Abstract
Background
Prior studies have identified age as a factor in determining an individual’s likelihood of receiving a prosthesis following a lower limb amputation. These studies are limited to specific subsets of the general population and are unable to account for pre-amputation characteristics within their study populations. Our study seeks to determine the effect of pre-amputation characteristics on the probability of receiving a prosthesis for the general population in the United States.
Objective
Identify pre-amputation characteristics that predict of the likelihood of receiving a prosthesis following an above-knee amputation (AKA).
Design
A retrospective, population-based cohort study.
Setting
Olmsted County, Minnesota (2010 population: 144,248)
Participants
Individuals (n=93) over the age of 18 years who underwent an AKA i.e. knee disarticulation or trans-femoral amputation while residing in Olmsted County, MN between 1987 and 2013.
Methods
Characteristics affecting the receipt of a prosthesis were analyzed using a logistic regression and a random forest algorithm for classification trees. Pre-amputation characteristics include age, sex, amputation etiology, year of amputation, mobility, cognitive ability, comorbidities, and time between surgery and the prosthesis decision.
Main Outcome Measures
The association of pre-amputation characteristics with the receipt of a prosthesis following an AKA.
Results
Twenty Four of the participants received a prosthesis. The odds of receiving a prosthesis were almost 30 times higher in those able to walk independently prior to an amputation relative to those who could not walk independently. A 10-year increase in age was associated with a 53.8% decrease in the likelihood of being fit for a prosthesis (odds ratio=0.462, p-value =.030). Time elapsed between surgery and the prosthesis decision was associated with a rise in probability of receiving a prosthesis for the first three months in the random forest algorithm. No other observed characteristics were associated with receipt of a prosthesis.
Conclusions
The association of pre-amputation mobility and age with the likelihood of being fit for a prosthesis is well-understood. The effect of age, after controlling for confounders, still persists and is associated with the likelihood of being fit for a prosthesis.
Keywords: Prosthesis, amputation, logistic regression, machine learning, predictive models
INTRODUCTION
Above-knee amputations can result from the progression of dysvascular conditions (e.g. diabetes or peripheral vascular disease) or a non-vascular event (e.g., trauma or cancer). Following an above-knee amputation, an individual’s suitability for a prosthesis is typically determined using post-amputation assessments based on mobility and balance measures of the individual without a prosthesis 1. The nature of these assessments does not allow for these evaluations to be reliably administered prior to the amputation. Additionally, amputation etiology, age at amputation, and comorbidities are often correlated with one another and therefore, it is necessary to control for each of these factors in analysis looking at pre-amputation characteristics and their effects on the probability of receiving prosthesis.
Individuals with amputations who had more comorbidities are less likely to receive a high Medicare Functional Classification Level, which is directly related to an individual’s eligibility for a prosthesis and prosthesis type 1. Age, often associated with more comorbidities, has been previously shown to affect an individual’s likelihood of receiving a prosthesis. Within the elderly US Veteran population, being 75 years old or younger increased a veteran’s likelihood of receiving a prosthesis within the first year following a lower-limb amputation by almost 5 times compared to those veterans over the age of 85 2. Additionally, veterans with peripheral vascular disease are less likely to receive a prosthetic prescription. Outcomes following lower limb amputations for the entire population of the Marshall Islands offer more generalizable results as compared to looking only at outcomes within the US Veteran population. In the Marshall Islands – where all of the amputations in a single year were of dysvascular etiology – a third of patients received a prosthesis, though none of the patients with transfemoral amputations used their prosthesis for ambulation after being discharged from rehabilitation 3.
Following an amputation, an individual’s mobility and function are reduced, but receiving a prosthesis can be an important factor in improving mobility and overall quality of life 4. Physical activity is important in the maintenance of overall health; increased physical activity is linked with reduced risks for early death, diabetes mellitus, coronary heart disease, high blood pressure, strokes, and depression along with other negative health factors 5. Individuals with lower-limb amputations are at a higher risk of developing coronary artery disease, though this varies by amputation etiology with dysvascular individuals having a greater risk 6. Mortality rates among individuals with dysvascular amputations are linked to coronary artery disease, diabetes, and renal failure with CAD increasing the risk of mortality by more than three times 7.
