Abstract
Repurposing the macrolide antibiotic azithromycin has recently been suggested as a promising neuroprotective strategy for the acute treatment of ischemic stroke. Here, we aim at further characterizing the immunomodulatory properties of intraperitoneal (i.p.) administration of this drug and, more importantly, at assessing whether neuroprotection can also be achieved by the more clinically relevant intravenous (i.v.) route of administration in a mouse model of focal cerebral ischemia induced by transient (30-min) middle cerebral artery occlusion (MCAo).
A single i.p. injection of azithromycin (150 mg/kg) upon reperfusion prevented ischemia-induced spleen contraction and increased the number of MAC-1-immunopositive microglia/macrophages in the ischemic hemisphere 48 h after the insult. This was paralleled by an elevation of alternatively activated phenotypes (i.e., Ym1-immunopositive M2-polarized cells) and by a reduced expression of the pro-inflammatory marker myeloperoxidase. More importantly, i.v. administration of azithromycin upon reperfusion reduced MCAo-induced infarct volume and cerebral edema to an extent comparable to that obtained via the i.p. route. Although the i.p. route is often used for research purposes, it is impractical in the clinical setting; however, i.v. administration can easily be used in ischemic stroke patients who usually have i.v. access already established on hospital admission.
The neuroprotective efficacy of the clinically relevant i.v. administration of azithromycin, together with its beneficial immunomodulatory properties reported in mice subjected to transient MCAo, suggests that this macrolide antibiotic can be effectively repurposed for the acute treatment of ischemic stroke. To this end, further work is needed to validate the efficacy of azithromycin in the clinical setting.
Introduction
Innate immunity is strongly implicated in the development of ischemic brain injury whereby, beside the activation of cerebral glia, a spatiotemporally defined brain recruitment of leukocytes accompanies the progression of cerebral inflammation and damage.1 Accordingly, recent blood genomic profiling studies have shown that the majority of the genes upregulated in patients early after an ischemic stroke control inflammation and are expressed by innate immune cells, namely polymorphonuclear leukocytes and monocytes.2–5
Innate immune cells participate either in detrimental responses or in repair and regenerative mechanisms, depending on the specific cell type engaged. In particular, local activation of microglia as well as cerebral infiltration of blood-borne macrophages and neutrophils exert a dualistic role in ischemic brain damage.6 The classic M1 phenotype of microglia/macrophages triggers injurious responses, whereas alternatively activated M2 phenotypes scavenge debris and promote angiogenesis, tissue remodeling, and repair.7–11 Intriguingly, although neutrophils have classically been regarded as detrimental, being correlated with poor histological and functional outcomes after stroke,12–16 recent findings suggest that brain recruitment of N2 phenotypes may provide beneficial effects.17,18
Thus, a strategic approach to rescue ischemic brain injury would consist in promoting polarization shifts toward M2 or N2 phenotypes, while reducing activation of pro-inflammatory phenotypes during the acute phase after stroke. Following this aim, few drugs have to date proved successful in preclinical settings and most of these studies focused on repurposing existing drugs.19 In fact, the use of drugs with a well-established safety profile and for which the target in humans has been already validated allows to drastically reduce the rate of clinical trial failure that has dominated the unsuccessful development of neuroprotective drugs in stroke during the past decades.19–21
Following the concept of drug repurposing, with the aim of exerting a rational immunomodulation, we have recently validated the preclinical efficacy of azithromycin (9-deoxy-9a-aza-9a-methyl-9a-homoerythromycin A), a dibasic macrolide antibiotic that accumulates in macrophages and neutrophils22–24 and displays prolonged antibacterial as well as anti-inflammatory and immunomodulatory effects.25 Acute intraperitoneal (i.p.) administration of azithromycin to mice subjected to transient middle cerebral artery occlusion (MCAo) significantly reduced blood–brain barrier leakage and cerebral damage by decreasing brain infiltration of circulating neutrophils and by promoting macrophage polarization toward the non-inflammatory M2 phenotype.26
Here, we aim at extending these findings by assessing the effects of a clinically relevant administration route and by further characterizing the drug-induced regulation of the immune system in a murine model of focal cerebral ischemia. Our findings demonstrate that azithromycin was able to prevent ischemia-induced spleen contraction, while increasing the number of activated microglia/macrophages in the ischemic hemisphere. This was associated with a reduced expression of pro-inflammatory markers and with significant neuroprotection. Notably, the reduction of cerebral infarct damage produced by intravenous (i.v.) administration of azithromycin upon reperfusion was comparable to that observed when the drug was administered intraperitoneally.
Materials and Methods
Animals and Drug Treatments
All the experiments were performed on adult C57Bl/6 male mice, weighing 24–26 g (Charles River Laboratories), housed under controlled conditions (temperature of 22°C, relative humidity of 65%, and 12 h light:12 h dark cycle), with free access to food and water.
Animal care and experimental procedures were performed in accordance with the guidelines of the Italian Ministry of Health (DM 116/1992 and DL 26/2014) and with the European directive 2010/63/UE. The protocols (numbers 120000344 and 1277/2015-PR) were approved by the committee set up by the Ministry of Health at the National Institute of Health (Rome). All efforts were made to keep to a minimum the number of animals used and their suffering.
Animals were randomly allocated to each experimental group, namely ischemia or sham surgery, drug or vehicle administration, and i.p. or i.v. route of administration. Azithromycin (Zithromax®, azithromycin dihydrate for injection; Pfizer) was dissolved in saline (0.9% NaCl) and administered at the dose of 150 mg/kg by the i.p. or i.v. route upon reperfusion. Vehicle-control animals received an i.p. or i.v. injection of saline (1 mL/kg) upon reperfusion.
Transient Focal Cerebral Ischemia
Focal brain ischemia was obtained by proximal occlusion of the origin of the middle cerebral artery, using a relatively non-invasive technique.27 Briefly, mice were anesthetized with 1.5%–2% isoflurane that was vaporized in air, and the external carotid artery was isolated and cut ∼1.5 mm above the common carotid artery bifurcation. A silicone-coated nylon filament (diameter: 0.23 mm; Doccol Corporation) was then inserted into the external carotid artery and advanced through the internal carotid artery up to the circle of Willis. To allow reperfusion, the filament was withdrawn 30 min after vessel occlusion.
During surgery, cerebral blood flow was continuously monitored over the fronto-parietal cerebral cortex of the ischemic hemisphere, corresponding to the supply territory of the middle cerebral artery, by laser-Doppler flowmetry (Periflux System 5000; Perimed).
Sham-operated animals underwent all the surgical procedures performed for MCAo, with the exception of complete filament insertion.
