Abstract
Our objective was to compare patients' health care experiences, related to their weight, across racial and ethnic groups. In Summer 2015, we distributed a written survey with telephone follow-up to a random sample of 5400 racially/ethnically and geographically diverse U.S. adult health plan members with overweight or obesity. The survey assessed members' perceptions of their weight-related healthcare experiences, including their perception of their primary care provider, and the type of weight management services they had been offered, or were interested in. We used multivariable multinomial logistic regression to examine the relationship between race/ethnicity and responses to questions about care experience. Overall, 2811 members (53%) responded to the survey and we included 2725 with complete data in the analysis. Mean age was 52.7 years (SD 15.0), with 61.7% female and 48.3% from minority racial/ethnic groups. Mean BMI was 37.1 kg/m2 (SD 8.0). Most (68.2%) respondents reported having previous discussions of weight with their provider, but interest in such counseling varied by race/ethnicity. Non-Hispanic blacks were significantly less likely to frequently avoid care (for fear of discussing weight/being weighed) than whites (OR 0.49, 95% CI 0.26–0.90). Relative to whites, respondents of other race/ethnicities were more likely to want weight-related discussions with their providers. Race/ethnicity correlates with patients' perception of discussions of weight in healthcare encounters. Clinicians should capitalize on opportunities to discuss weight loss with high-risk minority patients who may desire these conversations.
Keywords: Race/ethnicity, Obesity bias, Care experience, Weight management
Highlights
-
•
Minority patients may desire more information about weight management.
-
•
Non-Hispanic whites may be more likely to avoid care due to fear of weight bias.
-
•
Clinicians could conduct more sensitive weight loss discussions with all patients.
1. Introduction
People with obesity face societal biases that result in discrimination at school, work, and general everyday settings (Puhl and Heuer, 2009). These biases also exist within health care, where medical students, (Wear et al., 2006) physicians, (Foster et al., 2003, Hebl and Xu, 2001, Gudzune et al., 2011) and other care team members (Schwartz et al., 2003) may view or treat patients with obesity differently than those of healthy weight. Provider biases are described as “explicit” if the provider is aware of and able to verbalize the bias (Teachman and Brownell, 2001). For example, in a 2003 survey of US primary-care physicians (PCPs), one third of respondents viewed patients with obesity as “weak-willed, sloppy or lazy.” In contrast, some bias in health care is “implicit” — unconscious patterns of thinking, which nonetheless, may impact care delivery and the patient's experience of care (Foster et al., 2003, Teachman and Brownell, 2001, Phelan et al., 2014). Explicit and implicit biases may both negatively impact health (Phelan et al., 2015). Patients with obesity may, for example, avoid going to the doctor or miss important screenings, because of prior negative experiences in a healthcare setting (Amy et al., 2006, Wee et al., 2000, Rosen and Schneider, 2004).
Although there is growing evidence that the healthcare setting can be unwelcoming to patients with obesity, less attention has focused on the potential for heterogeneity according to other patient characteristics, such as race or ethnicity. Prior research has examined the impact of patient race/ethnicity on care delivery within pain management, (Weisse et al., 2001) cancer screening, (Mouton et al., 2010) and cardiovascular care, (Schulman et al., 1999) where explicit and implicit biases around racial/ethnic minority patients may influence the care that doctors provide (Green et al., 2007, Moskowitz et al., 2012) or patients' perception of care (Mouton et al., 2010). For racial/ethnic minorities, the experience of weight-related care may particularly differ from that of non-Hispanic whites, due to cultural differences in body image and norms around diet and physical activity, (Robinson et al., 2012, Kumanyika et al., 2012) as well as differing propensity toward weight misperception (Choi et al., 2015, Duncan et al., 2011, Dorsey et al., 2010).
In this study, we sought to understand whether the patient experience related to obesity differs across racial/ethnic groups. We hypothesized that patients from minority racial/ethnic groups, particularly those with cultural norms embracing heavier body weights, would report different experiences and preferences than non-Hispanic whites.
2. Methods
2.1. Data source
The Patient Outcomes Research to Advance Learning (PORTAL) network is a clinical data research network funded by the Patient Centered Outcomes Research Institute to promote collaboration across several large health systems with electronic medical records (EMR) (McGlynn et al., 2014). It includes all of the Kaiser Permanente regions, Group Health Cooperative, Health Partners, and Denver Health. Within PORTAL, a cohort of overweight and obese adults (age ≥ 18) was identified, and included adult members in a participating health plan between 1/2012 and 12/2013 2012–2013, who had a non-pregnant body mass index (BMI) ≥ 23 kg/m2 in the EMR (to include individuals with lower BMI cutoffs for overweight, such as Asians). This “obesity cohort” includes over 5 million adults and will serve as the basis for a number of observational studies of overweight and obesity.
2.2. Survey administration and overview
Between March and July 2015, we conducted a cross-sectional survey on a subsample of the obesity cohort to better understand the health care experiences of overweight and obese patients. We randomly sampled 5400 cohort members equally distributed across three geographically diverse Kaiser Permanente regions (Southeast, Northern and Southern California, Hawaii, Colorado, and Northwest) and Denver Health sites. For the survey, we selected for English or Spanish speakers with BMI ≥ 25 kg/m2 who had at least one outpatient visit in the prior 12 months. We oversampled patients with BMI ≥ 40 kg/m2, as this group might have lower response rates due to high likelihood of prior weight stigma experiences in the healthcare setting (Puhl and Heuer, 2009, Spahlholz et al., 2016). The study was approved by the Kaiser Permanente Southern California (KPSC) Institutional Review Board, with other sites ceding review.