Identifying characteristics associated with the likelihood of receiving a prosthesis could be used in a pre-amputation assessment to determine an individual’s likelihood of receiving a prosthesis following an amputation. It is also important that the predictors of prosthetic prescription match the factors used in a clinical assessment to determine an individual’s eligibility for a prosthesis. We sought to identify pre-amputation characteristics that are predictive of the probability of receiving a prosthesis following an above-knee amputation i.e. trans-femoral amputation or knee-disarticulation and compare these predictors to those commonly used by clinicians. It is likely that older individuals, those with amputations of dysvascular etiology, and those with reduced mobility prior to the amputation have a lower probability of receiving a prosthesis.
METHODS
Data Source and Study Population
Individuals with above-knee amputations residing in XXXXX, XX were identified using the resources available through the XXXXX (XXX; NIH XXXXX). The XXXXX was designed to take advantage of the unique circumstances within XXXXX: being relatively isolated from other urban areas and having only a few healthcare providers (including XXXXX, XXXXX and their affiliated hospitals) that all agreed to share medical records and administrative data 8.
It should be noted that the XXXXX population is quite similar to the XXXXX population but is less diverse, wealthier, and more educated than the general US population, yet results from other studies using this population are applicable to populations outside the XXXXX 9.
Using the resources of the XXX, we identified individuals who underwent an above-knee amputation procedure as a resident of XXXXX from 1987 to 2013 (n=93). These individuals were initially identified using the ICD-9-CM procedure code of 84.17. Medical records for these individuals were reviewed to confirm their amputation status and level. Demographics; amputation etiology; year of amputation; pre-amputation mobility level; cognitive ability – limited to the presence or absence of dementia, Alzheimer’s, or psychiatric disorders; pre-amputation comorbidities; and receipt of a prosthesis following the above-knee amputation were also recorded. Patients who had denied research authorization for use of their medical records in research were excluded. This study was approved by both the XXXXX and XXXXX Institutional Review Boards.
Outcomes Measured
A review of the individual’s medical record was used to: 1) classify the etiology of the amputation (unknown, diabetes mellitus type I, diabetes mellitus type II, peripheral vascular disease, trauma, or cancer) along with 2) the side of the limb amputated 3) if the individual had a bilateral amputation 4) the pre-amputation mobility level (wheelchair dependent, walking with an assistive device, or walking independently) 5) pre-amputation living situation (residing in a nursing home or in the community to include assisted living facilities) and 6) pre-amputation cognitive ability (presence or absence of dementia, Alzheimer’s, or psychiatric disorders) with full cognitive ability defined as the absence of a diagnosis of dementia, Alzheimer’s, or a psychiatric disorder in the medical records. The level of amputation i.e. knee disarticulation or transfemoral amputation, was verified by surgical reports from the amputation procedure. All individuals with a verified above-knee amputation were included; the ability view the entire medical records ensured that all pre-amputation characteristics were recorded for each individual. Individuals were also classified as unilateral or bilateral amputees. The outcome of interest was whether an individual was fitted for and provided a prosthesis following an above-knee amputation. An individual was defined as having received a prosthesis if a provisional or final prosthesis was fit and this was recorded in the medical records. No attempt was made to determine whether or not this individual continued to use the prosthesis after receiving it. Comorbidities were extracted from administrative data and classified using modified Charlson comorbidities via the icd9 package in R 10,11.
Statistical Analysis
Descriptive statistics, multivariate logistic regressions, and a random forest algorithm for classification trees were used to look at associations between pre-amputation characteristics and the receipt of a prosthesis. All of the pre-amputation characteristics, besides age at amputation and year of amputation, were treated as categorical variables. Following the initial analysis, year of amputation was divided into three, five, and ten-year-groups starting at 1987; the last year-group always ended in 2013 and could be shorter than the rest of the year-groups depending on the interval covered. This was done to ensure there were sufficient observations in each year-group category. Characteristics were compared across the two outcome categories using a two-sided two-sample t test. Differences throughout all of the analysis were considered statistically significant at p <.05.
The logistic regression is useful for examining outcomes that are not linear in nature, especially dichotomous outcomes like the receipt of a prosthetic prescription. Finding predictors that perform well outside our data is also important; therefore we explored the results generated by a random forest algorithm for classification trees. The random forest algorithm uses a subsampling methodology to create many predictive models using a classification tree framework from a single dataset and therefore performs well when making predictions 12,13. The random forest algorithm’s predictive power is informative in other musculoskeletal applications looking at clinical outcomes that are classification problems 14.
All of the statistical analysis was conducted using R version 3.1.2 15. Multivariate logistic regressions were run using the glm package and the random forest algorithm used RandomForestSRC, and the ggRandomForests for random forest algorithm graphics 16–18.
