Abstract
Context:
We noted a bimodal relationship between mortality and shock index (SI), the ratio of heart rate to systolic blood pressure.
Aims:
To determine if extremes of SI can predict mortality in trauma patients.
Settings and Designs:
Retrospective evaluation of adult trauma patients at a tertiary care center from 2000 to 2012 in the United States.
Materials and Methods:
We examined the SI in trauma patients and determined the adjusted mortality for patients with and without head injuries.
Statistical Analysis Used:
Descriptive statistics and multivariable logistic regression. Results: SI values demonstrated a U-shaped relationship with mortality. Compared with patients with a SI between 0.5 and 0.7, patients with a SI of <0.3 had an odds ratio for death of 2.2 (95% confidence interval [CI] 21.2–4.1) after adjustment for age, Glasgow Coma score, and injury severity score while patients with SI >1.3 had an odds ratio of death of 3.1. (95% CI 1.6–5.9). Elevated SI is associated with increased mortality in patients with isolated torso injuries, and is associated with death at both low and high values in patients with head injury.
Conclusion:
Our data indicate a bimodal relationship between SI and mortality in head injured patients that persists after correction for various co-factors. The distribution of mortality is different between head injured patients and patients without head injuries. Elevated SI predicts death in all trauma patients, but low SI values only predict death in head injured patients.
Keywords: Mortality in trauma, shock, shock index
INTRODUCTION
In an attempt to identify otherwise well-appearing individuals who have occult shock, the shock index (SI), the ratio of heart rate to systolic blood pressure (SBP), has been proposed as a quick and reliable indicator of perfusion in trauma patients.[1] It has been suggested that SI ≥ 0.9 upon admission can identify most critically ill patients despite having “stable” or “normal” vital signs.[2]
Recent data in trauma patients suggest that hypotension as well as hypertension can predict mortality in trauma patients.[3,4,5] Zafar et al.[6] have demonstrated that both hypertensive and hypotensive traumatic brain injured patients have increased mortality. The absence of tachycardia in the presence of other markers of hypoperfusion (e.g. lactate, base deficit) is associated with poor outcome in trauma.[7] We hypothesize that both low and high SI will predict death in a large cohort of trauma patients.
MATERIALS AND METHODS
A retrospective review of all trauma patients at Beth Israel Deaconess Medical Center, an urban ACS-verified level one trauma center, was performed from January 1, 2000 to September 1, 2012. Institutional Review Board approval was obtained prior to initiating this study and a waiver of informed consent was granted.
All patients ≥18-year-old admitted to the trauma service were included. Only first admissions were included to preserve independence of observations. We excluded patients without vital signs on admission and those whose values were missing or invalid. Demographic data (age, sex, mechanism of injury), vital signs on admission (heart rate, SBP) as well as trauma scores (Glasgow Coma score [GCS], injury severity score [ISS], and abbreviated injury score) were determined. Hospital discharge status (i.e., alive or dead) was determined. SI was calculated as follows:
SI =First recorded heart rate/first recorded SBP.
Our primary outcome was in-hospital mortality and our principal independent variable of interest was SI. We report continuous data as means with standard deviations and categorical data as proportions. Ordinal data were reported as medians with interquartile ranges (IQRs).
For unadjusted analyses, we performed tests of difference using Fisher’s exact test for categorical data. For continuous data, we used the t-test or Wilcoxon rank-sum, depending on the distribution of the variable. To estimate the independent relationship of SI to mortality, we performed multivariable logistic regression. Statistical significance was defined as a P < 0.05.