A written survey taking approximately 10 min to complete, consisting of 36 multiple choice and fill-in-the-blank items, was mailed to 5400 individuals deemed eligible based on EMR information. The survey was offered in English or Spanish, based on a patient's written language preference noted in the EMR. If a mailed response was not received within 4 weeks, we attempted telephone contact for verbal survey administration. From the original sample (n = 5400), 1569 individuals (29%) did not respond, 925 (17%) refused, and 114 (2%) were ineligible – making our eligible denominator 5286. Our overall response rate was 53% (2197 written; 614 phone).
2.3. Independent variable
The primary independent variable was a respondent's racial/ethnic group, categorized as: 1) non-Hispanic white (white), 2) non-Hispanic black (black), 3) Hispanic, 4) Asian, or 5) Native Hawaiian/Other Pacific Islanders/American Indian/Native Alaskan (NA/PI). We combined the NA/PI group due to very small sample sizes of individual subgroups. If a survey indicated multiple races (240, 8.5%) or no race was selected (100, 3.5%), we grouped individuals according to EMR-recorded race/ethnicity, which is not necessarily self-reported, and uses an algorithm to prioritize the least-represented group in cases where a patient is from multiple race/ethnic backgrounds. To validate the EMR-measure, we tested for agreement between survey and EMR race/ethnicity when both were present, finding excellent agreement (92% of cases matched). Overall missingness for race/ethnicity was < 1%.
2.4. Dependent variables
Dependent variables focused on patients' perceptions of the health care experience related to being overweight or obese, using 7 items based on the Rudd Center's Patient Survey of Weight-Sensitive Healthcare Practices (Rudd Center for Food Policy and Obesity, n.d.). Respondents were asked to complete the items based on services received at their usual place of care, from their PCPs. Respondents described whether and how often: (a) their providers brought up their weight during a clinic visit; (b) they avoid coming to their provider because they do not want to be weighed or have a discussion about their weight; and (c) their providers were able to appropriately address their weight-related concerns in a supportive fashion (response choices: Frequently, Sometimes, No, Don't Remember, or Not Applicable). Next, they were asked whether they think that their provider understands the physical and emotional challenges faced by individuals who are overweight or obese (response choices: Yes, No, Don't Remember, or Not applicable). Finally, they were asked a series of questions about what kind of weight management options had been discussed with them, and what they wanted more information about (i.e., dietary changes, physical activity, classes, medications, meal replacements, and bariatric surgery). Non-response rates varied by question (Appendix A: Table A.2), and missingness tended to be < 4% (overall responses, not separated by race, are provided in Appendix A:Table A.3).
2.5. Covariates
We generated covariates using EMR data and survey responses. EMR-derived variables included: sex, age category (18–39, 40–59, ≥ 60), diabetes, hypertension, Charlson Index score (0, 1, 2, 3, 4 or higher) as an overall measure of morbidity, (Deyo et al., 1992) Medicaid enrollment, language preference, site and BMI. Survey-derived variables included: emotional well-being (PHQ-4), (Kroenke et al., 2009) perceived weight status (overweight, not overweight), and educational attainment (less than high school, high school graduate or GED, college graduate).
2.6. Statistical analysis
We excluded individuals with missing data (6 respondents missing race/ethnicity; 80 missing other covariates), leaving 2725 respondents in our final analysis (Table 1). Descriptive statistics were generated and compared across racial/ethnic groups using Kruskal-Wallis and Chi-Square testing, as appropriate.
Table 1.
Baseline characteristics of survey respondents according to racial/ethnic group.
| White (n = 1410 51.7%) | Black (n = 575, 21.1%) | Asian (n = 159, 5.8%) | Hispanic (n = 398, 14.6%) | NA/PI (n = 183, 6.7%) | p-value | Total sample (n = 2725) | |
|---|---|---|---|---|---|---|---|
| Age category in years (%) | |||||||
| 18–39 | 213 (15.1%) | 117 (20.3%) | 43 (27%) | 128 (32.2%) | 59 (32.2%) | < 0.01a | 560 (20.6%) |