RESULTS
The study population comprised 93 XXXXX residents who had above-knee amputations between 1987 and 2013. An additional 63 individuals with above-knee amputations were residing in XXXXX during this period but had amputations performed before adulthood or while not residing in XXXXX (i.e. prevalent cases). Prosthetic fittings were provided to 24 of the 93 incident individuals within an average of 105 days following the amputation (median of 78 days, IQR = 56–155 days). Individuals not receiving a prosthesis were notified within an average of 35 days following the amputation (median of 1 days, IQR = 0 – 7 days, the decision for one individual took 665 days). As illustrated in Table 1, patients who received a prosthesis were, on average, almost 20 years younger than those not receiving a prosthesis (59±20 years vs 78±11 years). A smaller percentage of dysvascular patients received a prosthesis compared to those who did not receive a prosthesis (71% vs 96%). Wheelchair dependent and those using assistive devices such as walkers or canes prior to the amputation had a lower rate of receiving a prosthesis (4% vs 55% and 17% vs 33%). A higher percentage of those able to walk independently prior to the amputation received a prosthesis (79% vs 12%). A similar trend was seen in those who had full cognitive abilities prior to the amputation (96% vs 74%). No other characteristics appeared to differ between those who did and did not receive a prosthetic prescription.
Table 1.
Population characteristics by prosthesis status following an above-knee amputation
| Characteristics | Received a Prosthesis | p-value | |
|---|---|---|---|
| Yes (n=24) | No (n=69) | ||
| Mean Age | 59 ± 20 | 78 ± 11 | <.001* |
| Female | 16 (67) | 34 (49) | .140 |
| Race, white | 22 (92) | 66 (96) | .530 |
| Bilateral amputation | 4 (17) | 19 (28) | .257 |
| Left side amputation | 8 (33) | 35 (51) | .140 |
| Dysvascular | 17 (71) | 66 (96) | .018* |
| Community dweller | 21 (88) | 33 (48) | <.001* |
| Full cognitive ability | 23 (96) | 51 (74) | .002* |
| Mobility | |||
| Wheelchair dependent | 1 (4) | 38 (55) | <.001* |
| Used assistive device | 4 (17) | 23 (33) | .090* |
| Independent walker | 19 (79) | 8 (12) | <.001* |
| Comorbidities | |||
| Congestive Heart Failure | 11 (46) | 41 (59) | .263 |
| Renal disease | 7 (29) | 28 (41) | .314 |
| Cerebrovascular disease | 10 (42) | 43 (62) | .089 |
| Rheumatic disease | 1 (4) | 9 (13) | .133 |
statistically significant
Reasons for not providing an individual with a prosthetic prescription as recorded by the physicians were extracted during the chart review. The most frequently cited reason was “mobility” (Table 2). Death as reason for not receiving a prosthesis occurred in about 10% of the population; amputation procedures carry with them a high risk of mortality. Age was not mentioned in any of the comments.
Table 2.
Most frequent qualitative reasons for not prescribing a prosthesis
| Reason | Count (N=69*) |
|---|---|
| Mobility | 21 |
| Death | 10 |
| Comorbidities | 7 |
| Mental status | 7 |
| Frail or weak | 4 |
20 individuals had other or no documentation for not receiving a prosthesis
Results from the logistic regressions and random forest algorithm were consistent (Table 3). Note that the random forest results are not regression coefficients, but rather measures of relative importance of each variable, i.e. the variable’s ability to correctly predict the receipt of a prosthesis within the study population. Overall, the fit of the logistic regression was sufficient with a c statistic of 0.939 (0.885–0.993).
Table 3.