Quantification of Ischemic Brain Damage
To assess brain infarct damage, animals were sacrificed 48 h after the beginning of reperfusion and their brains were immediately frozen. Thirteen 20 μm-thick coronal sections were obtained using a cryostat, at 0.5 mm intervals from the frontal pole, mounted on glass slides, and stained with cresyl violet. Images were blindly analyzed using an image analysis software (ImageJ, version 1.30), and infarct volume (mm3) was calculated by summing the infarcted (pale) areas of the coronal slices and multiplying the obtained value by the interval thickness between sections. Infarct edema was calculated by subtracting the size of the entire contralateral hemisphere from the total ipsilateral (infarcted) hemisphere.
To investigate the involvement of the spleen in stroke pathology, spleens were quickly dissected 48 h after the beginning of reperfusion (or after sham surgery) and weighed.
Immunofluorescence
Animals (n = 3 per experimental group) were anesthetized with isoflurane and perfused through the heart with heparinized (4,000 U/mL) saline (0.9% NaCl) followed by 4% paraformaldehyde in phosphate buffer (PB, 0.1 M; pH 7.4). Brains were dissected, post-fixed for 2 h, and cryoprotected in 30% sucrose in PB solution at 4°C. Forty micrometer-thick coronal brain sections, at the level of the middle cerebral artery territory (1.18 to −0.10 from Bregma), were obtained using a cryostat and collected in PB.
After a pre-incubation for 1 h in blocking solution (5% normal donkey serum, 0.3% Triton X-100 in PB), sections were incubated overnight at 4°C with the following primary antibodies: rat anti-MAC-1 (CD11b, 1:200 dilution, code MCA74; AbD Serotec), rabbit anti-myeloperoxidase (MPO, 1:200, code sc-16129; Santa Cruz Biotechnology), and/or rabbit anti-Ym1 (1:100, code 01404; StemCell Technologies) to label alternatively activated microglia/macrophages.28,29 After three washes in PB, sections were incubated for 2 h at room temperature in a solution containing an appropriate mixture of the corresponding secondary antibodies labeled with AlexaFluor 488 or AlexaFluor 594 (1:400 dilution; Molecular Probes, Invitrogen). Finally, nuclei were counterstained with 4′,6-diamidino-2-phenylindole (DAPI, 1:500; Sigma-Aldrich), and the sections were mounted on slides and coverslipped as previously described.30 Immunostaining was examined under a fluorescence microscope (Leica DMI6000B; Leica Microsystems Srl) equipped with a high-resolution digital camera (Leica DFC350FX) and a dedicated software (LAS AF6000) for image analysis and deconvolution.
To quantify microglia/macrophages, MAC-1-immunopositive cells were counted in the ipsilateral striatum of vehicle- and azithromycin-treated mice subjected to transient MCAo. Briefly, three coronal brain sections, corresponding to the middle cerebral artery territory, were taken from each brain at 0.98, 0.38, and −0.22 mm from Bregma. Digitized images were acquired under identical microscope settings and cells were counted off-line, using ImageJ software, in three different optic fields of the confocal images (acquired through the 20 × objective). For each optic field, the total number of DAPI-stained cells labeled for MAC-1 were counted and expressed as number of immunopositive cells/mm2.
Statistical Analysis
Data are expressed as mean ± standard error of the mean and subjected to statistical analysis using Graph-Pad Prism version 5.00 for Windows (GraphPad Software). The two-tailed Student's t-test was used for comparison of a single factor between two groups, whereas one-way or two-way ANOVA was used to compare more than two groups. P values below 0.05 were regarded as statistically significant.
Results
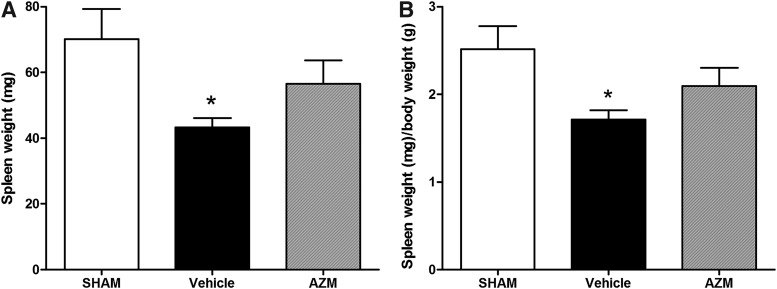
To evaluate the immunomodulatory properties of azithromycin, we initially examined its effects on spleen modifications induced by transient MCAo in mice. According to previous studies,31–33 we found that spleen size was significantly reduced after 48h of reperfusion with respect to sham surgery (Fig. 1A). By contrast, spleen size was unaffected in mice subjected to transient MCAo receiving an i.p. injection of azithromycin (150 mg/kg) upon reperfusion (Fig. 1A). Since body and spleen weights are significantly correlated in normal mice,34 we assessed the possibility that splenic contraction may be due to body weight loss due to the ischemic insult. Normalization of spleen weight by body weight still revealed significant splenic contraction in vehicle-injected ischemic mice, but not in animals treated with azithromycin (Fig. 1B).
Fig. 1.
Effect of azithromycin on spleen weight in mice subjected to transient MCAo. Quantification of spleen size expressed as absolute weight (A) or as ratio of spleen to body weight (B). Mice subjected to 30-min MCAo, followed by 48 h of reperfusion, show a significant reduction in their spleen size as compared with sham-operated animals. Conversely, in mice treated with azithromycin (150 mg/kg, i.p., upon reperfusion), spleen weight was unaffected by the ischemic insult. *P < 0.05 versus sham (one-way ANOVA followed by Tukey's multiple-comparison test, n = 5 animals per experimental group). ANOVA, analysis of variance; i.p., intraperitoneal; MCAo, middle cerebral artery occlusion.
