CLINICAL INTRODUCTION
A 59-year-old woman with hypertension presented with right-sided weakness and vision loss. Her vital signs were normal; cardiopulmonary exam was significant for a systolic and diastolic murmur. MRI of the brain showed multiple chronic bilateral infarctions, and Doppler ultrasound revealed acute left lower extremity deep vein thrombosis. Transthoracic echocardiography (TTE) to determine cardioembolic source of stroke was significant only for severe aortic valve regurgitation. To assess for cardiac vegetations, transoesophageal echocardiography (TEE) was performed (figure 1). Thrombophilic workup revealed positive antinuclear antibody (titre 1:640) and lupus anticoagulant; the remaining lupus serologies were negative. She was afebrile, without leukocytosis or positive blood cultures. During evaluation for vaginal bleeding 5 days later, she was diagnosed with stage IIIB endometrial carcinoma.
Figure 1.
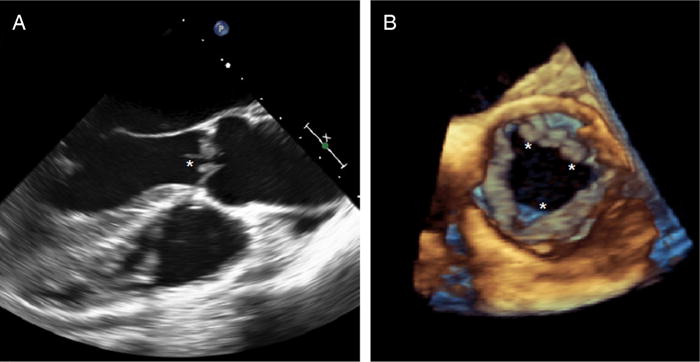
Transoesophageal echocardiogram (TEE) revealing multiple densities (*) attached to the ventricular surface of the aortic valve, seen in 2D TEE (long-axis view, A) and 3D TEE (short-axis view, B).
CLINICAL QUESTION
What is the most likely diagnosis?
Papillary fibroelastoma
Infective endocarditis
Non-bacterial thrombotic endocarditis (NBTE)
Lambl’s excrescences
Valvular calcification
ANSWER: C
NBTE is identified in 1.6% of autopsy cases and is associated with prothrombotic conditions, including malignancy and systemic lupus erythematosus.1 Patients commonly present with signs and symptoms related to recurrent embolism.2 NBTE is thought to result from endothelial damage caused by circulating cytokines during a hypercoagulable state.3 Aortic and mitral valves are most commonly affected, with vegetations consisting of sterile fibrin and platelet-rich thrombi.4 Treatment entails systemic anticoagulation and targeted therapy for the underlying aetiology; surgery is typically reserved for cardiac complications.
The patient was given intravenous heparin, and she underwent aortic valve repair with leaflet debridement for recurrent strokes and severe aortic regurgitation a week later. Intraoperative TEE and 1-month postoperative TTE showed residual trace of aortic regurgitation. Surgical pathology of the vegetation revealed fibrin, platelets and interspersed mononuclear cells, consistent with marantic aetiology (see online supplementary figures S1 and S2). Her NBTE was attributed to a prothrombotic state from malignancy and lupus anticoagulant. Figure 1 demonstrated aortic valve thickening with multiple large nodular echodensities, without thin stalk attachments commonly present in papillary fibroelastomas and without bright echogenicity characteristic of valvular calcification. Lambl’s excrescences appear as thin strands. Infective endocarditis was not present, as cultures were negative.
She has not had further recurrences since receiving chemotherapy and warfarin. Although heparin anticoagulants are recommended for treatment of NBTE and malignancy-related deep vein thrombosis (DVT) by the American College of Chest Physicians, warfarin was chosen due to postoperative bleeding risk and patient preference.5 Six-month follow-up of TTE showed mildly thickened aortic valve leaflets and mild aortic insufficiency, but no vegetations.
Footnotes
Contributors OE wrote the manuscript. JW edited and revised the manuscript and provided the images. RS edited and revised the manuscript.
Competing interests None.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/heartjnl-2014-306723).
References
- 1.Asopa S, Patel A, Khan OA, et al. Non-bacterial thrombotic endocarditis. Eur J Cardiothorac Surg. 2007;32:696–701. doi: 10.1016/j.ejcts.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 2.Dutta T, Karas MG, Segal AZ, et al. Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia. Am J Cardiol. 2006;97:894–8. doi: 10.1016/j.amjcard.2005.09.140. [DOI] [PubMed] [Google Scholar]
- 3.el-Shami K, Griffiths E, Streiff M. Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. Oncologist. 2007;12:518–23. doi: 10.1634/theoncologist.12-5-518. [DOI] [PubMed] [Google Scholar]
- 4.Steiner I. Nonbacterial thrombotic endocarditis—a study of 171 case reports. Cesk Patol. 1993;29:58–60. [PubMed] [Google Scholar]
- 5.Whitlock RP, Sun JC, Fremes SE, et al. Antithrombotic and thrombolytic therapy for valvular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e576S. doi: 10.1378/chest.11-2305. [DOI] [PMC free article] [PubMed] [Google Scholar]


