Abstract
Objective
To compare maternal and neonatal outcomes based on length of latent phase during induction with rupture of membrane (ROM) prior to 6 cm dilation.
Methods
This is a retrospective cohort study using data from the Consortium of Safe Labor study, including 9,763 nulliparous and 8,379 multiparous women with singleton, term pregnancies undergoing induction at ≤ 2 cm dilation with ROM before 6 cm dilation, after which latent phase ended.. Outcomes were evaluated according to duration of oxytocin and ROM.
Results
At time points from 6 to 18 hours of oxytocin and ROM, the rates of nulliparous women remaining in the latent phase declined (35.9% to 1.4%) and the rates of vaginal delivery for those remaining in the latent phase at these time period decreased (54.1% to 29.9%) Nulliparous women remaining in the latent phase for 12 hours compared to women who had exited the latent phase had significantly increased rates of chorioamnionitis (12.1% versus 4.1%), endometritis (3.6% versus 1.3%); and increased rates of neonatal intensive care unit (NICU) admission (8.7% versus 6.3%). Similar patterns were present for multiparous women at 15 hours.
Conclusion
Based on when neonatal morbidity increased, in an otherwise uncomplicated induction of labor with ROM, a latent phase following initiation of oxytocin of at least 12 hours for nulliparous women and 15 hours in multiparous women are reasonable criteria for diagnosing a failed induction.
Precis
At least 12 hours of oxytocin and rupture of membranes in nulliparous and 15 hours in multiparous women is reasonable before considering an induction to have failed.
INTRODUCTION
More than 22% of pregnant women underwent induction of labor in 2013, making it one of the most commonly performed procedures in the United States.1 While the goal of induction is to achieve a vaginal delivery, the criteria of failed induction of labor is not clear. 2
The American College of Obstetricians and Gynecologists (the College) statement that “cesarean deliveries for failed induction of labor in the latent phase can be avoided by requiring that oxytocin be administered for at least 12–18 hours after membrane rupture before deeming the failed induction”3 is based on limited data from small studies.2, 4, 5 Previous studies demonstrated that 13–60% of women in the latent phase after 12 hours of oxytocin and rupture of membranes (ROM) eventually had vaginal deliveries. 2, 4, 5 However, these studies were limited by a small number of women, precluding evaluation of infrequent maternal and neonatal complications. Furthermore, data regarding maternal and neonatal complications in women remaining in the latent phase after more than 12 hours of oxytocin and ROM compared to women who exited the latent phase are limited. Determining whether an induction of labor is failed requires the balance between benefit of vaginal delivery and maternal–neonatal complications. Our study group was women undergoing induction of labor with an unfavorable cervix and ROM prior to the active phase of labor. We sought to compare maternal and neonatal outcomes between women in the latent phase and women who exited latent phase according to the duration of oxytocin.
MATERIALS AND METHODS
The Consortium on Safe Labor (CSL) was a retrospective cohort study of all women delivering at 23 weeks of gestation or greater between 2002 and 2008 in 12 clinical centers with 19 hospitals across 9 College districts.6 All participating institutions obtained Institutional Review Board (IRB) approval. IRB approval was obtained for this analysis.
The CSL included a total of 228,562 deliveries with 233,736 newborns delivered at ≥ 23 weeks of gestation after excluding 106 deliveries due to errors in identification. Data from the electronic medical record (EMR) were abstracted and mapped to predefined categories at the data coordinating center. The accuracy of data was validated for four diagnoses including cesarean delivery for non-reassuring fetal heart rate tracing, asphyxia, neonatal intensive care unit (NICU) admission due to a respiratory diagnosis, and shoulder dystocia. The variables were highly concordant with the medical records (greater than 95% for 16 out of 20 variables and greater than or equal to 91.9% for all).6 We limited the current analysis to singleton gestations with cephalic presentation at 37 weeks or greater with known ROM time (either premature, spontaneous or artificial ROM) and oxytocin initiation time who underwent induction of labor (Appendix 2, available online at http://links.lww.com/xxx). One study site did not report the time of ROM (n=4,220) and two sites did not report the time of oxytocin initiation (n=8,543). Therefore, these three sites were excluded. Women who had spontaneous labor and labor augmentation as recorded in the medical record were excluded in this study. We limited analysis to women with an unfavorable cervix defined as an initial cervical exam of 2 cm dilation or less and ROM prior to cervical dilation 6 cm, which we defined as the point at which active phase started. In our study, we did not take cervical ripening into account because the definition for failed induction3 does not take prior cervical ripening agent into account. We also excluded women with a prior uterine scar, human immune virus infection, herpes simplex virus infection, induction of labor for chorioamnionitis, antepartum stillbirth, and major congenital abnormalities as well as maternal pre-existing comorbidities such as pre-existing diabetes, heart disease, and renal disease. To avoid intrapersonal correlation, we selected the first delivery from each subject in the study. The final analysis was limited to 18,470 deliveries.