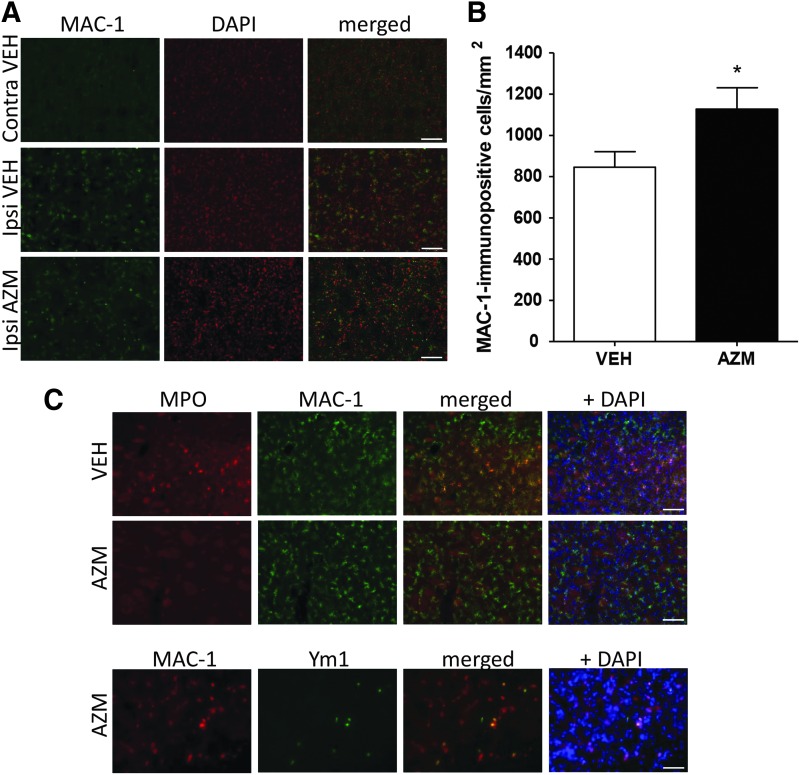
Since previous work has suggested that splenic atrophy strongly influences the progression of ischemic brain injury by promoting brain infiltration of leukocytes and local activation of microglial cells, we have here assessed the relevance of these mechanisms in the neuroprotection exerted by azithromycin. After 30-min MCAo followed by 48 h of reperfusion, in the ischemic striatum of vehicle-injected animals, MAC-1-immunopositive cells were significantly elevated (Fig. 2A). Microglia displayed the typical morphological modifications induced by an ischemic insult, namely enlarged cell bodies, shortened processes, and acquisition of an amoeboid phenotype indistinguishable from infiltrating macrophages.11,35,36
Fig. 2.
Azithromycin elevates the number of non-inflammatory microglia/macrophages in the ipsilateral ischemic hemisphere of mice subjected to transient MCAo. (A) Representative immunofluorescence images showing expression of MAC-1 (green fluorescence) in the ipsilateral (Ipsi) and contralateral (Contra) striatum of mice subjected to 30-min MCAo followed by 48 h of reperfusion and injected with vehicle (VEH, saline, 1 mL/kg) or azithromycin (AZM, 150 mg/kg), i.p., upon reperfusion. Cell nuclei were counterstained with DAPI (red signal). (B) As compared with vehicle-injected animals, azithromycin elevates the number of MAC-1-immunopositive microglia/macrophages in the ipsilateral striatum. Scale bar: 100 μm. *P < 0.05 versus vehicle (two-tailed Student's t-test, n = 3 animals per experimental group). (C) Representative immunofluorescence images of the ischemic striatum showing colocalization of the microglia/macrophages marker MAC-1 with MPO, a marker of M1 polarization in vehicle-injected animals (VEH, saline 1 mL/kg, i.p., upon reperfusion), but not in mice treated with azithromycin (AZM, 150 mg/kg, i.p., upon reperfusion) subjected to 30-min MCAo followed by 48 h of reperfusion. Conversely, microglia/macrophages from mice treated with azithromycin were immunopositive for the M2 marker Ym1. Cell nuclei were counterstained with DAPI (blue signal). Scale bars: 100 μm. MPO, myeloperoxidase.
Acute treatment with azithromycin (150 mg/kg.i.p., upon reperfusion) further elevated the number of activated microglia/macrophages in the ischemic striatum, as documented by both immunofluorescence images (Fig. 2A) and quantitative analysis of MAC-1-immunopositive cells (Fig. 2B). In vehicle-injected animals, we observed that not only numerous MAC-1-immunopositive microglia/macrophages (Fig. 2C) but also some Ly6B-immunopositive neutrophils (data not shown) were immunopositive for MPO. The expression of this pro-inflammatory enzyme was almost absent in mice treated with azithromycin, where we detected a selective enhancement of the M2 marker Ym1 in microglia/macrophages (Fig. 2C, lower panel).
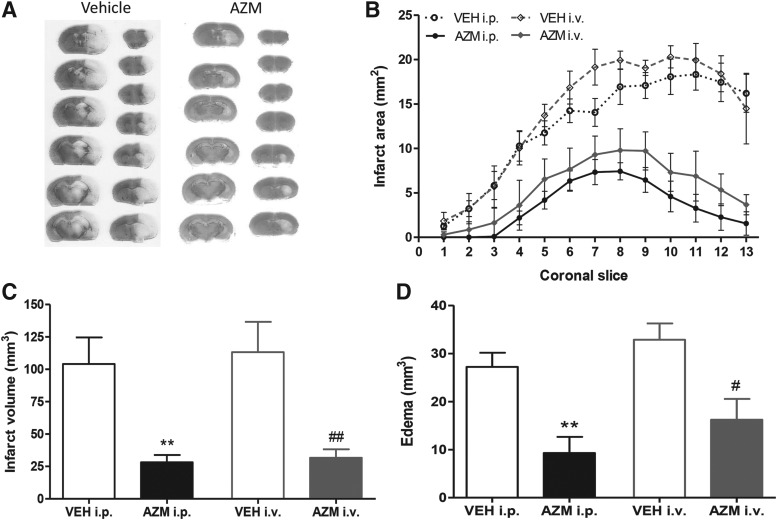
These immunomodulatory properties of azithromycin resulted in a significant reduction of brain infarct damage and edema (Fig. 3). Moreover, to increase the translational value of our findings, we have assessed the effects of a clinically relevant route of administration. Thus, we found that an i.v. injection of azithromycin reduced infarct damage in peri-ischemic cortical regions, as revealed by cresyl violet staining of coronal brain sections (Fig. 3A). Notably, the reduced extension of cerebral infarct (Fig. 3B, C) and edema (Fig. 3D) produced by i.v. administration of azithromycin was comparable to the neuroprotection exerted by i.p. administration of the same dose (150 mg/kg) of the drug.
Fig. 3.
Reduction of ischemic brain damage produced by a single i.v. administration of azithromycin is comparable to the neuroprotection observed after i.p. administration of the drug. (A) Representative cresyl violet-stained coronal brain sections from mice subjected to transient MCAo and receiving an i.v. injection of vehicle (saline, 1 mL/kg) or azithromycin (AZM, 150 mg/kg) upon reperfusion. (B) Brain infarct areas (pale areas in A), (C) infarct volume, and (D) edema of mice subjected to transient MCAo and treated i.p. or i.v. with a single dose of azithromycin (AZM, 150 mg/kg) or vehicle (VEH, saline, 1 mL/kg) upon reperfusion. **P < 0.01 versus VEH i.p.; ##P < 0.01 versus VEH i.v.; and #P < 0.05 versus VEH i.v. (two-way ANOVA followed by Bonferroni post-test, n = 5 mice per experimental group). i.v., intravenous.
Discussion
The results of the present study demonstrate that neuroprotection exerted by azithromycin involves modulation of the immune system, as documented by the evidence that this drug prevents ischemia-induced spleen atrophy and elevates the number of non-inflammatory microglia/macrophages in the ischemic hemisphere.
