Abstract
Background and Purpose
External counterpulsation (ECP) is a noninvasive method used to enhance cerebral perfusion by elevating the blood pressure in ischemic stroke. However, the response of the beat-to-beat blood pressure variability (BPV) in ischemic stroke patients during ECP remains unknown.
Methods
We enrolled recent ischemic stroke patients and healthy controls. Changes in the blood flow velocities in bilateral middle cerebral arteries and the continuous beat-to-beat blood pressure before, during, and after ECP were monitored. Power spectral analysis revealed that the BPV included oscillations at very low frequency (VLF; <0.04 Hz), low frequency (LF; 0.04–0.15 Hz), and high frequency (HF; 0.15–0.40 Hz), and the total power spectral density (TP; <0.40 Hz) and LF/HF ratio were calculated.
Results
We found that ECP significantly increased the systolic and diastolic blood pressures in both stroke patients and controls. ECP decreased markedly the systolic and diastolic BPVs at VLF and LF and the TP, and the diastolic BPV at HF when compared with baseline. The decreases in diastolic and systolic BPV reached 37.56% and 23.20%, respectively, at VLF, 21.15% and 12.19% at LF, 8.76% and 16.59% at HF, and 31.92% and 23.62% for the total TP in stroke patients, which did not differ from those in healthy controls. The change in flow velocity on the contralateral side was positively correlated with the total TP systolic BPV change induced by ECP (r=0.312, p=0.035).
Conclusions
ECP reduces the beat-to-beat BPV when increasing the blood pressure and cerebral blood flow velocity in ischemic stroke patients. ECP might be able to improve the clinical outcome by decreasing the beat-to-beat BPV in stroke patients, and this should be explored further in future studies.
Keywords: blood pressure, blood pressure variability, cerebral hemodynamics, external counterpulsation, ischemic stroke
INTRODUCTION
Hypertension is the most-prevalent treatable risk factor for stroke,1 and blood pressure (BP) reduction is effective in preventing stroke.2 However, the clinical benefits of antihypertensive treatment in stroke prevention are not only related to lowering the BP,3 but also to blood pressure variability (BPV).4,5 Stead et al.6 found that wide fluctuations of BP in the first 3 hours after acute ischemic stroke were associated with an increased risk of death at 90 days in a cohort of 71 patients. Another previous study has shown that beat-to-beat BPV is increased after acute stroke compared with age- and sex-matched control subjects, and that high BPV is related to a poor outcome at 30 days after ischemic stroke.7 Sykora et al.8 also found that the fluctuation of beat-to-beat BPV played an important role in the outcome after stroke. Therefore, controlling the BPV in patients following stroke may be an effective way to improve their prognosis.
External counterpulsation (ECP) is a noninvasive and well-established method for treating ischemic heart disease.9,10,11 It involves applying electrocardiography-triggered diastolic pressure to the lower extremities by means of air-filled cuffs. This diastolic augmentation of the blood flow and the simultaneous decrease in the systolic afterload increases the blood flow to vital organs such as the heart, brain, and kidneys.9,12 Our pilot study showed that ECP is feasible for improving the clinical neurological deficit in ischemic stroke patients with large-artery disease.13 We recently found that ECP may improve the cerebral perfusion and collateral blood supply in ischemic stroke by augmenting the BP and cerebral blood flow velocity (CBFV).10 However, the effect of ECP on BPV in ischemic stroke remains unknown. The relationship between cerebral augmentation effects and BPV changes induced by ECP have also not been investigated previously. We therefore conducted this study in order to examine the effect of ECP on beat-to-beat BPV and the correlation between the cerebral augmentation effects and beat-to-beat BPV changes induced by ECP in patients with recent ischemic stroke.
METHODS
Subjects
Patients with a good temporal acoustic window admitted within 14 days of stroke onset at Prince of Wales Hospital in Hong Kong between November 2007 and August 2011 were included in this study. Stroke was diagnosed according to the definition of the World Health Organization, and ischemia was confirmed by computed tomography or magnetic resonance imaging. All patients were examined by transcranial Doppler ultrasonography (TCD), duplex ultrasound, or magnetic resonance angiography. Intracranial or extracranial large-artery stenosis was diagnosed using standard protocols.14,15 All of the recruited patients presented with unilateral infarction. Patients with the following characteristics were excluded: evidence of cardioembolic stroke such as atrial fibrillation and rheumatic heart disease; evidence of hemorrhage on brain computed tomography; evidence of arteriovenous malformation, arteriovenous fistula, or aneurysm; history of intracerebral hemorrhage, brain tumor, or malignancy; sustained hypertension [systolic BP (SBP) >180 mm Hg or diastolic BP (DBP) >100 mm Hg]; severe symptomatic peripheral vascular disease; evidence of coexisting systemic diseases of renal failure (creatinine >300 µmol/L), cirrhosis, or thrombocytopenia (platelet count <100,000/mm3); severe dementia or psychosis; or pregnancy. Fourteen volunteers aged ≥45 years without a history of cerebrovascular events or risk factors were recruited as healthy controls. Each healthy controls underwent TCD and carotid duplex ultrasonography to rule out large-artery stenosis disease.
