Abstract
Aims:
To study the impact of hypothermia upon admission to the Intensive Care Unit (ICU) on early and late mortality and to develop a prediction model for late mortality in severely injured trauma patients.
Materials and Methods:
A multicenter retrospective cohort study was performed in adult trauma patients admitted to the ICU of two Level-1 trauma centers between 2007 and 2012. Hypothermia was defined as a core body temperature of ≤35° Celsius. Logistic regression analyses were performed to quantify the effect of hypothermia on 24-hour and 28-day mortality and to develop a prediction model.
Results:
A total of 953 patients were included, of which 354 patients had hypothermia (37%) upon ICU admission. Patients were divided into a normothermic or hypothermic group. Hypothermia was associated with a significantly increased mortality at 24 hours and 28 days (OR 2.72 (1.18-6.29 and OR 2.82 (1.83-4.35) resp.). The variables included in the final prediction model were hypothermia, age, APACHE II score (corrected for temperature), INR, platelet count, traumatic brain injury and Injury Severity Score. The final prediction model discriminated between survivors and non-survivors with high accuracy (AUC = 0.871, 95% CI 0.844-0.898).
Conclusions:
Hypothermia, defined as a temperature ≤35° Celsius, is common in critically ill trauma patients and is one of the most important physiological predictors for early and late mortality in trauma patients. Trauma patients admitted to the ICU may be at high risk for late mortality if the patient is hypothermic, coagulopathic, severely injured and has traumatic brain injury or an advanced age.
Keywords: Hypothermia, Intensive Care Unit, mortality, trauma
INTRODUCTION
Accidental hypothermia on the emergency department (ED) is frequently observed in trauma patients and is associated with poor outcomes,[1,2,3,4,5,6,7,8] although not all studies provided consistent results.[9,10] Hypothermia in trauma patients is generally defined as a core temperature of ≤35°C.[11] The association with early mortality[4,5,6,7,8,12] is thought to occur via deterioration of coagulation abilities,[13] as hypothermia causes a decreased function of clotting factors and an impaired platelet function[14] and is associated with increased blood loss and the transfusion of more blood products.[4,15]
Between time of arrival on the ED and Intensive Care Unit (ICU) admission, stabilization efforts with trauma resuscitation, medication, coiling, and damage control surgery may all influence temperature and subsequently may reverse accidental hypothermia. The impact of hypothermia present upon ICU admission on mortality occurring after stabilization efforts is not known. Of note, the occurrence of “indoor” hypothermia was found to be associated with worse outcome than “outdoor” hypothermia in a small study in a medical ICU population.[16] Transient hypothermia might have a different etiology and outcome compared to persistent hypothermia or hypothermia which occurs during hospital stay. Furthermore, well-known prediction models for mortality in trauma patients admitted to the ICU were developed in a nontrauma population or in nonintubated patients, which renders these models less suitable as prediction models for mortality in critically ill trauma patients.[17,18,19] Therefore, this study had two aims:First to study the incidence and impact of hypothermia on admission to the ICU on early and late mortality, controlling for variables that are associated with trauma-related mortality. Second to develop a prediction model for late mortality in critically ill trauma patients.
MATERIALS AND METHODS
Study design
This study was a multicenter retrospective cohort study of adult trauma patients admitted to the ED and subsequently transferred to the ICU of two Level 1-trauma centers in Amsterdam, the Netherlands. Patients were recruited between January 2007 and December 2012. All adult trauma patients who were admitted to the ICU and with core temperature measurements available upon ICU admission were eligible. The Institutional Review Board approved the study and waived the need for informed consent.
Data collection
Data on patient demographics, baseline vitals on ICU admission, injury severity as classified by the Injury Severity Score (ISS), laboratory tests, temperature on ICU admission, National Intensive Care Evaluation (NICE) score, ICU length of stay, 24-h and 28-day mortality were collected retrospectively. Demographic data and measures of severity of illness were obtained from the NICE database and the electronic patient data management system. The NICE database contains continuous and complete recordings of patients demographics, vital signs, treatment, and outcome data of patients who were admitted to the ICU to contribute to the quality of Intensive Care Medicine in the Netherlands.[20] In addition, all participants of the NICE database are trained in collecting data accurately according to clear defined definitions (http://www.stichting-nice.nl). The ISS was obtained from the ED registry. Hypothermia was measured by nasopharynx or rectal thermistor temperature probes. Only temperature measurements which were validated by nurses were taken into account for analysis.