We established 3 categories of precursors for induction: indicated, elective, and no recorded indication as previously described.7 We used the indication for induction to identify the precursors for delivery and classified using the following hierarchy. First, women with premature rupture of membranes (PROM) were always classified as such. Second, we identified indicated precursors of induction including hypertensive disease (chronic hypertension, gestational hypertension, preeclampsia, and hemolysis, elevated liver enzymes, low platelet syndrome [HELLP syndrome]), postdates, fetal condition (including fetal growth restriction and abnormal antenatal testing), gestational diabetes, and abruption. More than one precursor for induction could be applicable for a given subject. Third, if a site indicated that the induction was elective without any indicated precursors of induction (including hypertensive disease, postdates, fetal condition, gestational diabetes, or abruption), the precursor for induction was designated as elective. Finally, the “no recorded indication” category encompassed all inductions without indications provided by site and with no other obstetric, fetal, or maternal conditions affecting the pregnancy.
Previous studies2, 4, 5 used the same definition (duration of oxytocin and ROM) to report outcomes of induction of labor. Therefore, we defined time zero as starting with the occurrence of both oxytocin and ROM. For example, if a woman was given oxytocin and then ROM occurred, the interval started with the time of ROM. If a woman had ROM and then oxytocin was started, the interval started with the oxytocin initiation time. According to the duration of oxytocin and ROM (6, 9, 12, 15, and 18 hours), women were assessed regarding their labor status (latent phase, active phase, delivered via vaginal delivery, delivered via cesarean delivery in latent phase, delivered via cesarean delivery in active phase). All cases reaching vaginal or cesarean delivery outcomes from each former time point accumulated to the next time point. We defined the active phase of labor to begin at ≥6 cm dilatation based on the findings from a previous study from the CSL dataset which found that the active phase of labor starts after 6 cm cervical dilation in both nulliparous and multiparous women.8 Thus, the latent phase ended when 6 cm dilation was achieved.
We evaluated eventual vaginal delivery rates of women in latent labor. We also evaluated maternal morbidity including chorioamnionitis, endometritis, and postpartum hemorrhage and neonatal morbidity including Neonatal Intensive Care Unit (NICU) admission, need for mechanical ventilation, and neonatal sepsis in women who were in latent phase compared to women who exited the latent phase (active phase or delivered) at 6, 9, 12, 15 and 18 hours of oxytocin and ROM. Precursors for induction (hypertensive disease, postdates, fetal condition, premature rupture of membranes, gestational diabetes, and abruption), NICU admission, and mechanical ventilation were solely derived from medical records. Chorioamnionitis, endometritis, and neonatal sepsis were derived from medical records and supplemented with International Classification of Diseases, Clinical Modification (ICD-9-CM) codes. Postpartum hemorrhage was defined as recorded in the medical record, and estimated blood loss greater than 500 mL for vaginal delivery and greater than 1,000 mL for cesarean delivery and supplemented with ICD-9-CM codes.
Descriptive statistics were calculated for all study variables. Chi-square test, Fisher’s exact test, or Wilcoxon rank-sum test were performed to determine associations between outcomes and latent phase. Cochran-Armitage Trend Test was used to calculate the trend of eventual vaginal delivery rates in women who remained in latent phase according to the duration of oxytocin and ROM. Multivariable logistic regression was used to calculate adjusted P-values to compare maternal and neonatal outcomes between women who remained in the latent phase and women who exited the latent phase, controlling for gestational age at delivery, race/ethnicity, body mass index (kg/m2) on admission, and hospital type. A P-value <.05 was considered significant. All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
Maternal, obstetric and neonatal characteristics are presented in Table 1. In nulliparous women, 69.5% of the inductions were indicated, 18.0% were elective, and 12.6% had no recorded indication. Hypertensive disease was the most common precursor for induction in nulliparous women (21.8%), followed by postdates (16.0%). In multiparous women, 41.3% of inductions were indicated, 45.3% were elective, and 13.4% had no recorded indication. Hypertensive disease again was the most common precursor for induction in multiparous women (10.7%).