Logistic Regression and Random Forest Algorithm results: characteristics associated with receiving a prosthesis
| Logistic Regression§ | Random Forest Algorithm | ||
|---|---|---|---|
| Odds Ratio | 95% CI | Relative Influence† | |
| Amputation Age (in decades) | 0.46* | (0.21 – 0.89) | 18.1 |
| Bilateral amputation | 0.61 | (0.08 – 4.15) | 1.4 |
| Time to Prosthesis Decision (fraction of a year) | 3.07 | (0.33 – 27.74) | 100.0 |
| Sex | 0.0 | ||
| Female | 1.21 | (0.2 – 8.08) | -- |
| Etiology | 3.6 | ||
| Dysvascular | 0.50 | (0.01 – 27) | -- |
| Race | 0.0 | ||
| White | 1.56 | (0.02 – 49.89) | -- |
| Amputation Side | 3.2 | ||
| Left | 0.34 | (0.05 – 1.95) | |
| Year of Amputation | 0.0 | ||
| Between 1997 and 2007 | 0.55 | (0.07 – 3.92) | -- |
| After 2007 | 0.82 | (0.06 – 14.49) | -- |
| Community dweller | 0.22 | (0.01 – 3.08) | 6.2 |
| Full cognitive ability | 61.27 | (1.57 – 12096.64) | 3.0 |
| Mobility | 40.0 | ||
| Walking prior to amputation | 29.62** | (3.51 – 748.67) | -- |
| Comorbidities | |||
| Congestive Heart Failure | 2.53 | (0.4 – 20.37) | 1.4 |
| Renal disease | 0.96 | (0.16 – 5.52) | 0.0 |
| Cerebrovascular disease | 0.38 | (0.05 – 2.2) | 2.1 |
| Rheumatic disease | 0.48 | (0.01 – 11.3) | 0.0 |
Only the specification of the model with 10 year-groups is presented. Other year-group specification did not change the effect of amputation year
The variables with the most predictive power are set to 100 with all others scaled relative for these variables
p-value <.05,
p-value <.01,
p-value <.001
NB: Confidence intervals were calculated using the profile likelihood method which relaxes the assumption that estimators are normally distributed. The method was particularly relevant given our smaller sample size. Statistical significance was calculated using p-values derived from the untransformed logistic regression, which used Wald-type estimates. Profile likelihood derived confidence intervals are presented and may not include 1, but are still associated with a parameter that is not statistically significant.
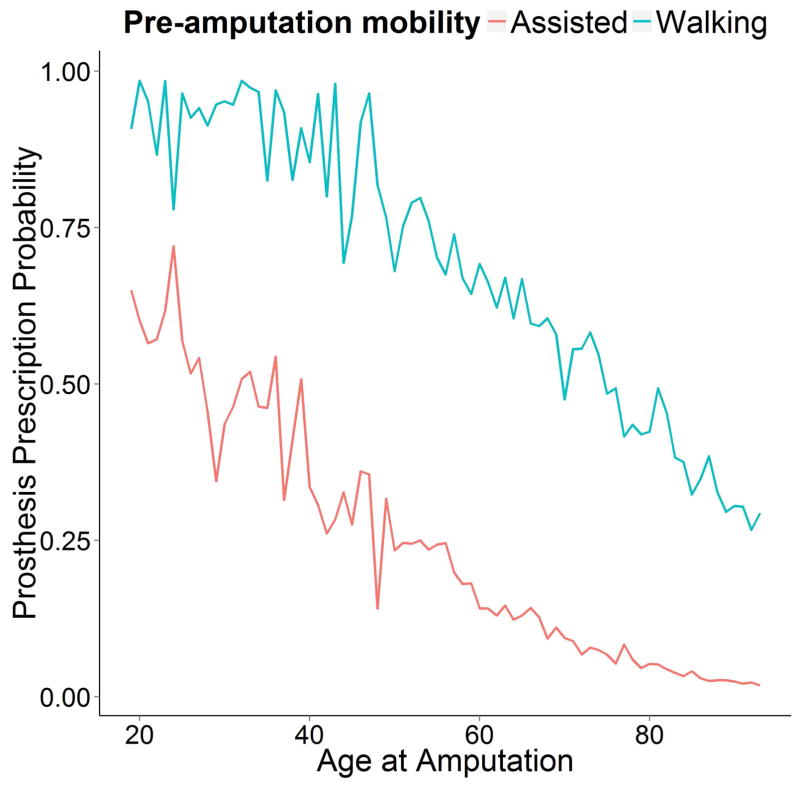
Age and walking prior to an amputation were associated with the likelihood of receiving a prosthetic prescription. Every 10 years of aging was associated with a 53.8% decrease in the probability of receipt of a prosthetic prescription. The odds of receiving a prosthesis for those who were able to walk independently prior to an amputation were almost 30 times higher than those not able to walk independently prior to an amputation (Corrected Relative Risk =9.35, implying a pre-amputation walker was 9.35 times more likely to receive a prosthesis) 19. Figure 1 illustrates the different rates of prosthesis prescription based on pre-amputation mobility; the decline in probability with age is present across both groups.
Figure 1.