Hypothermia was defined as a core temperature of ≤35°C on ICU admission.[11] Management of hypothermia on the ICU consisted of a warm environment, blankets, and active movement (if possible) if the temperature was between 32°C and 35°C. A temperature between 28°C and 32°C was managed by a bear hugger and warming of parenteral fluids using a fluido. Extracorporeal membrane oxygenation and cardiopulmonary bypass were added when patients had a temperature below 32°C.
The primary outcome of this study was the mortality rate at 24 h and 28 days.
Statistical analysis
Patients were categorized into a normothermic or hypothermic group. Continuous normally distributed variables are expressed by their mean and standard deviation or when not normally distributed as median and their interquartile ranges. Categorical variables are expressed as n (%). To test group differences, the Students t-test was used, if continuous data are not normally distributed the Mann–Whitney U-test was used. Categorical variables are compared with the Chi-square test.
Automatically multiple imputation by logistic regression of data was performed to handle missing values, with the exception of missing outcome variables. Reference distribution in the imputed dataset was set equal to the original dataset. Data are represented as pooled values of 10 imputations. The goal of the primary analysis (logistic regression) was to quantify the net effect of hypothermia at admission to the ICU on 24-h and 28-day mortality, controlling for variables associated with trauma-related mortality. Confounders were identified with univariable logistic regression models [Appendixes 1 and 2]. Variables included in the univariable logistic regression models were: Gender, age, weight, height, traumatic brain injury (TBI), ISS, Acute Physiology and Chronic Health Evaluation (APACHE) score corrected for temperature, mean arterial pressure (MAP), hemoglobin, pH, the total amount of blood products administered and platelet count. Furthermore, interaction terms were added to the logistic regression models to evaluate if hypothermia was a result of the injury mechanism (ISS, presence of head injury) or of resuscitation (the amount of allogeneic blood products transfused). Variables that are part of the APACHE II score were excluded to avoid redundancy in the analysis. Categorization of continuous potential confounders was used to examine linearity between these confounders and 24-h and 28-day mortality. Square terms or log transformations were used to correct for nonlinearity. A P ≤ 0.2 in the univariable logistic regression models was considered as a relevant confounding effect. Variables with a relevant confounding effect were included in the multivariable logistic regression models as predictors for 24-h and 28-day mortality by using backward selection. Only those variables with a significant association with mortality after backward selection were included in the final multivariable logistic regression models. A P = 0.05 was used as cut off value for backward selection.
The final logistic regression model for 28-day mortality was used as a prediction model and to generate a formula to predict 28-day mortality. In this formula, β-coefficients of the logistic regression model were used to develop a weighted point system. The area under the curve (AUC) of the receiver operating characteristic curve was used to evaluate the discrimination of the final model, the Hosmer–Lemeshow statistic was used to define goodness-of-fit of the model.
Statistical significance is considered to be P ≤ 0.05. Appropriate statistical uncertainty was expressed by the 95% confidence levels. Analysis was performed with SPSS Statistics 21 (IBM, Chicago, IL, USA). Methods and results were reported according to the “transparent reporting of a multivariable prediction model for individual prognosis or diagnosis” statement.[21]
RESULTS
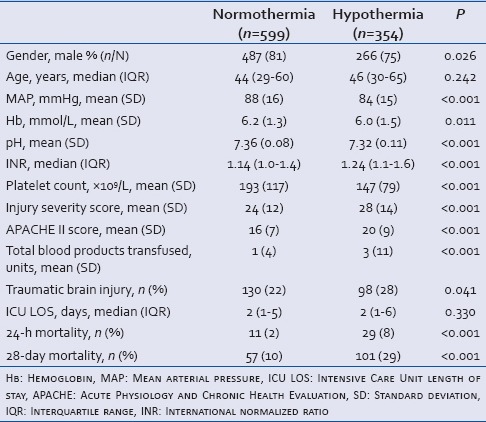
Of a total of 953 patients admitted to the ICU, 354 (37%) patients had hypothermia. Table 1 describes the different demographic characteristics of the cohort for the hypothermic and normothermic group. The majority of the patient characteristics were different between both groups. The hypothermic group was more severely injured, coagulopathic, acidotic, and had higher mortality rates. Almost 50% of the patients who died within 28 days had a core body temperature lower than 32°C on admission to the ICU.