RESULTS
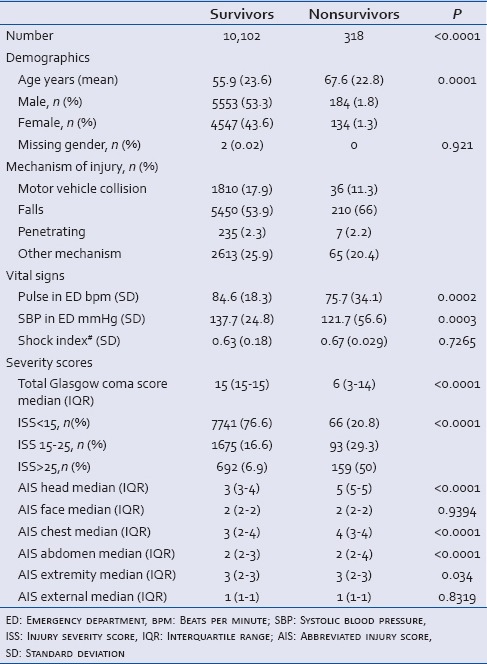
Our cohort included 10,420 patients in our trauma registry who had a recorded initial SBP and heart rate (HR), of whom 318 (3.05%) died during the hospital admission [Table 1]. The mean age of survivors was 55.9 years (standard deviation [SD] 23.6) versus 67.6 years (SD 22.83) for nonsurvivors. The median GCS of 15 (IQR 15–15) in survivors was higher than in nonsurvivors (6, IQR 3–14). The median ISS was 9 (IQR 4–13) in survivors and was significantly higher than in nonsurvivors in every category except for facial and external injuries. In terms of vital signs, the average HR was higher and the mean SBP was lower in nonsurvivors. There was no difference in SI between survivors and nonsurvivors.
Table 1.
Characteristics of cohort
In univariate analysis treating SI as a continuous variable, SI was not associated with mortality (P = 0.6, Wilcoxon rank-sum). Increasing age and increasing ISS were both associated with increasing mortality [Table 2]. The highest SI values were associated with increased mortality in patients with an isolated head injury, and were associated with death at both low and high values in patients with torso injuries and no head injury [Table 2].
Table 2.
Analysis of cohort
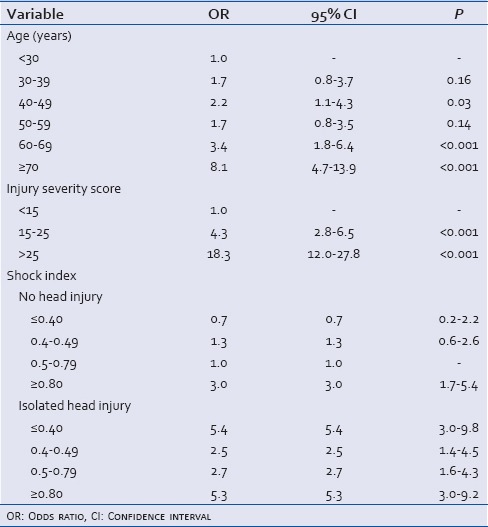
SI values for the entire cohort demonstrated a U-shaped relationship with mortality [Figure 1]. This relationship was maintained in multivariable analysis. Compared with patients with a SI between 0.5 and 0.7, patients with a SI of <0.3 had an odds ratio for death of 2.2 (95% CI 21.2–4.1) after adjustment for age, Glasgow Coma Score, and ISS while patients with SI > 1.3 had an OR of death of 31. (95% confidence interval 1.6–5.9) [Table 3]. This model had good discrimination and calibration (c statistic = 0.87; Hosmer–Lemeshow Chi-square 8.1).
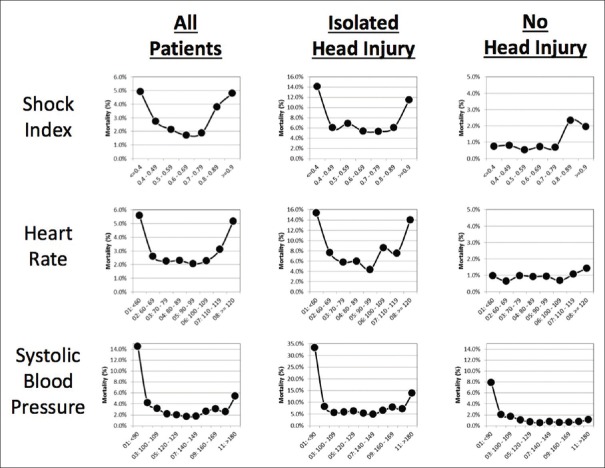
Figure 1.
Shock index values for head injured and nonhead injured patients are displayed individually
Table 3.