ECP TCD Monitoring
ECP was performed using an enhanced ECP system (model number MC2, Vamed Medical Instrument Company, Foshan, China). The treatment pressure of ECP was 150 mm Hg. This ECP system includes three pairs of pneumonic cuffs that are applied to the calves, lower thighs, and upper thighs. The electrocardiograph triggers cuff inflation sequentially from the distal to proximal regions during diastole, and releases the cuff pressure before the start of systole. The standard duration of ECP is generally several weeks (5 daily 1-hour sessions each week for 7 weeks, giving a total of 35 sessions), based on empirical data from a study in China.16 TCD monitoring of CBFV in bilateral middle cerebral arteries (MCA) was performed before, during, and after ECP using an ST3 TCD system (Spencer Technologies, Seattle, WA, USA). A 2-MHz pulsed Doppler probe insonated the MCA through the temporal window at a depth of 50–65 mm on each side. In order to ensure reliable values of CBFV during ECP despite the possible presence of movement artifacts, we first optimized the individual TCD signal by selecting an insonation depth of 50–65 mm. After optimizing the Doppler signal, the probes were attached to the skull at a fixed angle using an adjustable headband. The standard duration of ECP therapy is 35 hours (7 weeks), and since this study was focused investigating hemodynamic changes during ECP, we recorded the blood flow velocity in the MCA before and during ECP for 3 minutes each. Immediately after ECP treatment stopped, we recorded a further 3 minutes of MCA blood flow changes.10
Measurement of BPV
The beat-to-beat BP and respiration were recorded continuously (Task Force Monitor 3040i, CNSystems Medizintechnik, Graz, Austria) during the period of TCD monitoring. The BP was measured through finger cuffs on the index fingers and the middle fingers of the left hand, with a cuff of the appropriate size (small, medium, or large) chosen based on the hand size. The BP was measured in the supine position with the respiration at a target frequency of 15 cycles per minute to minimize bias due to differences in breathing patterns between individuals. The BP and respiratory signals were first edited automatically, then sampled digitally and transferred from the Task Force Monitor 3040i system to a computer for analysis of the beat-to-beat BPV using power spectral methods.
For spectral analysis, histograms of the SBP and DBP for sinus beats were computed and digitized at 10 samples per second. Autoregressive modeling was used to construct frequency-domain spectrograms of the BPV.17 The BPV included oscillations at very low frequency (VLF; <0.04 Hz), low frequency (LF; 0.04–0.15 Hz), and high frequency (HF; 0.15–0.40 Hz), and the total power spectral density (TP; <0.40 Hz) and LF/HF ratio18 were calculated. Evidence is presented that myogenic vascular function, the renin-angiotensin system (RAS), and endothelium-derived nitric oxide all affect BPV at VLF,18,19 whereas the LF BPV has previously been demonstrated to reflect changes in sympathetic activity.20 In addition, the HF BPV is mainly influenced by changes in cardiac output, and the LF/HF ratio has been validated as a marker of sympathetic vascular activity.18
Data analysis
The mean flow velocity in the MCA was automatically recorded by the TCD system as the mean value of the area under the envelope curve during a complete cardiac cycle. TCD data of stroke patients were analyzed based on the side ipsilateral to the infarct or on the contralateral side, while TCD data of healthy controls were analyzed based on the left or right cerebral side. The cerebral augmentation index (CAI) was used to evaluate the augmentation effect of ECP, which was calculated as the increase in the percentage mean flow velocity during ECP compared with baseline. Normally distributed continuous data are presented as mean±SD values, while category data are presented as number and percentage values. Differences between two groups were detected using the two-tailed Student's t-test or the nonparametric test as appropriate. All statistical analyses were performed with SPSS (version 19.0; SPSS Inc., Chicago, IL, USA). Differences with a probability value of p<0.05 were considered significant.
Ethical approval
This study was approved by the local medical ethics committee (Joint CUHK-NTEC Clinical Research Ethics Committee). Written informed consent was obtained from all study participants prior to enrollment.
RESULTS
Baseline characteristics
Forty-six patients with ischemic stroke (41 males; age 64.30±11.07 years) and a good temporal acoustic window, and 14 healthy controls (6 males; age 59.36±2.24 years) agreed to undergo ECP TCD monitoring. All of the patients had a unilateral infarct in the anterior circulation territory. The sex distribution differed significantly between the two groups (p=0.001), and stroke patients were older than the healthy controls (p=0.006). All of the patients underwent measurements on the first session of ECP treatment, with a mean interval from the stroke onset of 4.91 days. The stroke patients had moderate neurological deficits, with a mean admission score of 6 on the National Institutes of Health Stroke Scale. The other baseline characteristics of the stroke patients are given in Table 1.
Table 1. Baseline characteristics.
| Parameter | Stroke patients (n=46) | Healthy controls (n=14) | p |
|---|---|---|---|
| Gender (male/female) | 41/5 | 6/8 | 0.001 |
| Age (mean±SD), years | 64.30±11.07 | 59.36±2.24 | 0.006 |
| Interval from stroke onset to examination (mean±SD), days | 4.91±2.97 | NA | |
| Admission NIHSS score (mean±SD) | 5.57±4.49 | NA | |
| Hypertension, n (%) | 39 (84.78) | 0 (0) | |
| Diabetes, n (%) | 20 (43.48) | 0 (0) | |
| Hyperlipidemia, n (%) | 27 (58.70) | 0 (0) | |
| Previous stroke, n (%) | 12 (26.10) | 0 (0) | |
| Smoker, n (%) | 26 (56.52) | 0 (0) | |
| Drinker, n (%) | 7 (15.22) | 0 (0) | |
| Intracranial large-artery disease, n (%) | 32 (69.60) | 0 (0) | |
| Extracranial large-artery disease, n (%) | 2 (4.30) | 0 (0) | |
| Anterior circulation infarct, n (%) | 46 (100.0) | NA | |
| Large-artery disease, n (%) | 37 (80.40) | NA | |
| Small-vessel disease, n (%) | 8 (17.40) | NA | |
| Undetermined, n (%) | 1 (2.20) | NA |
Smoker and drinker categories include both ex- and current smokers and drinkers.
