Abstract
Purpose
Docetaxel-based chemotherapy (DTX) improves overall survival (OS) of men with metastatic castration-resistant prostate cancer (mCRPC). Considering the potential existence of androgen receptors that remain active at this stage, we aimed to assess the impact of the combined use of androgen deprivation therapy (ADT) with DTX for mCRPC.
Materials and Methods
We performed a single-institutional retrospective analysis of patients with mCRPC who received either DTX alone (DTX group, n=21) or concurrent DTX and ADT (DTX+ADT group, n=26) between August 2006 and February 2014. All patients received DTX doses of 75 mg/m2 every three weeks for at least three cycles. In the DTX+ADT group, all patients used luteinizing hormone releasing hormone agonist continuously as a concurrent ADT.
Results
The median follow-up period was 24.0 months (interquartile range 12.0–37.0) for the entire cohort. The median radiographic progression-free survival (rPFS) was 9.0 months and 6.0 months in the DTX+ADT and DTX groups, respectively (log-rank p=0.036). On multivariable Cox regression analysis, concurrent administration of ADT was the only significant predictor of rPFS [hazard ratio (HR)=0.525, 95% confidence intervals (CI) 0.284–0.970, p=0.040]. The median OS was 42.0 and 38.0 months in the DTX+ADT and DTX groups, respectively (log-rank p=0.796). On multivariable analysis, hemoglobin level at the time of DTX initiation was associated with OS (HR=0.532, 95% CI 0.381–0.744, p<0.001).
Conclusion
In chemotherapy-naive patients with mCRPC, the combined use of ADT with DTX improved rPFS. Our result suggests that the concurrent administration of ADT and DTX is superior to DTX alone.
Keywords: Prostatic neoplasms, castration-resistant; neoplasm metastasis; disease-free survival; docetaxel; drug therapy, combination; gonadotropin-releasing hormone
INTRODUCTION
Prostate cancer (PCa) is the second most common cancer and the fifth leading cause of cancer-related deaths in males worldwide.1 Death from PCa is typically the result of castration-resistant prostate cancer (CRPC), a clinical state in which disease progression occurs despite maintenance of castrate serum testosterone levels.2,3 According to recent analyses, approximately 84% of CRPC patients present with metastatic disease at the time of diagnosis,4 and patients with metastatic CRPC (mCRPC) are expected to survive up to 18 to 19 months.5
CRPC was once regarded as androgen-insensitive or hormone-refractory; however, it is now widely accepted that androgen receptor (AR) signaling activity is persistent in the prostate in CRPC and that residual androgens continue to drive AR signaling activity.6,7,8,9,10 Various molecular studies have shown that tumor progression in CRPC is related to AR-associated signaling mechanisms.11 Reported mechanisms include AR overexpression and amplification, AR mutations, and increased AR ligand expression in the surrounding stroma. According to these mechanisms, the increase in AR protein sensitizes PCa cells to respond to low levels of ligands,12,13 and AR mutations are associated with production of a receptor that is more sensitive to native ligands.14 In this regard, discontinuation of androgen deprivation therapy (ADT) in patients with CRPC who have not undergone surgical castration could result in tumor growth and proliferation. However, there are drawbacks to maintaining ADT. It has been reported that continuation of ADT is associated with serious health problems–coronary heart disease, myocardial infarction, fracture, anemia, and diabetes–and thus can affect the survival outcomes of patients.15,16,17,18
In terms of survival advantage, the benefits of concurrent administration of ADT in CRPC patients under cytotoxic chemotherapy are debatable. Retrospective reviews of trials by the Eastern Cooperative Oncology Group (ECOG) and the Southwest Oncology Group (SWOG) have been performed, and they provided conflicting results with regard to survival.19,20 Due to the absence of tangible results from related studies, concurrent administration of luteinizing hormone-releasing hormone agonist for CRPC patients under cytotoxic chemotherapy cannot be reimbursed by the Korean National Health Insurance system under the present guidelines. Considering the potential presence of ARs that remain active at this stage of the disease, we sought to assess the impact of the combined use of ADT and cytotoxic chemotherapy, particularly docetaxel-based chemotherapy (DTX) for mCRPC.
MATERIALS AND METHODS
Study sample
This retrospective study included data from a total of 199 consecutive patients with mCRPC who received DTX at the Department of Urology, Yonsei University Health System (Seoul, Korea), between August 2006 and February 2014. Collection of the retrospective data used in the study was approved by the Institutional Ethics Committee after reviewing the protocol and procedures employed (2009-0131-001). The study was carried out in lieu of a formal ethics committee and followed the principles of the Helsinki Declaration.
Patients with the following criteria were included in the present analysis: 1) histologically confirmed adenocarcinoma of the prostate with clinical or radiologic evidence of metastatic disease and defined as CRPC according to the European Association of Urology guidelines 2011,21 2) ECOG performance status ≤2, 3) computed tomography or magnetic resonance imaging, and radionuclide bone scans performed at every three cycles of DTX, 4) serum prostate specific antigen (PSA) levels measured at each cycle, and 5) adequate bone marrow and organ function. Patients were excluded if they received cytotoxic chemotherapy or radioisotope therapy before the administration of docetaxel or if they had incomplete follow-up data, reduced doses of docetaxel, serious or uncontrolled concomitant medical illness, history of other cancer within five years, or evidence of central nervous system metastasis. Additionally, patients who received less than three cycles of DTX were excluded due to the possibility of a PSA surge.
Of the 199 mCRPC patients who received DTX, 47 fulfilled the criteria described above, and 152 patients were excluded for the following reasons: prior cytotoxic chemotherapy (n=23), dose reduction of docetaxel (n=82), combination with immunotherapy or other cytotoxic chemotherapy agents (n=25), and less than three cycles of DTX (n=22). The 47 included patients were divided into two groups: those who received DTX with ADT (DTX+ADT group, n=26), and those who received DTX without ADT (DTX group, n=21).