| 40–59 | 576 (40.9%) | 294 (51.1%) | 60 (37.7%) | 176 (44.2%) | 81 (44.3%) | 1187 (43.6%) | |
| ≥ 60 | 621 (44.0%) | 164 (28.5%) | 56 (35.2%) | 94 (23.6%) | 43 (23.5%) | 978 (35.9%) | |
| Female (%) | 841 (59.6%) | 406 (70.6%) | 83 (52.2%) | 237 (59.5%) | 113 (61.7%) | < 0.01a | 1680 (61.7%) |
| Mean BMI in kg/m2 (SD) | 37.0 (7.9) | 39.4 (8.2) | 33.1 (7.6) | 37.3 (7.6) | 39.0 (7.8) | < 0.01b | 37.4 (8.0) |
| Diabetes status (%) | |||||||
| None | 669 (47.4%) | 278 (48.3%) | 66 (41.5%) | 199 (50.0%) | 64 (35%) | < 0.01a | 1276 (46.8%) |
| Prediabetesc | 434 (30.8%) | 142 (24.7%) | 49 (30.8%) | 110 (27.6%) | 50 (27.3%) | 785 (28.8%) | |
| Diabetes Mellitusd | 307 (21.8%) | 155 (27%) | 44 (27.7%) | 89 (22.4%) | 69 (37.7%) | 664 (24.4%) | |
| Hypertension statuse (%) | 548 (38.9%) | 327 (56.9%) | 74 (46.5%) | 154 (38.7%) | 82 (44.8%) | < 0.01a | 1185 (43.5%) |
| Educational attainment (%) | |||||||
| Less than high school | 41 (2.9%) | 26 (4.5%) | 8 (5%) | 98 (24.6%) | 6 (3.3%) | < 0.01a | 179 (6.6%) |
| High school graduate or GED | 797 (56.5%) | 345 (60.0%) | 72 (45.3%) | 222 (55.8%) | 128 (69.9%) | 1561 (57.3%) | |
| College graduate | 572 (40.6%) | 204 (35.5%) | 79 (49.7%) | 78 (19.6%) | 49 (26.8%) | 982 (36.1%) | |
| Medicaid beneficiary (%) | 46 (3.3%) | 17 (3.0%) | 3 (1.9%) | 22 (5.5%) | 16 (14.2%) | < 0.01a | 114 (4.2%) |
| English-speaking and writing (%) | 1335 (94.7%) | 541 (94.1%) | 148 (93.1%) | 279 (70.1%) | 177 (96.7%) | < 0.01a | 2480 (91.0%) |
| Perceives self as overweight (%) | 1221 (86.6%) | 499 (86.8%) | 121 (76.1%) | 343 (86.1%) | 166 (90.7%) | < 0.01a | 2350 (86.2%) |
Abbreviations: White — non-Hispanic white; Black — non-Hispanic black; NA/PI — Native Hawaiians, Pacific Islanders, American Indians, and Alaska Natives (Nichols et al., 2015).
Differences between race/ethnic groups significant (p < 0.01) based on Chi-Square test.
Differences between race/ethnic groups significant (p < 0.01) based on Kruskal Wallis test.
Prediabetes defined as at least one outpatient ICD-9 code of 790.2, 790.29, 790.21, or 790.22 OR at least one A1c 5.7–6.4% OR at least one fasting plasma glucose 100-125 mg/dL OR at least one oral glucose tolerance test value 140–199 mg/dL during 2009–2013.
Diabetes defined using the “Supreme DM” definition (Nichols et al., 2015) applied to labs and diagnosis codes from 2009 to 2013.
Hypertension defined based on the presence of one inpatient or two outpatient ICD-9 codes 401.xx-405.xx in 2009–2013. Study conducted on a U.S.-based sample in 2015.
To evaluate the association between a patient's race/ethnicity and their perceived weight management experience, we estimated odds ratios using multinomial logistic regression adjusted for the above covariates. White patients served as the reference group for the analyses. The reference answer choice for each survey question was selected through a combination of theoretical usefulness and response rate allowing for stable estimates. Analyses were conducted using R software, version 3.2.1.
3. Results
3.1. Population characteristics
Among the included 2725 respondents, mean age was 52.7 (SD 15) years, with 79.5% of respondents over 40 years (Table 1). More women than men participated – 61.7% were female. Our sample was diverse, with 21.1% of respondents identifying as black, 14.6% Hispanic, 5.8% Asian, 6.7% NA/PI, and 51.7% white. Mean BMI was 37.4 (SD 8.0) kg/m2, 24.4% had diabetes and 43.5% had hypertension. Most respondents (86.2%) perceived themselves to be overweight. Overall, respondents were reflective of our targeted survey population, although respondents were older than non-respondents and there was some over-representation of whites and under-representation of Hispanics (Appendix: Table A.1).
There were significant differences in measured baseline covariates across racial/ethnic groups (Table 1). Mean (SD) BMI among Asian respondents was 33.1 (7.6) kg/m2, compared with 39.4 (8.2) kg/m2 among black respondents. Diabetes was most prevalent among NA/PI respondents (37.7%) and least prevalent among white respondents (21.8%). NA/PI respondents were most likely to be Medicaid beneficiaries (14.2% compared to 4.2% overall), and Hispanic respondents had the lowest proportion of English speaking and writing (70% compared to 91% overall). Asian respondents were least likely to self-perceive as overweight (76% compared to 86% overall).
