Abstract
CONTEXT:
Parenting interventions may prevent adolescent substance use; however, questions remain regarding the effectiveness of interventions across substances and delivery qualities contributing to successful intervention outcomes.
OBJECTIVE:
To describe the effectiveness of parent-focused interventions in reducing or preventing adolescent tobacco, alcohol, and illicit substance use and to identify optimal intervention targeted participants, dosage, settings, and delivery methods.
DATA SOURCES:
PubMed, PsycINFO, ERIC, and CINAHL.
STUDY SELECTION:
Randomized controlled trials reporting adolescent substance use outcomes, focusing on imparting parenting knowledge, skills, practices, or behaviors.
DATA EXTRACTION:
Trained researchers extracted data from each article using a standardized, prepiloted form. Because of study heterogeneity, a qualitative technique known as harvest plots was used to summarize findings.
RESULTS:
A total of 42 studies represented by 66 articles met inclusion criteria. Results indicate that parenting interventions are effective at preventing and decreasing adolescent tobacco, alcohol, and illicit substance use over the short and long term. The majority of effective interventions required ≤12 contact hours and were implemented through in-person sessions including parents and youth. Evidence for computer-based delivery was strong only for alcohol use prevention. Few interventions were delivered outside of school or home settings.
LIMITATIONS:
Overall risk of bias is high.
CONCLUSIONS:
This review suggests that relatively low-intensity group parenting interventions are effective at reducing or preventing adolescent substance use and that protection may persist for multiple years. There is a need for additional evidence in clinical and other community settings using an expanded set of delivery methods.
Despite recent encouraging trends, youth tobacco, alcohol, and other illicit drug use continue to represent a considerable source of youth morbidity and mortality and establish behavioral patterns that have detrimental health outcomes into adulthood.1,2 There is therefore a need to identify effective prevention strategies and to better understand the delivery qualities contributing to successful intervention outcomes.
One approach to adolescent substance use prevention builds on the recognition that parents play a key role in promoting healthy adolescent behaviors and therefore focuses on strengthening parenting skills.2 The influence that parents have on their adolescent children has been substantiated by numerous studies linking a well-defined set of parenting practices (ie, monitoring, discipline, communication) and qualities of parent-youth relationships (ie, warmth, support, acceptance, attachment) to adolescent behavioral outcomes including substance use.3,4 Parenting interventions for parents of adolescents broadly focus on building parent self-efficacy in implementing skills and engaging with their children in a manner encouraging health-protective and preventing risk behaviors. Previous reviews suggest that parent-focused interventions directed at adolescent substance use are effective; however, to the best of our knowledge, no systematic review of parenting interventions delivered during adolescence has looked across multiple substances,3,5,6 nor has any considered intervention delivery modalities or contexts.
With increasing focus on evidence-based adolescent health promotion, and given that poor reach is a known challenge for parenting interventions, consideration of evidence regarding how to most effectively and efficiently reach families of adolescents becomes important.7 Practical questions of interest from the perspective of future implementers include the following: Who needs to be involved, for how long, in what settings, and through what means? However, to the best of our knowledge, no reviews have comprehensively examined the state of the evidence regarding targeted participants (parents only vs both parents and youth), minimal dosages required to achieve outcomes, ideal delivery settings (schools, community organizations, clinics, homes), and optimal delivery modalities. The lack of evidence regarding success of implementation within clinics is problematic at a time when prevention and integrated services are emerging as pediatric primary care targets within the Affordable Care Act.8 In addition, although multiple modalities of program delivery are known to appeal to parents and increasing evidence supports the use of online prevention programming, few reviews have examined the state of the literature across delivery methods for parenting interventions focused on adolescent substance use prevention.7,9
This systematic review therefore aims to assess the effectiveness of parenting interventions over the short and long term on reducing adolescent tobacco, alcohol, and illicit substance use and, secondarily, to describe effectiveness in relation to intervention characteristics (targeted participants, intervention dosage, delivery settings, and delivery method), using visual depictions of qualitative data summaries called harvest plots. These plots represent a novel approach to synthesizing the findings of systematic reviews focused on complex and heterogeneous interventions that cannot be combined into a meta-analysis.10 Results of this review will inform the development, tailoring, and delivery of parent-focused interventions to improve adolescent health.
Methods
Search Strategy
As reported in the review protocol (PROSPERO systematic review registry number CRD42014013069), we searched PubMed, PsycINFO, ERIC, and CINAHL for studies investigating parent-focused interventions designed to reduce substance use in adolescents. Search terms are presented in Table 1. The search included all dates available by respective online databases up to the date of March 1, 2015.
TABLE 1.
Search Terms Used to Search for Articles in PubMed, ERIC, CINAHL, and PsycInfo
| PubMed | (“Family”[Mesh] OR Famil* OR Parent*) AND “Adolescent”[Mesh] AND (“Clinical Trial” [Publication Type] OR “Clinical Trials as Topic”[Mesh]) AND (“Alcohol Drinking”[Mesh] OR “Smoking”[Mesh] OR “Substance-Related Disorders”[Mesh] OR smok* OR substance* OR alcohol* OR marijuana* OR cocaine* OR amphetamine* OR heroine*) |
| ERIC | (parent* OR famil*) AND (“Clinical Trials+” OR Randomized OR “Parenting Education” OR “parent education”) AND (Adol* OR teen* OR youth*) AND (tobacco or smok* or alcohol OR substance or marijuana or cocaine or heroin or methamphetamine or amphetamine or prescription or drug*) |
| CINAHL | (parent* OR famil*) AND (“Clinical Trials+” OR Randomized OR “Parenting Education” OR “parent education”) AND (Adol* OR teen* OR youth*) AND (tobacco or smok* or alcohol OR substance or marijuana or cocaine or heroin or methamphetamine or amphetamine or prescription or drug*) |
| PSYCINFO | (adolescent or teen or youth or adolescents or teens or youths or adolescence) AND (exp family/ or exp Parents/ or exp Parenting Skills/ or exp Family Relations/ or exp Parenting/ or exp Parent Child Relations/) AND (exp Parent Training/ or exp clinical trials/ or exp Family Intervention/ or exp Intervention/) AND (exp Alcohols/ OR exp Drugs/ or drug.mp OR exp Tobacco Smoking/ OR smoking.mp OR tobacco.mp) |
Eligibility Criteria
This review included studies published in any language meeting the following criteria: (1) intervention studies focused on adolescents (mean age of participating youth between 10 and 19 years), (2) reported youth smoking, alcohol, or illicit substance outcomes (intention, initiation, or use), and (3) involved parent training with focus on imparting parenting knowledge, skills, practices, or behaviors.
Exclusion criteria were (1) design not a randomized controlled trial, (2) adolescents were the participating parents, (3) intervention focused on specific populations (eg, parents of children with cystic fibrosis or other medical conditions), (4) study compared 2 parenting interventions without a usual care condition, and (5) individual family therapy interventions distinguished from parenting-skills interventions in their focus on changing behaviors though therapeutic rather than curricular approaches.
Two independent reviewers (DGH and RP) screened titles, abstracts, and full texts of potential articles. A third reviewer (MLA) resolved disagreements regarding inclusion of a study.
Data Extraction and Risk of Bias Assessments
All manuscripts were grouped by study and assigned a study number. Trained researchers (D.G.H., D.C., and J.M.) extracted data from each article using a standardized, prepiloted form. For studies with multiple arms, data were only extracted for the arms that had a parent focus. Extracted outcomes were adolescent smoking, alcohol, other illicit substance, and polysubstance intention to use; initiation of use; and use. Results were documented as either reduced, no change, or increased when compared with control groups at the P < .05 level of significance. Time to follow-up for all reported outcomes were grouped by time from baseline as ≤12 months, 12.1 to 24 months, 24.1 to 48 months, and >48 months. If 2 time points fell within a grouping, the longest time point presented was presented.
Risk of bias was evaluated using the Cochrane Risk of Bias Assessment Tool, a widely used and validated tool.11 Sources of study bias assessed were a) random sequence generation, b) allocation concealment, c) blinding of study personnel and outcome assessment, d) incomplete outcome data, and e) selective outcome reporting. Risk of bias was judged as low, high, or unclear. A summary with the criteria for low risk of bias in each of the domains is presented as a footnote in the Supplemental Table 3. As per Cochrane systematic review recommendations,12 if insufficient information was presented to permit judgment, the risk was scored as “unclear.” To confirm unclear scores, study protocols were searched, and authors were contacted asking additional information on each source of bias. Two independent coders (D.G.H. and J.M.) reviewed each article, study protocol, and authors’ response to determine the risk of bias of each study. Disagreement between coders was resolved by consensus.