More importantly, to increase the clinical relevance of our findings, we have demonstrated that azithromycin reduces ischemic brain damage when administered intravenously, namely via a route that is compatible with human treatment. In fact, the route of drug administration is a critical consideration in preclinical investigation of novel therapeutics. Although the i.p. route is often used for research purposes, it is impractical and cumbersome in the clinical setting. By contrast, i.v. administration can easily be used in patients, especially in those who have undergone an ischemic stroke and who usually have i.v. access already established on hospital admission.
Moreover, given the rapidity of the effects of brain ischemia on cerebral metabolism, neuroprotective treatment should be given by the most rapidly effective means, which, in practice, means intravenously, allowing to attain effective plasma and brain levels of drugs promptly.37 As such, i.v. administration of azithromycin is not inferior to the i.p. route, making it attractive for clinical application. This, together with the evidence that the neuroprotective effects of azithromycin are observed at doses demonstrated to be well tolerated in humans,26,38 encourages further work that is aimed at assessing the efficacy of azithromycin in human stroke, to provide support to the effective repositioning of this macrolide antibiotic for the treatment of cerebral ischemia.
The relevance of the repurposing approach in ischemic stroke is related to the fact that during the past three decades, all the clinical trials performed with neuroprotective drugs have failed due to excessive toxicity or lack of efficacy.21,39 In this context, the use of drugs for which the human target has often been already validated, which are characterized by a well-established safety profile, will dramatically reduce the risk of clinical trial failure, thus significantly boosting the discovery of novel stroke therapeutics.19,40–42 This latter aim is further supported by the fact that azithromycin provides neuroprotection through the modulation of immune mechanisms that are recruited at later times after the acute event, allowing to extend the therapeutic time-window.
In addition to our previous observations,26 the effect of azithromycin on the peripheral immune system is demonstrated by its ability to prevent ischemia-induced splenic atrophy, a hallmark of post-stroke peripheral immune activation. In fact, a few days after stroke, a significant reduction of immune cells, particularly monocytes/macrophages, T and B cells occurs in secondary lymphatic organs, leading to their atrophy.43–46 Accordingly, here we found that spleen weight is significantly reduced 48 h after reperfusion in mice subjected to transient MCAo. In fact, compared with pre-stroke conditions, spleen weight is reduced by 3 h until 7 days after transient focal cerebral ischemia in mice, and this contraction is accompanied by monocyte/macrophage mobilization and migration to the stroked brain.46,47
Although some studies have failed to confirm that monocytes/macrophages mobilized from the spleen have a direct role in ischemic brain injury,46 there is strong evidence supporting the concept that splenic atrophy may affect ischemic brain injury by exacerbating the inflammatory response through the release of spleen-derived immune cells into the circulation, their migration to the brain, and the activation of microglial cells.32–34,48–51 Accordingly, splenic contraction in stroke patients is positively correlated with higher circulating levels of several cytokines.52 Indeed, our data show a clear correlation between ischemia-induced splenic atrophy or azithromycin-induced splenic preservation and the histological outcome, confirming previous evidence.18,53,54
Interestingly, although splenic preservation by azithromycin was accompanied by a further elevation of activated microglia/macrophages in the ischemic hemisphere, these cells were characterized by an anti-inflammatory phenotype. This suggests that spleen size may not directly reflect mobilization of cells to the brain, but it is, indeed, correlated with the inflammatory cerebral milieu. In addition, the profound systemic immunodepression caused by brain ischemia predisposes to infectious complications that represent a major cause of death in ischemic stroke patients.43,55 Therefore, it is intriguing to speculate that by attenuating splenic atrophy, azithromycin may also ameliorate stroke-induced immunodepression, lowering the risk of post-stroke infections independently from its antibacterial activity.
Brain injury triggered by ischemic stroke involves an important activation of local microglia that is accompanied by a significant infiltration of peripheral immune cells into the infarcted area.35,56,57 Among these cells, monocytes/macrophages exert a dualistic role on the progression of post-ischemic inflammation and injury, depending on their polarization toward inflammatory M1 or reparative M2 phenotypes.1,6 According to previous findings, we observed a significant elevation of activated microglia/macrophages that were immunopositive for MPO in the ipsilateral hemisphere after 48h of reperfusion.36,58,59 Paradoxically, azithromycin further elevates the number of microglia/macrophages in the ischemic brain, although these cells did not express MPO, while showing immunopositivity for the M2 marker Ym1.
MPO is a key inflammatory enzyme that has been implicated in ischemic stroke pathophysiology both in animal models13,60 and in patients.61,62 MPO is widely distributed in ischemic tissues, and it correlates positively with infarct size; peak levels of its activity in vivo occur on day 3 after ischemia.63,64 Upon activation by the ischemic insult, MPO generates highly reactive oxygen species and provides detrimental effects by inducing apoptosis, nitro-tyrosination of proteins and by enhancing the expression of pro-inflammatory cytokines.65–67
Since MPO is abundantly found within the azurophilic granules of neutrophils,68 its expression or activity has been extensively used to quantify neutrophil infiltration in the ischemic brain.13,14,69–74 Nevertheless, MPO activity assay is an indirect method and does not exclusively detect neutrophils. In fact, although to a lesser extent, MPO is also expressed in other myeloid cells, especially in monocytes and microglia/macrophages.64,69,75–77 Unlike macrophages in other parts of the body, brain microglia are positive for MPO during neurodegenerative diseases,77–79 whereas normal brain microglia rarely express this enzyme.77,80,81 Accordingly, in the present study, we have demonstrated that the elevated expression of MPO does mainly occur in microglia/macrophages of the ischemic hemisphere of mice subjected to transient MCAo.
Nevertheless, it cannot be excluded that MPO immunopositivity may stem from neutrophil debris phagocytosed by microglia/macrophages. In fact, resolution of the neutrophil inflammatory response after cerebral ischemia begins with the removal of neutrophils, either by necrosis or by apoptosis, followed by macrophage phagocytosis.63,82 Consequently, previous studies that have used MPO as a marker to measure neutrophil accumulation may have miscalculated the number of neutrophils within the ischemic territory and, thus, their contribution to the progression of the infarct.63,83
The evidence that expression of MPO is virtually absent in microglia/macrophages populating the infarcted hemisphere of the mice treated with azithromycin suggests that this drug reduces cellular polarization toward detrimental phenotypes. In fact, the elevation of MPO-like peroxidase activity has been associated with the shift of microglia from a protective to a neurotoxic phenotype.84 This is consistent with previous findings highlighting that azithromycin significantly reduces lipopolysaccharide-induced elevation of MPO concentration in lung homogenates of mice.85 Moreover, we previously demonstrated that the number of F4/80+/CD11b+ microglia/macrophages of the ipsilateral hemisphere was dramatically reduced by azithromycin in mice subjected to transient MCAo followed by two hours of reperfusion in mice.26 This was coincident with a significant reduction in F4/80+/Gr1+ infiltrating inflammatory macrophages in the ischemic hemisphere.