Table 1.
Patient characteristics
Hypothermia and mortality
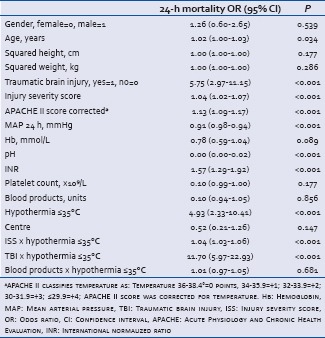
Of the patients with hypothermia, 29 (8%) patients died within 24 h and 101 patients (57%) within 28 days. The mortality rate in normothermic patients was significantly lower, 11 (2%) and 57 (10%, P < 0.001). The APACHE score II score corrected for temperature, MAP, TBI were identified as relevant confounders for 24-h mortality, whereas the APACHE score II score corrected for temperature, MAP, TBI, ISS, age, and platelet count were identified as confounding variables for 28-day mortality [Appendixes 1 and 2]. After adjustment for these confounders, hypothermia on arrival to the ICU was associated with an increased 24-h mortality (odds ratio [OR]: 2.72, 95% confidence interval [CI]: 1.18–6.29) and an increased 28-day mortality (OR: 2.82, 95% CI: 1.83–4.35). Thereby, hypothermia was one of the most important physiological predictors for both 24-h and 28-day mortality [Tables 2 and 3]. Of note, the interaction terms (hypothermia × ISS, hypothermia × TBI and hypothermia × transfusion) were not statistically significant in the multivariable logistic regression models and were therefore excluded.
Table 2.
Multivariable logistic regression model for 24-h mortality

Table 3.
Multivariable logistic regression model for 28-day mortality

Prediction model for late mortality
The final logistic regression model for 28-day mortality was used as prediction model and to generate a formula to predict 28-day mortality. Besides hypothermia, TBI, international normalized ratio (INR), APACHE II score corrected for temperature, age, ISS, and platelet count were included as predictors in the prediction model. The formula generated to predict 28-day mortality is shown in Box 1. The AUC of the final prediction model was 0.871 (95% CI: 0.844–0.898). The calibration of the model was reflected by the Hosmer–Lemeshow test of the different imputation sets, which ranged between 0.081 and 0.912 with a mean P = 0.556. This indicates that there is no significant difference between the observed and predicted outcome of the developed model.
Box 1.
Formula for predicted risk of 28.day mortality
Formula for predicted risk of mortality=1/(1+e^(−(−6.547+1.036 (if body temperature ≥35°C)+0.087 × APACHE II score corrected for temperature . 0.003 × platelet count (×109)+0.033× age+0.025 × ISS+0.287 × INR+1.153 (if TBI=yes)
DISCUSSION
This study shows that upon ICU admission following trauma, hypothermia is one of the most important physiological predictors for both early and late mortality in trauma patients. Other predictors for late mortality are age; APACHE II score corrected for temperature, INR, platelet count 109/L, TBI, and ISS. A prediction model, which combines these independent predictors, may be able to identify trauma patients at high risk for late mortality on ICU admission.