Medical records were reviewed for the following characteristics: patient age, body mass index (BMI), Gleason score, tumornode-metastasis classification of the American Joint Committee on Cancer,22 neoadjuvant treatments, responses to prior antiandrogen therapies, ECOG performance status, baseline hemoglobin (Hb), neutrophil-to-lymphocyte ratio, albumin, PSA levels, presence of visceral metastases, and extent of the disease.
Treatment
All patients received docetaxel plus prednisone therapy with or without ADT. The regimen consisted of docetaxel (75 mg/m2), which was administered through intravenous infusion once on day 1 every 3 weeks, plus oral prednisolone 5 mg twice daily starting on day 1 and continuing throughout the treatment.
DTX continued until uncontrolled toxicity, disease progression, planned termination of individual patient, death, or treatment refusal by the patient. The National Cancer Institute Common Toxicity Criteria version 4.0 was used to evaluate the toxicity during each cycle.23
Study endpoints
The primary endpoints were biochemical progression-free survival (bPFS) and radiographic progression-free survival (rPFS). The secondary endpoint was overall survival (OS). Biochemical progression was defined as a >50% increase from the PSA nadir, with a minimum increase of 5 ng/mL.24 The PSA nadir was defined as the lowest PSA level achieved during DTX. The time to biochemical progression was assessed between the day of treatment initiation and biochemical progression. The time to radiographic progression was defined as the time interval from the day of DTX initiation to the first occurrence of either progression on imaging studies. Progression on bone scans was assessed according to the Prostate Cancer Working Group (PCWG)-2 criteria,25 and soft tissue progression was evaluated with reference to the Response Evaluation Criteria in Solid Tumors version 1.1.26 OS was calculated from the date of DTX initiation to that of death from any cause. For all patients, survival and cause of death were investigated based on the National Cancer Registry Database or institutional electronic medical records.
Statistical analysis
The descriptive values of the variables are expressed as median and interquartile range (IQR) according to the results of normality testing. Differences in baseline characteristics were compared between groups using a chi-square test or Fisher's exact test for categorical variables and the Mann-Whitney U test for continuous variables.
rPFS, OS, and bPFS were calculated and analyzed using the Kaplan-Meier method and the log-rank test. Univariable and multivariable analyses used Cox proportional hazards models. Factors associated with progression or mortality with a p value of less than 0.20 on univariable analyses were entered in the multivariable model, and nonsignificant factors were removed by means of a backward-elimination procedure. The hazard ratio (HR) and 95 % confidence intervals (CI) were estimated for each variable.
All of the tests were two-sided, and p<0.05 was considered to be statistically significant. All statistical analyses were performed using SPSS version 18 (SPSS Inc., Chicago, IL, USA).
RESULTS
Patient demographics are presented in Table 1. Both groups were similar in terms of age, BMI, pretreatment laboratory values, stage and grade, extent of metastasis, duration of ADT prior to DTX, response to previous ADT, and number of DTX cycles received. As shown in Table 2, there was no difference in adverse events between the two groups. The reasons for discontinuation of treatment are outlined in Table 3.
Table 1. Patient Demographics.
| DTX | DTX+ADT | p value | |
|---|---|---|---|
| Number of patients | 21 | 26 | NS |
| Thrombocytopenia | 69 (67-74) | 68 (63-72) | 0.459 |
| BMI (kg/m2) | 24.0 (22.5-25.4) | 24.2 (23.3-26.6) | 0.708 |
| ECOG PS ≥1, n (%) | 8 (38.1) | 15 (57.7) | 0.181 |
| Gleason score at diagnosis, n (%) | |||
| ≤8 | 8 (38.1) | 8 (30.8) | 0.598 |
| ≥9 | 13 (61.9) | 18 (69.2) | 0.598 |
| Clinical T stage at diagnosis, n (%) | |||
| ≤T3 | 14 (66.7) | 15 (57.7) | 0.529 |
| T4 | 7 (33.3) | 11 (42.3) | 0.529 |
| Clinical N stage at diagnosis, n (%) | |||
| N1 | 13 (61.9) | 14 (53.8) | 0.579 |
| Prior treatment, n (%) | |||
| Radical prostatectomy | 5 (23.8) | 6 (23.1) | 1.000 |
| Definitive EBRT | 0 (0.0) | 1 (3.8) | 1.000 |
| Palliative EBRT | 7 (33.3) | 9 (34.6) | 0.927 |
| Duration of ADT prior to DTX | 12 (7-32.5) | 10.5 (7-31.5) | 0.464 |
| Response to primary ADT | |||
| PSA nadir (ng/mL) | 2.3 (0.4-14.5) | 0.7 (0.2-7.8) | 0.380 |
| PSA velocity (ng/mL/yr) | 28.9 (6.7-252.1) | 33.5 (14.6-158.9) | 0.906 |
| PSA doubling time (ng/mL/yr) | 0.16 (0.11-0.42) | 0.18 (0.09-0.30) | 0.700 |
| Laboratory values | |||
| PSA at diagnosis (ng/mL) | 68.9 (29.7-449.0) | 85.2 (25.4-262.0) | 0.881 |
| PSA at CRPC diagnosis (ng/mL) | 41.5 (26.9-112.0) | 42.2 (28.8-173.4) | 0.966 |
| Hb (g/dL) | 11.6 (10.8-12.9) | 11.9 (10.9-13.0) | 0.676 |
| NLR | 2.06 (1.39-3.64) | 2.28 (1.57-4.13) | 0.341 |
| Albumin (g/dL) | 4.1 (3.8-4.6) | 4.2 (3.6-4.4) | 0.772 |
| Number of DTX cycles | 7 (6-11) | 9.5 (5-12) | 0.643 |
| Extent of disease at CRPC diagnosis, n (%) | |||
| Bone metastasis | 18 (85.7) | 25 (96.2) | 0.311 |
| Lymph node metastasis | 15 (71.4) | 17 (65.4) | 0.659 |
| Lung or liver metastasis | 1 (4.8) | 1 (3.8) | 1.000 |
DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; EBRT, external-beam radiation therapy; PSA, prostate-specific antigen; CRPC, castration-resistant prostate cancer; Hb, hemoglobin; NLR, neutrophil-tolymphocyte ratio.