Probability of receiving a prosthesis by age and pre-amputation mobility status
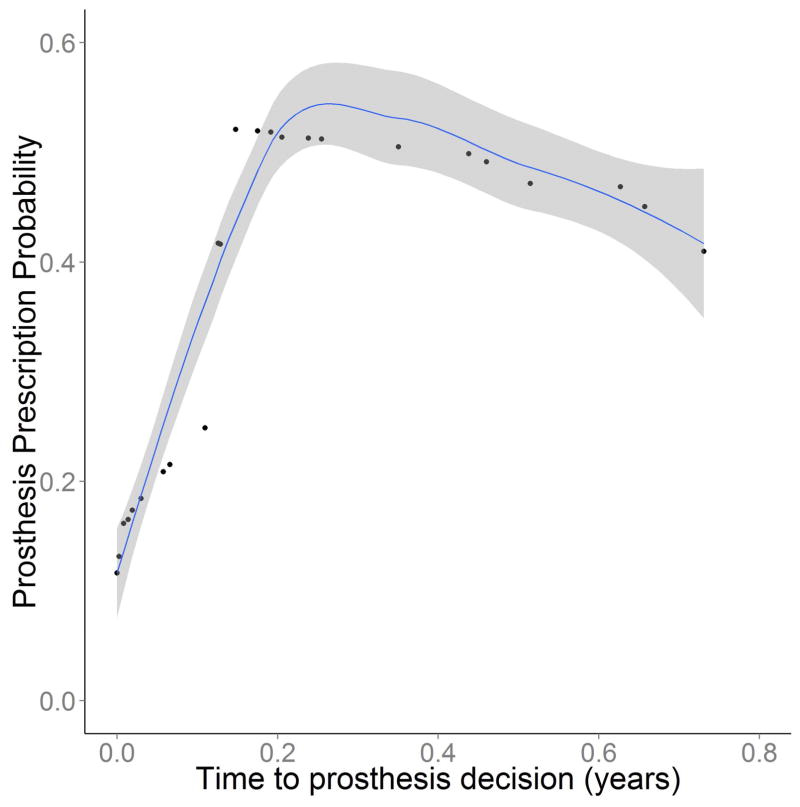
The random forest algorithm also reported that age and mobility were meaningful predictors of receiving a prosthesis along with the time elapsed from the amputation until the decision to provide or not provide a prosthesis was made. The relative influence, the average increased misclassification rate of prosthetic receipt status for a given variable with random variation added to each observation of that variable, illustrated that time until the prosthesis decision was the most important predictor in the random forest algorithm. Simulated probabilities from the random forest algorithm illustrate that an individual’s probability of receiving a prosthesis increased for the first 3 months and then slowly declined (Figure 2).
Figure 2.
Probability of receiving a prosthesis as a function of time elapsed after the amputation until prosthesis decision with 95% CI regions shaded
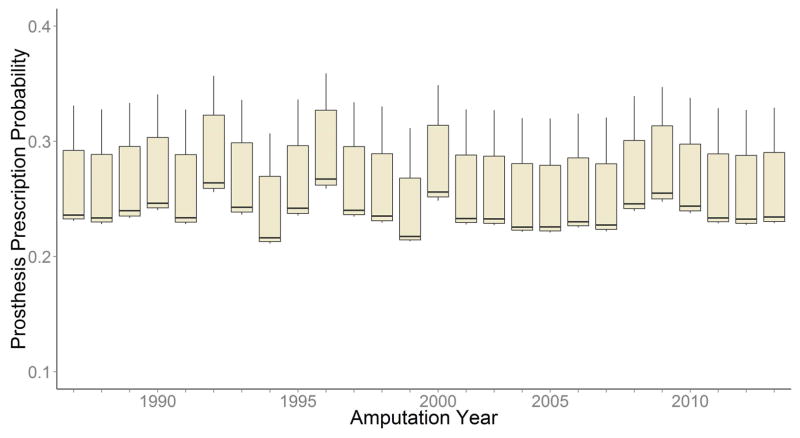
An individual’s pre-amputation living situation, cerebrovascular disease status, cognitive ability, amputation side, and amputation etiology offered minimal predictive power in classifying the prosthesis prescription decision. In the random forest, the year that the amputation occurred has minimal influence on predicting the prosthesis prescription decision; there was a lack of any trend over time (Figure 3).
Figure 3.
Prosthetic prescription probability by year from the random forest algorithm. The boxes cover the IQR, whiskers extend 1.5(IQR) beyond the IQR
Etiology was not associated with any change in the likelihood of receiving a prosthesis (p=.729) and offered little improvement in classifying outcomes in the random forest algorithm (relative influence =3.6). Sex and race had no association with the likelihood of receiving a prosthetic prescription (p=.839 & p=.955) within the logistic regression. Additionally, neither characteristic provided any additional information for properly classifying the prosthetic prescription outcome in the random forest algorithm (relative influences of 0.0 for both sex and race). None of the comorbidities in the logit regression model were associated with the probability of receiving a prosthesis (p-values ranged from .294 to .961).