NA: not applicable, NIHSS: National Institutes of Health Stroke Scale.
Blood flow velocity changes on both sides
The MCA mean flow velocities of stroke patients increased markedly under ECP both on the side ipsilateral to the infarct and on the contralateral side compared with baseline (p<0.001). In contrast, the mean flow velocities in healthy controls did not differ between the right and left sides at baseline and during ECP (p=0.777). Therefore, the flow velocities of healthy controls on both sides were averaged. The mean flow velocities in healthy controls were not changed by ECP (p=0.147). The CAI of patients was 4.63% on the ipsilateral side and 4.3% on the contralateral side, which were significantly higher than the values for healthy controls (mean -0.94%; p=0.005 and p<0.001, respectively) (Table 2).
Table 2. CAI in healthy controls and stroke patients.
| Velocity | Healthy controls | Stroke patients (ipsilateral side) | Stroke patients (contralateral side) |
|---|---|---|---|
| Baseline, cm/s | 57.20±13.61 | 52.78±21.23 | 51.84±15.93 |
| ECP, cm/s | 56.55±13.13 | 54.85±21.21 | 53.90±15.89 |
| p (baseline vs. ECP) | 0.147 | <0.001 | <0.001 |
| CAI, % | −0.94±3.95 | 4.63±6.59* | 4.32±4.44* |
*p<0.05 relative to control.
CAI: cerebral augmentation index, ECP: external counterpulsation.
BP changes
The SBP and DBP increased significantly during ECP compared with baseline in both stroke patients and healthy controls. After ECP, the SBP and DBP of stroke patients differed significantly from baseline, but only the SBP of healthy controls remained higher than baseline. The percentage increase in BP during ECP was comparable in stroke patients and healthy controls (Table 3).
Table 3. BP changes.
| Parameter | Stroke patients | Healthy controls | ||
|---|---|---|---|---|
| SBP | DBP | SBP | DBP | |
| Baseline BP, mm Hg | 130.22±17.42 | 85.87±14.74 | 116.43±15.38 | 77.58±7.91 |
| BP during ECP, mm Hg | 137.76±18.58 | 92.36±15.11 | 121.70±14.93 | 84.17±11.62 |
| p (baseline vs. during ECP) | <0.001 | <0.001 | 0.001 | 0.001 |
| Increase in BP during ECP from baseline, % | 5.90±5.54 | 8.06±9.10 | 4.73±4.30 | 8.28±7.76 |
| BP after ECP | 136.35±20.52 | 88.86±14.69 | 132.48±14.86 | 79.14±12.90 |
| p (baseline vs. after ECP) | <0.001 | 0.006 | <0.001 | 0.513 |
| Increase in BP after ECP from baseline, % | 4.78±8.14* | 3.93±8.18 | 14.36±8.70 | 1.79±11.35 |
*p<0.05 relative to control.
BP: blood pressure, DBP: diastolic blood pressure, ECP: external counterpulsation, SBP: systolic blood pressure.
In both stroke patients and healthy controls, the BPV at VLF and LF and the total TP, and the diastolic BPV at HF decreased markedly during ECP compared with baseline in addition to LF/HF ratio. The decreases in diastolic and systolic BPV reached 37.56% and 23.20%, respectively, at VLF, 21.15% and 12.19% at LF, 8.76% and 16.59% at HF, and 31.92% and 23.62% for TP in stroke patients, which did not differ from the corresponding values in healthy controls. However, the systolic LF/HF ratio increased during ECP, reaching almost 20% in stroke patients as well as in healthy controls. After ECP, the BPV at VLF and LF and the TP and systolic BPV at HF in both groups remained lower than baseline. There were significant differences in the decrease after ECP from baseline in the diastolic BPV of LF (p=0.012), TP (p=0.031), and the systolic BPV of LF (p=0.002), HF (p<0.001) and the TP (p=0.005) between the stroke patients and healthy controls (Table 4 and 5).