Data are median (interquartile range) and number (%).
Table 2. Adverse Events during DTX.
| Overall | DTX | DTX+ADT | p value | |
|---|---|---|---|---|
| CTCAE grade ≤2, n (%) | ||||
| Thrombocytopenia | 1 (2.1) | 1 (4.8) | 0 (0.0) | 0.266 |
| Anemia | 8 (17.0) | 3 (14.3) | 5 (19.2) | 0.657 |
| Aspartate/alanine aminotransferase increased | 14 (29.8) | 5 (23.8) | 9 (34.6) | 0.426 |
| Nausea & vomiting | 29 (61.7) | 15 (71.4) | 14 (53.8) | 0.223 |
| Diarrhea | 9 (19.1) | 6 (28.6) | 3 (11.5) | 0.144 |
| Constipation | 13 (27.7) | 8 (38.1) | 5 (19.2) | 0.155 |
| Peripheral neuropathy | 7 (14.9) | 3 (14.3) | 4 (15.4) | 0.917 |
| Dry mouth | 14 (29.8) | 8 (38.1) | 6 (23.1) | 0.268 |
| Dry eye | 12 (25.5) | 7 (33.3) | 5 (19.2) | 0.275 |
| Edema limbs | 6 (12.8) | 2 (9.5) | 4 (15.4) | 0.554 |
| Myalgia | 11 (23.4) | 6 (28.6) | 5 (19.2) | 0.457 |
| CTCAE grade ≥3, n (%) | ||||
| Febrile neutropenia | 8 (17.0) | 4 (19.0) | 4 (15.4) | 0.742 |
| Anemia | 1 (2.1) | 0 (0.0) | 1 (3.8) | 0.369 |
| Nausea & vomiting | 2 (4.3) | 2 (9.5) | 0 (0.0) | 0.112 |
| Peripheral neuropathy | 2 (4.3) | 0 (0.0) | 2 (7.7) | 0.199 |
| Fatigue | 2 (4.3) | 1 (4.8) | 1 (3.8) | 0.878 |
CTCAE, common terminology criteria for adverse events; DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy.
Table 3. Reasons for Discontinuation of DTX.
| Overall | DTX | DTX+ADT | p value | |
|---|---|---|---|---|
| Treatment toxicity, n (%) | 15 (31.9) | 7 (33.3) | 8 (30.8) | 0.851 |
| Neutropenia | 8 (17.0) | 4 (19.0) | 4 (15.4) | |
| Anemia | 1 (2.1) | 0 (0.0) | 1 (3.8) | |
| Nausea & vomiting | 2 (4.3) | 2 (9.5) | 0 (0.0) | |
| Peripheral neuropathy | 2 (4.3) | 0 (0.0) | 2 (7.7) | |
| Fatigue | 2 (4.3) | 1 (4.8) | 1 (3.8) | |
| Disease progression, n (%) | 19 (40.4) | 10 (47.6) | 9 (34.6) | 0.366 |
| Planned, n (%) | 9 (19.1) | 3 (14.3) | 6 (23.1) | 0.711 |
| Death, n (%) | 2 (4.3) | 0 (0.0) | 2 (7.7) | 0.495 |
| Patient refusal, n (%) | 2 (4.3) | 1 (4.8) | 1 (3.8) | 1.000 |
DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy.
The median follow-up period was 24.0 months (IQR 12.0–37.0) for the entire cohort, 23.0 months (IQR 13.5–32.5) for the DTX+ADT group, and 24.0 months (IQR 11.5–40.0) for the DTX group. Overall, 22 patients expired at the final follow-up, and the reason for patient mortality was PCa-related death in all patients.
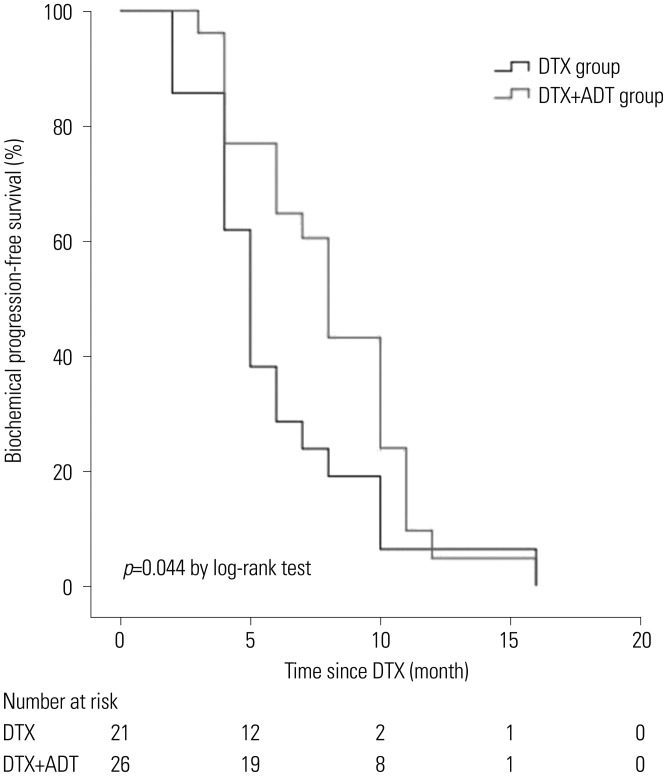
The median bPFS was 8.0 months (95% CI 6.854–9.146) in the DTX+ADT group and 5.0 months (95% CI 4.128–5.872) in the DTX group. Kaplan-Meier analysis revealed a significant association between concurrent administration of ADT and prolonged bPFS (log-rank p=0.044) (Fig. 1). In univariable and multivariable Cox regression analyses, the number of DTX cycles was the only significant predictor of bPFS (Table 4).