Hypothermia
This study found that hypothermia on ICU admission is common in trauma patients. More than one-third of the critically ill trauma patients in this study had hypothermia on arrival at the ICU. Similar results are found in studies investigating the incidence of hypothermia on the ED.[5,10] These findings suggest that therapy on the ED may not be focused on prevention or correction of hypothermia. Obviously, the focus of therapy in severely injured patients is on efforts to stop the bleeding and to protect the patient from further injury by failure of oxygenation of vital signs or central nervous system, which requires multiple actions and interventions. Hypothermia may aggravate bleeding, and therefore management of body temperature is part of trauma management protocols.[22] However, body core temperature is collected in 30–60%[6,23,24] of the trauma patients upon admission to the ED. Thereby, screening of body core temperature may be regarded as less important in the care of trauma patients. An alternative explanation for hypothermia upon ICU admission may be that it is not feasible to correct core body temperature, as interventions may require that the patient is (partly) uncovered and that treatment and surgical procedures may further cool the patient,[25] even when devices with warm resuscitation fluids or other rewarming techniques are applied.
Hypothermia and mortality
We have, in contrast to previous studies, examined accidental hypothermia upon admission to the ICU instead of on admission to the ED. The effect of accidental hypothermia at ICU admission on mortality is less well-documented, and may be influenced by stabilization efforts during trauma resuscitation. Therefore, the clinical significance of hypothermia may be different between these 2 time points. We found that hypothermia on ICU admission was associated with an increased mortality. This is in line with the results of two previous studies.[26,27] Furthermore, we observed that hypothermia was more frequently observed in patients with TBI and in transfused patients, which suggests that hypothermia is merely a result of the injury severity, TBI or transfusion of blood products than an independent predictor for mortality, provoked by massive blood loss and transfusion or by an impaired thermoregulation system due to TBI, also known as the lethal triad. However, in our logistic regression models, TBI and transfusion did not interact with hypothermia, which suggests that hypothermia is an independent predictor for mortality and not a result of TBI, blood loss or injury severity. Hypothermia may be a result of interventions which require that the patient is (partly) uncovered and by treatment and surgical procedures which may further cool the patient.[25] Aggressive prevention or correction of the body temperature by rewarming techniques could potentially influence the incidence of hypothermia on ICU admission and subsequently mortality. However, studies investigating the effectiveness of these rewarming devices are limited.[28,29] Further research in this field is therefore required.
Prediction model for late mortality
The results of this study identified coagulopathy, the severity of injury, the age of patients and TBI as other predictors for late mortality in trauma patients admitted to the ICU. These findings are in line with results of previous studies.[4,14,15,26] However, a prediction model for late mortality in trauma patients upon admittance to the ICU has not been developed previously. Well-known prediction models for mortality in trauma patients are the APACHE II score[18] and the trauma and ISS (TRISS).[17] The APACHE II score was developed in a nontrauma population and included no anatomical component, which reduces the ability to predict mortality in trauma patients.[19] The TRISS is a model to predict mortality in trauma patients based on predictors available on the ED like age, trauma mechanism and an estimated ISS. A disadvantage of the TRISS is the exclusion of intubated patients, which renders the TRISS not suitable as prediction model for mortality in critically ill patients. The prediction model developed in this study contains physiological and anatomical parameters and may be a promising tool for predicting mortality in trauma patients on arrival to the ICU. However, external validation of the developed model is still required. Therefore, prospective studies are warranted to confirm the accuracy of the developed prediction model.
Limitations to this study should be acknowledged. Data on surgical procedures, core body temperature upon admission to the ED and time between arrival on the ED and the ICU were not available. Furthermore, the retrospective design of this study does not control for all possible confounders. In addition, temperature measurements were done at different sites, (rectum and nasopharynx) which lag behind changes in esophageal temperature which is the gold standard for core temperature.