By contrast, at later reperfusion times, that is, 24 h after intraluminal filament removal, the mice treated with azithromycin were characterized by an elevated number of F4/80+/CD11b+ microglia/macrophages in the ischemic hemisphere as compared with vehicle-injected animals, and this was accompanied by an elevation of markers of M2 polarization.26 In the present work, we further extend these findings by showing that 48 h after the beginning of reperfusion, azithromycin elevates the number of MAC-1-immunopositive microglia/macrophages in the ischemic hemisphere as compared with vehicle-injected control animals. These cells were characterized by a globular morphology, likely resembling reactive amoeboid microglia or infiltrating macrophages. Despite the elevation of MAC-1-immunopositive cells, the ischemic striatum of azithromycin-treated mice was characterized by a reduced expression of the pro-inflammatory enzyme MPO, whereby microglia/macrophages mainly expressed Ym1, a marker of M2 polarization.
The ability of azithromycin to trigger the shift of microglia/macrophages toward protective M2 phenotypes may represent a crucial mechanism involved in neuroprotection. In fact, preservation of alternatively activated M2 microglia/macrophages promotes neuronal survival and functional recovery under ischemic/hypoxic conditions.8–10,86–88
The mechanism by which azithromycin shifts macrophages from the classically activated (M1) to the alternatively activated (M2) phenotype has not been completely elucidated89–91; however, AP-1 activation and impairment of lysosomal functions may be probably involved.92,93 These immunomodulatory properties contribute to the clinical efficacy of azithromycin in respiratory diseases,25 whereas their relevance in neurodegenerative conditions has only been partially explored.
The immunomodulatory effects of azithromycin result in a significant neuroprotection exerted by an i.p. injection of the drug upon reperfusion.26 Here, we extend our previous observation and demonstrate that a reduction of infarct volume, comparable to that provided by i.p. administration, is produced by administering azithromycin intravenously, namely via a clinically relevant route of administration. This is consistent with the recommendations provided by the Stroke Therapy Academic Industry Roundtable (STAIR) that is aimed at improving preclinical studies to increase the translational potential of experimental stroke treatments.94 This is crucial, since promising treatments validated in preclinical models usually fail in clinical trials. Although the validity of the STAIR's recommendations has not been always confirmed,95–97 they represent a useful guide for researchers planning preclinical stroke studies by providing directions on the selection and execution of the animal model, the fundamentals of good scientific inquiry, the choice and measurement of outcomes, and the drug/treatment administration, including the route and time-window.98–100 We have previously defined the dose–response curve and the time-window for the neuroprotective effects of acute i.p. administration of azithromycin to mice subjected to transient MCAo.26 The ED50 (0.59 mg/kg) is lower than the bactericidal dose of the drug in mice and is 100 times lower than the dose demonstrated to be well tolerated in humans.38 This, together with the evidence that azithromycin is effective when administered up to 4.5 h after the insult, makes this drug compatible with human treatment. Here, we have extended our previous findings, with the aim of increasing their translational potential, by demonstrating that azithromycin is also effective when administered intravenously, namely through a clinically relevant route that can safely and easily be used in stroke patients who usually have i.v. access established in the hospital setting. By contrast, potentially damaging routes (e.g., intracerebroventricular or intrathecal routes) or oral administration, which is often unfeasible in stroke patients, are usually less preferred.
In conclusion, the present work reaffirms the potentiality of developing azithromycin as a novel acute treatment for ischemic stroke, given the advantages of repurposing an off-patent drug, characterized by a low toxicity profile in humans, that provides significant neuroprotection in pre-clinical models by modulating the immune response.
Abbreviations Used
- ANOVA
analysis of variance
- AZM
azithromycin
- DAPI
4′,6-diamidino-2-phenylindole
- i.p.
intraperitoneal
- i.v.
intravenous
- MCAo
middle cerebral artery occlusion
- MPO
myeloperoxidase
- PB
phosphate buffer
- STAIR
Stroke Therapy Academic Industry Roundtable
- VEH
vehicle
Acknowledgments
Financial support from the Italian Ministry of University and Research (PRIN prot. 20089 BARSR_004 to GB) and from the University of Calabria (ex quota 60%) is gratefully acknowledged. Mr. Guido Fico is acknowledged for skillful technical assistance.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1.Amantea D, Micieli G, Tassorelli C, et al. : Rational modulation of the innate immune system for neuroprotection in ischemic stroke. Front Neurosci 2015;9:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang Y, Xu H, Du X, et al. : Gene expression in blood changes rapidly in neutrophils and monocytes after ischemic stroke in humans: a microarray study. J Cereb Blood Flow Metab 2006;26:1089–1102 [DOI] [PubMed] [Google Scholar]
- 3.Barr TL, Conley Y, Ding J, et al. : Genomic biomarkers and cellular pathways of ischemic stroke by RNA gene expression profiling. Neurology 2010;75:1009–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barr TL, VanGilder R, Rellick S, et al. : A genomic profile of the immune response to stroke with implications for stroke recovery. Biol Res Nurs 2015;17:248–256 [DOI] [PubMed] [Google Scholar]
- 5.Oh SH, Kim OJ, Shin DA, et al. : Alteration of immunologic responses on peripheral blood in the acute phase of ischemic stroke: blood genomic profiling study. J Neuroimmunol 2012;249:60–65 [DOI] [PubMed] [Google Scholar]
- 6.Amantea D, Tassorelli C, Petrelli F, et al. : Understanding the multifaceted role of inflammatory mediators in ischemic stroke. Curr Med Chem 2014;21:2098–2117 [DOI] [PubMed] [Google Scholar]
- 7.Gliem M, Klotz L, van Rooijen N, et al. : Hyperglycemia and PPARγ antagonistically influence macrophage polarization and infarct healing after ischemic stroke. Stroke 2015;46:2935–2942 [DOI] [PubMed] [Google Scholar]