3.2. Patient experiences of weight-related care
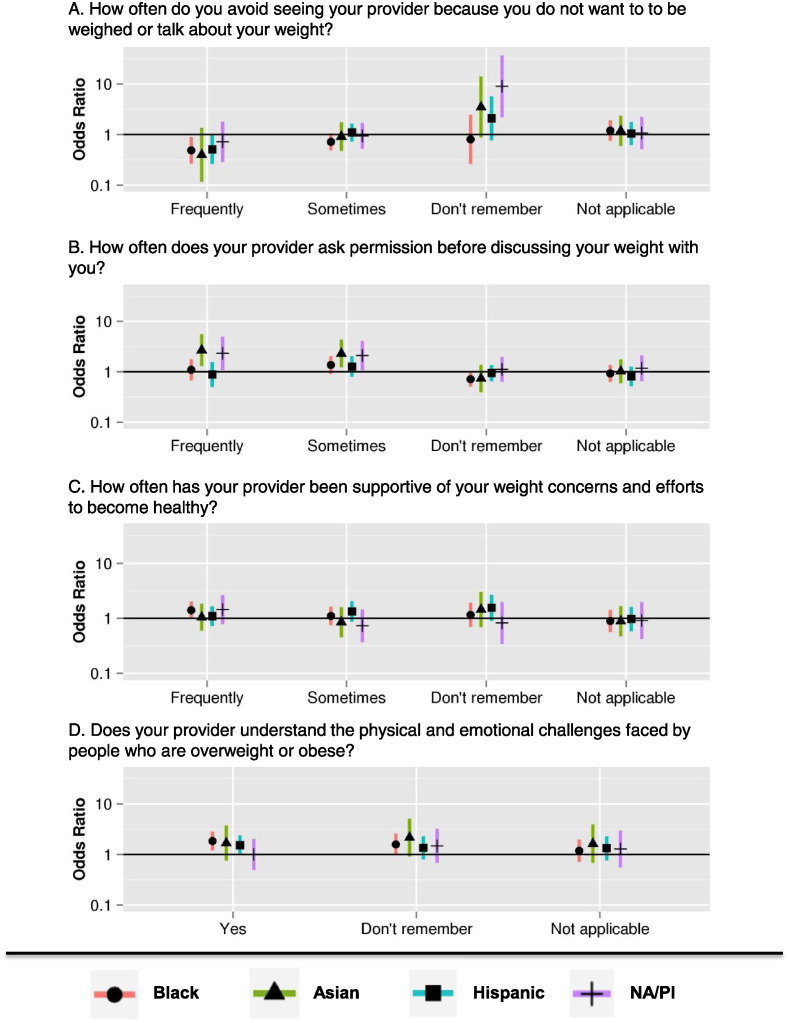
3.2.1. How often do you avoid seeing your provider because you do not want to be weighed or talk about your weight?
Respondents of all races/ethnicities were equally likely to say that sometimes or frequently they avoided seeing their provider for these reasons (compared with never), with 15.3% of all respondents (17.8% of those with BMI ≥ 30, 23.8% with BMI ≥ 40) indicating that they had avoided care as such. In multivariable multinomial logistic regression models, black respondents were less likely than whites to report that they frequently avoided care from their provider for these reasons (OR 0.49 (0.26–0.90)), with a trend toward all groups being less likely to report frequent avoidance compared to whites (Fig. 1). NA/PI respondents were more likely than whites to report that they did not remember if they had avoided care for these reasons (OR 9.0 (2.2, 36.9)).
Fig. 1.
Emotional aspects of overweight/obese patients' prior weight-related care experiences by race/ethnicity relative to whites.
3.2.2. How often does your provider ask your permission before discussing your weight?
Just over half of respondents (59.3%) indicated that their providers never asked for their permission before discussing their weight. Compared to whites, Asian and NA/PI respondents were more likely to report that their providers either frequently (Fig. 1) (Asians: OR 2.7 (1.3–5.6); NA/PI: OR 2.3 (1.1,5.0)), or sometimes (Asians: OR 2.3 (1.2–4.3); NA/PI: OR 2.1 (1.1–4.1)) asked their permission before discussing their weight (as opposed to never asking).
3.2.3. How often has your provider been supportive of your weight concerns and efforts to be healthy?
Over half of respondents (61.9%) indicated that their providers were sometimes or frequently supportive of their weight concerns. There were no significant differences in response frequency across racial and ethnic groups for this survey item (Fig. 1). We found that 13.3% of survey respondents felt this question was not applicable to them.
3.2.4. Does your provider understand the physical and emotional challenges faced by people who are overweight or obese?
Just over half of respondents (52.0%) indicated that they felt their providers understood these challenges. Black respondents were more likely than whites to respond “yes” (OR 1.8 (1.2–2.8)) (Fig. 1), with no other significant differences across race/ethnic categories.