Intervention characteristics extracted included “targeted participants,” classified as parents only, parents and youth, and multilevel (targeted teachers, medical providers, or others). “Intervention dosage” was calculated as the amount of time parents were intended to participate in the intervention and was classified into low (≤12 parent-hours), moderate (12.1–24 parent-hours), and high (>24 parent-hours). “Delivery setting” was defined as the primary location of intervention, classified as home, school, community agency, or combination. The primary “method of intervention delivery” was categorized as in-person, typically group sessions with a professional; workbook based; computer based; or a combination. Additional extracted data included youth age described as a range in years or grade level and sex as percent female. Participant race/ethnicity was classified as reported by authors or by the race/ethnicity that comprised >75% of the participants or as diverse populations if no one race/ethnicity comprised >75% of the participants.
Data Synthesis
We used harvest plots to graphically synthesize the findings for the study aims.10 In these plots, each study or study arm for those evaluating multiple interventions is represented by a bar, and the properties of the bar represent features of the study. The height presents the study risk of bias; taller bars represent studies with fewer sources of bias. Because some studies did not achieve low risk of bias on any criteria and thus received a count of zero, the heights on the harvest plots represent the raw counts plus 1. The location within a column represents the study results classified as detrimental effect, no difference, or positive effect using an α of .05. The bar’s color or fill and location within a row represent the analyses of interest.
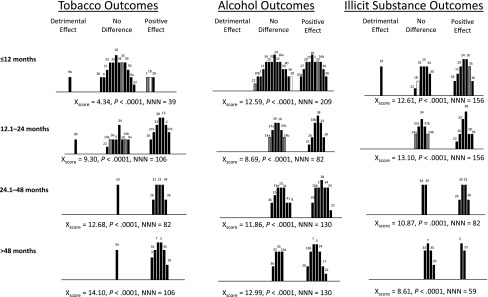
For the first aim, to assess the efficacy of the parenting interventions (see Fig 2), we included all adolescent smoking, alcohol, and illicit substance use outcomes for all reported time points within each study. The bar color indicates whether substance use (black), substance use initiation (gray), or substance use intention (white) was reported in the study. When >1 outcome was reported for a substance, we presented 1 outcome based on the following hierarchy: use, initiation, and intention. The bar’s location within rows represent the follow-up times that the study reported. The 4 studies reporting only polysubstance use outcomes are not included in the harvest plots.
FIGURE 2.
Tobacco, alcohol, and illicit substance use, initiation, and intention outcomes according to length of participant follow-up. Black, substance use; gray, substance use initiation; white, substance use intention. Taller columns represent studies with lower risk of bias. Numbers indicate study ID. Xscore, number of studies needed to be null (NNN).
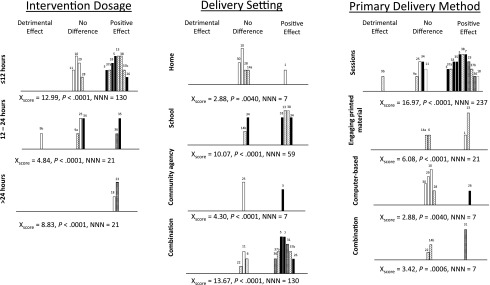
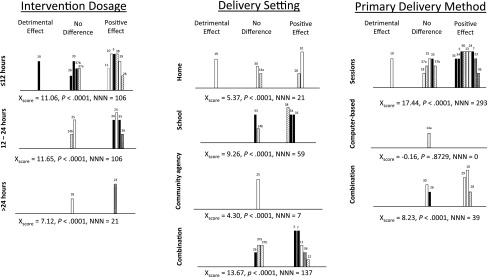
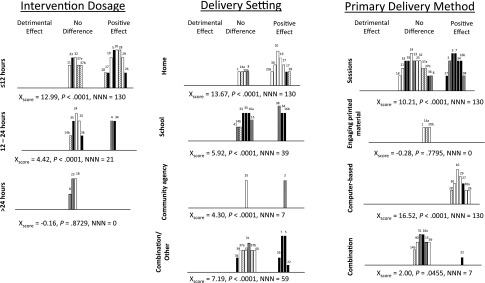
For the second aim, to determine the interventions’ characteristics associated with efficacy (see Figs 3–5), harvest plots synthesize dose intensity, delivery setting, and delivery method for each substance. Only studies reporting these characteristics were included in the plots. In these harvest plots, the bar pattern indicates the longest time point of follow-up for each study; white = ≤12 months, dotted = 12.1 to 24 months, horizontal stripes = 24.1 to 48 months, black = >48 months. The bar’s location within rows represents the characteristic of the intervention in each study. Participant types (eg, parents vs parents and youth) were not presented in harvest plots because of a lack of variability.
FIGURE 3.
Tobacco use at the longest follow-up time according to dose of intervention, setting, primary delivery method, and program duration. White columns, ≤12 months of follow-up; dotted columns, 12.1–24 months of follow-up; horizontal stripe columns, 24.1–48 months of follow-up; black, >48 months of follow-up. Taller columns represent studies with lower risk of bias. Numbers indicate study ID. Xscore, number of studies needed to be null (NNN).
FIGURE 5.
Illicit substance use at the longest follow-up time according to dose of intervention, setting, primary delivery method, and program duration. White columns, ≤12 months of follow-up; dotted columns, 12.1–24 months of follow-up; horizontal stripes, 24.1–48 months of follow-up; black columns, >48 months of follow-up. Taller columns represent studies with lower risk of bias. Numbers indicate study ID. Xscore, number of studies needed to be null (NNN).
Because comparing counts between the number of studies with positive and null results based on the study’s P value for the difference between intervention and control groups might be misleading,13 we conducted a binomial test of proportions for each outcome of interest, using the following formula:
 |
where H is the number of positive studies, K is the number of total studies with the characteristic of interest, and p is the criterion for positivity by a 2-sided test (0.05 / 2 = 0.025).13 P values were calculated from a normal distribution. We defined a “positive” study as one reporting results with P values ≤.05 or lower; under the null hypothesis, 1 in 20 studies would be expected to meet this criterion. A significant Xscore suggests that there is sufficient evidence to conclude that the proportion of studies showing effective outcomes is greater than what would have been found by chance.13 Using this same formula, we calculated the number of studies that would need to be null to change the conclusions of the review in any given category.
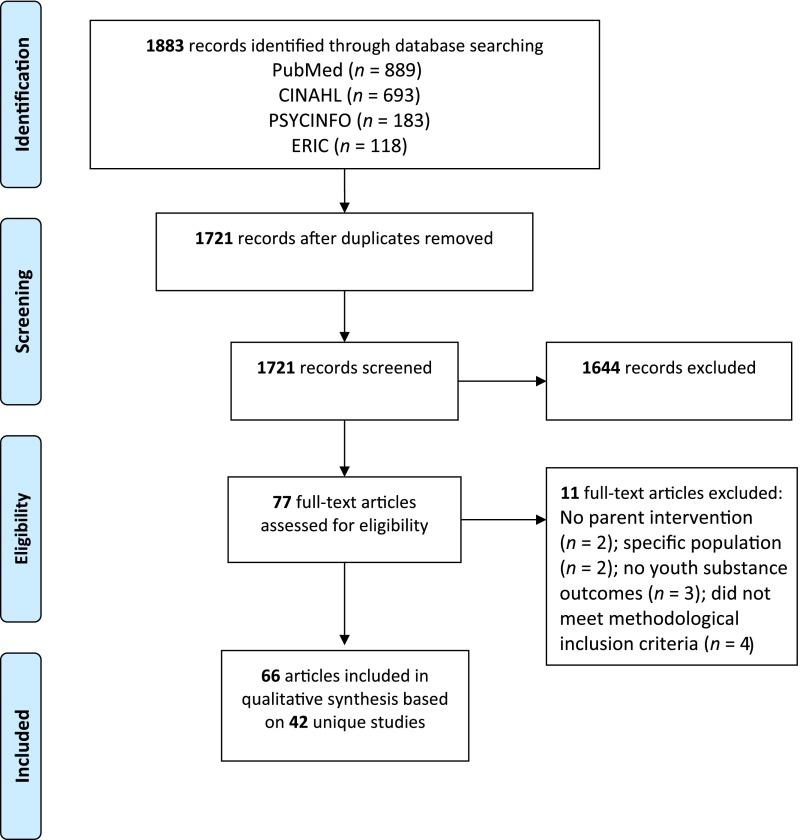
Results
Of the 1883 studies identified, 1721 unique articles were screened (Fig 1). A total of 1644 articles were excluded, largely because they did not evaluate family skills interventions, did not focus on substance use, or were not randomized controlled trials. The remaining 77 articles were screened in full, and 11 additional articles (representing 7 studies) were excluded because (1) parents were not a target of the intervention (n = 2), (2) the study targeted a population with a specific medical problem (n = 2), (3) youth substance use outcomes were not reported (n = 3), or (4) study did not meet methodological inclusion criteria (n = 4).