- 8.Frieler RA, Meng H, Duan SZ, et al. : Myeloid-specific deletion of the mineralocorticoid receptor reduces infarct volume and alters inflammation during cerebral ischemia. Stroke 2011;42:179–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu X, Li P, Guo Y, et al. : Microglia/macrophage polarization dynamics reveal novel mechanism of injury expansion after focal cerebral ischemia. Stroke 2012;43:3063–3070 [DOI] [PubMed] [Google Scholar]
- 10.Xu Y, Qian L, Zong G, et al. : Class A scavenger receptor promotes cerebral ischemic injury by pivoting microglia/macrophage polarization. Neuroscience 2012;218:35–48 [DOI] [PubMed] [Google Scholar]
- 11.Fumagalli S, Perego C, Pischiutta F, et al. : The ischemic environment drives microglia and macrophage function. Front Neurol 2015;6:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akopov S, Simonian N, Grigorian G: Dynamics of polymorphonuclear leukocyte accumulation in acute cerebral infarction and their correlation with brain tissue damage. Stroke 1996;27:1739–1743 [DOI] [PubMed] [Google Scholar]
- 13.Matsuo Y, Onodera H, Shiga Y, et al. : Correlation between myeloperoxidase-quantified neutrophil accumulation and ischemic brain injury in the rat. Effects of neutrophil depletion. Stroke 1994;25:1469–1475 [DOI] [PubMed] [Google Scholar]
- 14.Jiang N, Moyle M, Soule HR, et al. : Neutrophil inhibitory factor is neuroprotective after focal ischemia in rats. Ann Neurol 1995;38:935–942 [DOI] [PubMed] [Google Scholar]
- 15.Connolly ES, Winfree CJ, Springer TA, et al. : Cerebral protection in homozygous null ICAM-1 mice after middle cerebral artery occlusion. Role of neutrophil adhesion in the pathogenesis of stroke. J Clin Invest 1996;97:209–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perez-de-Puig I, Miró-Mur F, Ferrer-Ferrer M, et al. : Neutrophil recruitment to the brain in mouse and human ischemic stroke. Acta Neuropathol 2015;129:239–257 [DOI] [PubMed] [Google Scholar]
- 17.Cuartero MI, Ballesteros I, Moraga A, et al. : N2 neutrophils, novel players in brain inflammation after stroke: modulation by the PPARγ agonist rosiglitazone. Stroke 2013;44:3498–3508 [DOI] [PubMed] [Google Scholar]
- 18.Certo M, Endo Y, Ohta K, et al. : Activation of RXR/PPARγ underlies neuroprotection by bexarotene in ischemic stroke. Pharmacol Res 2015;102:298–307 [DOI] [PubMed] [Google Scholar]
- 19.Amantea D, Bagetta G: Drug repurposing for immune modulation in acute ischemic stroke. Curr Opin Pharmacol 2016;26:124–130 [DOI] [PubMed] [Google Scholar]
- 20.Tymianski M: Novel approaches to neuroprotection trials in acute ischemic stroke. Stroke 2013;44:2942–2950 [DOI] [PubMed] [Google Scholar]
- 21.Grupke S, Hall J, Dobbs M, et al. : Understanding history, and not repeating it. Neuroprotection for acute ischemic stroke: from review to preview. Clin Neurol Neurosurg 2015;129:1–9 [DOI] [PubMed] [Google Scholar]
- 22.Fieta A, Merlini C, Grassi G: Requirements for intracellular accumulation and release of clarithromycin and azithromycin by human phagocytes. J Chemother 1997;9:23–31 [DOI] [PubMed] [Google Scholar]
- 23.Bosnar M, Kelnerić Z, Munić V, Eraković VPM: Cellular uptake and efflux of azithromycin, erythromycin, clarithromycin, telithromycin, and cethromycin. Antimicrob Agents Chemother 2005;49:2372–2377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu P, Allaudeen H, Chandra R, et al. : Comparative pharmacokinetics of azithromycin in serum and white blood cells of healthy subjects receiving a single-dose extended-release regimen versus a 3-day. Antimicrob Agents Chemother 2007;51:103–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parnham MJ, Haber VE, Giamarellos-Bourboulis EJ, et al. : Azithromycin: mechanisms of action and their relevance for clinical applications. Pharmacol Ther 2014;143:225–245 [DOI] [PubMed] [Google Scholar]
- 26.Amantea D, Certo M, Petrelli F, et al. : Azithromycin protects mice against ischemic stroke injury by promoting macrophage transition towards M2 phenotype. Exp Neurol 2016;275:116–125 [DOI] [PubMed] [Google Scholar]
- 27.Amantea D, Tassorelli C, Russo R, et al. : Neuroprotection by leptin in a rat model of permanent cerebral ischemia: effects on STAT3 phosphorylation in discrete cells of the brain. Cell Death Dis 2011;2:e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sica A, Mantovani A: Macrophage plasticity and polarization: in vivo veritas. J Clin Invest 2012;122:787–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viscomi MT, Florenzano F, Latini L, et al. : Methylprednisolone treatment delays remote cell death after focal brain lesion. Neuroscience 2008;154:1267–1282 [DOI] [PubMed] [Google Scholar]
- 30.Amantea D, Certo M, Russo R, et al. : Early reperfusion injury is associated to MMP2 and IL-1β elevation in cortical neurons of rats subjected to middle cerebral artery occlusion. Neuroscience 2014;277:755–763 [DOI] [PubMed] [Google Scholar]
- 31.Prass K, Meisel C, Höflich C, et al. : Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by poststroke T helper cell type 1-like immunostimulation. J Exp Med 2003;198:725–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liesz A, Hagmann S, Zschoche C, et al. : The spectrum of systemic immune alterations after murine focal ischemia: immunodepression versus immunomodulation. Stroke 2009;40:2849–2858 [DOI] [PubMed] [Google Scholar]
- 33.Jin R, Zhu X, Liu L, et al. : Simvastatin attenuates stroke-induced splenic atrophy and lung susceptibility to spontaneous bacterial infection in mice. Stroke 2013;44:1135–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bao Y, Kim E, Bhosle S, et al. : A role for spleen monocytes in post-ischemic brain inflammation and injury. J Neuroinflammation 2010;7:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stevens SL, Bao J, Hollis J, et al. : The use of flow cytometry to evaluate temporal changes in inflammatory cells following focal cerebral ischemia in mice. Brain Res 2002;932:110–119 [DOI] [PubMed] [Google Scholar]
- 36.Amantea D, Bagetta G, Tassorelli C: Identification of distinct cellular pools of interleukin-1 β during the evolution of the neuroinflammatory response induced by transient middle cerebral artery occlusion in the brain of rat. Brain Res 2010;1313:259–269 [DOI] [PubMed] [Google Scholar]
- 37.Dyker AG, Lees KR: Duration of neuroprotective treatment for ischemic stroke. Stroke 1998;29:535–542 [DOI] [PubMed] [Google Scholar]