Fig. 1. Kaplan-Meier curve of biochemical progression-free survival. DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy.
Table 4. Associated Baseline Factors of Biochemical Progression-Free Survival via Univariable and Multivariable Analyses.
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | p value | HR | (95% CI) | p value | |
| Age | 1.009 | (0.968-1.052) | 0.680 | |||
| BMI | 0.938 | (0.831-1.059) | 0.302 | |||
| ECOG PS ≥1 | 1.042 | (0.572-1.898) | 0.893 | |||
| Gleason score | ||||||
| ≤8 | 1.356 | (0.697-2.638) | 0.370 | |||
| ≥9 | 0.738 | (0.379-1.436) | 0.370 | |||
| Clinical T stage | ||||||
| ≥T3 | 0.907 | (0.484-1.699) | 0.760 | |||
| T4 | 1.103 | (0.589-2.065) | 0.760 | |||
| Clinical N stage | ||||||
| N1 | 0.736 | (0.392-1.382) | 0.340 | |||
| PSA at diagnosis | 1.000 | (1.000-1.000) | 0.647 | |||
| PSA at CRPC diagnosis | 1.000 | (1.000-1.001) | 0.307 | |||
| Hb | 0.904 | (0.738-1.107) | 0.328 | |||
| NLR | 1.027 | (0.944-1.117) | 0.534 | |||
| Albumin | 1.732 | (0.797-3.765) | 0.165 | |||
| Prior radical prostatectomy | 0.728 | (0.355-1.494) | 0.387 | |||
| Prior palliative EBRT | 1.292 | (0.675-2.472) | 0.439 | |||
| DTX+ADT | 0.583 | (0.316-1.075) | 0.084 | |||
| Number of DTX cycles | 0.876 | (0.796-0.964) | 0.007 | 0.876 | (0.796-0.964) | 0.007 |
| Extent of disease | ||||||
| Bone metastasis | 0.855 | (0.303-2.414) | 0.767 | |||
| Lymph node metastasis | 1.087 | (0.563-2.096) | 0.804 | |||
| Lung or liver metastasis | 0.788 | (0.188-3.304) | 0.745 | |||
HR, hazard ratio; CI, confidence interval; DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; EBRT, external-beam radiation therapy; PSA, prostate-specific antigen; CRPC, castration-resistant prostate cancer; Hb, hemoglobin; NLR, neutrophil-to-lymphocyte ratio.
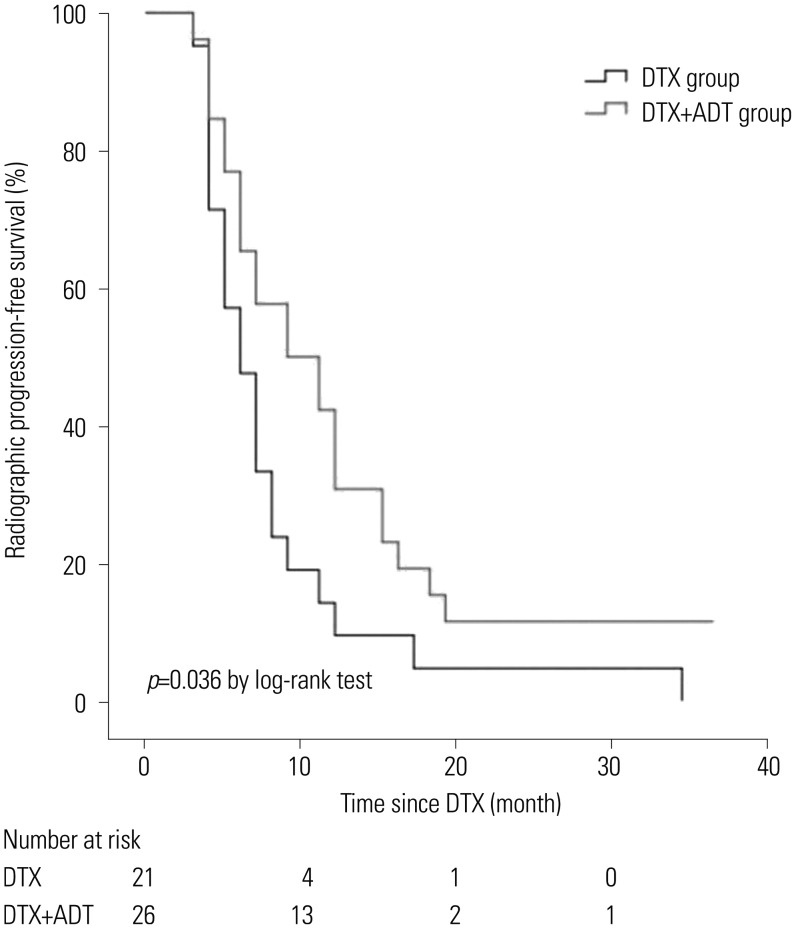
The median rPFS was 9.0 months (95% CI 4.003–13.997) in the DTX+ADT group and 6.0 months (95% CI 4.206–7.794) in the DTX group. Kaplan-Meier analysis revealed a significant association between concurrent administration of ADT and prolonged rPFS (log-rank p=0.036) (Fig. 2). On univariable Cox regression analysis, the number of DTX cycles and concurrent administration of ADT were significantly associated with rPFS, and concurrent administration of ADT was the only significant predictor in multivariable analysis (Table 5).