Table 4. BPV of DBP in healthy controls and stroke patients.
| BPV parameter | Subjects | Baseline | ECP | p† | Change during ECP from baseline (%) | After ECP | p‡ | Change after ECP from baseline (%) |
|---|---|---|---|---|---|---|---|---|
| VLF DBP, mm Hg | Control | 3.40 (0.83, -8.80) | 2.87 (0.66, 4.39) | 0.020 | -41.02 (-55.35, 7.83) | 0.70 (0.44, 1.25) | 0.007 | -71.16 (-86.03, -42.00) |
| Stroke | 5.40 (1.92, 18.21) | 4.27 (1.41, 9.97) | <0.001 | -37.56 (-47.04, -20.49) | 2.13 (1.27, 6.65) | <0.001 | -58.54 (-71.88, -26.01) | |
| LF DBP, mm Hg | Control | 4.61 (1.72, 12.93) | 3.94 (1.37, 9.13) | 0.024 | -24.47 (-32.35, -4.10) | 1.23 (0.75, 2.60) | 0.010 | -59.59 (-78.09, -40.35) |
| Stroke | 3.23 (1.12, 7.46) | 2.13 (1.06, 5.21) | 0.001 | -21.15 (-39.94, -1.10) | 1.94 (1.03, 3.03) | <0.001 | -37.36 (-55.26, -2.48)* | |
| HF DBP, mm Hg | Control | 0.68 (0.28, 2.00) | 0.58 (0.23, 1.26) | 0.009 | -24.18 (-32.18, -1.24) | 0.46 (0.28, 1.07) | 0.006 | -9.11 (-54.84, 11.10) |
| Stroke | 0.75 (0.43, 2.05) | 0.78 (0.48, 1.50) | 0.014 | -8.76 (-21.78, 4.22) | 1.06 (0.53, 1.91) | 0.840 | 2.95 (-23.65, 51.31) | |
| TP DBP, mm Hg | Control | 8.28 (3.25, 23.40) | 6.81 (3.37, 14.78) | 0.012 | -31.31 (-41.72, -8.48) | 2.80 (1.71, 4.01) | 0.004 | -63.80 (-78.63, -48.44) |
| Stroke | 9.74 (4.23, 27.30) | 8.24 (3.06, 17.09) | <0.001 | -31.92 (-38.34, -18.45) | 5.46 (3.4, 10.70) | <0.001 | -41.55 (-59.75, -15.64)* | |
| LF/HF, DBP | Control | 1.15 (0.60, 1.84) | 1.44 (0.67, 2.59) | 0.727 | 27.43 (5.95, 51.98) | 1.27 (0.61, 2.27) | 0.026 | 20.87 (-45.95, 90.53) |
| Stroke | 0.50 (0.39, 0.98) | 0.76 (0.43, 1.15) | 0.111 | 18.41 (-12.74, 78.87) | 0.63 (0.40, 1.05) | 0.120 | 20.69 (-12.79, 73.88) |
Data are mean (range) values.
*p<0.05 relative to control, p†: comparing between during ECP and baseline, p‡: comparing between after ECP and baseline.
BPV: blood pressure variability, DBP: diastolic blood pressure, ECP: external counterpulsation, HF: high frequency, LF: low frequency, TP: total power spectral density, VLF: very low frequency.
Table 5. BPV of SBP in healthy controls and stroke patients.
| BPV parameter | Subjects | Baseline | ECP | p† | Change during ECP from baseline (%) | After ECP | p‡ | Change after ECP from baseline (%) |
|---|---|---|---|---|---|---|---|---|
| VLF SBP, mm Hg | Control | 5.71 (2.98, 20.31) | 4.77 (1.60, 11.10) | 0.008 | -40.57 (-46.34, -6.35) | 1.50 (0.78, 3.12) | 0.001 | -73.86 (-85.82, -64.30) |
| Stroke | 11.43 (4.62, 29.82) | 6.70 (3.43, 22.34) | <0.001 | -23.20 (-45.17, -5.16) | 5.38 (2.24, 13.27) | <0.001 | -53.25 (-69.58, -20.92) | |
| LF SBP, mm Hg | Control | 7.59 (3.81, 18.05) | 6.80 (2.39, 16.97) | 0.007 | -28.06 (-38.13, -7.20) | 2.15 (1.43, 5.24) | 0.011 | -59.89 (-77.90, -45.95) |
| Stroke | 5.09 (2.32, 9.34) | 5.35 (2.10, 8.30) | 0.013 | -12.19 (-28.49, 0.91) | 3.41 (1.74, 5.89) | <0.001 | -29.94 (-51.80, -9.20)* | |
| HF SBP, mm Hg | Control | 1.80 (0.90, 6.00) | 1.33 (0.55, 4.64) | 0.331 | -27.02 (-31.87, -23.69) | 0.80 (0.47, 1.79) | 0.010 | -59.27 (-70.86, -49.30) |
| Stroke | 2.28 (1.48, 6.58) | 1.86 (1.14, 4.04) | <0.001 | -16.59 (-26.98, -9.43) | 1.96 (1.21, 3.41) | <0.001 | -22.42 (-41.96, -1.62)* | |
| TP SBP, mm Hg | Control | 13.18 (8.72, 43.39) | 13.30 (4.86, 32.10) | 0.001 | -31.44 (-38.54, -24.19) | 4.63 (2.72, 9.57) | 0.001 | -71.13 (-75.87, -55.93) |
| Stroke | 18.41 (9.90, 45.07) | 15.52 (6.60, 32.71) | <0.001 | -23.62 (-33.97, -10.74) | 10.67 (6.18, 19.83) | <0.001 | -44.56 (-61.57, -22.52)* | |
| LF/HF, SBP | Control | 0.97 (0.56, 1.71) | 1.33 (0.63, 2.27) | 0.876 | 22.87 (6.85, 50.17) | 1.12 (0.79, 1.88) | 0.331 | 50.83 (-25.50, 103.66) |
| Stroke | 0.45 (0.32, 0.93) | 0.65 (0.38, 1.15) | 0.074 | 23.30 (-15.92, 80.43) | 0.62 (0.33, 1.04) | 0.049 | 27.11 (-14.36, 77.61) |
Data are mean (range) values.