Table 1.
Maternal, obstetric and neonatal characteristics for women with known rupture of membranes and oxytocin duration
| Nulliparous women (n=9,763) |
Multiparous women (n=8,379) |
|
|---|---|---|
| Maternal age (year) | 25.2 ±5.8 | 29.4 ±5.2 |
| Body mass index at delivery (kg/m2), | 31.4 ±6.4 | 31.2 ±6.1 |
| Race or ethnicity | ||
| Non-Hispanic white | 4,980 (51.0) | 5,526 (66.0) |
| Non-Hispanic black | 2,030 (20.8) | 1,110 (13.3) |
| Hispanic | 1,645 (16.9) | 1,112 (13.3) |
| Asian or pacific islander | 380 (3.9) | 164 (2.0) |
| Other or unknown | 728 (7.5) | 467 (5.6) |
| Insurance | ||
| Private | 5,952 (61.0) | 5,838 (69.7) |
| Public or self-pay | 3,152 (32.3) | 2,152 (25.7) |
| Other | 659 (6.8) | 389 (4.6) |
| Hospital type | ||
| University affiliated hospital | 4,181 (42.8) | 2,206 (26.3) |
| Teaching community hospital | 4,629 (47.4) | 4,083 (48.7) |
| Non-teaching community hospital | 953 (9.8) | 2,090 (24.9) |
| Pregnancy complications | ||
| Gestational diabetes | 430 (4.4) | 403 (4.8) |
| Chronic hypertension | 383 (3.9) | 271 (3.2) |
| Dilation on admission (cm) | ||
| 0 | 1,407 (14.4) | 367 (4.4) |
| 0.5 | 573 (5.9) | 191 (2.3) |
| 1 | 4,168 (42.7) | 2,647 (31.6) |
| 1.5 | 744 (7.6) | 534 (6.4) |
| 2 | 2,871 (29.4) | 4,640 (55.4) |
| Effacement on admission | 60 (20–80) | 60 (30–80) |
| Station on admission | −2 (−4 – −1) | −2 (−3 – −1) |
| Group B streptococcus infection | 2,269 (23.2) | 1,957 (23.4) |
| Precursors for induction* | ||
| Hypertensive disease† | 2,128 (21.8) | 896 (10.7) |
| Postdates | 1,559 (16.0) | 521 (6.2) |
| Fetal condition‡ | 955 (9.8) | 583 (7.0) |
| Premature rupture of the membranes | 824 (8.4) | 309 (3.7) |
| Gestational diabetes | 430 (4.4) | 403 (4.8) |
| Abruption | 52 (0.5) | 63 (0.8) |
| Other | 660 (6.8) | 618 (7.4) |
| Precursors for induction | ||
| Indicated induction | 6,780 (69.5) | 3,457 (41.3) |
| Elective induction | 1,758 (18.0) | 3,797 (45.3) |
| No recorded indication | 1,225 (12.6) | 1,125 (13.4) |
| Gestational age at delivery (week) | 39.5 ±1.2 | 39.2 ±1.0 |
| Neonatal birth weight (gram) | 3351.2 ±453.2 | 3388.8 ±432.1 |
Data shown as mean ± standard deviation, n (%), or median (10th–90th percentile).
Women could have more than one indication.
Hypertensive disease included chronic hypertension, gestational hypertension, preeclampsia, and hemolysis, elevated liver enzyme, low platelet syndrome.
Fetal condition included conditions such as intrauterine growth restriction and abnormal antenatal testing.