Fig. 2. Kaplan-Meier curve of radiographic progression-free survival. DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy.
Table 5. Associated Baseline Factors of Radiographic Progression-Free Survival via Univariable and Multivariable Analyses.
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | p value | HR | (95% CI) | p value | |
| Age | 1.024 | (0.979-1.070) | 0.301 | |||
| BMI | 0.995 | (0.879-1.127) | 0.938 | |||
| ECOG PS ≥1 | 0.720 | (0.394-1.317) | 0.287 | |||
| Gleason score | ||||||
| ≤8 | 1.363 | (0.725-2.559) | 0.336 | |||
| ≥9 | 0.734 | (0.391-1.379) | 0.336 | |||
| Clinical T stage | ||||||
| ≤T3 | 1.620 | (0.861-3.048) | 0.134 | |||
| T4 | 0.617 | (0.328-1.161) | 0.134 | |||
| Clinical N stage | ||||||
| N1 | 0.788 | (0.435-1.429) | 0.433 | |||
| PSA at diagnosis | 1.000 | (1.000-1.000) | 0.695 | |||
| PSA at CRPC diagnosis | 1.001 | (1.000-1.001) | 0.120 | |||
| Hb | 0.913 | (0.737-1.131) | 0.406 | |||
| NLR | 0.955 | (0.879-1.039) | 0.283 | |||
| Albumin | 0.853 | (0.403-1.808) | 0.679 | |||
| Prior radical prostatectomy | 1.189 | (0.596-2.372) | 0.623 | |||
| Prior palliative EBRT | 1.306 | (0.696-2.452) | 0.406 | |||
| DTX+ADT | 0.550 | (0.300-1.007) | 0.053 | 0.525 | (0.284-0.970) | 0.040 |
| Number of DTX cycles | 0.948 | (0.884-1.017) | 0.134 | 0.940 | (0.872-1.013) | 0.104 |
| Extent of disease | ||||||
| Bone metastasis | 1.136 | (0.349-3.700) | 0.832 | |||
| Lymph node metastasis | 1.349 | (0.708-2.572) | 0.363 | |||
| Lung or liver metastasis | 1.385 | (0.331-5.796) | 0.656 | |||
HR, hazard ratio; CI, confidence interval; DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; EBRT, external-beam radiation therapy; PSA, prostate-specific antigen; CRPC, castration-resistant prostate cancer; Hb, hemoglobin; NLR, neutrophil-to-lymphocyte ratio.
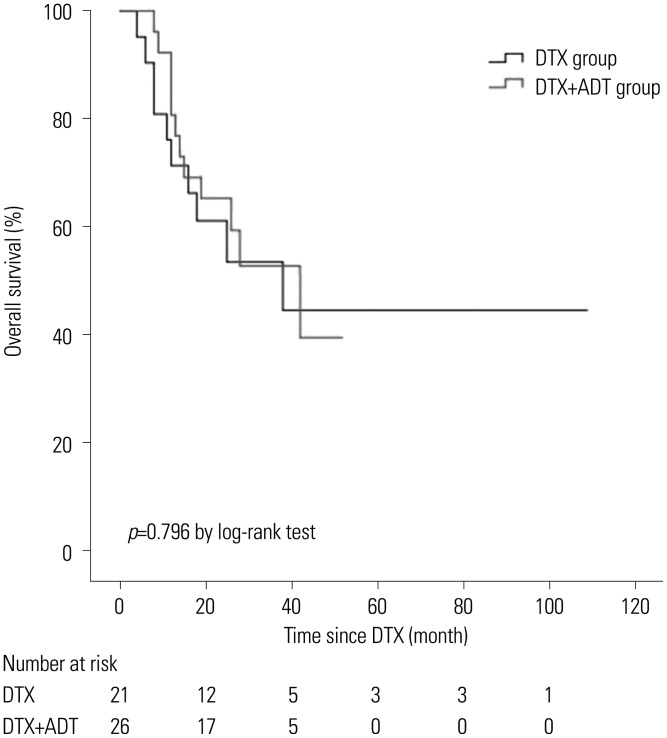
The median OS was 42.0 months (95% CI 19.677–64.323) and 38.0 months (95% CI 7.752–68.243) in the DTX+ADT and DTX groups, respectively (log-rank p=0.796) (Fig. 3). On multivariable analysis, Hb level at the time of DTX initiation was associated with OS (Table 6).
Fig. 3. Kaplan-Meier curve of overall survival. DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy.
Table 6. Associated Baseline Factors of Overall Survival via Univariable and Multivariable Analyses.