DISCUSSION
During the period of the study – 1987 to 2013 – XXXXX was (and still is) served by a single amputee clinic whose individual physicians have each served for over 20 years. Over 95% of XXXXX residents with above-knee amputations were seen XXXXX. While formal clinical algorithms are not employed to assist in prosthetic eligibility, the small physician staff, similar training in amputee care, and close working relationships with the local prosthetic laboratories have de facto led to common guiding principles and approach to prosthetic eligibility and selection. It is important to note that the clinical outcomes of this de facto standardized approach to prosthetic prescriptions were not analyzed in this study; it could be the case that prescriptions were not provided to everyone that would have benefited from them.
From 1987 to 2013, about a quarter (26%) of the individuals in XXXXX undergoing an above-knee amputation received a prosthesis. This rate is similar to those found in other studies of individuals with above-knee amputations 20–22. Relatively few of the pre-amputation characteristics of individuals who underwent above-knee amputations in XXXXX between 1987 and 2013 appear to be predictive of receiving a prosthesis. The effect of being able to walk independently prior to the amputation was the strongest predictor of receiving a prosthesis. A decision to not provide a prosthesis to an individual with limited pre-amputation mobility is likely based on correlation between poor pre-amputation mobility and decreased use of a prosthesis in individuals with above-knee amputees who were prescribed a prosthesis 23,24. The age effect was also present and similar to previous studies of elderly US military veterans where a 10-year age difference translated into a 78% decrease in the likelihood of receiving a prosthesis 2. The age effect among veterans is about 25% greater than the effect found in XXXXX (62.8% decrease for every 10-year age difference). The age range in our population includes younger individuals which may mute the age effect, though none of the models indicated that there was any non-linearity in the age-receipt of a prosthesis relationship. Previous research, based on expert opinion consensus, indicates that age, alone, is not a significant factor in the decision to prescribe a prosthesis but should be considered in the context of declining functional ability 25. Our results suggest that age, independent of other factors, influences the providers’ decision of whether or not to prescribe a prosthesis following an above-knee amputation. Clinicians and patients should weigh the risks of a primary amputation versus a revascularization procedure with a high likelihood of subsequent amputation given the fact that a patient will be older in the second scenario than if they had initially undergone an amputation.
The time elapsed between the amputation and the prosthesis decision was not associated with the receipt of a prosthesis in the logit model, but was the most influential variable in the random forest algorithm. Previous research found that the longer the time between amputation and rehabilitation led to poor outcomes, but a quicker prosthesis decision was associated with a lower likelihood of receiving a prosthesis in our study 23. This time measure likely acted as a proxy for stump healing and general recovery times for the patient; the rise in probability over the first three months reflected an immediate decision by the clinician to not provide a prosthesis or a “wait and see” position until the stump healed.
Both sex and race have been associated with high rates of amputations in previous studies. Female patients are 1.4 times more likely to undergo a transfemoral amputation and non-white patients are at least 2 times as likely to undergo an amputation of dysvascular etiology; data on the relative likelihood of receiving a prosthesis was not reported for either group 26. In XXXXX, the probability of receiving a prosthesis following an above knee amputation did not vary by sex or race, although XXXXX is considerably more homogenous than the general population so the lack of racial disparities in prosthetic prescriptions might not be generalizable to the US population 9. While calendar year initially appeared to be associated with prosthetic prescriptions, we did not observe noticeable trend over time which is consistent with the steady rate of successful prosthetic fittings in the geriatric population within XXXXX from 1956 to 1995 22.
Our statistical methodology may have potential limitations. Logistic regressions are used widely in medicine to predict clinical outcomes of dichotomous outcomes related to diseases and have been specifically applied to musculoskeletal disorders; yet it is not without its shortfalls 27–29. Odds ratios are not intuitive and fitting a model on an entire sample or population can result in overfitting that will reduce the model’s ability to provide predictions for future cases. To address the issue of odds ratio interpretably, we created predicted probability curves for variables of interest to see how the probability of receiving a prosthesis changed with age by variables of interest 30. The issue of overfitting is not unique to the logistic regression model, but to any model fit on an entire data set. We addressed overfitting by using a machine learning method, the random forest algorithm. The machine learning methods used subsets of our data to create various model specifications with a goal of finding predictors that worked outside of our data set 31. For our population, the qualitative results from both approaches were mostly similar suggesting that a logistic regression may provide good predictability for most applications looking at clinical outcomes where there are relatively few observations and possible covariates. Yet results from the random forest algorithm helped illustrate the non-linear association between time elapsed between the amputation and the prosthesis decision.