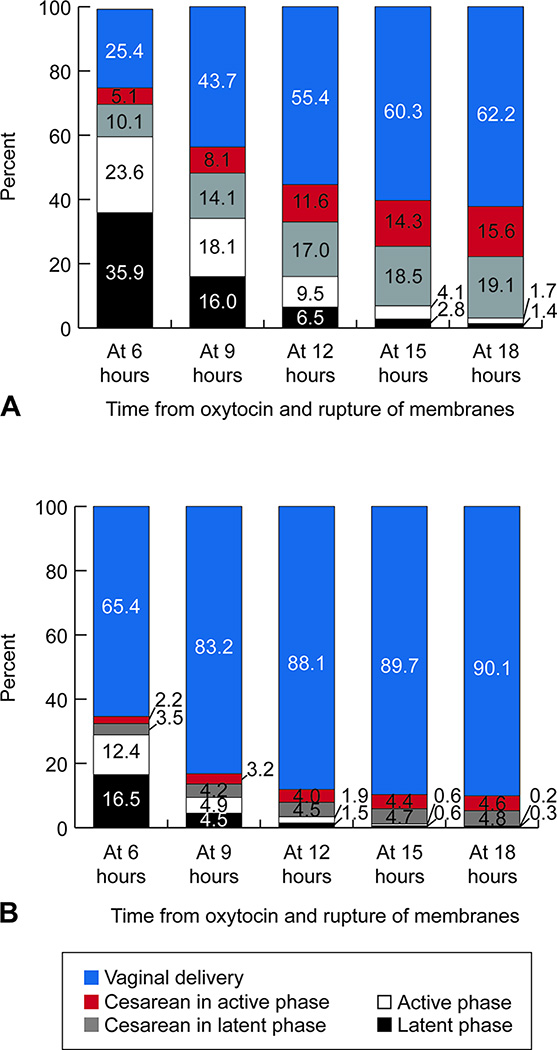
Labor status of women by duration of oxytocin and ROM is presented in Figure 1. For example, by 6 hours duration of oxytocin and ROM in nulliparous women, 25.4% had delivered vaginally, 5.1% had a cesarean delivery in the active phase, 10.1% had a cesarean delivery in the latent phase, 23.6% were in the active phase and 35.9% were in the latent phase of labor. These numbers are cumulative. For example, in nulliparous women, the rate of vaginal delivery (43.7%) at 9 hours included the vaginal delivery rate (25.4%) at 6 hours. The majority of nulliparous women (97.2%) achieved active phase or delivered after 15 hours of oxytocin and ROM. The majority of multiparous women (98.5%) achieved active phase or delivered after 12 hours of oxytocin and ROM.
Figure 1.
Labor status by time from oxytocin and rupture of membrane. A. Nulliparous women (n=9,763); B. Multiparous women (n=8,379). Latent phase was defined as ending when cervical exam 6 cm achieved. Active phase was defined as starting when 6 cm dilation achieved. For example, by 6 hours duration of oxytocin and ROM in nulliparous women, 25.4% had delivered vaginally, 5.1% has a cesarean delivery in the active phase, 10.1% had a cesarean delivery in the latent phase, 23.6% were in the active phase and 35.9% were in the latent phase. These numbers are cumulative. All cases reaching vaginal or cesarean delivery outcomes from each former time point accumulated to the next time point.
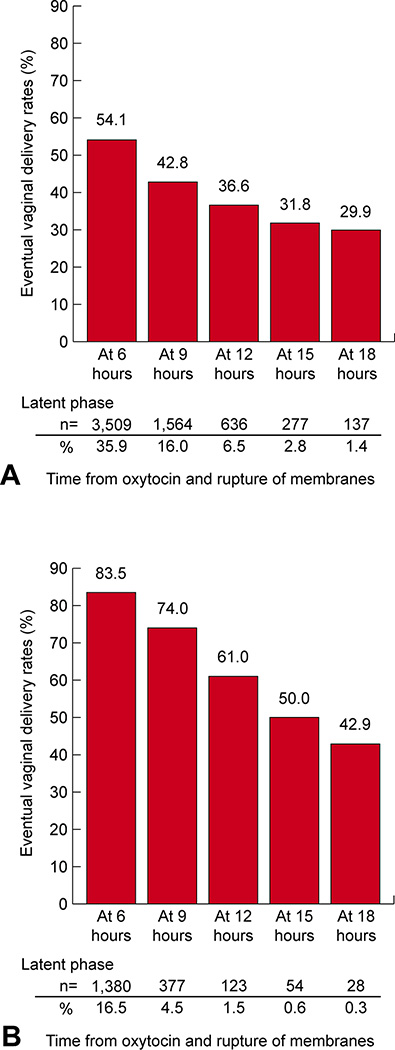
Eventual vaginal delivery rates of nulliparous and multiparous women remaining in the latent phase are presented in Figure 2. Women remaining in the latent phase with longer duration of oxytocin and ROM had decreasing rate of vaginal delivery (P <.001 in both nulliparous and multiparous women). For example, at 12 hours of oxytocin and ROM, 6.5% of nulliparous women remained in the latent labor, of whom 36.6% eventually had a vaginal delivery, and 1.5% of multiparous women remained in the latent labor, of whom 61.0% eventually had a vaginal delivery. At 18 hours of oxytocin and ROM, 1.4% of nulliparous women remained in the latent labor, of which 29.9% eventually had a vaginal delivery, and 0.3% of multiparous women remained in the latent labor, of whom 42.9% eventually had a vaginal delivery.
