Abstract
Purpose:
Mastectomy with immediate reconstruction (MIR) requires coordination between breast and reconstructive surgical teams, leading to increased preoperative delays that may adversely impact patient outcomes and satisfaction. Our cancer center established a target of 28 days from initial consultation with the breast surgeon to MIR. We sought to determine if a centralized breast/reconstructive surgical coordinator (BRC) could reduce care delays.
Methods:
A 60-day pilot to evaluate the impact of a BRC on timeliness of care was initiated at our cancer center. All reconstructive surgery candidates were referred to the BRC, who had access to surgical clinic and operating room schedules. The BRC worked with both surgical services to identify the earliest surgery dates and facilitated operative bookings. The median time to MIR and the proportion of MIR cases that met the time-to-treatment goal was determined. These results were compared with a baseline cohort of patients undergoing MIR during the same time period (January to March) in 2013 and 2014.
Results:
A total of 99 patients were referred to the BRC (62% cancer, 21% neoadjuvant, 17% prophylactic) during the pilot period. Focusing exclusively on patients with a cancer diagnosis, an 18.5% increase in the percentage of cases meeting the target (P = .04) and a 7-day reduction to MIR (P = .02) were observed.
Conclusion:
A significant reduction in time to MIR was achieved through the implementation of the BRC. Further research is warranted to validate these findings and assess the impact the BRC has on operational efficiency and workflows.
INTRODUCTION
Timely diagnosis and treatment of breast cancer, endorsed by organizations such as ASCO and the National Comprehensive Cancer Network, are important care standards aimed to optimize clinical outcomes, patient satisfaction, and care quality. For a majority of women diagnosed with early-stage breast cancer, breast surgery is the first step in the treatment pathway. Rates of mastectomy with immediate reconstruction (MIR) have nearly tripled in the United States, and at our comprehensive cancer center approximately 60% of women with breast cancer who undergo mastectomy elect immediate reconstruction.1-3
Several factors associated with care delays have been identified in the literature, including the receipt of additional imaging and the coordination of multimodality care teams, with studies demonstrating an increase in preoperative wait times for breast surgery nationally in the past decade.3-13 A centralized patient or nurse navigator role has been introduced in several cancer centers in an effort to mitigate care delays, although most of the existing literature focuses on the impact that navigators have on reducing the time from initial presentation of symptoms to cancer diagnosis.14-18
In an effort to address timeliness and care coordination for patients with breast cancer at our cancer center, breast leadership established a quality improvement initiative and set time-to-treatment targets from initial consultation to first definitive surgery. Using the DMAIC model (define, measure, analyze, improve, and control), a multidisciplinary process improvement team was formed to elucidate the root causes of delays and to identify solutions to reduce time to MIR. The aim of this study was to examine the impact of a centralized breast/reconstructive coordinator (BRC) on coordination and timeliness to MIR.
METHODS
Setting
We examined the care of adult women treated for breast cancer at the Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC), a National Cancer Institute–designated comprehensive cancer center with a national and international referral population. With more than 3,000 unique new patients with breast cancer annually, the DF/BWCC Breast Cancer program includes 26 medical oncologists, 12 surgical oncologists, 13 breast reconstruction surgeons, and six radiation oncologists, who practice across five ambulatory sites. For patients who undergo surgery up front, 65% undergo lumpectomy, 25% undergo MIR, and 15% undergo mastectomy alone. The new patient volume also includes patients with metastatic disease and one-time second opinions.
Quality Improvement Methodology (DMAIC)
Define
Breast center leadership at DF/BWCC identified the opportunity to reduce delays for women with breast cancer undergoing MIR. Through a series of interviews and meetings with breast and reconstructive surgeons, administrative support staff, and administrators, barriers in the coordination and scheduling of MIR cases were identified, including allocation of operating room block time, alignment of breast and plastic surgery clinic and operating room schedules, receipt of genetic testing, breast surgeon referral patterns, visibility of clinic and operating room schedules across practices, and administrative processes. Through a consensus process, time-to-treatment targets were established, including a target of 7 days from initial appointment with a breast surgeon to a consultation with a reconstructive surgeon and a target of 28 days from initial consultation to MIR. These goals were developed after reviewing new patient volume, number of surgical procedures performed, number of surgeons, and operating room block availability.