*p<0.05 relative to control, p†: comparing between during ECP and baseline, p‡: comparing between after ECP and baseline.
BPV: blood pressure variability, ECP: external counterpulsation, HF: high frequency, LF: low frequency, SBP: systolic blood pressure, TP: total power spectral density, VLF: very low frequency.
Correlation between CAI and BPV changes during ECP from baseline
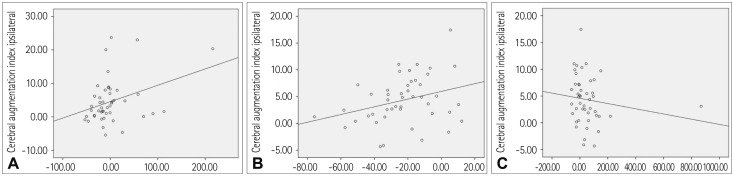
In the stroke patients, during ECP, the CAI on the ipsilateral side presented a borderline significant trend of a positive correlation with an HF diastolic change in BPV (r=0.283, p=0.057) (Fig. 1A). The CAI on the contralateral side was positively correlated with systolic BP TP change (r=0.312, p=0.035) (Fig. 1B). The CAI on the contralateral side showed a borderline significant trend of a negative correlation with the LF/HF SBP change (r=-0.281, p=0.059) (Fig. 1C). In healthy controls, there was no significant correlation between CAI and any changes in the BPV parameters during ECP from baseline.
Fig. 1. Correlation between CAI and BPV changes during ECP from baseline. A: Correlation between CAI on the ipsilateral side and the percentage decrease in the HF DBP during ECP from baseline. B: Correlation between CAI on the contralateral side and the percentage decrease in TP of the SBP during ECP from baseline. C: Correlation between CAI on the contralateral side and the percentage decrease in LF/HF of the SBP during ECP from baseline. CAI: cerebral augmentation index, DBP: diastolic blood pressure, ECP: external counterpulsation, HF: high frequency, LF: low frequency, SBP: systolic blood pressure.
DISCUSSION
This study first found that ECP reduced the beat-to-beat BPV in stroke patients and healthy controls. The cerebrovascular reactivity in response to the ECP intervention stabilized within 1 minute.8 Therefore, we performed open-label ECP treatment for 3 minutes and monitored real-time changes in cerebral blood flow in this study. ECP increased the mean MCA flow velocities on both cerebral sides in ischemic stroke patients, but it did not change the flow velocities in healthy controls, although BP was elevated, which is consistent with our previous studies.10 In addition, the CAI on the ipsilateral and contralateral sides showed a borderline significant trend of a positive correlation with HF diastolic BPV changes and the TP of systolic BPV change during ECP from baseline, respectively.
ECP treatment usually takes 35 hours (in daily 1-hour sessions) and lasts for 7 weeks. The most-common adverse effects of ECP are pain in the legs and lower back, hematuria, and skin abrasion. The Multicenter Study of Enhanced External Counterpulsation (MUST-EECP) trial found that most patients tolerated ECP treatment well and were free from limiting side effects.21 The potential risks of increasing BP during acute stroke may include intracerebral hemorrhage and aggravation of edema. Sustained severe hypertension in our exclusion criteria and real-time BP monitoring during ECP are helpful for reducing the risks of these hypertension-related events. All patients tolerated the ECP treatment well and were free of limiting side effects in our study.
The cerebral hemodynamic changes induced by ECP in our study might be partially attributable to the effect of ECP on the collateral circulation. We are aware of two main ways to enhance the collateral perfusion: 1) opening or expanding the existing vessels, and 2) forming new vessels. Several studies found that ECP could increase the arterial wall shear stress via different pathophysiological processes.22,23 Such changes in the release of shear-dependent vasomediators as well as augmentation of the arterial pressure may help to open the existing collateral channels, which is the simplest way to increase the collateral perfusion. On the other hand, an increase in shear stress induced by ECP may influence angiogenesis, which may in turn also improve the collateral perfusion. Further analysis of the acquired imaging data will require animal experiments, which may provide evidence for which cerebral collateral channel is more important during the ECP procedure in ischemic stroke patients.
The SBP and DBP increased significantly compared with baseline in both healthy controls and patients. These results are mostly consistent with previous investigations. Shimizu et al.24 showed that ECP increases the venous return and cardiac output during ECP in addition to causing diastolic augmentation and systolic unloading. Meanwhile, our results further confirmed that ECP provides diastolic augmentation and systolic unloading through enhancing venous return by squeezing the venous system.23
Fluctuations in the arterial pressure occur across diverse timescales, ranging from beat-to-beat to day-to-day variabilities. All of these variabilities are associated with a multitude of overlapping and interacting physiological processes.25 To the best of our knowledge, beat-to-beat or minute-to-minute variability quantifies physiological mechanisms operating within this timescale, such as the cardiac cycle (e.g., approx. ≥1 Hz), respiratory frequency (e.g., HF, 0.15–0.4 Hz), sympathetic/baroreflex modulation (e.g., LF, 0.04–0.15 Hz), and myogenic activity (e.g., VLF, 0.004–0.04 Hz).18,26,27,28,29 In our study, most of the beat-to-beat BPV parameters decreased during ECP in both healthy controls and ischemic stroke patients including the BP at VLF, LF, and HF, the TP of the DBP in the healthy controls, and the TP in the patients.