Figure 2.
Eventual vaginal delivery rates of women remaining in latent phase. A. Nulliparous women (n=9,763); B. Multiparous women (n=8,379). X-axis displays the duration of oxytocin and rupture of membranes. P-values for both nulliparous and multiparous women were both P <.001 (Cochran-Armitage Trend Test). % (number of women in the latent phase divided by all women).
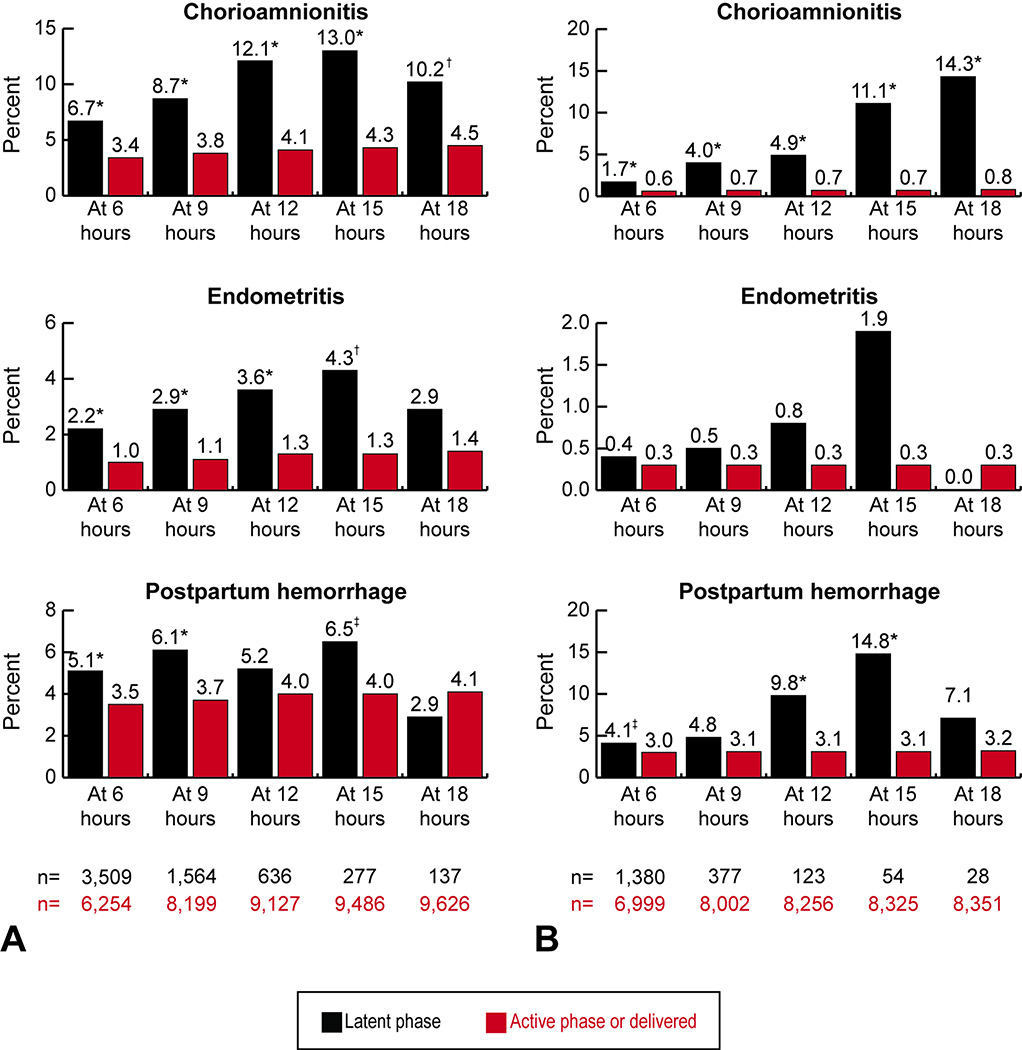
Maternal outcomes of nulliparous and multiparous women are presented in Figure 3. Nulliparous women who remained in latent phase compared to women who exited the latent phase had increased rates of chorioamnionitis at all time points (P < .001 for 6, 9, 12, 15 hours and P < .01 for 18 hours) with the highest difference occurring at 15 hours of 13.0% versus 4.3% (P <.001), endometritis at 6, 9, 12, and 15 hours (P< .001 for 6, 9, and 12 hours and P< .01 for 15 hours) with the highest difference occurring at 15 hours of 4.3% versus 1.3% (P <.01), and postpartum hemorrhage at 6, 9, and 15 hours (P <.001 for 6 and 9 hours, and P <.05 for 15 hours) with the highest difference occurring at 15 hours of 6.5% versus 4.0% (P <.05). Multiparous women who remained in latent phase compared to women who exited the latent phase had increased rates of chorioamnionitis at all time points (P <.001 for all) with the highest difference occurring at 18 hours of 14.3% versus 0.8% (P < .001), and postpartum hemorrhage at 6, 12, and 15 hours (P <.05 for 6 hours and P < .001 for 12, and 15 hours) with the highest difference occurring at 15 hours of 14.8% versus 3.1% (P <.001).
Figure 3.