Measure
An internal data set was created to generate descriptive statistics on the time from initial consultation with a breast surgeon to MIR at both the hospital- and provider-specific levels at two primary surgical sites from January 2013 to March 2015. Patients undergoing neoadjuvant therapy were excluded from the data set.
Current standard of care workflows were generated to document the process of obtaining reconstructive surgery consultations and scheduling MIR across breast surgeon practices to identify variations in process and best practices.
Analyze
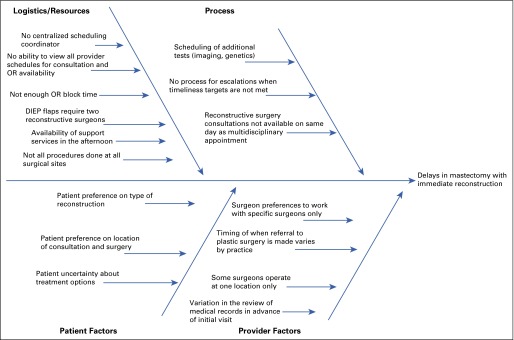
Before selecting the BRC role as the primary intervention, facilitated sessions with key stakeholders were held to identify potential root causes of delays for MIR, including patient factors, administrative processes, resources, and provider-specific factors (Fig 1).
FIG 1.
Factors associated with delays to mastectomy with immediate reconstruction. DIEP, deep inferior epigastric perforators; OR, operating room.
Improve
Solutions aimed at alleviating delays to MIR were identified by the multidisciplinary team and prioritized using a priority pay-off matrix. Focusing on breast surgeon referral patterns and administrative processes, an opportunity to streamline the scheduling process for MIR was identified through the development of a single centralized coordinator position (the BRC) to facilitate multidisciplinary scheduling. To assess the feasibility and impact of a BRC, a pilot was initiated with the following objectives: defining the responsibility of the role; defining the workflows between surgeons, administrative support staff, and BRC; creating an efficient workflow for booking plastic surgery consultations and MIR surgeries; and ensuring that 60% of patients with breast cancer undergo MIR within the target time frame.
As part of the workflow, requests for reconstructive surgery consultations, from the new patient office at DF/BWCC, the breast surgeon, or the program nurse, were routed through the BRC. The BRC had access to all breast and plastic surgeon calendars, and on a weekly basis the plastic surgery department provided a list of available operating room times for the upcoming 35 days to the BRC, including both block time and segments of other time that could be used. The BRC identified the earliest date of surgery and coordinated with administrative staff from both services to secure the operating room date and schedule the reconstruction consultation. All breast and reconstructive surgeons participated in the pilot.
Control
The BRC role was sustained during the 60-day pilot. Data on the date of referral to the BRC, the date of the reconstructive surgery consultation, the proposed date of surgery, and the staff member referring the patient to the BRC were recorded. Through retrospective chart reviews, surgery case completions were confirmed, and those cases that were canceled were excluded from the analysis. Weekly calls among the multidisciplinary project team were held to identify any process issues.
RESULTS
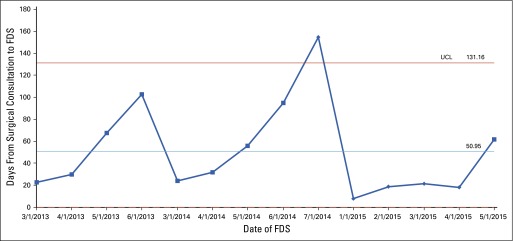
A total of 99 women were referred to the BRC (62% cancer, 21% neoadjuvant, 17% prophylactic [BRCA1/2 mutation carriers]) during the pilot period. Focusing exclusively on patients with a breast cancer diagnosis at initial consultation, the median number of days to MIR was 40.0 (interquartile range, 17.0) for the baseline period and 33.0 (interquartile range, 20.0) after implementation of the BRC (P = .02). An 18.5% increase in the percentage of cases that met the timeliness target (42.2% v 23.7%; P = .04) was observed postintervention. A statistical process control chart (Fig 2) showing the median time from initial consultation to MIR between January and March 2013, 2014, and 2015 demonstrates that the introduction of the BRC reduced variability in wait times.
FIG 2.
Median time from surgical consultation to first definitive surgery (FDS) for mastectomy with immediate reconstruction. UCL, upper control limit.