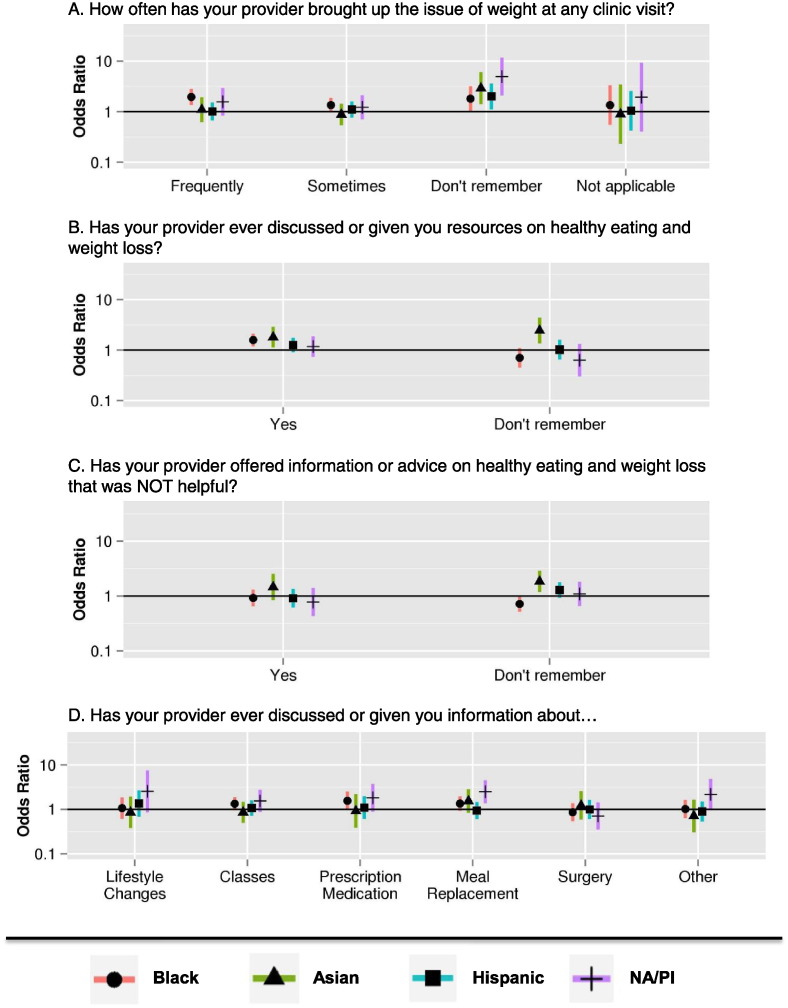
3.2.5. How often has your provider brought up the issue of weight at any clinic visit?
Among all respondents (Appendix A TableA.2), 23.1% reported that their provider never brought up the issue of weight, compared to 68.2% who said it was brought up sometimes or frequently. Among just respondents whose BMI was ≥ 30 kg/m2, 15.5% reported that the issue of weight was never brought up by their providers. In models using “never” as the reference answer, black patients were more likely than whites (OR 2.0, 95%CI (1.4–2.8)) to report that their providers frequently discussed their weight with them at clinic visits (Fig. 2). In contrast, all groups of patients were more likely than whites to say they didn't remember if their provider had discussed their weight, compared with saying it never happened (for Asian, OR 2.9 (1.4–6.1); for Hispanic OR 2.0 (1.1–3.6); for NA/PI OR 5.0 (2.1–11.7); for Black OR 1.8 (1.0,3.2)).
Fig. 2.
Overweight/obese patients' recall of the content of prior weight-related discussions by race/ethnicity relative to whites.
3.2.6. Has your provider ever given or discussed resources on healthy eating and weight loss?
Over half (59.7%) of respondents said their providers had given or discussed resources with them. Black and Asian respondents were more likely than whites to say that such discussions happened (Black respondents: OR 1.6 (1.2–2.1); Asian respondents OR 1.8 (1.1–2.9)). Asians were also more likely to say they didn't remember (OR 2.4 (1.4–4.4)) (Fig. 2).
3.2.7. Types of weight loss resources reported and desired by survey respondents
Among the 1627 respondents who indicated receiving weight loss resources or recommendations, we asked specifically about what kind of discussions they had, or what resources were provided. A majority (89.2%) indicated that their providers had given them general information about lifestyle changes (diet or physical activity), while fewer (63.3%) had been given information about formal classes or programs to address these lifestyle changes. Most respondents indicated they had received no information about weight loss medications (82.4% overall; 82.3% of those with BMI ≥ 30), meal replacement products (72.6% overall; 72.3% for BMI ≥ 30), or bariatric surgery (78.2% overall; 70.4% for BMI ≥ 40). There were few differences across racial/ethnic groups according to what types of resources had been discussed or recommended, except that NA/PI respondents were more likely than whites to report that a provider had recommended meal replacements (OR 2.5 (1.4–4.5)) (Fig. 2).
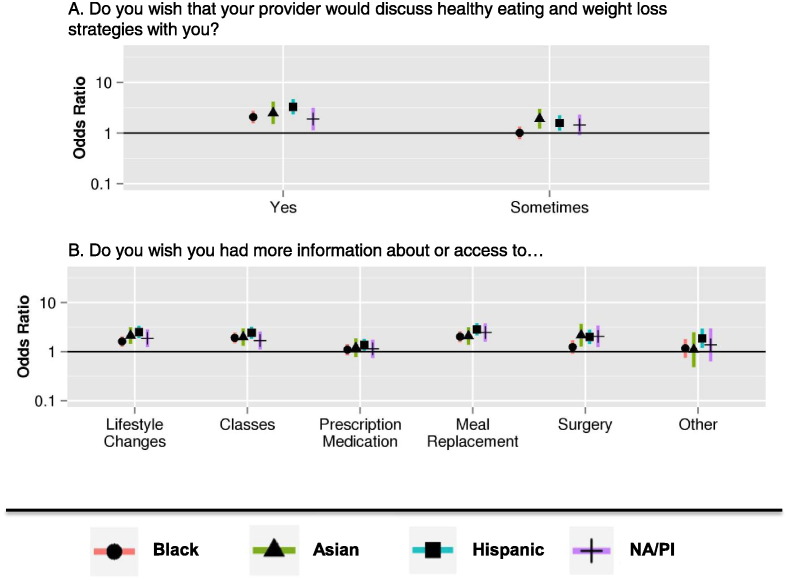
When asked whether they wished their providers would discuss or offer other weight management resources with them, over half of respondents indicated “Sometimes” or “Yes” (62.4%). However, responses to this item differed strongly across racial and ethnic categories. Compared to white respondents, those from all other racial/ethnic categories surveyed were more likely to respond “Yes” to this question compared to “No” (Asian OR 2.5 (1.5–4.2); black OR 2.1 (1.6–2.8); Hispanic OR 3.3 (2.3–4.7); NA/PI OR 1.9 (1.1–3.2)) (Fig. 3).
Fig. 3.
Overweight/obese patients' desired weight-related care experiences by race/ethnicity relative to whites.