Maternal outcomes of women remaining in latent phase compared with women in active phase or who had delivered. A. Nulliparous women (n=9,763); B. Multiparous women (n=8,379). X-axis displays the duration of oxytocin and rupture of membranes. Adjusted P-values were controlled for gestational age, race/ethnicity, body mass index (kg/m2) on admission, and hospital type. Latent phase was defined as ending when cervical exam 6 cm achieved. Active phase was defined as starting when 6 cm dilation achieved. *Adjusted P <.001; †adjusted P <.01; ‡adjusted P <.05.
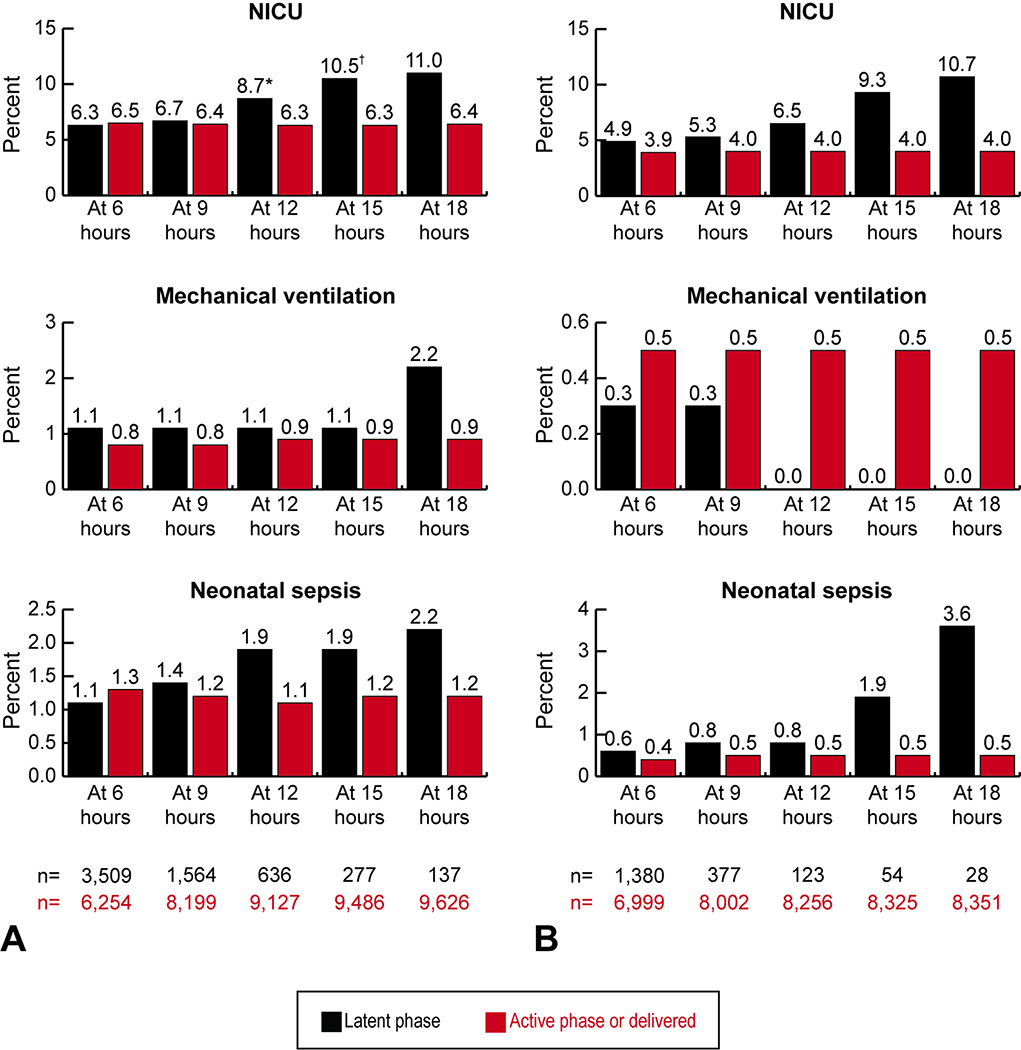
Neonatal outcomes of nulliparous and multiparous women are presented in Figure 4. Infants of nulliparous women who remained in latent phase compared to women who exited the latent phase had higher rates of NICU admission with increasing duration; however, only increased rates of NICU admission in women who remained in the latent labor after 12 and 15 hours were statistically significant (P <.05 for 12 hours and P <.01 for 15 hours). There was no statistical significant difference in the rates of mechanical ventilation and neonatal sepsis. For nulliparous women remaining in the latent phase, the rates of neonatal sepsis at 12, 15, and 18 hours were 1.9–2.2% which were higher than the 1.1% at 6 hours and 1.4% at 9 hours, and were also higher compared to the 1.1–1.3% rate at all time points for women who exited the latent phase. For infants of multiparous women who remained in the latent phase, the rates of neonatal sepsis at 15 and 18 hours were 1.9–3.6% which were higher than 0.6–0.8% at 6, 9, and 12 hours, and were also higher compared to the 0.4–0.5% rates at all time points for women who exited the latent phase. There was no difference in NICU admission, mechanical ventilation and neonatal sepsis. Detailed information on maternal and neonatal outcomes in nulliparous and multiparous women are provided in Appendixes 3 and 4, available online at http://links.lww.com/xxx.