Multivariable analysis showing U-shaped relationship between shock index and mortality
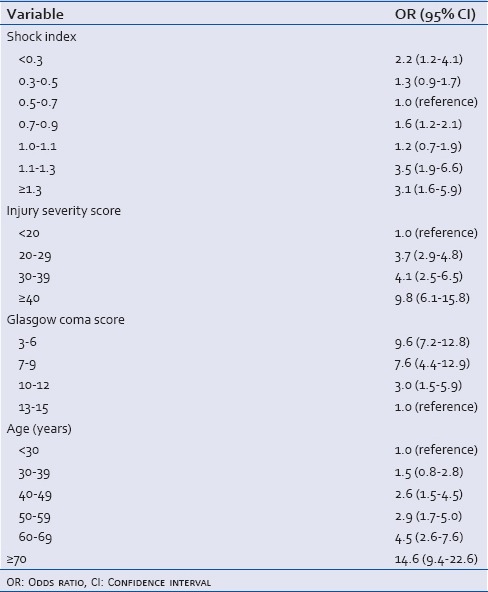
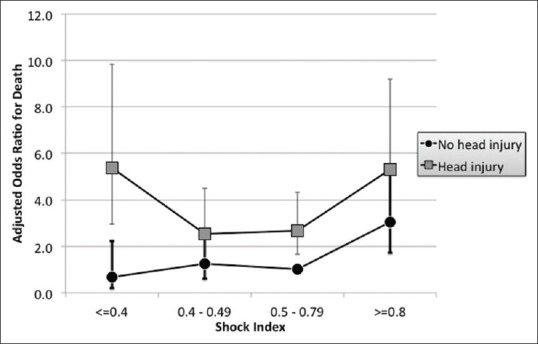
Figure 2 demonstrates that the U-shaped association between mortality and SI only applies to patients with an isolated head injury. Patients without head injury have an increased mortality at SI > 0.8, but there is no increased mortality at low SI levels. Indeed, hypotension is the only clearly associated variable with mortality in patients without head injury and both hypotension and hypertension are associated with mortality in isolated head injuries. Likewise, tachycardia and bradycardia are associated with increased mortality in isolated head injured patients.
Figure 2.
Mortality curves for patients overall, with head injuries and without head injuries with contribution of shock index and its components (heart rate and systolic blood pressure) presented separately
DISCUSSION
Our data indicate a bimodal relationship between SI and mortality in head injured patients that persists after correction for various co-factors. The distribution of mortality is different between head injured patients and patients without head injuries. Elevated SI predicts death in all trauma patients, but low SI values only predict death in head injured patients. The difference is primarily related to differences in blood pressure. Namely, hypotension is a severe problem in all trauma patients, but hypertension is also associated with increased mortality in head injured patients.
Recent associations have been shown between hypertension and mortality after traumatic brain injury.[6] The authors postulate that intracranial hyperperfusion and resultant cerebral edema result from this systemic hypertension. In this study, initial hypotension was associated with early death, while hypertension was associated with late death, for unclear reasons.
Determination of shock in trauma patients is not always clear. The term “occult hypoperfusion” has been used to describe patients in whom vital signs are normal, but serum lactate is high, indicating tissue hypoperfusion, and can suggest either underresuscitation, ongoing hemorrhage, or both. Scoring systems are cumbersome to use early in the course of resuscitation, or cannot be calculated until the patient has been in the hospital for some time, limiting their use in the early recognition of shock in trauma patients. It is clear that hypotension can be a clinical marker of shock, and that normal SBP can belie underlying shock. What is less clear is why some trauma patients with systolic hypertension have occult hypoperfusion.
Early recognition of shock is critical to survival in trauma. Numerous scoring systems have been developed based on physiologic or mechanistic criteria that attempt to predict trauma patients that are at high risk of mortality.[8,9,10,11,12,13] Lactate is a known marker of tissue hypoperfusion, even in the absence of other clinical markers of shock.[5] Also, the clearance of lactate is an independent predictor of mortality in trauma.[5,14] It is known that elevated SI is correlated with mortality in trauma patients.[15,16] Specifically, SI ≥ 0.9 has been used as a cut-off to predict increased mortality.[2]
In traumatic brain injury, both low and high SI is correlated with mortality. Only high SI predicts death in patients without head injury. SI is a better predictor of shock than either blood pressure or heart rate alone in both head injured patients and patients without head injury.