Despite the population-based design, inclusion of patients irrespective of insurance status, and collecting data from medical records, findings should be interpreted in light of potential limitations. Age and prior mobility seem to have strong effects on receiving a prosthesis, it could be that other clinicians account for other factors associated with age through different clinical protocols that would negate the age effect we found. The data gathered relied solely on medical records which can be prone to error or inconsistencies across healthcare providers. One limitation of the data collected from the medical records is that the diagnosis of mild dementia may not be recorded (along with other cognitive impairments beyond dementia, Alzheimer’s, or psychiatric disorders). If these measures of cognitive ability deficits are not reported but are used as factors in the prosthetic prescription decision then we have underestimated the effect of having full cognitive ability on the probability of receiving a prosthesis. Other observable factors such as strength that were not recorded in the medical records most certainly factor into the decision on whether or not an individual is a candidate for a prosthesis following an above-knee amputation. Generalizing these results beyond the XXXXX should be done with caution due to the homogeneity of the XXXXX population and the limited power to observe race effects within the study population, where 95% of individuals with above-knee amputations were white. Future research should look at sex and race disparities related to prosthetic prescriptions along with improving mobility for elderly adults with above-knee amputations through improved prostheses or other assistive devices, as well as pre-amputation interventions to improve mobility.
CONCLUSIONS
The likelihood of receiving a prosthesis did not change over the 26-year period in XXXXX even though there has been an overall decrease in amputation rates over a similar time period 22. Etiology, sex, and race were not associated with prosthetic prescriptions, though the lack of racial disparities could be due to the relative homogeneity of the study population. Older individuals were less likely to receive a prosthesis in this study population.
As the US population continues to age, more individuals will undergo above-knee amputations later in life. While preventing an amputation is the best way to avoid not receiving a prosthesis, it is important to standardize the prosthetic prescription process. If prosthetic provision is to be standardized, resulting in more predictable eligibility, more studies are necessary to characterize those clinical factors found to be associated with better quality of life for prosthesis users.
Footnotes
The authors declare that they have no conflicts of interest concerning this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gailey RS, Roach KE, Applegate EB, et al. The Amputee Mobility Predictor: An instrument to assess determinants of the lower-limb amputee’s ability to ambulate. Archives of Physical Medicine and Rehabilitation. 2002;83:613–27. doi: 10.1053/apmr.2002.32309. [DOI] [PubMed] [Google Scholar]
- 2.Kurichi JE, Kwong PL, Reker DM, Bates BE, Marshall CR, Stineman MG. Clinical factors associated with prescription of a prosthetic limb in elderly veterans. Journal of the American Geriatrics Society. 2007;55:900–6. doi: 10.1111/j.1532-5415.2007.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harding K. Major lower limb amputations in the Marshall Islands: incidence, prosthetic prescription, and prosthetic use after 6–18 months. Pacific Health Dialogue. 2005;12:59–66. [PubMed] [Google Scholar]
- 4.Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthetics and Orthotics International. 2011;35:90–6. doi: 10.1177/0309364610397087. [DOI] [PubMed] [Google Scholar]
- 5.2008 Physical Activity Guidelines for Americans. Washington, D.C: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 6.Nallegowda M, Lee E, Brandstater M, Kartono AB, Kumar G, Foster GP. Amputation and Cardiac Comorbidity: Analysis of Severity of Cardiac Risk. Physical Medicine & Rehabilitation. 2012;4:657–66. doi: 10.1016/j.pmrj.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Chin JWS, Teague L, McLaren A-M, Mahoney JL. Non traumatic lower extremity amputations in younger patients: an 11-year retrospective study. International Wound Journal. 2013;10:73–8. doi: 10.1111/j.1742-481X.2012.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocca WA, Yawn BP, StSauver JL, Grossardt BR, Melton LJ. History of the Rochester Epidemiology Project: Half a Century of Medical Records Linkage in a US Population. Mayo Clinic Proceedings. 2012;87:1202–13. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.StSauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, III, Rocca WA. Generalizability of Epidemiological Findings and Public Health Decisions: An Illustration From the Rochester . Epidemiology Project Mayo Clinic Proceedings. 2012;87:151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 11.Wasey JO. icd9: Tools for Working with ICD-9 Codes, and Finding Comorbidities. 2015. [Google Scholar]