Figure 4.
Neonatal outcomes of women remaining in latent phase compared with women in active phase or who had delivered. A. Nulliparous women (n=9,763); B. Multiparous women (n=8,379). Abbreviations: NICU, neonatal intensive care unit. X-axis displays the duration of oxytocin and rupture of membranes. Adjusted P-values were controlled for gestational age, race/ethnicity, body mass index (kg/m2) on admission, and hospital type. Latent phase was defined as ending when cervical exam 6 cm achieved. Active phase was defined as starting when 6 cm dilation achieved. *Adjusted P <.05; †adjusted P <.01.
Discussion
In this large, multi-institutional cohort of women undergoing induction of labor with an unfavorable cervix, we found that only 6.5% of nulliparous and 0.6% of multiparous women remained in the latent phase of labor at 12 hours and 15 hours, respectively. Even so, 36.6% and 50.0% of these women, respectively, delivered vaginally. We also found that nulliparous women who remained in the latent phase had increasing rates of chorioamnionitis, endometritis, and postpartum hemorrhage compared to women who exited the latent phase. The rate of NICU admission for nulliparous women remaining in the latent phase at 12 and 15 hours were increased compared to women who exited the latent phase. Multiparous women who remained in the latent phase had increasing rates of chorioamnionitis and postpartum hemorrhage compared to women who exited the latent phase. The rates of NICU admission and neonatal sepsis for multiparous women who remained in the latent phase rose at 15 hours compared to women who exited the latent phase, although these were not statistically significant.