Respondents indicated they wanted more information from their providers about the following types of weight management resources: lifestyle change information (46.0%); classes/programs (46.1% overall; 46.4% of BMI ≥ 30); prescription medications (33.6% overall; 38.0% of BMI ≥ 30); meal replacements (33.9% overall; 36.9% of BMI ≥ 30) and bariatric surgery (18.0% overall; 28.2% of BMI ≥ 40). As was observed with other similar items, respondents from racial/ethnic minority groups were more likely than whites to say that they wanted more information about lifestyle changes, classes, and meal replacements (Fig. 3). Other than black respondents, all other racial/ethnic groups were also more likely than whites to indicate that they wanted more information about bariatric surgery.
4. Discussion
In this survey of overweight and obese health plan members, we explored weight-related health care experiences, and how they might differ by patient race/ethnicity. While most respondents indicated that weight counseling occurred, desire for weight management advice and perceived provider communication differed strongly by race/ethnicity. Black respondents were less likely than whites to report frequently avoiding care for fear of weight loss discussions, and were more likely to perceive providers as understanding the challenges of being overweight. Notably, patients of all other races/ethnicities were more likely than whites to endorse a desire for weight loss discussions with their provider.
4.1. Perceptions of weight-related care overall
Nearly a quarter of respondents indicated that they had never had a discussion about weight with their medical provider, which implies higher levels of counseling than documented in other studies (Bleich et al., 2012, Bleich et al., 2011). Nonetheless, there is room for improvement, as providers may still not be routinely addressing this issue. Making patients aware of their weight status has been shown to increase the likelihood of weight loss attempts (Durant et al., 2009).
While providers do need to more routinely address weight with patients, the approach to such discussions requires sensitivity. Fifteen percent of respondents overall, and nearly a quarter of those with class III obesity, reported avoiding primary care for fear that their weight might be discussed. Care avoidance is of particular concern given that it may contribute to worse health outcomes (Amy et al., 2006, Hansson and Rasmussen, 2014). In our sample, over half of respondents indicated that providers never asked permission before talking about their weight. Implementing this simple practice, (Pollak et al., 2010) might improve perceptions of healthcare and reduce care avoidance.
Weight management strategies discussed with respondents were primarily limited to lifestyle changes, even when we restricted to patients with BMI ≥ 30 kg/m2 for medications/meal replacements, or BMI ≥ 40 kg/m2 for surgery. While more intensive strategies such as medication or surgery are not indicated in all patients, their omission from weight management discussions may reflect a lack of comfort with or provider biases against these approaches.
4.2. Differing perceptions of weight-related care by racial/ethnic group
Black respondents were more likely than whites to report that their weight had been discussed frequently by providers. This finding differs from prior work that suggests that black patients may be less likely to receive weight counseling, (Bleich et al., 2012) perhaps attributable to our sample of a managed care population. Additionally, patients in our sample predominantly correctly perceived themselves as overweight, and prior work has shown that correct weight perception predicts higher likelihood of weight loss behaviors, (Duncan et al., 2011) although perhaps less so among African-Americans (Dorsey et al., 2010). Black respondents were also more likely to report that they wished that their providers would have more discussions of weight with them. Non-Hispanic blacks are heavily burdened by obesity and its comorbidities, (Wang and Beydoun, 2007) so it is promising that they were generally favorable about receiving weight-related advice. Our results may be a signal to clinicians that they need not avoid such discussions for fear of raising a sensitive topic (Gudzune et al., 2012).
Asian respondents were more likely than whites to indicate that they didn't remember if a weight-related interaction had taken place with their provider. This could be related to the fact that they were also more likely to mis-perceive themselves as being of “normal weight”, perhaps making them more likely to forget such discussions. This finding is somewhat in contrast to prior work by Choi et al. which found that, relative to whites, normal weight Korean Americans were more likely to misperceive themselves as overweight (Choi et al., 2015). Our sample, however, contained a diverse group of Asian Americans, perhaps explaining this difference. The misperception of weight status in this group is especially of concern given that our survey was limited to BMI ≥ 25 kg/m2, and the WHO now recommends using a lower “overweight” cutoff of BMI ≥ 23 kg/m2 in Asians (Jih et al., 2014).
Compared to whites, Hispanic respondents had similar responses in terms of perceptions of care, satisfaction and support. This finding contrasts with prior work suggesting that “Latino” patients may express lower satisfaction ratings with their PCPs than black and white patients, (Blair et al., 2013) perhaps because our sample of managed carepatients engages more regularly with the healthcare system than the general population. It was promising to find that Hispanic respondents desired weight loss discussions and were equally likely as other races to have discussed their weight with providers, particularly as this group may be more likely to change health behaviors as a result of such discussions (Durant et al., 2009).
Our sample of Native Hawaiian/Pacific Islanders and American Indians/Native Americans represented a small subset overall; therefore we may have lacked sufficient power to detect some meaningful differences between this group and our white respondents. Additionally, the grouping together of these culturally-distinct subpopulations may have obscured important patterns that could have been observed with a larger sample. As with other racial/ethnic groups, these respondents indicated wanting more information about a variety of weight management options.
Differing cultural norms around body habitus may partially explain the patterns that we observed relative to non-Hispanic white respondents (Chugh et al., 2013). White women, for example, tend to have norms that favor a thinner body habitus, and may therefore be more sensitive to fat-shaming or anti-fat biases, making them more likely to avoid situations that bring these issues to the forefront (Puhl and Heuer, 2009, Hebl and Heatherton, 1998, Wee et al., 2015). Additionally, there may be unmeasured provider-level differences between groups (e.g., patient-provider racial concordance may vary by patient race/ethnicity, level of comfort with obesity counseling, or physician weight status) that might impact communication or patient perceptions around weight (Bleich et al., 2012, Cooper-Patrick et al., 1999, Dutton et al., 2014).