DISCUSSION
Our quality improvement project uncovered multiple barriers to ensuring the timely completion of MIR on the basis of the targets set by breast center leadership, including patient factors such as decision-making delays, hospital resources, staffing, and physician and administrative processes. Focusing on solutions within provider and/or administrative staff control, our present study offers a potential approach to reduce preoperative delays by expediting the administrative processes through the implementation of a centralized coordinator role.
With the implementation of a BRC, patients with breast cancer who underwent MIR experienced a 7-day decrease in wait times to surgery compared with the baseline cohort, which included MIR cases from the same time period over the previous 2 years. Although there is no evidence that a 7-day time savings would result in improved survival outcomes,13,19,20 we believe that this savings represents an improvement in patient care. This time savings may be most critical to patients who receive adjuvant chemotherapy, with recent studies demonstrating that patients who undergo MIR are more likely to experience delays in chemotherapy initiation, and delays in adjuvant chemotherapy may result in worse breast cancer–specific survival.21,22 Also, patient stress and anxiety can be alleviated by reducing preoperative delays. Streamlining the scheduling of appointments and surgeries likely reduces administrative burden and improves access to care for new patients.23 At consecutive debriefing meetings with clinical and administrative staff from both surgical services there was universal agreement that a significant reduction in the number of e-mails and phone calls required to schedule an MIR procedure was observed with BRC implementation.
Our project is subject to several limitations. The BRC was a pilot, and data would have to be collected over a longer period of time to determine whether these preliminary results could be sustained and to demonstrate the cost effectiveness of this intervention. During the pilot, a senior administrative specialist with longstanding knowledge of breast and reconstructive services assumed the responsibilities of the BRC, which may have had an enhanced positive impact on the success of the role. We were also unable to determine the effect of the BRC on patient experience, as we did not conduct any postvisit or postsurgery patient satisfaction surveys. Further research is warranted to validate these initial findings and determine additional impacts the BRC may have on operational efficiency and provider and patient satisfaction.
Despite these limitations, our study demonstrates that improvements in timeliness of MIR can be achieved through the implementation of standardized workflows using a centralized coordinator with access to all relevant clinical and surgical schedules. We are currently considering the permanent implementation of a BRC role at our center.
Acknowledgment
Supported in part by Grant No. R25 CA089017 from the National Institutes of Health. M.G. and K.L. are co-first authors; they have contributed equally to this manuscript.
AUTHOR CONTRIBUTIONS
Conception and design: Mehra Golshan, Katya Losk, Kristen Camuso, Linda Cutone, Stephanie Caterson, Craig A. Bunnell
Administrative support: Mehra Golshan
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Implementation of a Breast/Reconstruction Surgery Coordinator to Reduce Preoperative Delays for Patient Undergoing Mastectomy With Immediate Reconstruction
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Mehra Golshan
No relationship to disclose
Katya Losk
No relationship to disclose
Melissa A. Mallory
No relationship to disclose
Kristen Camuso
No relationship to disclose
Linda Cutone
No relationship to disclose
Stephanie Caterson
No relationship to disclose
Craig A. Bunnell
No relationship to disclose
References
- 1.Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: Part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e–326e. doi: 10.1097/PRS.0b013e31827cf576. [DOI] [PubMed] [Google Scholar]
- 2.Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150:9–16. doi: 10.1001/jamasurg.2014.2895. [DOI] [PubMed] [Google Scholar]
- 3.Golshan M, Losk K, Kadish S, et al. Understanding process-of-care delays in surgical treatment of breast cancer at a comprehensive cancer center. Breast Cancer Res Treat. 2014;148:125–133. doi: 10.1007/s10549-014-3124-2. [DOI] [PubMed] [Google Scholar]