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | p value | HR | (95% CI) | p value | |
| Age | 1.036 | (0.969-1.109) | 0.301 | |||
| BMI | 0.950 | (0.806-1.120) | 0.543 | |||
| ECOG PS ≥1 | 1.121 | (0.485-2.592) | 0.789 | |||
| Gleason score | ||||||
| ≤8 | 0.772 | (0.301-1.980) | 0.590 | |||
| ≥9 | 1.295 | (0.505-3.322) | 0.590 | |||
| Clinical T stage | ||||||
| ≤T3 | 0.910 | (0.391-2.118) | 0.826 | |||
| T4 | 1.099 | (0.472-2.558) | 0.826 | |||
| Clinical N stage | ||||||
| N1 | 1.302 | (0.545-3.113) | 0.552 | |||
| PSA at diagnosis | 0.999 | (0.997-1.000) | 0.130 | 0.999 | (0.997-1.000) | 0.138 |
| PSA at CRPC diagnosis | 1.001 | (1.000-1.003) | 0.012 | |||
| Hb | 0.610 | (0.453-0.822) | 0.001 | 0.532 | (0.381-0.744) | <0.001 |
| NLR | 1.039 | (0.938-1.151) | 0.465 | |||
| Albumin | 0.391 | (0.144-1.056) | 0.064 | |||
| Prior radical prostatectomy | 0.656 | (0.222-1.945) | 0.447 | |||
| Prior palliative EBRT | 1.842 | (0.779-4.355) | 0.164 | |||
| DTX+ADT | 1.116 | (0.481-2.591) | 0.798 | |||
| Number of DTX cycles | 1.012 | (0.938-1.092) | 0.759 | |||
| Extent of disease | ||||||
| Bone metastasis | 0.487 | (0.143-1.656) | 0.249 | |||
| Lymph node metastasis | 1.946 | (0.716-5.281) | 0.192 | |||
| Lung or liver metastasis | 1.175 | (0.156-8.878) | 0.876 | |||
HR, hazard ratio; CI, confidence interval; DTX, docetaxel-based chemotherapy; ADT, androgen deprivation therapy; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; EBRT, external-beam radiation therapy; PSA, prostate-specific antigen; CRPC, castration-resistant prostate cancer; Hb, hemoglobin; NLR, neutrophil-to-lymphocyte ratio.
DISCUSSION
DTX has been a standard chemotherapy treatment for CRPC since 2004, and both the SWOG 99-16 study and the Taxanes (TAX) 327 study demonstrated the superiority of DTX over mitoxantrone.27,28 The patients enrolled in both the SWOG 99-16 and TAX 327 trials continued on ADT due to the possible detrimental effects of its discontinuation. AR activation and enzymatic androgen synthesis are potential mechanisms of CRPC, and these mechanisms can increase the sensitivity of neoplastic cells to very low concentrations of testosterone.6,7,8,9,10,11,12,13,14 A study related to abiraterone acetate revealed that reducing serum testosterone to undetectable levels was correlated with extended survival for patients with mCRPC.29 Organizations such as the American Society of Clinical Oncology, the National Comprehensive Cancer Network, and others also recommend that ADT should be continued in nonorchiectomized CRPC patients during clinical trials for the same reason.
There have been several studies on the effectiveness of continued ADT in CRPC patients under cytotoxic chemotherapy; however, the results have been inconsistent. Taylor, et al.19 examined data from 341 patients enrolled in ECOG trials and found that patients who maintained castrate levels of testosterone had a longer median survival of 2 months. On the other hand, Hussain, et al.20 analyzed data from 205 patients with CRPC enrolled in SWOG phase II chemotherapy trials, and there was no difference in median survival between patients who maintained castrate levels of testosterone and those who did not. Recently, a retrospective study was published on patients with CRPC who were treated with DTX, and clinical outcomes were not significantly different between patients who received concurrent ADT and those who did not.30
In our study, the rPFS and bPFS rates were significantly better in the DTX+ADT group than in the DTX group; however, they did not show efficacy for OS, which has been considered the most important endpoint for the evaluation of new treatments in oncology.31 Death is clinically important, objective, and easily defined. However, OS is associated with several drawbacks, which can in turn lead to inappropriate conclusions. First, it requires a long-term follow-up period and a large number of patients to detect realistic OS, as it may not be appropriate for evaluating the superiority of a treatment in smallscale retrospective studies. Second, potential differences in OS between the experimental and control groups could be masked by the use of second-line therapy after tumor progression on first-line therapy. In our study, excluding expired patients, various types of second line chemotherapies were administrated to the disease-progressed patients. Third, OS can be influenced by survival post-progression. According to a study of Broglio and Berry,32 a lack of statistical significance in OS does not imply a lack of improvement in OS for clinical trials with a PFS benefit, particularly for diseases with long median survival post-progression. If there is long-term survival after disease progression, there is also the potential for multiple additional treatments, which can dilute the treatment effect. Broglio and Berry32 suggested that longer periods of survival post-progression (i.e., 12 months), would cause statistical significance in OS to be decreasingly likely. The median survival post-progressions periods were 13.0 and 18.0 months (radiographic and biochemical, respectively) in our study, thus, these long periods may have potentially affected OS. Therefore, it was not appropriate to evaluate the efficacy of continuing ADT based solely on OS in our study.
As described above, use of OS as the primary endpoint is often limited, and it may be helpful to use an appropriate surrogate endpoint in such cases. PFS is an attractive endpoint as a surrogate of survival, given that it can be used in studies with small sample sizes, as the definition of PFS includes a greater number of events than that of OS. Moreover, progression of a disease occurs before survival can be measured; thus, PFS is not confounded by the effects of interim treatments. Due to these advantages, the European Agency for the Evaluation of Medical Products accepts a prolongation in the time to progression as a primary requirement for new drug registration in the European Union.33 Particularly in recent years, radiographic progression defined using the PCWG-2 criteria has emerged as a feasible surrogate endpoint of OS. Sonpavde, et al.34 showed that rPFS was significantly associated with OS in patients with mCRPC who received first-line DTX or post-docetaxel therapy. Kendall's τ was 0.50 (p<0.001) in a setting of docetaxel-based therapy and 0.34 (p<0.001) in the post-docetaxel setting for association between rPFS and OS. Unlike radiographic progression, PSA response has not been demonstrated to produce robust results as a surrogate endpoint of OS in studies on the survival outcomes of mCRPC after chemotherapy. PSA cannot differentiate variability in tumor response across different disease sites.35 Moreover, PSA surge and flare up phenomena, which lead to transient PSA elevation following chemotherapy, are not uncommon in patients with CRPC who respond to chemotherapy. 36,37,38 It is reported that these phenomena occur between 1 and 8 weeks following a drop in the level of serum PSA.39 For this reason, we only included patients who continued for at least three cycles of DTX in this study.