- 38.Luke DR, Foulds G, Cohen SF, et al. : Safety, toleration, and pharmacokinetics of intravenous azithromycin. Antimicrob Agents Chemother 1996;40:2577–2581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ginsberg MD: Neuroprotection for ischemic stroke: past, present and future. Neuropharmacology 2008;55:363–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strittmatter SM: Overcoming drug development bottlenecks with repurposing: old drugs learn new tricks. Nat Med 2014;20:590–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jin G, Wong STC: Toward better drug repositioning: prioritizing and integrating existing methods into efficient pipelines. Drug Discov Today 2014;19:637–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amantea D, Michelangelo C, Bagetta G: Drug repurposing and beyond: the fundamental role of pharmacology. Funct Neurol 2015;30:79–81 [PMC free article] [PubMed] [Google Scholar]
- 43.Dirnagl U, Klehmet J, Braun JS, et al. : Stroke-induced immunodepression: experimental evidence and clinical relevance. Stroke 2007;38:770–773 [DOI] [PubMed] [Google Scholar]
- 44.Brait VH, Arumugam TV, Drummond GR, et al. : Importance of T lymphocytes in brain injury, immunodeficiency, and recovery after cerebral ischemia. J Cereb Blood Flow Metab 2012;32:598–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chamorro Á, Meisel A, Planas AM, et al. : The immunology of acute stroke. Nat Rev Neurol 2012;8:401–410 [DOI] [PubMed] [Google Scholar]
- 46.Kim E, Yang J.D Beltran C, et al. . Role of spleen-derived monocytes/macrophages in acute ischemic brain injury. J Cereb Blood Flow Metab 2014;07396:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang J, Dotson AL, Murphy SJ, et al. : Adoptive transfer of immune subsets prior to MCAO does not exacerbate stroke outcome in splenectomized mice. J Syst Integr Neurosci 2015;1:20–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Offner H, Subramanian S, Parker SM, et al. : Splenic atrophy in experimental stroke is accompanied by increased regulatory T cells and circulating macrophages. J Immunol 2006;176:6523–6531 [DOI] [PubMed] [Google Scholar]
- 49.Ajmo CT, Vernon DOL, Collier L, et al. : The spleen contributes to stroke-induced neurodegeneration. J Neurosci Res 2008;86:2227–2234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seifert HA, Hall AA, Chapman CB, et al. : A transient decrease in spleen size following stroke corresponds to splenocyte release into systemic circulation. J Neuroimmune Pharmacol 2012;7:1017–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seifert HA, Leonardo CC, Hall AA, et al. : The spleen contributes to stroke induced neurodegeneration through interferon gamma signaling. Metab Brain Dis 2012;27:131–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vahidy FS, Parsha KN, Rahbar MH, et al. : Acute splenic responses in patients with ischemic stroke and intracerebral hemorrhage. J Cereb Blood Flow Metab 2016;36:1012–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vendrame M, Gemma C, Pennypacker KR, et al. : Cord blood rescues stroke-induced changes in splenocyte phenotype and function. Exp Neurol 2006;199:191–200 [DOI] [PubMed] [Google Scholar]
- 54.Dotson AL, Zhu W, Libal N, et al. : Different immunological mechanisms govern protection from experimental stroke in young and older mice with recombinant TCR ligand therapy. Front Cell Neurosci 2014;8:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Westendorp WF, Nederkoorn PJ, Vermeij J-D, et al. : Post-stroke infection: a systematic review and meta-analysis. BMC Neurol 2011;11:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gelderblom M, Leypoldt F, Steinbach K, et al. : Temporal and spatial dynamics of cerebral immune cell accumulation in stroke. Stroke 2008;40:1849–1857 [DOI] [PubMed] [Google Scholar]
- 57.Jin R, Yang G, Li G: Inflammatory mechanisms in ischemic stroke: role of inflammatory cells. J Leukoc Biol 2010;87:779–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morioka T, Kalehua AN, Streit WJ: Characterization of microglial reaction after middle cerebral artery occlusion in rat brain. J Comp Neurol 1993;327:123–132 [DOI] [PubMed] [Google Scholar]
- 59.Perego C, Fumagalli S, De Simoni M-G: Temporal pattern of expression and colocalization of microglia/macrophage phenotype markers following brain ischemic injury in mice. J Neuroinflammation 2011;8:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Takizawa S, Aratani Y, Fukuyama N, et al. : Deficiency of myeloperoxidase increases infarct volume and nitrotyrosine formation in mouse brain. J Cereb Blood Flow Metab 2002;22:50–54 [DOI] [PubMed] [Google Scholar]
- 61.Hoy A, Leininger-Muller B, Poirier O, et al. : Myeloperoxidase polymorphisms in brain infarction. Association with infarct size and functional outcome. Atherosclerosis 2003;167:223–230 [DOI] [PubMed] [Google Scholar]
- 62.Re G, Azzimondi G, Lanzarini C, et al. : Plasma lipoperoxidative markers in ischaemic stroke suggest brain embolism. Eur J Emerg Med 1997;4:5–9 [PubMed] [Google Scholar]
- 63.Weston RM, Jones NM, Jarrott B, et al. : Inflammatory cell infiltration after endothelin-1-induced cerebral ischemia: histochemical and myeloperoxidase correlation with temporal changes in brain injury. J Cereb Blood Flow Metab 2007;27:100–114 [DOI] [PubMed] [Google Scholar]
- 64.Breckwoldt MO, Chen JW, Stangenberg L, et al. : Tracking the inflammatory response in stroke in vivo by sensing the enzyme myeloperoxidase. Proc Natl Acad Sci U S A 2008;105:18584–18589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lo EH, Moskowitz MA. Jacobs TP: Exciting, radical, suicidal: how brain cells die after stroke. Stroke 2005;36:189–192 [DOI] [PubMed] [Google Scholar]
- 66.Lau D, Baldus S: Myeloperoxidase and its contributory role in inflammatory vascular disease. Pharmacol Ther 2006;111:16–26 [DOI] [PubMed] [Google Scholar]
- 67.Lefkowitz DL, Lefkowitz SS: Microglia and myeloperoxidase: a deadly partnership in neurodegenerative disease. Free Radic Biol Med 2008;45:726–731 [DOI] [PubMed] [Google Scholar]
- 68.Rausch PG, Pryzwansky KB, Spitznagel JK: Immunocytochemical identification of azurophilic and specific granule markers in the giant granules of Chediak-Higashi neutrophils. N Engl J Med 1978;298:693–698 [DOI] [PubMed] [Google Scholar]
- 69.Barone FC, Hillegass LM, Tzimas MN, et al. : Time-related changes in myeloperoxidase activity and leukotriene B4 receptor binding reflect leukocyte influx in cerebral focal stroke. Mol Chem Neuropathol 1995;24:13–30 [DOI] [PubMed] [Google Scholar]
- 70.Barone FC, Hillegass LM, Price WJ, et al. : Polymorphonuclear leukocyte infiltration into cerebral focal ischemic tissue: myeloperoxidase activity assay and histologic verification. J Neurosci Res 1991;29:336–345 [DOI] [PubMed] [Google Scholar]