- 4.Golshan M, Losk K, Mallory MA. 2015. Variation in additional breast imaging orders and impact on surgical wait times at a comprehensive cancer center. Ann Surg Oncol 22:428-434 doi: 10.1245/s10434-015-4834-3(suppl 3)
- 5.Nessim C, Winocour J, Holloway DP, et al. Wait times for breast cancer surgery: Effect of magnetic resonance imaging and preoperative investigations on the diagnostic pathway. J Oncol Pract. 2015;11:e131–e138. doi: 10.1200/JOP.2014.002105. [DOI] [PubMed] [Google Scholar]
- 6.Liederbach E, Sisco M, Wang C, et al. Wait times for breast surgical operations, 2003-2011: A report from the National Cancer Data Base. Ann Surg Oncol. 2015;22:899–907. doi: 10.1245/s10434-014-4086-7. [DOI] [PubMed] [Google Scholar]
- 7.Cordeiro E, Dixon M, Coburn N, et al. A patient centered approach to wait times in the surgical management of breast cancer in the province of Ontario. Ann Surg Oncol. 2015;22:2509–2516. doi: 10.1245/s10434-014-4320-3. [DOI] [PubMed] [Google Scholar]
- 8.Bleicher RJ, Ruth K, Sigurdson ER, et al. Preoperative delays in the US Medicare population with breast cancer. J Clin Oncol. 2012;30:4485–4492. doi: 10.1200/JCO.2012.41.7972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bilimoria KY, Ko CY, Tomlinson JS, et al. Wait times for cancer surgery in the United States: Trends and predictors of delays. Ann Surg. 2011;253:779–785. doi: 10.1097/SLA.0b013e318211cc0f. [DOI] [PubMed] [Google Scholar]
- 10.Hulvat M, Sandalow N, Rademaker A, et al. Time from diagnosis to definitive operative treatment of operable breast cancer in the era of multimodal imaging. Surgery. 2010;148:746–750. doi: 10.1016/j.surg.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Wright GP, Wong JH, Morgan JW, et al. Time from diagnosis to surgical treatment of breast cancer: factors influencing delays in initiating treatment. Am Surg. 2010;76:1119–1122. [PubMed] [Google Scholar]
- 12.Angarita FA, Acuna SA, Fonseca A, et al. Impact of preoperative breast MRIs on timing of surgery and type of intervention in newly diagnosed breast cancer patients. Ann Surg Oncol. 2010;17(suppl 3):273–279. doi: 10.1245/s10434-010-1239-1. [DOI] [PubMed] [Google Scholar]
- 13.Richards MA, Smith P, Ramirez AJ, et al. The influence on survival of delay in the presentation and treatment of symptomatic breast cancer. Br J Cancer. 1999;79:858–864. doi: 10.1038/sj.bjc.6690137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braun KL, Thomas WL, Jr, Domingo JL, et al. Reducing cancer screening disparities in medicare beneficiaries through cancer patient navigation. J Am Geriatr Soc. 2015;63:365–370. doi: 10.1111/jgs.13192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freund KM, Battaglia TA, Calhoun E, et al. 2014. Impact of patient navigation on timely cancer care: The Patient Navigation Research Program. J Natl Cancer Inst 106:dju 115.
- 16.Wagner EH, Ludman EJ, Aiello Bowles EJ, et al. Nurse navigators in early cancer care: A randomized, controlled trial. J Clin Oncol. 2014;32:12–18. doi: 10.1200/JCO.2013.51.7359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanley S, Arriola KJ, Smith S, et al. Reducing barriers to breast cancer care through Avon patient navigation programs. J Public Health Manag Pract. 2013;19:461–467. doi: 10.1097/PHH.0b013e318276e272. [DOI] [PubMed] [Google Scholar]
- 18.Vargas RB, Ryan GW, Jackson CA, et al. Characteristics of the original patient navigation programs to reduce disparities in the diagnosis and treatment of breast cancer. Cancer. 2008;113:426–433. doi: 10.1002/cncr.23547. [DOI] [PubMed] [Google Scholar]
- 19.Sue GR, Lannin DR, Killelea B, et al. Does time to definitive treatment matter in patients with ductal carcinoma in situ? Am Surg. 2013;79:561–565. [PubMed] [Google Scholar]
- 20.Landercasper J, Linebarger JH, Ellis RL, et al. A quality review of the timeliness of breast cancer diagnosis and treatment in an integrated breast center. J Am Coll Surg. 2010;210:449–455. doi: 10.1016/j.jamcollsurg.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Alderman AK, Collins ED, Schott A, et al. The impact of breast reconstruction on the delivery of chemotherapy. Cancer. 2010;116:1791–1800. doi: 10.1002/cncr.24891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gagliato DDM, Gonzalez-Angulo AM., Lei X, et al. Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol. 2014;32:735–744. doi: 10.1200/JCO.2013.49.7693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hislop TG, Harris SR, Jackson J, et al. Satisfaction and anxiety for women during investigation of an abnormal screening mammogram. Breast Cancer Res Treat. 2002;76:245–254. doi: 10.1023/a:1020820103126. [DOI] [PubMed] [Google Scholar]