FIGURE 1.
Study flow diagram. From Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009;151(4):264–269.
The final 66 manuscripts included in the review represented 42 unique studies (Table 2); 6 of these studies included multiple parent-focused arms. Studies and associated citations will hereafter be referred to by the study number in Table 2 with letter subscripts indicating arms for multiarmed studies (eg, 9[a], 9[b]). Some manuscripts reported combined data from multiple studies and are therefore presented in Table 2 multiple times.
TABLE 2.
Summary of Studies Using Parent-Focused Interventions to Reduce Youth Substance Use
| Study ID | Authors | Youth Demographics | Intervention Description | Control Description | Outcomes Measured | Resultsa (P < .05) | Number Low Risk of Bias Criteriab |
|---|---|---|---|---|---|---|---|
| 1 | Bauman et al (2001)14 | N = 1326; Female NA; Race NA; 12–14 y | 4 booklets + 4 follow-up calls (parent) | No intervention | Smoking initiation; alcohol use and initiation | 12 mo: no difference smoking use or alcohol use | 1 |
| 2 | Brody et al (2006)15 | N = 332; 53.6% Female; African American; 11–13.5 y | 7 sessions (youth + parents) | 3 leaflets | Alcohol use and intention | 3 mo: reduced alcohol initiation/use; 29 mo: reduced alcohol initiation/use | 3 |
| 3 | Brody et al (2010)16 | N = 667; Female (NA); African American; 10.8 y | 5 sessions (youth + parents) | 3 leaflets | Alcohol use and initiation | 29 mo: reduced alcohol use; 65 mo: reduced alcohol use | 2 |
| 4 | Brody et al (2012)17 | N = 502; 51% Female; African American; Age 16 y (10th grade) | 5 sessions (youth + parents) | 5 sessions on nutrition (youth + parents) | Smoking, alcohol, substance and polysubstance use | 22 mo: reduced polysubstance use | 1 |
| 5 | Connell et al (2006,18 2007)19 | N = 998; 47.3% Female; Diverse population; 11–17 y | 6 sessions (youth) + 3 family checkups + elective family intervention (youth + parents) | No intervention | Smoking, alcohol, substance | 72 mo: reduced smoking use, alcohol use, and substance use | 4 |
| 6 | Curry et al (2003)20 | N = 4026; 52% Female; Primarily white; 10–12 y | 1 handbook + 2 counseling calls + 1 newsletter (parent) | Standard care | Smoking intention and use | 6 mo: no difference smoking intention, or use; 12 mo: no difference smoking intention, or use; 20 mo: no difference smoking intention, or use | 1 |
| 7 | DeGarmo et al (2009)21 | N = 361; 51% Female; European American; 5th–12th grade | 6 sessions (youth + parent) + recess games (youth + teacher) + 7 phone calls (parent) + newsletters (teacher + parent) | No intervention | Smoking, alcohol, and substance use and initiation | 60 mo: reduced smoking and alcohol initiation, no difference substance initiation | 4 |
| 8 | Dembo et al (2002)22 | N = 315; 44% Female; Diverse population; 14.5 y | 30 home visits (youth + parent) | Phone contacts with staff and referrals if necessary | Alcohol use | 36 mo: no difference alcohol use | 1 |
| 9(a) | Dishion & Andrews (1995)23 | N = 65; 47.5% Female; 90% Caucasian; 10–14 y | 12 sessions + 6 newsletter (parents) | No intervention | Smoking and substance use | 4 mo: no change smoking use; 16 mo: no change smoking use | 1 |
| 9(b) | Dishion & Andrews (1995)23 | N = 70; 47.5% Female; 90% Caucasian; 10–14 y | 12 sessions + 6 newsletter (youth + parents) | No intervention | Smoking and substance use | 4 mo: increased smoking use; 16 mo: increased smoking use | 1 |
| 10 | Fang L, et al (2010)24 | N = 108; 100% Female; Asian American; 10–14 y | 9 online sessions (youth + parent) | No treatment | Smoking and alcohol use; substance use and intention | 6.25 mo: no difference smoking use, reduced alcohol use, substance use, and polysubstance intention | 4 |
| 11 | Forman SG et al (1990)25 | N = 279; Female (NA); White; 14.72 y | 10 youth sessions + 1 booster + 5 parent sessions (youth + parent) | 10 sessions + 2 booster on peer support, increase substance knowledge (youth only) | Smoking, alcohol and substance use | 12 mo: no difference smoking use or alcohol use, reduced substance use | 2 |
| 12 | Gonzales et al (2012)26 | N = 516; 50.8% Female; Mexican American; 12.3 y | 9 sessions + 2 home visits (youth + parent) | 1 workshop on school resources/ school success (youth + parent) | Smoking, alcohol, substance and polysubstance use | 12 mo: reduced polysubstance use | 4 |
| 13 | Guilamo-Ramos et al (2010)27 | N = 1386; 50.4% Female; Diverse population; 12.1 y | 2 youth sessions + 2 parent sessions + 2 booster calls (youth + parent) | 2 youth sessions + parent class on high school selection | Smoking use | 15 mo: reduced smoking use | 4 |
| 14(a) | Haggerty et al (2007)28 | N = 213; 48.7% Female; 50.8% Caucasian, 49.2% African American; 13.7 y (8th grade) | Intervention 1: self-administered video + workbook program (parent) | No treatment | Smoking initiation; alcohol, substance and polysubstance use and initiation | 24 mo: no change in tobacco, alcohol, substance or poly substance initiation | 1 |
| 14(b) | Haggerty et al (2007)28 | N = 224; 48.7% Female; 50.8%; Caucasian, 49.2% African American; 13.7 y (8th grade) | Intervention 2: 7 Group video + workbook sessions (youth + parent) | No treatment | Smoking initiation; alcohol, substance and polysubstance use and initiation | 24 mo: no change in tobacco, alcohol, substance or polysubstance initiation | 1 |
| 15 | Komro et al (2006,29 2008)30 | N = 5812; 50% Female; Diverse population; 11.8 y (6th grade) | Youth: 25 sessions + 9.5 peer leaderships training + community service project. Youth + parent: 12 at home booklets+ 2 family fun events + 13 parent postcards (youth + parent) | Standard care | Alcohol intention; alcohol and polysubstance use | 36 mo: no difference alcohol intention, alcohol or polysubstance use | 2 |
| 16(a) | Koning (2009,31 2011,32 2013)33 | N = 1736; 49% Female; Dutch; 12.6 y | Intervention 1: 1 presentation + 1 parent consensus meeting for rule making + 1 information leaflet (parent) | No intervention | Alcohol use | 10 mo: no difference alcohol use; 22 mo: no difference alcohol use; 34 mo: no difference alcohol use; 50 mo: no difference alcohol use | 3 |
| 16(b) | Koning (2009,31 2011,32 2013)33 | N = 1747; 49% Female; Dutch; 12.6 y | Intervention 2: 1 presentation + 1 parent consensus meeting for rule making + 1 information leaflet (parent) + 4 lessons + 1 booster session (youth) | No intervention | Alcohol use | 10 mo: reduced alcohol use; 22 mo: reduced alcohol use; 34 mo: reduced alcohol use; 50 mo: reduced alcohol use | 3 |
| 17 | Loveland-Cherry et al (1999)34 | N = 892; 54% Female; European American; 9 y (4th grade) | 3 home sessions + phone calls + newsletter | No intervention | Alcohol use and initiation | 60 mo: reduced alcohol use | 1 |
| 18 | Martinez et al (2005)35 | N = 73; 44% Female; Latino; 12.74 y (middle school) | 12 sessions + 12 notebook exercises (parent) | No project-related intervention | Smoking, alcohol and substance intention | 5.61 mo: reduced smoking intention, marginally reduced substance intention, no difference alcohol intention | 1 |
| 19 | Milburn et al (2012)36 | N = 151; 66.2% Female; Diverse population; 14.8 y | 5 sessions (youth + parent) | Standard care | Alcohol, substance and polysubstance use | 12 mo: reduced alcohol use, increased marijuana use, reduced hard substance use | 3 |
| 20(a) | O’Donnell et al (2010)37 | N = 268; 100% Female; Diverse population; 11–13 y | Intervention 1: 4 audio CDs (youth + parent) | No materials | Alcohol use | 12 mo: reduced alcohol use | 1 |
| 20(b) | O’Donnell et al (2010)37 | N = 268; 100% Female; Diverse population; 11–13 y | Intervention 2: 4 booklets (youth + parent) | No materials | Alcohol use | 12 mo: no change in alcohol use | 1 |
| 21 | Pantin et al (2009)38 | N = 213; 36% Female; Hispanic; 13.8 y (8th grade) | 9 group sessions +10 family visits + 4 booster sessions (youth + parent) | 3 individual and family referrals to agencies that serve delinquent youth | Smoking, alcohol, substance and polysubstance use | 30 mo: reduced polysubstance use | 3 |