Our study has several limitations. First, non-response bias may have influenced our results in several ways. Our respondents were, on average, older adults, and age may modify a patient's perception of care, (Blair et al., 2013) or the way they are treated by providers (Beach et al., 2006). Additionally, the lower than expected reported rates of care avoidance could be inaccurate if nonrespondents were more likely to be those patients disenchanted with healthcare. Language barriers may have led to underrepresentation of patients for whom English was not a first language, also resulting in an overly optimistic view of weight management counseling in our systems.
Provider-level factors may play an important role in a patient's experience of weight-related care, and we were unable to adjust for these. Additionally, we did not conduct psychometric testing of our measures in our population, which could mean that study respondents did not interpret the survey items exactly as we intended. Finally, our results are based on the subjective experiences of patients rather than objective observations of patient encounters. Therefore, personal feelings have greater potential to influence our results. Regardless, the subjective experience of care is very important and may have implications for future care utilization and health (Mouton et al., 2010).
In conclusion, our results suggest that racial/ethnic minority groups most heavily impacted by obesity want to receive more weight loss advice and discussion from their providers, focused on interventions beyond just diet and exercise, and most patients are having positive experiences with weight-related care across racial/ethnic groups. Primary care practitioners should engage overweight/obese patients in weight management discussions in a sensitive manner to ensure mindfulness of patient goals and explore patient preferences for all the different strategies to lose weight including lifestyle changes, meal replacements, medications and surgery.
Conflict of interest
None of the authors has any potential conflicts of interest to disclose.
Transparency document
Transparency document.
Funding
PCORI CDRN 1306-04681 — Patient Outcomes Research to Advance Learning.
Acknowledgements
This study used the infrastructure developed by the PORTAL (Patient Outcomes Research to Advance Learning) Network, a consortium of 4 integrated delivery systems (Kaiser Permanente, Group Health Cooperative, HealthPartners, and Denver Health) and their affiliated research centers, with funding support from a contract awarded by the Patient-Centered Outcomes Research Institute (PCORI). Additionally, we would like to especially thank Dr. Connie Mah Trinacty, of KP Hawaii, for her thoughtful comments and feedback on this manuscript.
Footnotes
The Transparency document related to this article can be found in the online version.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.pmedr.2016.06.015.
Appendix A. Supplementary data
Supplementary Tables.
References
- Amy N.K., Aalborg A., Lyons P., Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int. J. Obes. 2006;30(1):147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- Beach M.C., Roter D.L., Wang N.Y., Duggan P.S., Cooper L.A. Are physicians' attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ. Couns. 2006;62(3):347–354. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair I.V., Steiner J.F., Fairclough D.L. Clinicians' implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann. Fam. Med. 2013;11(1):43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich S.N., Pickett-Blakely O., Cooper L.A. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ. Couns. 2011;82(1):123–129. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich S.N., Simon A.E., Cooper L.A. Impact of patient-doctor race concordance on rates of weight-related counseling in visits by black and white obese individuals. Obesity (Silver Spring) 2012;20(3):562–570. doi: 10.1038/oby.2010.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J., Bender M.S., Arai S., Fukuoka Y. Factors associated with underestimation of weight status among Caucasian, Latino, Filipino, and Korean Americans—DiLH survey. Ethn. Dis. 2015;25(2):200–207. [PMC free article] [PubMed] [Google Scholar]
- Chugh M., Friedman A.M., Clemow L.P., Ferrante J.M. Women weigh in: obese African American and White women's perspectives on physicians' roles in weight management. J. Am. Board Fam. Med. 2013;26(4):421–428. doi: 10.3122/jabfm.2013.04.120350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Patrick L., Gallo J.J., Gonzales J.J. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Deyo R.A., Cherkin D.C., Ciol M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Dorsey R.R., Eberhardt M.S., Ogden C.L. Racial and ethnic differences in weight management behavior by weight perception status. Ethn. Dis. 2010;20(3):244–250. [PubMed] [Google Scholar]
- Duncan D.T., Wolin K.Y., Scharoun-Lee M., Ding E.L., Warner E.T., Bennett G.G. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int. J. Behav. Nutr. Phys. Act. 2011;8:20. doi: 10.1186/1479-5868-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durant N.H., Bartman B., Person S.D., Collins F., Austin S.B. Patient provider communication about the health effects of obesity. Patient Educ. Couns. 2009;75(1):53–57. doi: 10.1016/j.pec.2008.09.021. [DOI] [PubMed] [Google Scholar]