A complicated mechanism might underlie the decreased BPV induced by ECP. Kern et al.30,31 showed that ECP-induced increases in blood flow translate into enhanced endothelial shear stress, which represents a major stimulus for endothelial nitric oxide release and vasodilation.32,33,34 Shear stress also modulates the release of endothelin-1, since sustained exposure of the endothelium to low levels of shear stress stimulates endothelin-1 release, whereas longer exposure to higher shear stress levels is associated with a reduction of endothelial endothelin-1 release.34,35 On the other hand, there is increasing evidence for rapid beat-to-beat oscillations of BP being attributable to the interplay of different cardiovascular control systems, including the baroreceptor reflex, the RAS, the vascular myogenic response, and the release of nitric oxide from the endothelium.18 We speculate that the decreased beat-to-beat BPV induced by ECP is attributable to the enhancement of endothelial function and the release of nitric oxide.
The different components of BPV parameters could be controlled by different mechanisms, as illustrated above. Stauss18 reported that BPV was lower in stroke-prone hypertensive rats than in stroke-resistant hypertensive rats, reflective of reduced cerebrovascular myogenic function that usually protects the brain from hemorrhagic stroke. Some investigations have suggested that LF variability influences the arterial pressure in acute orthostatic intolerance, which is associated with enhanced vasomotor activity mediated by variations in sympathetic activity.18 BPV at HF is mainly influenced by changes in cardiac output.36 This is consistent with the main mechanism of ECP being able to change the cardiac output to enhance the cerebral perfusion. ECP could affect neurohormonal systems to decrease BPV in stroke patients, and thus improve the clinical progress of stroke patients receiving ECP treatment.
We found that the CAI on both sides showed a borderline significant trend of a positive correlation with certain BPV parameters. The autonomic system is damaged in stroke patients, which leads to impaired arterial baroreflex function, changes in humoral factors, and changes in ventilatory parameters.18,37 Increased BPV is a marker of autonomic dysfunction. This might indicate that BPV is an important determinant affecting the cerebral blood flow and perfusion to the ischemic penumbra.25 Our recent study demonstrated that the cerebral augmentation effect of ECP as measured by the CAI in ischemic stroke patients operates via the pathway of impaired cerebral autoregulation rather than by the well-established vasoreactivity to breath-holding.38 The positive correlation may reflect the association between the autonomic dysfunction and impaired cerebral autoregulation that follows ischemic stroke. ECP could ameliorate impaired cerebral autoregulation by decreasing the beat-to-beat BPV in stroke patients.
This study was subject to several limitations. First, the sample was relatively small. Second, the differences in the age and sex distributions between healthy controls and stroke patients may have contributed to their distinct hemodynamic responses to ECP. However, we mainly observed changes in CAI and BPV within individuals in the two groups. In this study we recruited more male participants, because the prevalence of stroke in China is higher in men than in women,39 and female subjects are more likely to have an insufficient bilateral temporal bone window for insonation due to the low density of the temporal bone.40 Third, the beat-to-beat BPV during ECP was monitored for only 3 minutes instead of applying the standard 35 daily 1-hour ECP treatment sessions. The effect of applying more ECP sessions on the beat-to-beat BPV in ischemic stroke remains unknown; we intend to explore this point in further studies. Stronger evidence for an increased BP during ECP could be obtained if an aortic root arterial pressure line or a peripheral arterial pressure line is used. Our study focused on the hemodynamic effects of ECP on BPV, which is an important factor in the progression of stroke, and the functional outcomes of the ECP-treated patients were not considered. However, there is an ongoing randomized controlled trial at our center involving conventional medical treatments of stroke patients as controls to investigate the effects of ECP on ischemic stroke patients. The results for functional outcomes from that study will be more convincing. Lastly, the BPV was assessed using 3-minute beat-to-beat monitoring instead of hour-to-hour or day-to-day measurements; however, the beat-to-beat and day-to-day BPVs reportedly have similar physiological correlates.41
In conclusion, ECP increases BP and the cerebral blood flow but decreases the beat-to-beat BPV in patients with ischemic stroke. ECP can ameliorate impaired cerebral autoregulation by decreasing the beat-to-beat BPV in stroke patients.
Acknowledgements
The authors thank the Chinese University of Hong Kong (Focused Investment Scheme B) and the Institute of Innovative Medicine, Chinese University of Hong Kong; the SH Ho Cardiovascular Disease and Stroke Center, Institute of Vascular Medicine, Chinese University of Hong Kong; and the Chinese University of Hong Kong Focused Innovative Scheme (Grant No. 1902062). This study was also supported by grants from the National Natural Science Foundation of China (No. 81371297) and the Innovation and Technology Funding, Hong Kong (No. GHP/008/11SZ).