| 22 | Perry et al (1996,39 2002)40 Williams et al (1999)41 | N = 2351; 48.7% Female; 94% Caucasian; 6th grade at baseline | Project Northland: classroom lessons, school environment enhancements, parent newsletters and workbooks, community environment enhancements | Standard care | Smoking, alcohol, substance and polysubstance use; alcohol intention and initiation | <6 mo: no difference smoking, alcohol or substance use or alcohol intention; 12 mo: no difference smoking, alcohol or substance use or alcohol intention; 24 mo: no difference smoking or substance use, reduced alcohol intention, initiation and use, reduced poly-substance use; 4 y: reduced alcohol use and intention; 6 y: reduced alcohol use and intention | 0 |
| 23 | Prado et al (2007)42 | N = 266; 51.9% Female; Hispanic; 13.4 (8th grade) | 15 sessions + 8 family visits + 2 “circles” on parenting and preventing substance use and risky sexual behavior (youth + parent) | Control 1: 8 ESOL classes (parent) + 6 group sessions + 2 family visits on risky sexual behavior (youth + parent). Control 2: 8 ESOL classes (parent) + 7 group sessions of family exercise (youth + parent) | Smoking, alcohol, substance and polysubstance use and initiation | 36 mo: reduced smoking use and initiation, reduced substance use comparing intervention with control 2 but not when comparing intervention with control 1; no difference alcohol use or alcohol or substance initiation | 3 |
| 24 | Prado et al (2012)43 | N = 242; 35.6% Female; Hispanic or Latino; 14.7 y | 8 parent group sessions + 4 family visits (youth + parent) | Standard care: included referrals for families | Alcohol, substance and polysubstance use | 12 mo: reduced polysubstance and substance use, no difference alcohol use | 4 |
| 25 | Riesch et al (2012)44 | N = 167; 48.5% Female; Diverse population; 9–11 y, 10.8 y average age | 7 sessions (youth + parent) | No intervention | Smoking, alcohol and substance use | 6 mo: no change in smoking, alcohol or substance use | 3 |
| 26 | Schinke et al (2004,45 2010)46 Schwinn et al (2010)47 | N = 325; 51.4% Female; Diverse population; 10–12 y | 10 online sessions (youth) + 1 videotape + 2 newsletters + 1 booster workshops (parent) | No intervention | Smoking, alcohol and substance use and intention | <6 mo: reduced smoking, alcohol, and substance use; 12 mo: reduced smoking, alcohol, and substance use; 24 mo: reduced smoking, alcohol, and substance use; 36 mo: reduced smoking, alcohol, and substance use; 6 y: reduced smoking and alcohol use, no change in substance use; 7 y: reduced smoking, alcohol use; reduced alcohol intention; no difference substance use | 1 |
| 27 | Schinke et al (2009)48 | N = 202; 100% Female; Diverse population; 10–13 y | 14 online modules (youth + parent) | No treatment | Alcohol use intention | 2 mo: reduced alcohol use, no effect on alcohol intention | 2 |
| 28 | Schinke et al (2009)49 | N = 916; 100% Female; Diverse population; 11–13 y | 9 online sessions + 2 online booster sessions (youth + parent) | No intervention | Smoking, alcohol and substance use and intention; polysubstance intention | 24 mo: reduced alcohol and substance use and polysubstance intention; no change in smoking use | 1 |
| 29 | Schinke et al (2009)50 | N = 591; 100% Female; Diverse population; 12.7 y | 9 online sessions (youth + parent) | No intervention | Smoking, alcohol and substance use and intention | 12 mo: no change smoking use; reduced alcohol use, substance intention & use | 3 |
| 30 | Schinke, SP (2011)51 | N = 546; 100% Female; Diverse population; 10–13 y | 10 online sessions (youth + parent) | No intervention | Smoking, alcohol and substance use; polysubstance intention | ≤6 mo: reduced, alcohol use and polysubstance intention; no change in tobacco or substance use | 2 |
| 31 | Simons-Morton (2005)52 | N = 2651; Female (NA); Race NA; 6th grade | 18 classroom lessons + 1 parent video and booklet + enhanced school environment | School district comparison group | Smoking and alcohol use and intention | 36 mo: reduced smoking intention and use | 3 |
| 32 | Spirito (2011)53 | N = 125; 53% Female; Diverse population; 13–17 y | Individual motivational interview (youth) + 1 family sessions (youth + parent) | Individual motivational interview (youth) | Alcohol use | 3 mo: reduced alcohol use | 3 |
| 33 | Spoth et al (1999,54 2001,55 2004,56 2006,57 2006,58 2008)59, Park et al (2000)60, Mason et al (2003)61, Guyll et al (2004)62 | N = 429; 52% Female; 99% Caucasian; 6th grade | Preparing for Drug Free Years (PDFY): 4 sessions (parent) + 1 session (youth + parent) | 4 leaflets on adolescent development (parent) | Smoking, alcohol, substance and polysubstance use and intention | 12 mo: no change in smoking, alcohol, substance or polysubstance initiation or use; 24 mo: reduced smoking, alcohol, substance and polysubstance initiation/use; 48 mo: reduced, alcohol use, marginally reduced smoking, alcohol, substance initiation, no change in tobacco or substance use; 6 y: reduced smoking initiation & use, no change in alcohol or substance initiation or use; 10 y: marginally reduced misuse of prescription drugs | 3 |
| 34 | Spoth et al (1999,54 1999,63 2001,55 2004,56 2006,57 2006,58 2008,59 2009,64 2012)65, Guyll et al (2004)62 | N = 446; 52% Female; 99% Caucasian; 6th grade | Intervention: Iowa Strengthening Families Program (ISFP): 7 sessions (youth + parent) | 4 leaflets on adolescent development (parent) | Smoking, alcohol, substance and polysubstance use and intention | 12 mo: Reduced alcohol initiation no change in smoking, substance or polysubstance initiation or use or alcohol use; 24 mo: reduced smoking, alcohol, substance and polysubstance initiation and marginally reduced smoking, alcohol, substance and polysubstance use; 48 mo: reduced smoking, alcohol, substance and polysubstance initiation, reduced tobacco and alcohol use no change in substance use; 6 y: reduced smoking, alcohol, substance and polysubstance initiation, reduced alcohol, substance and polysubstance use, no change in tobacco use; 10 y: reduced misuse of prescription drugs | 3 |
| 35 | Spoth et al (2002,66 2005,67 2008)68, Spoth et al (2006,57,58 2008)59 describes 2 studies (including this 1) | N = 1664; 47% female; Caucasian; 7th grade | 7 sessions (youth + parent) | 4 leaflets on adolescent development (parent) | Smoking, alcohol, substance and polysubstance use; alcohol and substance initiation | 12 mo: no difference smoking initiation; reduced alcohol initiation, substance initiation, and poly substance initiation; 2.5 y: reduced poly substance initiation; no change substance use; 5.5 y: reduced smoking initiation/use, alcohol initiation, substance use, and poly substance initiation/use; no change alcohol use or substance initiation | 3 |
| 36 | Spoth et al (2007,69 2011,70 2013)71, Redmond et al (2009)72 | N = 11 931; 51% Female; 85% Caucasian; 6th grade at baseline | Year 1: Strengthening Families Program (10–14 y): 7 sessions (youth + parent). Year 2: in-class lessons on substance avoidance (youth) | No project support | Smoking, alcohol and substance use, initiation and intention; polysubstance initiation and intention | 12 mo: reduced substance initiation and use, reduced poly-substance initiation, marginally reduced tobacco use and initiation, no change in alcohol use or initiation; 2 y: no difference polysubstance intention; 4 y: reduced smoking, alcohol, substance and polysubstance initiation; reduced substance use; marginally reduced tobacco use; no change in alcohol use; 6 y: reduced smoking and substance use; no change in alcohol use | 1 |
| 37(a) | Stanton et al (2004)73 | N = 579; 58% Female; 100% African American; 13–16 y | Intervention 1: Intervention 1 + 1 video (youth + parent) | 8 youth sessions alone | Smoking, alcohol and substance use | 24 mo: reduced smoking use; no change alcohol use; marginal change in substance use | 2 |
| 37(b) | Stanton B, et al (2004)73 | N = 559; 58% Female; 100% African American; 13-16 | Intervention 2: Intervention 1 + 4 booster sessions (youth + parent) | 8 youth sessions alone | Smoking, alcohol and substance use | 24 mo: reduced smoking use; no change alcohol use; marginal change in substance use | 2 |