The PCWG-2 recommends that early rising PSA levels should not be used as the sole criterion for discontinuing treatment on the basis of the description above.24 At the Advanced Prostate Cancer Consensus Conference, held in 2015, there was consensus (82% of the panel) that at least two of three criteria (PSA progression, radiographic progression and clinical deterioration) should be fulfilled to stop treatment of patients with advanced PCa.40 In this study, there was no patient who stopped DTX for PSA progression alone, and there was no significant difference in the respective reasons for discontinuing DTX between the two groups (Table 2). Additionally, there was no patient in the DTX+ADT group who stopped DTX due to the adverse effects of continuing ADT, such as coronary heart disease, myocardial infarction, bone fracture, or diabetes.
The present study was primarily designed to assess the impact of concurrent administration of ADT and DTX in patients with mCRPC using rPFS as a primary endpoint. None of the patients in this study had received cytotoxic chemotherapy before DTX; thus, our study was able to provide more accurate results. However, there were several limitations to this study: 1) our data were retrospectively collected at a single center, causing the results to be sensitive to selection bias; 2) serum testosterone measurements were not performed for all patients, and the limited number of samples precluded a meaningful analysis; and 3) this study involved a small sample size due to the relative rarity of chemotherapy-naive patients without a dose reduction of docetaxel. The limited sample size may have precluded a strong conclusion.
In this study involving men with mCRPC, the combined use of ADT and DTX improved rPFS and bPFS. Mentioned previously, there were several limitations related to using OS to evaluate the efficacy of treatment in our study, and rPFS could be a clinically meaningful surrogate of survival for several reasons. Therefore, the results of our study suggest that the combined use of ADT and DTX is superior to DTX alone.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11 [Internet] Lyon (France): International Agency for Research on Cancer; c2013. [updated 2014]. [cited 2015 Aug 4]. Available at: http://globocan.iarc.fr. [Google Scholar]
- 2.Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D'Amico AV, et al. Prostate cancer, version 2.2014. J Natl Compr Canc Netw. 2014;12:686–718. doi: 10.6004/jnccn.2014.0072. [DOI] [PubMed] [Google Scholar]
- 3.Lam JS, Leppert JT, Vemulapalli SN, Shvarts O, Belldegrun AS. Secondary hormonal therapy for advanced prostate cancer. J Urol. 2006;175:27–34. doi: 10.1016/S0022-5347(05)00034-0. [DOI] [PubMed] [Google Scholar]
- 4.Smith MR, Kabbinavar F, Saad F, Hussain A, Gittelman MC, Bilhartz DL, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23:2918–2925. doi: 10.1200/JCO.2005.01.529. [DOI] [PubMed] [Google Scholar]
- 5.Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–1197. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 6.Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6:76–85. doi: 10.1038/ncpuro1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donkena KV, Yuan H, Young CY. Recent advances in understanding hormonal therapy resistant prostate cancer. Curr Cancer Drug Targets. 2010;10:402–410. doi: 10.2174/156800910791208544. [DOI] [PubMed] [Google Scholar]
- 8.Hotte SJ, Saad F. Current management of castrate-resistant prostate cancer. Curr Oncol. 2010;17(Suppl 2):S72–S79. doi: 10.3747/co.v17i0.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Attar RM, Takimoto CH, Gottardis MM. Castration-resistant prostate cancer: locking up the molecular escape routes. Clin Cancer Res. 2009;15:3251–3255. doi: 10.1158/1078-0432.CCR-08-1171. [DOI] [PubMed] [Google Scholar]
- 10.Sharifi N, Dahut WL, Figg WD. The genetics of castration-resistant prostate cancer: what can the germline tell us? Clin Cancer Res. 2008;14:4691–4693. doi: 10.1158/1078-0432.CCR-08-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelmann EP. Molecular biology of the androgen receptor. J Clin Oncol. 2002;20:3001–3015. doi: 10.1200/JCO.2002.10.018. [DOI] [PubMed] [Google Scholar]
- 12.Chen CD, Welsbie DS, Tran C, Baek SH, Chen R, Vessella R, et al. Molecular determinants of resistance to antiandrogen therapy. Nat Med. 2004;10:33–39. doi: 10.1038/nm972. [DOI] [PubMed] [Google Scholar]
- 13.Gregory CW, Johnson RT, Jr, Mohler JL, French FS, Wilson EM. Androgen receptor stabilization in recurrent prostate cancer is associated with hypersensitivity to low androgen. Cancer Res. 2001;61:2892–2898. [PubMed] [Google Scholar]
- 14.Buchanan G, Yang M, Harris JM, Nahm HS, Han G, Moore N, et al. Mutations at the boundary of the hinge and ligand binding domain of the androgen receptor confer increased transactivation function. Mol Endocrinol. 2001;15:46–56. doi: 10.1210/mend.15.1.0581. [DOI] [PubMed] [Google Scholar]
- 15.Alibhai SM, Duong-Hua M, Sutradhar R, Fleshner NE, Warde P, Cheung AM, et al. Impact of androgen deprivation therapy on cardiovascular disease and diabetes. J Clin Oncol. 2009;27:3452–3458. doi: 10.1200/JCO.2008.20.0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsai HK, D'Amico AV, Sadetsky N, Chen MH, Carroll PR. Androgen deprivation therapy for localized prostate cancer and the risk of cardiovascular mortality. J Natl Cancer Inst. 2007;99:1516–1524. doi: 10.1093/jnci/djm168. [DOI] [PubMed] [Google Scholar]