- 12.Schonlau M. Boosted regression (boosting): An introductory tutorial and a Stata plugin. The Stata Journal. 2005;5:330–54. [Google Scholar]
- 13.Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning. Springer; 2009. [Google Scholar]
- 14.Schwartz MH, Rozumalski A, Truong W, Novacheck TF. Predicting the outcome of intramuscular psoas lengthening in children with cerebral palsy using preoperative gait data and the random forest algorithm. Gait & Posture. 2013;37:473–9. doi: 10.1016/j.gaitpost.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. 3.1.2 ed. [Google Scholar]
- 16.Ridgeway G. R package version. 2013. gbm: Generalized Boosted Regression Models. 2.1. [Google Scholar]
- 17.Ishwaran H, Kogalur UB. R package version. 2015. Random Forests for Survival, Regression and Classification (RF-SRC) 1.6.1 ed. [Google Scholar]
- 18.Ehrlinger J. R package version. 2015. ggRandomForests: Graphical Exploration of Random Forests. 1.1.3 ed. [Google Scholar]
- 19.Zhang J, Yu KF. What's the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes. Journal of the American Medical Association. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 20.Webster JB, Hakimi KN, Williams RM, Turner AP, Norvell DC, Czerniecki JM. Prosthetic fitting, use, and satisfaction following lower-limb amputation: a prospective study. Journal of Rehabilitation Research and Development. 2012;49:1493–504. doi: 10.1682/jrrd.2012.01.0001. [DOI] [PubMed] [Google Scholar]
- 21.Nehler MR, Coll JR, Hiatt WR, et al. Functional outcome in a contemporary series of major lower extremity amputations. Journal of Vascular Surgery. 2003;38:7–14. doi: 10.1016/s0741-5214(03)00092-2. [DOI] [PubMed] [Google Scholar]
- 22.Fletcher DD, Andrews KL, Hallett JW, Jr, Butters MA, Rowland CM, Jacobsen SJ. Trends in rehabilitation after amputation for geriatric patients with vascular disease: implications for future health resource allocation. Archives of Physical Medicine and Rehabilitation. 2002;83:1389–93. doi: 10.1053/apmr.2002.34605. [DOI] [PubMed] [Google Scholar]
- 23.Sansam K, Neumann V, O’Connor R, Bhakta B. Predicting walking ability following lower limb amputation: a systematic review of the literature. Journal of Rehabilitation Medicine. 2009;41:593–603. doi: 10.2340/16501977-0393. [DOI] [PubMed] [Google Scholar]
- 24.van Eijk MS, van der Linde H, Buijck B, Geurts A, Zuidema S, Koopmans R. Predicting prosthetic use in elderly patients after major lower limb amputation. Prosthetics and Orthotics International. 2012;36:45–52. doi: 10.1177/0309364611430885. [DOI] [PubMed] [Google Scholar]
- 25.Schaffalitzky E, Gallagher P, Maclachlan M, Wegener ST. Developing consensus on important factors associated with lower limb prosthetic prescription and use. Disability Rehabilitation. 2012;34:2085–94. doi: 10.3109/09638288.2012.671885. [DOI] [PubMed] [Google Scholar]
- 26.Sheehan TP, Gondo GC. Impact of Limb Loss in the United States. Physical Medicine and Rehabilitation Clinics of North America. 2014;25:9–28. doi: 10.1016/j.pmr.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 27.Rozbruch SR, Zonshayn S, Muthusamy S, Borst EW, Fragomen AT, Nguyen JT. What risk factors predict usage of gastrocsoleus recession during tibial lengthening? Clinical Orthopaedics and Related Research. 2014;472:3842–51. doi: 10.1007/s11999-014-3526-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Solomon DH, Avorn J, Warsi A, et al. Which patients with knee problems are likely to benefit from nonarthroplasty surgery? Development of a clinical prediction rule Archives of Internal Medicine. 2004;164:509–13. doi: 10.1001/archinte.164.5.509. [DOI] [PubMed] [Google Scholar]
- 29.Easterlin MC, Chang DC, Wilson SE. A practical index to predict 30-day mortality after major amputation. Annals of Vascular Surgery. 2013;27:909–17. doi: 10.1016/j.avsg.2012.06.030. [DOI] [PubMed] [Google Scholar]
- 30.Bewick V, Cheek L, Ball J. Statistics review 14: Logistic regression. Critical Care. 2005;9:112–8. doi: 10.1186/cc3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varian HR. Big Data: New Tricks for Econometrics. Journal of Economic Perspectives. 2014;28:3–28. [Google Scholar]