- Dutton G.R., Herman K.G., Tan F. Patient and physician characteristics associated with the provision of weight loss counseling in primary care. Obes. Res. Clin. Pract. 2014;8(2):e123–e130. doi: 10.1016/j.orcp.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster G.D., Wadden T.A., Makris A.P. Primary care physicians' attitudes about obesity and its treatment. Obes. Res. 2003;11(10):1168–1177. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- Green A.R., Carney D.R., Pallin D.J. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J. Gen. Intern. Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudzune K.A., Clark J.M., Appel L.J., Bennett W.L. Primary care providers' communication with patients during weight counseling: a focus group study. Patient Educ. Couns. 2012;89(1):152–157. doi: 10.1016/j.pec.2012.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudzune K.A., Huizinga M.M., Cooper L.A. Impact of patient obesity on the patient-provider relationship. Patient Educ. Couns. 2011;85(3):e322–e325. doi: 10.1016/j.pec.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson L.M., Rasmussen F. Association between perceived health care stigmatization and BMI change. Obes. Facts. 2014;7(3):211–220. doi: 10.1159/000363557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebl M.R., Heatherton T.F. The stigma of obesity in women: the difference is Black and White. Personal. Soc. Psychol. Bull. 1998;24:417–426. [Google Scholar]
- Hebl M.R., Xu J. Weighing the care: physicians' reactions to the size of a patient. Int. J. Obes. Relat. Metab. Disord. 2001;25(8):1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- Jih J., Mukherjea A., Vittinghof E. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev. Med. 2014;65:1–6. doi: 10.1016/j.ypmed.2014.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Kumanyika S., Taylor W.C., Grier S.A. Community energy balance: a framework for contextualizing cultural influences on high risk of obesity in ethnic minority populations. Prev. Med. 2012;55(5):371–381. doi: 10.1016/j.ypmed.2012.07.002. [DOI] [PubMed] [Google Scholar]
- McGlynn E.A., Lieu T.A., Durham M.L. Developing a data infrastructure for a learning health system: the PORTAL network. J. Am. Med. Inform. Assoc. 2014;21(4):596–601. doi: 10.1136/amiajnl-2014-002746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz G.B., Stone J., Childs A. Implicit stereotyping and medical decisions: unconscious stereotype activation in practitioners' thoughts about African Americans. Am. J. Public Health. 2012;102(5):996–1001. doi: 10.2105/AJPH.2011.300591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouton C.P., Carter-Nolan P.L., Makambi K.H. Impact of perceived racial discrimination on health screening in black women. J. Health Care Poor Underserved. 2010;21(1):287–300. doi: 10.1353/hpu.0.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols G.A., Schroeder E.B., Karter A.J. Trends in diabetes incidence among 7 million insured adults, 2006-2011: the SUPREME-DM project. Am. J. Epidemiol. 2015;181(1):32–39. doi: 10.1093/aje/kwu255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan S.M., Burgess D.J., Yeazel M.W., Hellerstedt W.L., Griffin J.M., van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 2015;16(4):319–326. doi: 10.1111/obr.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan S.M., Dovidio J.F., Puhl R.M. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring) 2014;22(4):1201–1208. doi: 10.1002/oby.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak K.I., Alexander S.C., Coffman C.J. Physician communication techniques and weight loss in adults: project CHAT. Am. J. Prev. Med. 2010;39(4):321–328. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R.M., Heuer C.A. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Robinson S.A., Webb J.B., Butler-Ajibade P.T. Body image and modifiable weight control behaviors among black females: a review of the literature. Obesity (Silver Spring) 2012;20(2):241–252. doi: 10.1038/oby.2011.54. [DOI] [PubMed] [Google Scholar]
- Rosen A.B., Schneider E.C. Colorectal cancer screening disparities related to obesity and gender. J. Gen. Intern. Med. 2004;19(4):332–338. doi: 10.1111/j.1525-1497.2004.30339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd Center for Food Policy and Obesity Preventing Weight Bias: Helping Without Harming in Clinical Practice. http://biastoolkit.uconnruddcenter.org (Accessed 12/6/2015, 2015)
- Schulman K.A., Berlin J.A., Harless W. The effect of race and sex on physicians' recommendations for cardiac catheterization. N. Engl. J. Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Schwartz M.B., Chambliss H.O., Brownell K.D., Blair S.N., Billington C. Weight bias among health professionals specializing in obesity. Obes. Res. 2003;11(9):1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- Spahlholz J., Baer N., Konig H.H., Riedel-Heller S.G., Luck-Sikorski C. Obesity and discrimination — a systematic review and meta-analysis of observational studies. Obes. Rev. 2016;17(1):43–55. doi: 10.1111/obr.12343. [DOI] [PubMed] [Google Scholar]
- Teachman B.A., Brownell K.D. Implicit anti-fat bias among health professionals: is anyone immune? Int. J. Obes. Relat. Metab. Disord. 2001;25(10):1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- Wang Y., Beydoun M.A. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol. Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Wear D., Aultman J.M., Varley J.D., Zarconi J. Making fun of patients: medical students' perceptions and use of derogatory and cynical humor in clinical settings. Acad. Med. 2006;81(5):454–462. doi: 10.1097/01.ACM.0000222277.21200.a1. [DOI] [PubMed] [Google Scholar]
- Wee C.C., Davis R.B., Chiodi S., Huskey K.W., Hamel M.B. Sex, race, and the adverse effects of social stigma vs. other quality of life factors among primary care patients with moderate to severe obesity. J. Gen. Intern. Med. 2015;30(2):229–235. doi: 10.1007/s11606-014-3041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee C.C., McCarthy E.P., Davis R.B., Phillips R.S. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann. Intern. Med. 2000;132(9):697–704. doi: 10.7326/0003-4819-132-9-200005020-00003. [DOI] [PubMed] [Google Scholar]
- Weisse C.S., Sorum P.C., Sanders K.N., Syat B.L. Do gender and race affect decisions about pain management? J. Gen. Intern. Med. 2001;16(4):211–217. doi: 10.1046/j.1525-1497.2001.016004211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.
Supplementary Tables.