(3):813–825. doi: 10.1097/PRS.0b013e318180ece3. [DOI] [PubMed] [Google Scholar]
- 6.Murphy D M, Khoury J G, Imbriglia J E, Adams B D. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg Am. 2003;28(4):570–576. doi: 10.1016/s0363-5023(03)00182-5. [DOI] [PubMed] [Google Scholar]
- 7.Anderson M C, Adams B D. Total wrist arthroplasty. Hand Clin. 2005;21(4):621–630. doi: 10.1016/j.hcl.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Graham T J, Harman T W, Higgins J P. et al. Rheumatoid wrist arthrodesis using plate fixation. Atlas Hand Clin. 2005;10:289–305. [Google Scholar]
- 9.Franko O I, Zurakowski D, Day C S. Functional disability of the wrist: direct correlation with decreased wrist motion. J Hand Surg Am. 2008;33(4):485–492. doi: 10.1016/j.jhsa.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality HCUP NIS database documentation Avalable at: http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed July 18, 2014
- 11.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP). HCUP comorbidity software Available at: http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/. Accessed July 18, 2014
- 12.Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.US Census Bureau 2010 census Available at: http://www.census.gov/population/race/data/cen2010.html. Accessed July 24, 2014
- 14.Morapudi S P, Marlow W J, Withers D, Ralte P, Gabr A, Waseem M. Total wrist arthroplasty using the Universal 2 prosthesis. J Orthop Surg (Hong Kong) 2012;20(3):365–368. doi: 10.1177/230949901202000321. [DOI] [PubMed] [Google Scholar]
- 15.Herzberg G. Prospective study of a new total wrist arthroplasty: short term results. Chir Main. 2011;30(1):20–25. doi: 10.1016/j.main.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 16.Herzberg G, Boeckstyns M, Sorensen A I. et al. “Remotion” total wrist arthroplasty: preliminary results of a prospective international multicenter study of 215 cases. J Wrist Surg. 2012;1(1):17–22. doi: 10.1055/s-0032-1323642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty: midterm follow-up study. J Hand Surg Am. 2011;36(6):967–973. doi: 10.1016/j.jhsa.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 18.Boeckstyns M E, Herzberg G, Merser S. Favorable results after total wrist arthroplasty: 65 wrists in 60 patients followed for 5–9 years. Acta Orthop. 2013;84(4):415–419. doi: 10.3109/17453674.2013.823588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harlingen Dv Heesterbeek P J, J de Vos M, High rate of complications and radiographic loosening of the biaxial total wrist arthroplasty in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years Acta Orthop 2011826721–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ward C M, Kuhl T, Adams B D. Five to ten-year outcomes of the Universal total wrist arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(10):914–919. doi: 10.2106/JBJS.H.01614. [DOI] [PubMed] [Google Scholar]
- 21.Kretschmer F, Fansa H. BIAX total wrist arthroplasty: management and results after 42 patients [in German] Handchir Mikrochir Plast Chir. 2007;39(4):238–248. doi: 10.1055/s-2007-964878. [DOI] [PubMed] [Google Scholar]
- 22.Nikiphorou E, Carpenter L, Morris S. et al. Hand and foot surgery rates in rheumatoid arthritis have declined from 1986 to 2011, but large-joint replacement rates remain unchanged: results from two UK inception cohorts. Arthritis Rheumatol. 2014;66(5):1081–1089. doi: 10.1002/art.38344. [DOI] [PubMed] [Google Scholar]
- 23.Feldon P, Terrono A L, Nalebuff E A, Millender L H. Philadelphia, PA: Churchill Livingstone; 2011. Rheumatoid arthritis and other connective tissue diseases; pp. 1993–2065. [Google Scholar]
- 24.Yeoh D, Tourret L. Total wrist arthroplasty: a systematic review of the evidence from the last 5 years. J Hand Surg Eur Vol. 2015;40(5):458–468. doi: 10.1177/1753193414539796. [DOI] [PubMed] [Google Scholar]
- 25.Krukhaug Y, Lie S A, Havelin L I, Furnes O, Hove L M. Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop. 2011;82(4):405–409. doi: 10.3109/17453674.2011.588858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiss A P, Kamal R N, Shultz P. Total wrist arthroplasty. J Am Acad Orthop Surg. 2013;21(3):140–148. doi: 10.5435/JAAOS-21-03-140. [DOI] [PubMed] [Google Scholar]