| 38 | Stormshak, et al (2011)74 Van Ryzin, et al (2012)75 | N = 593; 48.6% Female; Diverse population; 11.88 (6th grade) | 3 sessions (youth + parent) | School as usual | Smoking, alcohol and substance use | 24 mo: reduced smoking use, reduced alcohol use, reduced substance use; 36 mo: reduced alcohol use | 4 |
| 39 | Werch, CE et al (1998)76 | N = 211; 49.8% Female; 85% African American; 12.1 (6th grade) | 1 consultation (youth)+ 1 letter + 2-9 workbooks (youth + parent) | Booklet on alcohol (youth) | Alcohol use initiation and intention | 1 mo: no change alcohol use; 12 mo: no change alcohol use | 2 |
| 40 | Werch et al (2003)77 | N = 650; 46% female; Diverse population; 11.4 (6th grade) | 1 consultation + 1 follow-up consultation (youth) + 10 postcards +4 workbooks (youth + parent) | Booklet on alcohol (youth) | Alcohol use initiation and intention | 12 mo: reduced alcohol intention, no change alcohol use or initiation | 2 |
| 41 | West et al (2008)78 | N = 1981; Female (NA); Croatian; 6th–8th grade | Intervention encourages parent-child communication and peer communication (based on Project Northland) (youth + parent) | Control schools (curriculum is standard nationally in Croatia) | Alcohol use and intention | 2 y: reduced alcohol use; 3 y: no change alcohol use | 1 |
| 42(a) | Wolchik et al (2002)79 | N = 157; 49% Female; Primarily Caucasian; 10.8 at baseline | Intervention 1: 11 group + 2 individual sessions (parent) | Books on postdivorce adjustment (parent) | Alcohol, substance and polysubstance use | 6 y: no change in polysubstance use | 3 |
| 42(b) | Wolchik et al (2002)79 | N = 159; 51.8% female; Primarily Caucasian; 10.8 y at baseline | Intervention 2: 11 group + 2 individual sessions (parent) + 11 youth sessions | Books on postdivorce adjustment (parent) | Alcohol, substance and polysubstance use | 6 y: no change in polysubstance use | 3 |
NA, not available.
Reduction, no difference, or increase in substance use outcome.
Number of Cochran Criteria indicating low risk of bias from 0 to 5.
Studies varied in operationalization, measurement of substance use outcomes, which included tobacco, alcohol, and illicit substance intention to use, initiation, and current use, as well as polysubstance use. Twenty studies (48%) reported 3 substance use outcomes, 3 (7%) reported 2 substance use outcomes, 15 (36%) reported 1 substance use outcome, and 4 (9%) reported only poly-substance use. Outcomes are noted in Table 2 in the “Intervention Description” column. Control conditions were most often standard care, leaflets, or no intervention. All but 2 studies were conducted in the United States. Eleven studies (29%) included a majority of participants of white/Caucasian/European origin, 11 studies (29%) focused on other specific race/ethnic groups (5 on African American, 1 on Asian, and 5 on Latino youth), 16 (38%) included diverse youth populations, and 4 did not report race/ethnicity.
Risk of Bias
Of the 42 included studies, approximately half described how the randomization sequences were generated (n = 22, 52.4%), approximately a third described how these were concealed (n = 13, 31.0%), and few reported blinding outcome evaluators (n = 9, 21.4%). Many had high attrition rates and were selective in the outcomes that were reported in published manuscripts (n = 16, 38.1% for both domains). Summary counts of the risk of bias assessment is presented in Table 2 in the “Number of Low Risk of Bias Criteria” column and ranged from 0 (higher risk of bias, 1 study) to 4 (lower risk of bias, 7 studies) with an average number of low risk of bias criteria of 2.3 ± 1.1 of a maximum score of 5. Because all of the included studies had at least 1 feature that either was unclear or posed high risk of bias to the study findings (see Supplemental Table 3 for scoring on each criteria for each study), the overall risk of bias of this systematic review is high, suggesting results must be interpreted with caution.11
Aim 1: Evidence for Intervention Effectiveness
Four studies reported only polysubstance outcomes4,12,34,80 and so are presented in Table 2 but not in harvest plots. Of these, 3 were effective at outcome end points ranging from 12 to 30 months.4,12,80
For smoking, 26 unique studies assessed outcomes across the 4 time periods (Fig 2, column 1). The majority of studies reported smoking as opposed to intent or initiation; after 12 months, all but 1 study81 reported smoking as the outcome. The Xscores were significant at all time points, indicating that the proportion of studies showing effective outcomes was greater than what would be expected by chance. However, the number of studies that would need to be null to change this conclusion was much lower at the <12 months time point, suggesting a trend toward increasing effectiveness of interventions over time. The fact that 2 of the effective studies between 24.1 and 48 months26,28 and 1 of studies at >48 months27 reported no significant intervention effect at earlier time periods reinforces this trend. There was variation in the risk of bias in studies but no pattern indicting that studies with greater risk of bias were either more or less effective than those with less risk of bias.
Thirty-four studies reported alcohol outcomes (Fig 2, column 2), primarily use as opposed to intent or initiation. Effective studies at >24 months either did not report early outcomes or also indicated effectiveness at earlier time periods. The Xscores were significant at all time points. In this case, the number of studies needed to be null to change this conclusion was highest at the early time points. Variability in the studies’ risk of bias was similarly distributed among effective and ineffective studies.
Twenty-one studies examined other illicit substance outcomes (Fig 2, column 3), primarily use. The Xscores were again significant at all time points. Similar to alcohol, the number of studies needed to be null to change this conclusion was highest at the early time points. Again, there was variability in risk of bias across effective and ineffective interventions.
Across all 3 substances (Fig 2, all columns), few studies reported efficacy across multiple substance use outcomes. Three studies indicated significant effects for preventing or reducing use of 2 substances at <12 months,10,21,27 2 at 12 to 24 months,14,20 4 at 24 to 48 months,15,25,26,28 and 2 at >48 months.7,18 In terms of preventing all 3 substances, 1 study showed efficacy at <12 months,18 2 at 12 to 24 months,18,25 1 at 24 to 48 months,18 and none at >48 months.
Aim 2: Characteristics of Effective Interventions
For this aim, we assessed the participants, dosage, settings, and delivery methods of effective interventions. In terms of targeted participants, interventions largely included parents and youth; Xscores for each outcome were as follows: tobacco, 18.83, P < .001; alcohol, 20.97, P < .001; illicit drug use, 19.94, P < .001; and polydrug use, 17.94, P < .001. Seven interventions, 1, 6, 9(a), 14(a), 16(a), 18, and 42(a), focused exclusively on parents (see Table 2). Only 1 of these reported significant results.82
For the 26 studies reporting smoking outcomes, 69% reported information that allowed calculating the intervention dosage, 81% reported delivery setting, and 96% reported delivery method (Fig 3). In terms of dosage, (Fig 3, column 1), the majority of effective studies reported <12 hours of training, although Xscores were significant at all dosages. Most of the interventions reported delivery setting as schools or a combination of settings (Fig 3, column 2). Xscores were significant for all settings. Results regarding delivery method suggest that most of the effective interventions used sessions with a professional (Fig 3, column 3), as indicated by the high number of studies needed to be null to disprove this conclusion. The few studies using either printed material or computer-based approaches reported inconsistent findings.