CONCLUSION
A bimodal relationship between SI and mortality exists in trauma patients, but a difference exists in the head injured and the non-head injured patients. Elevated SI predicts death in all trauma patients, but low SI only predicts death in head injured patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rady MY, Edwards JD, Nightingale P. Early cardiorespiratory findings after severe blunt thoracic trauma and their relation to outcome. Br J Surg. 1992;79:65–8. doi: 10.1002/bjs.1800790123. [DOI] [PubMed] [Google Scholar]
- 2.Cerovic O, Golubovic V, Spec-Marn A, Kremzar B, Vidmar G. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med. 2003;29:1300–5. doi: 10.1007/s00134-003-1753-8. [DOI] [PubMed] [Google Scholar]
- 3.Ley EJ, Singer MB, Clond MA, Gangi A, Mirocha J, Bukur M, et al. Elevated admission systolic blood pressure after blunt trauma predicts delayed pneumonia and mortality. J Trauma. 2011;71:1689–93. doi: 10.1097/TA.0b013e31823cc5df. [DOI] [PubMed] [Google Scholar]
- 4.Clond MA, Mirocha J, Singer MB, Bukur M, Salim A, Marguiles DR, et al. Gender influences outcomes in trauma patients with elevated systolic blood pressure. Am J Surg. 2011;202:823–7. doi: 10.1016/j.amjsurg.2011.06.044. [DOI] [PubMed] [Google Scholar]
- 5.Odom SR, Howell MD, Silva GS, Nielsen VM, Gupta A, Shapiro NI, et al. Lactate clearance as a predictor of mortality in trauma patients. J Trauma Acute Care Surg. 2013;74:999–1004. doi: 10.1097/TA.0b013e3182858a3e. [DOI] [PubMed] [Google Scholar]
- 6.Zafar SN, Millham FH, Chang Y, Fikry K, Alam HB, King DR, et al. Presenting blood pressure in traumatic brain injury: A bimodal distribution of death. J Trauma. 2011;71:1179–84. doi: 10.1097/TA.0b013e3182140d38. [DOI] [PubMed] [Google Scholar]
- 7.Mizushima Y, Ueno M, Watanabe H, Ishikawa K, Matsuoka T. Discrepancy between heart rate and makers of hypoperfusion is a predictor of mortality in trauma patients. J Trauma. 2011;71:789–92. doi: 10.1097/TA.0b013e31822f7bbd. [DOI] [PubMed] [Google Scholar]
- 8.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 9.Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ. Trauma score. Crit Care Med. 1981;9:672–6. doi: 10.1097/00003246-198109000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Champion HR, Copes WS, Sacco WJ, Frey CF, Holcroft JW, Hoyt DB, et al. Improved predictions from a severity characterization of trauma (ASCOT) over trauma and injury severity score (TRISS): Results of an independent evaluation. J Trauma. 1996;40:42–8. doi: 10.1097/00005373-199601000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Gilpin DA, Nelson PG. Revised trauma score: A triage tool in the accident and emergency department. Injury. 1991;22:35–7. doi: 10.1016/0020-1383(91)90158-b. [DOI] [PubMed] [Google Scholar]
- 12.Boyd CR, Tolson MA. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. Am J Surg. 1987;153:448, 514. doi: 10.1016/0002-9610(87)90790-2. [DOI] [PubMed] [Google Scholar]
- 13.Gerdin M, Roy N, Khajanchi M, Kumar V, Dharap S, Felländer-Tsai L, et al. Correction: Predicting early mortality in adult trauma patients admitted to three public University Hospitals in Urban India: A Prospective Multicentre Cohort Study. PLoS One. 2015;10:e0144886. doi: 10.1371/journal.pone.0144886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heinonen E, Hardcastle TC, Barle H, Muckart DJ. Lactate clearance predicts outcome after major trauma. Afr J Emerg Med. 2014;4:61–5. [Google Scholar]
- 15.Paladino L, Subramanian RA, Nabors S, Sinert R. The utility of shock index in differentiating major from minor injury. Eur J Emerg Med. 2011;18:94–8. doi: 10.1097/MEJ.0b013e32833f212b. [DOI] [PubMed] [Google Scholar]
- 16.Aslar AK, Kuzu MA, Elhan AH, Tanik A, Hengirmen S. Admission lactate level and the APACHE II score are the most useful predictors of prognosis following torso trauma. Injury. 2004;35:746–52. doi: 10.1016/j.injury.2003.09.030. [DOI] [PubMed] [Google Scholar]