Consistent with previous studies, we found that remaining in the latent phase was uncommon (<5%) after 15 hours of oxytocin and ROM in nulliparous women and 12 hours in multiparous women. 2, 4, 5 Our findings of decreasing vaginal delivery rates with longer duration of oxytocin and ROM are consistent with previous studies.2, 4, 5 We found only one study that investigated the differences in maternal outcomes between women in the latent phase and women who exited the latent phase.4 In that study, the difference in endometritis was highest at 12 hours, although that study did not investigate after 12 hours. Our study demonstrated novel findings that rates of maternal morbidity continued to rise in at 15 hours and 15–18 hours in nulliparous and multiparous women, respectively. Unlike previous studies,2, 4, 5 our study with a larger sample size demonstrated increased NICU admission rates in nulliparous women who remained in the latent phase at 12 and 15 hours. Therefore, at least 12 hours of oxytocin and ROM is reasonable before considering an induction failed in nulliparous women. In multiparous women, the rates of NICU admission and neonatal sepsis rose at 15 hours for women who remained in the latent phase versus women who exited the latent phase, although these were not statistically significant. Therefore, in multiparous women, at least 15 hours of oxytocin and ROM is reasonable before considering an induction failed.
The major strength of this study is the large cohort with clinical data from a contemporary U.S. population with the ability to study a wide variety of outcomes, particularly neonatal morbidity, associated with longer duration of oxytocin and ROM. Prior data on women with prolonged oxytocin and ROM has been available from single sites with small numbers limiting generalizability. In addition, our study was able to describe the labor characteristics and morbidity of multiparous women with long duration of oxytocin and ROM lasting ≥12 hours.
The main weakness of our study is that labor management was not standardized. We postulate that an unknown percentage of those cesarean deliveries performed in the latent phase <12 hours might have been avoided if a standard protocol was in place to compel clinicians to wait longer. The rate of complications and route of delivery also could have been different if there was standardized labor management. However, our findings reflect current obstetric practice given the age of the CSL data. Also, there was no protocol regarding cervical examination, which made it difficult to determine the exact time when women entered into the active phase of labor.
In summary, we found women remaining in the latent phase with longer duration of oxytocin and ROM had decreasing vaginal delivery rates. Women who remained in the latent phase had higher maternal morbidity compared to women who exited the latent phase. Infants of nulliparous women who remained in the latent phase compared to those of women who exited the latent phase started to have increased risk of NICU admission at 12 hours. In multiparous women, the rates of NICU admission and neonatal sepsis rose at 15 hours for women who remained in the latent phase versus women who exited the latent phase. Based on retrospective data, we cannot make the definitive definition of failed induction of labor. However, in light of when neonatal morbidity increased, at least 12 hours of oxytocin and ROM in nulliparous women and 15 hours in multiparous women seems reasonable before considering an induction failed, as long as maternal and fetal condition allows.
Supplementary Material
Acknowledgments
The Consortium on Safe Labor was funded by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through Contract No. HHSN267200603425C. This project was funded in part with Federal funds (Grant # UL1TR000101 previously UL1RR031975) from the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through the Clinical and Translational Science Awards Program (CTSA), a trademark of DHHS, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise.”
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Institutions involved in the Consortium on Safe Labor are named in Appendix 1, available online at http://links.lww.com/xxx.
Paper presentation information
Presented as an oral presentation at the SMFM 36th Annual Meeting-The pregnancy meeting, Atlanta, GA (Feb 1–6, 2016).
Reference
- 1.Martin JA, Hamilton EB, Osterman JK, Curtin SC, Mathews TJ. Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–68. [PubMed] [Google Scholar]
- 2.Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, Ramin SM, et al. Failed labor induction: toward an objective diagnosis. Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU) Obstet Gynecol. 2011;117:267–272. doi: 10.1097/AOG.0b013e318207887a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Obstetrics and Gynecologists; Society for Maternal-Fetal Medicine. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193. doi: 10.1016/j.ajog.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 4.Rouse DJ, Owen J, Hauth JC. Criteria for failed labor induction: Prospective evaluation of a standard protocol. Obstet Gynecol. 2000;96:671–677. doi: 10.1016/s0029-7844(00)01010-3. [DOI] [PubMed] [Google Scholar]
- 5.Simon CE, Grobman WA. When has an induction failed? Obstet Gynecol. 2005;105:705–709. doi: 10.1097/01.AOG.0000157437.10998.e7. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203:323. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laughon SK, Zhang J, Grewal J, et al. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gynecol. 2012;206:486.e1–486.e9. doi: 10.1016/j.ajog.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–1287. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.