For the 34 studies reporting alcohol outcomes, 65% reported the intervention dosage, 85% reported delivery setting, and 94% reported delivery method (Fig 4). In terms of dosage (Fig 4, column 1), the majority of effective studies reported <12 hours of training. Most were delivered at home, school, or in a combination of settings; those delivered at home had the highest Xscores (Fig 4, column 2). Most studies reporting alcohol outcomes used sessions; however, all that used a computer-based approach were effective (Fig 4, column 3).
FIGURE 4.
Alcohol use at the longest follow-up time according to dose of intervention, setting, primary delivery method, and program duration. White columns, ≤12 months of follow-up; dotted columns, 12.1–24 months of follow-up; horizontal stripe columns, 24.1–48 months of follow-up; black columns, >48 months of follow-up. Taller columns represent studies with lower risk of bias. Numbers indicate study ID. Xscore, number of studies needed to be null (NNN).
For the 21 studies reporting illicit substance use outcomes, 86% reported the intervention dosage, 81% reported delivery setting, and 95% reported delivery method (Fig 5). In terms of dosage (Fig 5, column 1), most effective interventions included ≤24 hours of training, although Xscores were significant for all dosages. There was a variety of effective delivery settings for illicit substances (Fig 5, column 2); most occurred in schools or in a combination of settings. The majority of these studies used sessions with a professional as their delivery method (Fig 5, column 3). Xscores were significant for all delivery methods except for computer based.
Discussion
Results of this systematic review indicate that parenting interventions could be effective at preventing and decreasing adolescent tobacco, alcohol, and illicit substance use but that the substance of focus and delivery characteristics are important. The finding that Xscores were highly significant for all outcomes at all time periods supports the conclusion that parent-focused interventions may generate a reduction on youth substance use over the short and long term.
Despite the existence of multiple effective programs, prevention researchers have noted that uptake of evidence-based programming has been limited.81 Common challenges for translation of evidence-based interventions to nonresearch settings include intervention intensity, a discrepancy between skills needed to implement the interventions and those available with current staff, and intervention relevance (to population or setting).2 Maximal reach of interventions in this review would be achieved if evidence existed for a broad menu of minimally burdensome delivery modalities that could be easily accessed by families across a variety of settings and impact multiple outcomes, yet our results suggest a relatively limited set of options.
On the encouraging side, our findings indicate that relatively low-intensity interventions with a dosage of a manageable ≥12 parent contact hours achieve outcomes. Although the dosage is manageable, the delivery modality may be problematic. The finding that group sessions were the most common means for delivering these interventions to parents and youth may pose barriers for some community settings. When implemented well, in-person group sessions may be powerful because of social support and shared learning among the participants; however, high-quality sessions require dedicated staff with content expertise, strong facilitation skills, and high-intensity training on intervention implementation. The costs and staff requirements may be beyond the means of community organizations, particularly those in resource-limited settings where highest at-risk youth are often served and reside. In this review, alcohol use was unique among the substances in that multiple effective studies used computer-based delivery modalities. The success of these interventions suggests that this may be an effective and presumably less costly approach to reaching a larger group of parents of youth. An added benefit of computer-based delivery is that content may be tailored to a particular family’s needs or cultural preferences, increasing the likelihood of relevance and effectiveness.83 In sum, although group sessions represent the most common and evidence-based delivery modality for tobacco and illicit substance use prevention in particular, there is need for additional studies using alternative approaches, including social/online media, to develop a broader set of options for translation of effective programs.
Overall, many studies were delivered in a combination of settings, largely schools and home. Few studies occurred in nonschool community agencies, such as health clinics. There is evidence that parenting interventions can be successfully implemented in health care settings, yet few studies have made use of clinics as locations for implementation of family-based substance use prevention.84,85 As schools become overburdened with initiatives focusing on academic achievement, it is important to consider clinics and community agencies as alternative settings to promote, sustain, and fund parent training programming. This is particularly true with the increased focus on “moving prevention to the mainstream of health,” clinical-community and public health partnerships promoted through the Affordable Care Act,82 and integrated care within family- and patient-centered health care homes.8 This approach has shown positive results with newborns86; more research is needed to understand which delivery modalities are most appropriate for the clinic environment and how policies and clinical procedures can best sustain these effective programs with adolescents.
Finally, given limited resources available for prevention programming and competing demands within delivery agencies, parent-focused interventions would ideally effectively target multiple substance use outcomes; however, few studies were effective at reducing adolescent use of multiple substances over the long term. Future research should investigate common core principles, content, and delivery modalities that contribute to study outcomes for a given substance use to enhance programming in a manner that will increase the likelihood of interventions being efficacious across substances.
This study has notable strengths, including use of broad inclusion criteria to identify all relevant intervention studies, but given that the majority of studies had risk of bias based on available data, the overall conclusions must be interpreted with caution.11 Conclusions were limited by the degree to which authors adhered to the CONSORT (Consolidated Standards of Reporting Trials) guidelines for behavioral interventions when reporting study design and findings, particularly in the areas of randomization sequence generation and blinding of data collection processes.87 Better reporting of risk of bias outcomes within articles would potentially have increased the strength of our recommendations but not the results of our review. In addition, because of the heterogeneity of intervention components, contexts, samples, methods, outcomes, and measures, we did not perform a meta-analysis and instead used harvest plots to summarize the study findings and explore the effects of intervention delivery methods on tobacco, alcohol, and substance use outcomes. Although this approach does not provide effect estimate summaries as in meta-analyses, it is an alternative that visually represents different aspects of intervention complexity.80 In addition, using the binomial test of proportions to complement the harvest plots allowed us to estimate probabilities of observing the presented patterns of results, which produced quantitative evidence supporting the qualitative summary. The high number of studies needed to be null to change study conclusions support the findings of our review.
With the increased move to translate effective interventions into broad use and the call for collaboration between clinic and public health initiatives to promote disease-preventing programming, there is need to identify effective interventions that prevent adolescent substance use across multiple delivery modalities and settings, including clinics. Parent training interventions are an effective means to promote public health goals for adolescents, and an opportunity remains to extrapolate what works to varied community settings in a manner that prevents adolescent use of multiple substances.
Acknowledgments
The authors acknowledge the substantial contribution of Nicole Hassig in formatting the harvest plots.