- 71.Batteur-Parmentier S, Margaill I, Plotkine M: Modulation by nitric oxide of cerebral neutrophil accumulation after transient focal ischemia in rats. J Cereb Blood Flow Metab 2000;20:812–819 [DOI] [PubMed] [Google Scholar]
- 72.Beray-Berthat V, Croci N, Plotkine M, et al. : Polymorphonuclear neutrophils contribute to infarction and oxidative stress in the cortex but not in the striatum after ischemia-reperfusion in rats. Brain Res 2003;987:32–38 [DOI] [PubMed] [Google Scholar]
- 73.Kitagawa K, Matsumoto M, Mabuchi T, et al. : Deficiency of intercellular adhesion molecule 1 attenuates microcirculatory disturbance and infarction size in focal cerebral ischemia. J Cereb Blood Flow Metab 1998;18:1336–1345 [DOI] [PubMed] [Google Scholar]
- 74.Zhang ZG, Chopp M, Tang WX, et al. : Postischemic treatment (2–4 h) with anti-CD11b and anti-CD18 monoclonal antibodies are neuroprotective after transient (2 h) focal cerebral ischemia in the rat. Brain Res 1995;698:79–85 [DOI] [PubMed] [Google Scholar]
- 75.Kochanek PM, Hallenbeck JM: Polymorphonuclear leukocytes and monocytes/macrophages in the pathogenesis of cerebral ischemia and stroke. Stroke 1992;23:1367–1379 [DOI] [PubMed] [Google Scholar]
- 76.Zhang ZG, Chopp M: Measurement of myeloperoxidase immunoreactive cells in ischemic brain after transient middle cerebral artery occlusion in the rat. Neurosci Res Commun 1997;20:85–91 [Google Scholar]
- 77.Karakas M, Koenig W: Myeloperoxidase production by macrophage and risk of atherosclerosis. Curr Atheroscler Rep 2012;14:277–283 [DOI] [PubMed] [Google Scholar]
- 78.Reynolds WF, Rhees J, Maciejewski D, et al. : Myeloperoxidase polymorphism is associated with gender specific risk for Alzheimer's disease. Exp Neurol 1999;155:31–41 [DOI] [PubMed] [Google Scholar]
- 79.Choi D-K: Ablation of the inflammatory enzyme myeloperoxidase mitigates features of Parkinson's disease in mice. J Neurosci 2005;25:6594–6600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ulvestad E, Williams K, Mork S, et al. : Phenotypic differences between human monocytes/macrophages and microglial cells studied in situ and in vitro. J Neuropathol Exp Neurol 1994;53:492–501 [DOI] [PubMed] [Google Scholar]
- 81.Green PS, Mendez AJ, Jacob JS, et al. : Neuronal expression of myeloperoxidase is increased in Alzheimer's disease. J Neurochem 2004;90:724–733 [DOI] [PubMed] [Google Scholar]
- 82.Savill J, Fadok V: Corpse clearance defines the meaning of cell death. Nature 2000;407:784–788 [DOI] [PubMed] [Google Scholar]
- 83.Meszaros AJ, Reichner JS, Albina JE: Macrophage phagocytosis of wound neutrophils. J Leukoc Biol 1999;65:35–42 [DOI] [PubMed] [Google Scholar]
- 84.Sawada M: Neuroprotective and toxic changes in microglia in neurodegenerative disease. Park Relat Disord 2009;15:S39–S41 [DOI] [PubMed] [Google Scholar]
- 85.Bosnar M, Bosnjak B, Cuzic S, et al. : Azithromycin and clarithromycin inhibit lipopolysaccharide-induced murine pulmonary neutrophilia mainly through effects on macrophage-derived granulocyte-macrophage colony-stimulating factor and interleukin-1beta. J Pharmacol Exp Ther 2009;331:104–113 [DOI] [PubMed] [Google Scholar]
- 86.Ballesteros I, Cuartero MI, Pradillo JM, et al. : Rosiglitazone-induced CD36 up-regulation resolves inflammation by PPARγ and 5-LO-dependent pathways. J Leukoc Biol 2014;95:587–598 [DOI] [PubMed] [Google Scholar]
- 87.Jin Q, Cheng J, Liu Y, et al. : Improvement of functional recovery by chronic metformin treatment is associated with enhanced alternative activation of microglia/macrophages and increased angiogenesis and neurogenesis following experimental stroke. Brain Behav Immun 2014;40:131–142 [DOI] [PubMed] [Google Scholar]
- 88.Won S, Lee JK, Stein DG: Recombinant tissue plasminogen activator promotes, and progesterone attenuates, microglia/macrophage M1 polarization and recruitment of microglia after MCAO stroke in rats. Brain Behav Immun 2015;49:267–279 [DOI] [PubMed] [Google Scholar]
- 89.Murphy BS, Sundareshan V, Cory TJ, et al. : Azithromycin alters macrophage phenotype. J Antimicrob Chemother 2008;61:554–560 [DOI] [PubMed] [Google Scholar]
- 90.Feola DJ, Garvy BA, Cory TJ, et al. : Azithromycin alters macrophage phenotype and pulmonary compartmentalization during lung infection with Pseudomonas. Antimicrob Agents Chemother 2010;54:2437–2447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vrančić M, Banjanac M, Nujić K, et al. : Azithromycin distinctively modulates classical activation of human monocytes in vitro. Br J Pharmacol 2012;165:1348–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bosnar M, Čužić S, Bošnjak B, Nujić K, Ergović G, Marjanović N, Pašalić I, Hrvačić B, Polančec D, Glojnarić IEHV: Azithromycin inhibits macrophage interleukin-1beta production through inhibition of activator protein-1 in lipopolysaccharide-induced murine pulmonary neutrophilia. Int Immunopharmacol 2011;11:424–434 [DOI] [PubMed] [Google Scholar]
- 93.Nujić K, Banjanac M, Munić V, et al. : Impairment of lysosomal functions by azithromycin and chloroquine contributes to anti-inflammatory phenotype. Cell Immunol 2012;279:78–86 [DOI] [PubMed] [Google Scholar]
- 94.Kahle MP, Bix GJ: Successfully climbing the “sTAIRs”: surmounting failed translation of experimental ischemic stroke treatments. Stroke Res Treat 2012;2012:374098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Feuerstein GZ, Zaleska MM, Krams M, et al. : Missing steps in the STAIR case: a translational medicine perspective on the development of NXY-059 for treatment of acute ischemic stroke. J Cereb Blood Flow Metab 2008;28:217–219 [DOI] [PubMed] [Google Scholar]
- 96.Liu S, Zhen G, Meloni BP, et al. : Rodent stroke model guidelines for preclinical stroke trials (1st edition). J Exp Stroke Transl Med 2009;2:2–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Minnerup J, Sutherland BA, Buchan AM, et al. : Neuroprotection for stroke: current status and future perspectives. Int J Mol Sci 2012;13:11753–11772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fisher M, Feuerstein G, Howells DW, et al. : Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke 2009;40:2244–2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fisher M, Hanley DF, Howard G, et al. : Recommendations from the STAIR V meeting on acute stroke trials, technology and outcomes. Stroke 2007;38:245–248 [DOI] [PubMed] [Google Scholar]
- 100.Albers GW, Goldstein LB, Hess DC, et al. : Stroke treatment academic industry roundtable (STAIR) recommendations for maximizing the use of intravenous thrombolytics and expanding treatment options with intra-arterial and neuroprotective therapies. Stroke 2011;42:2645–2650 [DOI] [PubMed] [Google Scholar]