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Lawes CM, Vander Hoorn S, Rodgers A International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 2.Aiyagari V, Gorelick PB. Management of blood pressure for acute and recurrent stroke. Stroke. 2009;40:2251–2256. doi: 10.1161/STROKEAHA.108.531574. [DOI] [PubMed] [Google Scholar]
- 3.Ravenni R, Jabre JF, Casiglia E, Mazza A. Primary stroke prevention and hypertension treatment: which is the first-line strategy? Neurol Int. 2011;3:e12. doi: 10.4081/ni.2011.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlöf B, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–480. doi: 10.1016/S1474-4422(10)70066-1. [DOI] [PubMed] [Google Scholar]
- 5.Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet. 2010;375:906–915. doi: 10.1016/S0140-6736(10)60235-8. [DOI] [PubMed] [Google Scholar]
- 6.Stead LG, Gilmore RM, Vedula KC, Weaver AL, Decker WW, Brown RD., Jr Impact of acute blood pressure variability on ischemic stroke outcome. Neurology. 2006;66:1878–1881. doi: 10.1212/01.wnl.0000219628.78513.b5. [DOI] [PubMed] [Google Scholar]
- 7.Dawson SL, Manktelow BN, Robinson TG, Panerai RB, Potter JF. Which parameters of beat-to-beat blood pressure and variability best predict early outcome after acute ischemic stroke? Stroke. 2000;31:463–468. doi: 10.1161/01.str.31.2.463. [DOI] [PubMed] [Google Scholar]
- 8.Sykora M, Diedler J, Rupp A, Turcani P, Rocco A, Steiner T. Impaired baroreflex sensitivity predicts outcome of acute intracerebral hemorrhage. Crit Care Med. 2008;36:3074–3079. doi: 10.1097/CCM.0b013e31818b306d. [DOI] [PubMed] [Google Scholar]
- 9.Bonetti PO, Barsness GW, Keelan PC, Schnell TI, Pumper GM, Kuvin JT, et al. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol. 2003;41:1761–1768. doi: 10.1016/s0735-1097(03)00329-2. [DOI] [PubMed] [Google Scholar]
- 10.Lin W, Xiong L, Han J, Leung TW, Soo YO, Chen X, et al. External counterpulsation augments blood pressure and cerebral flow velocities in ischemic stroke patients with cerebral intracranial large artery occlusive disease. Stroke. 2012;43:3007–3011. doi: 10.1161/STROKEAHA.112.659144. [DOI] [PubMed] [Google Scholar]
- 11.Linnemeier G. Enhanced external counterpulsation--a therapeutic option for patients with chronic cardiovascular problems. J Cardiovasc Manag. 2002;13:20–25. [PubMed] [Google Scholar]
- 12.Zheng ZS, Yu LQ, Cai SR, Kambic H, Li TM, Ma H, et al. New sequential external counterpulsation for the treatment of acute myocardial infarction. Artif Organs. 1984;8:470–477. doi: 10.1111/j.1525-1594.1984.tb04323.x. [DOI] [PubMed] [Google Scholar]
- 13.Han JH, Leung TW, Lam WW, Soo YO, Alexandrov AW, Mok V, et al. Preliminary findings of external counterpulsation for ischemic stroke patient with large artery occlusive disease. Stroke. 2008;39:1340–1343. doi: 10.1161/STROKEAHA.107.500132. [DOI] [PubMed] [Google Scholar]
- 14.Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003;229:340–346. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- 15.Wong KS, Li H, Chan YL, Ahuja A, Lam WW, Wong A, et al. Use of transcranial Doppler ultrasound to predict outcome in patients with intracranial large-artery occlusive disease. Stroke. 2000;31:2641–2647. doi: 10.1161/01.str.31.11.2641. [DOI] [PubMed] [Google Scholar]
- 16.Michaels AD, McCullough PA, Soran OZ, Lawson WE, Barsness GW, Henry TD, et al. Primer: practical approach to the selection of patients for and application of EECP. Nat Clin Pract Cardiovasc Med. 2006;3:623–632. doi: 10.1038/ncpcardio0691. [DOI] [PubMed] [Google Scholar]
- 17.Parati G, Saul JP, Di Rienzo M, Mancia G. Spectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation. A critical appraisal. Hypertension. 1995;25:1276–1286. doi: 10.1161/01.hyp.25.6.1276. [DOI] [PubMed] [Google Scholar]
- 18.Stauss HM. Identification of blood pressure control mechanisms by power spectral analysis. Clin Exp Pharmacol Physiol. 2007;34:362–368. doi: 10.1111/j.1440-1681.2007.04588.x. [DOI] [PubMed] [Google Scholar]
- 19.Langager AM, Hammerberg BE, Rotella DL, Stauss HM. Very low-frequency blood pressure variability depends on voltage-gated L-type Ca2+ channels in conscious rats. Am J Physiol Heart Circ Physiol. 2007;292:H1321–H1327. doi: 10.1152/ajpheart.00874.2006. [DOI] [PubMed] [Google Scholar]
- 20.Malliani A, Pagani M, Lombardi F, Cerutti S. Cardiovascular neural regulation explored in the frequency domain. Circulation. 1991;84:482–492. doi: 10.1161/01.cir.84.2.482. [DOI] [PubMed] [Google Scholar]