Footnotes
Dr Allen conceptualized the study, led study design, contributed to data extraction, and wrote the initial draft of the manuscript; Dr Garcia-Huidobro contributed to study design, led data extraction, and reviewed and revised the manuscript; Dr Porta contributed to study design and reviewed and revised early drafts of the manuscript; Ms Curran and Ms Patel contributed to data extraction and study design and reviewed and revised early drafts of the manuscript; Mr Miller contributed to data extraction and reviewed and revised drafts of the manuscript; Dr Borowsky contributed to conceptualization of the study and reviewed and revised drafts of the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at the PROSPERO systematic review registry (identifier CRD42014013069).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Garcia-Huidobro was supported by National Research Service Award in Primary Medical Care, grant. T32HP22239 (principal investigator: Dr I Borowsky), Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the US government. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975–2014: Overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2015 [Google Scholar]
- 2.National Research Council and Institute of Medicine Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: The National Academies Press; 2009 [PubMed] [Google Scholar]
- 3.Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. Am Psychol. 2003;58(6–7):457–465 [DOI] [PubMed] [Google Scholar]
- 4.Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. J Abnorm Child Psychol. 2008;36(4):567–589 [DOI] [PubMed] [Google Scholar]
- 5.Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol or drugs misuse in children <18: a systematic review. Health Educ Res. 2007;22(2):177–191 [DOI] [PubMed] [Google Scholar]
- 6.Thomas RE, Baker PRA, Thomas BC, Lorenzetti DL Family-based programmes for preventing smoking by children and adolescents. Cochrane Database Syst Rev. 2015;(2):CD004493 [DOI] [PMC free article] [PubMed]
- 7.Metzler CW, Sanders MR, Rusby JC, Crowley RN. Using consumer preference information to increase the reach and impact of media-based parenting interventions in a public health approach to parenting support. Behav Ther. 2012;43(2):257–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bultas MW, McMillin SE, Broom MA, Zand DH. Brief, rapid response, parenting interventions within primary care settings. J Behav Health Serv Res. 2015;(Aug):20. [DOI] [PubMed] [Google Scholar]
- 9.Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988-2007. Prev Med. 2008;47(1):3–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogilvie D, Fayter D, Petticrew M, et al. The harvest plot: a method for synthesising evidence about the differential effects of interventions. BMC Med Res Methodol. 2008;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JP, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, United Kingdom: Wiley-Blackwell; 2008 [Google Scholar]
- 13.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Philadelphia, PA: Lippincott Williams & Wilkins; 2008 [Google Scholar]
- 14.Bauman KE, Foshee VA, Ennett ST, et al. The influence of a family program on adolescent tobacco and alcohol use. Am J Public Health. 2001;91(4):604–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brody GH, Murry VM, Kogan SM, et al. The Strong African American Families Program: a cluster-randomized prevention trial of long-term effects and a mediational model. J Consult Clin Psychol. 2006;74(2):356–366 [DOI] [PubMed] [Google Scholar]
- 16.Brody GH, Chen YF, Kogan SM, Murry VM, Brown AC. Long-term effects of the strong African American families program on youths’ alcohol use. J Consult Clin Psychol. 2010;78(2):281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brody GH, Chen YF, Kogan SM, et al. Family-centered program deters substance use, conduct problems, and depressive symptoms in black adolescents. Pediatrics. 2012;129(1):108–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Connell AM, Dishion TJ. Deater-Deckard K. Variable- and person-centered approaches to the analysis of early adolescent substance use: linking peer, family, and intervention effects with developmental trajectories. Merrill-Palmer Q. 2006;52(3):421–448 [Google Scholar]
- 19.Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to family intervention: linking engagement in family-centered intervention to reductions in adolescent problem behavior. J Consult Clin Psychol. 2007;75(4):568–579 [DOI] [PubMed] [Google Scholar]
- 20.Curry SJ, Hollis J, Bush T, et al. A randomized trial of a family-based smoking prevention intervention in managed care. Prev Med. 2003;37(6 Pt 1):617–626 [DOI] [PubMed] [Google Scholar]
- 21.DeGarmo DS, Eddy JM, Reid JB, Fetrow RA Evaluating mediators of the impact of the Linking the Interests of Families and Teachers (LIFT) multimodal preventive intervention on substance use initiation and growth across adolescence. Prev Sci 2009;10(3):208–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dembo R, Wothke W, Livingston S, Schmeidler J. The impact of a family empowerment intervention on juvenile offender heavy drinking: a latent growth model analysis. Subst Use Misuse. 2002;37(11):1359–1390 [DOI] [PubMed] [Google Scholar]
- 23.Dishion TJAD, Andrews DW. Preventing escalation in problem behaviors with high-risk young adolescents: immediate and 1-year outcomes. J Consult Clin Psychol. 1995;63(4):538–548 [DOI] [PubMed] [Google Scholar]
- 24.Fang L, Schinke SP, Cole KC Preventing substance use among early Asian-American adolescent girls: initial evaluation of a Web-based, mother-daughter program. J Adolesc Health 2010;47(5):529–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forman SFJLMB. Effects of coping skills training on adolescents at risk for substance use. Psychol Addict Behav. 1990;4(2):67–76 [Google Scholar]
- 26.Gonzales NA, Dumka LE, Millsap RE, et al. Randomized trial of a broad preventive intervention for Mexican American adolescents. J Consult Clin Psychol. 2012;80(1):1–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guilamo-Ramos V, Jaccard J, Dittus P, Gonzalez B, Bouris A, Banspach S; GuilamoRamos V . The Linking Lives health education program: a randomized clinical trial of a parent-based tobacco use prevention program for African American and Latino youths. Am J Public Health. 2010;100(9):1641–1647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haggerty KP, Skinner ML, MacKenzie EP, Catalano RF. A randomized trial of Parents Who Care: effects on key outcomes at 24-month follow-up. Prev Sci. 2007;8(4):249–260 [DOI] [PubMed] [Google Scholar]
- 29.Komro KA, Perry CL, Veblen-Mortenson S, et al. Cross-cultural adaptation and evaluation of a home-based program for alcohol use prevention among urban youth: the “Slick Tracy Home Team Program.” J Prim Prev. 2006;27(2):135–154 [DOI] [PubMed] [Google Scholar]
- 30.Komro KA, Perry CL, Veblen-Mortenson S, et al. Outcomes from a randomized controlled trial of a multi-component alcohol use preventive intervention for urban youth: project northland Chicago. Addiction. 2008;103(4):606–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koning IM, Vollebergh WA, Smit F, et al. Preventing heavy alcohol use in adolescents (PAS): cluster randomized trial of a parent and student intervention offered separately and simultaneously. Addiction. 2009;104(10):1669–1678 [DOI] [PubMed] [Google Scholar]
- 32.Koning IM, van den Eijnden RJ, Verdurmen JE, Engels RC, Vollebergh WA. Long-term effects of a parent and student intervention on alcohol use in adolescents: a cluster randomized controlled trial. Am J Prev Med. 2011;40(5):541–547 [DOI] [PubMed] [Google Scholar]
- 33.Koning IM, van den Eijnden RJ, Verdurmen JE, Engels RC, Vollebergh WA. A cluster randomized trial on the effects of a parent and student intervention on alcohol use in adolescents four years after baseline; no evidence of catching-up behavior. Addict Behav. 2013;38(4):2032–2039 [DOI] [PubMed] [Google Scholar]
- 34.Loveland-Cherry CJ, Ross LT, Kaufman SR Effects of a home-based family intervention on adolescent alcohol use and misuse. J Stud Alcohol Suppl 1999;13:94–102 [DOI] [PubMed] [Google Scholar]
- 35.Martinez CR Jr, Eddy JM. Effects of culturally adapted parent management training on Latino youth behavioral health outcomes. J Consult Clin Psychol. 2005;73(5):841–851 [DOI] [PubMed] [Google Scholar]
- 36.Milburn NG, Iribarren FJ, Rice E, et al. A family intervention to reduce sexual risk behavior, substance use, and delinquency among newly homeless youth. J Adolesc Health 2012;50(4):358–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Donnell L, Myint-U A, Duran R, Stueve A. Especially for daughters: parent education to address alcohol and sex-related risk taking among urban young adolescent girls. Health Promot Pract. 2010;11(suppl 3):70S–78S [DOI] [PubMed] [Google Scholar]
- 38.Pantin H, Prado G, Lopez B, et al. A randomized controlled trial of Familias Unidas for Hispanic adolescents with behavior problems. Psychosom Med. 2009;71(9):987–995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perry CLWC, Williams CL, Veblen-Mortenson S, et al. Project Northland: outcomes of a communitywide alcohol use prevention program during early adolescence. Am J Public Health. 1996;86(7):956–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perry CLWC, Williams CL, Komro KA, et al. Project Northland: long-term outcomes of community action to reduce adolescent alcohol use. Health Educ Res. 2002;17(1):117–132 [DOI] [PubMed] [Google Scholar]
- 41.Williams CL, Perry CL, Farbakhsh K, Veblen-Mortenson S Project Northland: comprehensive alcohol use prevention for young adolescents, their parents, schools, peers and communities. J Stud Alcohol Suppl 1999;13:112–124 [DOI] [PubMed]