- 17.Shahinian VB, Kuo YF, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352:154–164. doi: 10.1056/NEJMoa041943. [DOI] [PubMed] [Google Scholar]
- 18.Strum SB, McDermed JE, Scholz MC, Johnson H, Tisman G. Anaemia associated with androgen deprivation in patients with prostate cancer receiving combined hormone blockade. Br J Urol. 1997;79:933–941. doi: 10.1046/j.1464-410x.1997.00234.x. [DOI] [PubMed] [Google Scholar]
- 19.Taylor CD, Elson P, Trump DL. Importance of continued testicular suppression in hormone-refractory prostate cancer. J Clin Oncol. 1993;11:2167–2172. doi: 10.1200/JCO.1993.11.11.2167. [DOI] [PubMed] [Google Scholar]
- 20.Hussain M, Wolf M, Marshall E, Crawford ED, Eisenberger M. Effects of continued androgen-deprivation therapy and other prognostic factors on response and survival in phase II chemotherapy trials for hormone-refractory prostate cancer: a Southwest Oncology Group report. J Clin Oncol. 1994;12:1868–1875. doi: 10.1200/JCO.1994.12.9.1868. [DOI] [PubMed] [Google Scholar]
- 21.Mottet N, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2011;59:572–583. doi: 10.1016/j.eururo.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 22.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, et al. AJCC cancer staging manual. 7th ed. New York: Springer; 2010. [Google Scholar]
- 23.US Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 [Internet] Bethesda (MD): National Institutes of Health, National Cancer Institute (US); c2009. [updated 2010 Jun 14]. [cited 2015 Aug 4]. Available at: http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf. [Google Scholar]
- 24.Bubley GJ, Carducci M, Dahut W, Dawson N, Daliani D, Eisenberger M, et al. Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol. 1999;17:3461–3467. doi: 10.1200/JCO.1999.17.11.3461. [DOI] [PubMed] [Google Scholar]
- 25.Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–1159. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 27.Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–1512. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 28.Petrylak DP, Tangen CM, Hussain MH, Lara PN, Jr, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–1520. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]
- 29.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee JL, Eun Kim J, Ahn JH, Lee DH, Lee J, Kim CS, et al. Role of androgen deprivation treatment in patients with castration-resistant prostate cancer, receiving docetaxel-based chemotherapy. Am J Clin Oncol. 2011;34:140–144. doi: 10.1097/COC.0b013e3181d2ed7d. [DOI] [PubMed] [Google Scholar]
- 31.Sargent D. General and statistical hierarchy of appropriate biologic endpoints. Oncology (Williston Park) 2006;20(6 Suppl 5):5–9. [PubMed] [Google Scholar]
- 32.Broglio KR, Berry DA. Detecting an overall survival benefit that is derived from progression-free survival. J Natl Cancer Inst. 2009;101:1642–1649. doi: 10.1093/jnci/djp369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.EMA. Guideline on the evaluation of anticancer medicinal products in man (CHMP/205/95/Rev.4) [Internet] London (UK): European Medicines Agency; 2012. [cited 2015 Aug 4]. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2013/01/WC500137128.pdf. [Google Scholar]
- 34.Sonpavde G, Pond GR, Armstrong AJ, Galsky MD, Leopold L, Wood BA, et al. Radiographic progression by Prostate Cancer Working Group (PCWG)-2 criteria as an intermediate endpoint for drug development in metastatic castration-resistant prostate cancer. BJU Int. 2014;114:E25–E31. doi: 10.1111/bju.12589. [DOI] [PubMed] [Google Scholar]
- 35.Koo KC, Park SU, Kim KH, Rha KH, Hong SJ, Yang SC, et al. Prognostic impacts of metastatic site and pain on progression to castrate resistance and mortality in patients with metastatic prostate cancer. Yonsei Med J. 2015;56:1206–1212. doi: 10.3349/ymj.2015.56.5.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nelius T, Klatte T, de Riese W, Filleur S. Impact of PSA flare-up in patients with hormone-refractory prostate cancer undergoing chemotherapy. Int Urol Nephrol. 2008;40:97–104. doi: 10.1007/s11255-007-9221-y. [DOI] [PubMed] [Google Scholar]
- 37.Han KS, Hong SJ. Exponential rise in prostate-specific antigen (PSA) during anti-androgen withdrawal predicts PSA flare after docetaxel chemotherapy in patients with castration-resistant prostate cancer. Yonsei Med J. 2015;56:368–374. doi: 10.3349/ymj.2015.56.2.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koo KC, Lee DH, Kim KH, Lee SH, Hong CH, Hong SJ, et al. Unrecognized kinetics of serum testosterone: impact on short-term androgen deprivation therapy for prostate cancer. Yonsei Med J. 2014;55:570–575. doi: 10.3349/ymj.2014.55.3.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thuret R, Massard C, Gross-Goupil M, Escudier B, Di Palma M, Bossi A, et al. The postchemotherapy PSA surge syndrome. Ann Oncol. 2008;19:1308–1311. doi: 10.1093/annonc/mdn062. [DOI] [PubMed] [Google Scholar]
- 40.Gillessen S, Omlin A, Attard G, de Bono JS, Efstathiou E, Fizazi K, et al. Management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015. Ann Oncol. 2015;26:1589–1604. doi: 10.1093/annonc/mdv257. [DOI] [PMC free article] [PubMed] [Google Scholar]