- 21.Arora RR, Chou TM, Jain D, Fleishman B, Crawford L, McKiernan T, et al. The multicenter study of enhanced external counterpulsation (MUST-EECP): effect of EECP on exercise-induced myocardial ischemia and anginal episodes. J Am Coll Cardiol. 1999;33:1833–1840. doi: 10.1016/s0735-1097(99)00140-0. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, He X, Chen X, Ma H, Liu D, Luo J, et al. Enhanced external counterpulsation inhibits intimal hyperplasia by modifying shear stress responsive gene expression in hypercholesterolemic pigs. Circulation. 2007;116:526–534. doi: 10.1161/CIRCULATIONAHA.106.647248. [DOI] [PubMed] [Google Scholar]
- 23.Barsness GW. Enhanced external counterpulsation in unrevascularizable patients. Curr Interv Cardiol Rep. 2001;3:37–43. [PubMed] [Google Scholar]
- 24.Shimizu T, Kyo S, Morizumi S, Ando T, Gon S, Suematsu Y. Effect of external counterpulsation on cardiac work following cardiac surgery: implications of the mechanism responsible for clinical benefits. J Cardiol. 2012;59:84–90. doi: 10.1016/j.jjcc.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Rickards CA, Tzeng YC. Arterial pressure and cerebral blood flow variability: friend or foe? A review. Front Physiol. 2014;5:120. doi: 10.3389/fphys.2014.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown TE, Beightol LA, Koh J, Eckberg DL. Important influence of respiration on human R-R interval power spectra is largely ignored. J Appl Physiol (1985) 1993;75:2310–2317. doi: 10.1152/jappl.1993.75.5.2310. [DOI] [PubMed] [Google Scholar]
- 27.Cooke WH, Cox JF, Diedrich AM, Taylor JA, Beightol LA, Ames JE, 4th, et al. Controlled breathing protocols probe human autonomic cardiovascular rhythms. Am J Physiol. 1998;274(2 Pt 2):H709–H718. doi: 10.1152/ajpheart.1998.274.2.h709. [DOI] [PubMed] [Google Scholar]
- 28.Julien C. The enigma of Mayer waves: facts and models. Cardiovasc Res. 2006;70:12–21. doi: 10.1016/j.cardiores.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 29.Tzeng YC, Chan GS, Willie CK, Ainslie PN. Determinants of human cerebral pressure-flow velocity relationships: new insights from vascular modelling and Ca2+ channel blockade. J Physiol. 2011;589(Pt 13):3263–3274. doi: 10.1113/jphysiol.2011.206953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kern MJ, Aguirre FV, Tatineni S, Penick D, Serota H, Donohue T, et al. Enhanced coronary blood flow velocity during intraaortic balloon counterpulsation in critically ill patients. J Am Coll Cardiol. 1993;21:359–368. doi: 10.1016/0735-1097(93)90676-r. [DOI] [PubMed] [Google Scholar]
- 31.Kern MJ, Aguirre F, Bach R, Donohue T, Siegel R, Segal J. Augmentation of coronary blood flow by intra-aortic balloon pumping in patients after coronary angioplasty. Circulation. 1993;87:500–511. doi: 10.1161/01.cir.87.2.500. [DOI] [PubMed] [Google Scholar]
- 32.Corson MA, James NL, Latta SE, Nerem RM, Berk BC, Harrison DG. Phosphorylation of endothelial nitric oxide synthase in response to fluid shear stress. Circ Res. 1996;79:984–991. doi: 10.1161/01.res.79.5.984. [DOI] [PubMed] [Google Scholar]
- 33.Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, Zeiher AM. Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- 34.Davies PF. Flow-mediated endothelial mechanotransduction. Physiol Rev. 1995;75:519–560. doi: 10.1152/physrev.1995.75.3.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuchan MJ, Frangos JA. Shear stress regulates endothelin-1 release via protein kinase C and cGMP in cultured endothelial cells. Am J Physiol. 1993;264(1 Pt 2):H150–H156. doi: 10.1152/ajpheart.1993.264.1.H150. [DOI] [PubMed] [Google Scholar]
- 36.Janssen BJ, Oosting J, Slaaf DW, Persson PB, Struijker-Boudier HA. Hemodynamic basis of oscillations in systemic arterial pressure in conscious rats. Am J Physiol. 1995;269(1 Pt 2):H62–H71. doi: 10.1152/ajpheart.1995.269.1.H62. [DOI] [PubMed] [Google Scholar]
- 37.Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–155. doi: 10.1038/nrcardio.2013.1. [DOI] [PubMed] [Google Scholar]
- 38.Lin W, Xiong L, Han J, Leung T, Leung H, Chen X, et al. Hemodynamic effect of external counterpulsation is a different measure of impaired cerebral autoregulation from vasoreactivity to breath-holding. Eur J Neurol. 2014;21:326–331. doi: 10.1111/ene.12314. [DOI] [PubMed] [Google Scholar]
- 39.Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6:456–464. doi: 10.1016/S1474-4422(07)70004-2. [DOI] [PubMed] [Google Scholar]
- 40.Wijnhoud AD, Franckena M, van der Lugt A, Koudstaal PJ, Dippel ED. Inadequate acoustical temporal bone window in patients with a transient ischemic attack or minor stroke: role of skull thickness and bone density. Ultrasound Med Biol. 2008;34:923–929. doi: 10.1016/j.ultrasmedbio.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 41.Webb AJ, Rothwell PM. Physiological correlates of beat-to-beat, ambulatory, and day-to-day home blood pressure variability after transient ischemic attack or minor stroke. Stroke. 2014;45:533–538. doi: 10.1161/STROKEAHA.113.003321. [DOI] [PubMed] [Google Scholar]