- 42.Prado G, Pantin H, Briones E, et al. A randomized controlled trial of a parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. J Consult Clin Psychol. 2007;75(6):914–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prado G, Cordova D, Huang S, et al. The efficacy of Familias Unidas on drug and alcohol outcomes for Hispanic delinquent youth: main effects and interaction effects by parental stress and social support. Drug Alcohol Depend 2012;125(suppl 1):S18–25 [DOI] [PMC free article] [PubMed]
- 44.Riesch SK, Brown RL, Anderson LS, Wang K, Canty-Mitchell J, Johnson DL. Strengthening families program (10-14): effects on the family environment. West J Nurs Res. 2012;34(3):340–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schinke SP, Schwinn TM, Di Noia J, Cole KC. Reducing the risks of alcohol use among urban youth: three-year effects of a computer-based intervention with and without parent involvement. J Stud Alcohol . 2004;65(4):443–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schinke SP, Schwinn TM, Fang L Longitudinal outcomes of an alcohol abuse prevention program for urban adolescents. J Adolesc Health 2010;46(5):451–457 [DOI] [PMC free article] [PubMed]
- 47.Schwinn TM, Schinke SP. Preventing alcohol use among late adolescent urban youth: 6-year results from a computer-based intervention. J Stud Alcohol. 2010;71(4):535–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schinke SP, Cole KCA, Fang L. Gender-specific intervention to reduce underage drinking among early adolescent girls: A test of a computer-mediated, mother-daughter program. J Stud Alcohol. 2009;70(1):70–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schinke SP, Fang L, Cole KC. Computer-delivered, parent-involvement intervention to prevent substance use among adolescent girls. Prev Med. 2009;49(5):429–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schinke SP, Fang L, Cole KC. Preventing substance use among adolescent girls: 1-year outcomes of a computerized, mother-daughter program. Addict Behav. 2009;34(12):1060–1064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schinke SP, Fang L, Cole KC, Cohen-Cutler S. Preventing substance use among Black and Hispanic adolescent girls: results from a computer-delivered, mother-daughter intervention approach. Subst Use Misuse. 2011;46(1):35–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simons-Morton B, Haynie D, Saylor K, Crump AD, Chen R The effects of the going places program on early adolescent substance use and antisocial behavior. Prev Sci 2005;6(3):187–197 [DOI] [PubMed] [Google Scholar]
- 53.Spirito A, Sindelar-Manning H, Colby SM, et al. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: results of a randomized clinical trial. Arch Pediatr Adolesc Med. 2011;165(3):269–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spoth R, Lopez Reyes M, Redmond C, Shin C. Assessing a public health approach to delay onset and progression of adolescent substance use: latent transition and log-linear analyses of longitudinal family preventive intervention outcomes. J Consult Clin Psychol. 1999;67(5):619–630 [DOI] [PubMed] [Google Scholar]
- 55.Spoth RL, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: adolescent substance use outcomes 4 years following baseline. J Consult Clin Psychol. 2001;69(4):627–642 [DOI] [PubMed] [Google Scholar]
- 56.Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: school-level growth curve analyses 6 years following baseline. J Consult Clin Psychol. 2004;72(3):535–542 [DOI] [PubMed] [Google Scholar]
- 57.Spoth R, Shin C, Guyll M, Redmond C, Azevedo K. Universality of effects: an examination of the comparability of long-term family intervention effects on substance use across risk-related subgroups. Prev Sci 2006;7(2):209–224 [DOI] [PubMed] [Google Scholar]
- 58.Spoth RL, Clair S, Shin C, Redmond C. Long-term effects of universal preventive interventions on methamphetamine use among adolescents. Arch Pediatr Adolesc Med. 2006;160(9):876–882 [DOI] [PubMed] [Google Scholar]
- 59.Spoth R, Trudeau L, Shin C, Redmond C. Long-term effects of universal preventive interventions on prescription drug misuse. Addiction. 2008;103(7):1160–1168 [DOI] [PubMed] [Google Scholar]
- 60.Park J, Kosterman R, Hawkins JD, et al. Effects of the “Preparing for the Drug Free Years” curriculum on growth in alcohol use and risk for alcohol use in early adolescence. Prev Sci. 2000;1(3):125–138 [DOI] [PubMed] [Google Scholar]
- 61.Mason WA, Kosterman R, Hawkins JD, Haggerty KP, Spoth RL Reducing adolescents’ growth in substance use and delinquency: randomized trial effects of a parent-training prevention intervention. Prev Sci 2003;4(3):203–212 [DOI] [PubMed] [Google Scholar]
- 62.Guyll M, Spoth RL, Chao W, Wickrama KA, Russell D. Family-focused preventive interventions: evaluating parental risk moderation of substance use trajectories. J Fam Psychol. 2004;18(2):293–301 [DOI] [PubMed] [Google Scholar]
- 63.Spoth R, Redmond C, Lepper H Alcohol initiation outcomes of universal family-focused preventive interventions: one- and two-year follow-ups of a controlled study. J Stud Alcohol Suppl 1999;13:103–111 [DOI] [PubMed] [Google Scholar]
- 64.Spoth R, Guyll M, Shin C. Universal intervention as a protective shield against exposure to substance use: long-term outcomes and public health significance. Am J Public Health. 2009;99(11):2026–2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Spoth RL, Trudeau LS, Guyll M, Shin C Benefits of universal intervention effects on a youth protective shield 10 years after baseline. J Adolesc Health 2012;50(4):414–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Spoth RL, Redmond C, Trudeau L, Shin C Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychol Addict Behav 2002;16(2):129–134 [PubMed] [Google Scholar]
- 67.Spoth R, Randall GK, Shin C, Redmond C. Randomized study of combined universal family and school preventive interventions: patterns of long-term effects on initiation, regular use, and weekly drunkenness. Psychol Addict Behav. 2005;19(4):372–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Spoth RL, Randall GK, Trudeau L, Shin C, Redmond C. Substance use outcomes 51/2 years past baseline for partnership-based, family-school preventive interventions. Drug Alcohol Depend. 2008;96(1-2):57–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance-use outcomes at 18 months past baseline: the PROSPER Community-University Partnership Trial. Am J Prev Med. 2007;32(5):395–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community-university partnerships: randomized controlled trial outcomes 4½ years past baseline. Am J Prev Med. 2011;40(4):440–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Schainker L. PROSPER community-university partnership delivery system effects on substance misuse through 6 1/2 years past baseline from a cluster randomized controlled intervention trial. Prev Med. 2013;56(3–4):190–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Redmond C, Spoth RL, Shin C, Schainker LM, Greenberg MT, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community-university partnership. J Prim Prev. 2009;30(5):513–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stanton B, Cole M, Galbraith J, et al. Randomized trial of a parent intervention: parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Arch Pediatr Adolesc Med. 2004;158(10):947–955 [DOI] [PubMed] [Google Scholar]
- 74.Stormshak EA, Connell AM, Véronneau MH, et al. An ecological approach to promoting early adolescent mental health and social adaptation: family-centered intervention in public middle schools. Child Dev. 2011;82(1):209–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Van Ryzin MJ, Stormshak EA, Dishion TJ Engaging parents in the family check-up in middle school: longitudinal effects on family conflict and problem behavior through the high school transition. J Adolesc 2012;50(6):627–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Werch CE, Pappas DM, Carlson JM, DiClemente CC. Short- and long-term effects of a pilot prevention program to reduce alcohol consumption. Subst Use Misuse. 1998;33(11):2303–2321 [DOI] [PubMed] [Google Scholar]
- 77.Werch CE, Owen DM, Carlson JM, DiClemente CC, Edgemon P, Moore M. One-year follow-up results of the STARS for Families alcohol prevention program. Health Educ Res. 2003;18(1):74–87 [DOI] [PubMed] [Google Scholar]
- 78.West B, Abatemarco D, Ohman-Strickland PA, Zec V, Russo A, Milic R. Project Northland in Croatia: results and lessons learned. J Drug Educ. 2008;38(1):55–70 [DOI] [PubMed] [Google Scholar]
- 79.Wolchik SA, Sandler IN, Millsap RE, et al. Six-year follow-up of preventive interventions for children of divorce: a randomized controlled trial. JAMA. 2002;288(15):1874–1881 [DOI] [PubMed] [Google Scholar]
- 80.Petticrew M, Rehfuess E, Noyes J, et al. Synthesizing evidence on complex interventions: how meta-analytical, qualitative, and mixed-method approaches can contribute. J Clin Epidemiol. 2013;66(11):1230–1243 [DOI] [PubMed] [Google Scholar]
- 81.Green LW. Translation 2 research—the roadmap less traveled. Am J Prev Med. 2007;33(2):137–138 [Google Scholar]
- 82.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363(14):1296–1299 [DOI] [PubMed] [Google Scholar]
- 83.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3-4):214–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Borowsky IW, Mozayeny S, Stuenkel K, Ireland M. Effects of a primary care-based intervention on violent behavior and injury in children. Pediatrics. 2004;114(4). Available at: www.pediatrics.org/cgi/content/full/114/4/e392 [DOI] [PubMed] [Google Scholar]
- 85.Perrin EC, Sheldrick RC, McMenamy JM, Henson BS, Carter AS. Improving parenting skills for families of young children in pediatric settings: a randomized clinical trial. JAMA Pediatr. 2014;168(1):16–24 [DOI] [PubMed] [Google Scholar]
- 86.Weisleder A, Cates CB, Dreyer BP, et al. Promotion of Positive Parenting and Prevention of Socioemotional Disparities. Pediatrics. 2016;137(2):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C; CONSORT Group . Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148(4):295–309 [DOI] [PubMed] [Google Scholar]