CONCLUSION
Hypothermia, defined as a temperature ≤35°C, is common in trauma patients upon ICU admission and is associated with increased mortality. Hypothermic trauma patients admitted to the ICU may be at high risk for late mortality if the patient is also coagulopathic, severely injured, has TBI or an advanced age.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIXES: Appendix Table 1: Univariable logistic regression for 24-h mortality
Appendix Table 2: Univariable logistic regression for 28-day mortality

REFERENCES
- 1.Reynolds BR, Forsythe RM, Harbrecht BG, Cuschieri J, Minei JP, Maier RV, et al. Hypothermia in massive transfusion: Have we been paying enough attention to it? J Trauma Acute Care Surg. 2012;73:486–91. [PubMed] [Google Scholar]
- 2.Beilman GJ, Blondet JJ, Nelson TR, Nathens AB, Moore FA, Rhee P, et al. Early hypothermia in severely injured trauma patients is a significant risk factor for multiple organ dysfunction syndrome but not mortality. Ann Surg. 2009;249:845–50. doi: 10.1097/SLA.0b013e3181a41f6f. [DOI] [PubMed] [Google Scholar]
- 3.Rubiano AM, Sanchez AI, Estebanez G, Peitzman A, Sperry J, Puyana JC. The effect of admission spontaneous hypothermia on patients with severe traumatic brain injury. Injury. 2013;44:1219–25. doi: 10.1016/j.injury.2012.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bukur M, Hadjibashi AA, Ley EJ, Malinoski D, Singer M, Barmparas G, et al. Impact of prehospital hypothermia on transfusion requirements and outcomes. J Trauma Acute Care Surg. 2012;73:1195–201. doi: 10.1097/TA.0b013e31826fc7d9. [DOI] [PubMed] [Google Scholar]
- 5.Ireland S, Endacott R, Cameron P, Fitzgerald M, Paul E. The incidence and significance of accidental hypothermia in major trauma – A prospective observational study. Resuscitation. 2011;82:300–6. doi: 10.1016/j.resuscitation.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Martin RS, Kilgo PD, Miller PR, Hoth JJ, Meredith JW, Chang MC. Injury-associated hypothermia: An analysis of the 2004 National Trauma Data Bank. Shock. 2005;24:114–8. doi: 10.1097/01.shk.0000169726.25189.b1. [DOI] [PubMed] [Google Scholar]
- 7.Shafi S, Elliott AC, Gentilello L. Is hypothermia simply a marker of shock and injury severity or an independent risk factor for mortality in trauma patients. Analysis of a large national trauma registry? J Trauma. 2005;59:1081–5. doi: 10.1097/01.ta.0000188647.03665.fd. [DOI] [PubMed] [Google Scholar]
- 8.Wang HE, Callaway CW, Peitzman AB, Tisherman SA. Admission hypothermia and outcome after major trauma. Crit Care Med. 2005;33:1296–301. doi: 10.1097/01.ccm.0000165965.31895.80. [DOI] [PubMed] [Google Scholar]
- 9.van der Ploeg GJ, Goslings JC, Walpoth BH, Bierens JJ. Accidental hypothermia: Rewarming treatments, complications and outcomes from one university medical centre. Resuscitation. 2010;81:1550–5. doi: 10.1016/j.resuscitation.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 10.Mommsen P, Andruszkow H, Frömke C, Zeckey C, Wagner U, van Griensven M, et al. Effects of accidental hypothermia on posttraumatic complications and outcome in multiple trauma patients. Injury. 2013;44:86–90. doi: 10.1016/j.injury.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Soar J, Perkins GD, Abbas G, Alfonzo A, Barelli A, Bierens JJ, et al. European resuscitation council guidelines for resuscitation 2010 section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010;81:1400–33. doi: 10.1016/j.resuscitation.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Hildebrand F, Giannoudis PV, van Griensven M, Chawda M, Pape HC. Pathophysiologic changes and effects of hypothermia on outcome in elective surgery and trauma patients. Am J Surg. 2004;187:363–71. doi: 10.1016/j.amjsurg.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 13.Mikhail J. The trauma triad of death: Hypothermia, acidosis, and coagulopathy. AACN Clin Issues. 1999;10:85–94. [PubMed] [Google Scholar]
- 14.Zhang JN, Wood J, Bergeron AL, McBride L, Ball C, Yu Q, et al. Effects of low temperature on shear-induced platelet aggregation and activation. J Trauma. 2004;57:216–23. doi: 10.1097/01.ta.0000093366.98819.fe. [DOI] [PubMed] [Google Scholar]
- 15.Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108:71–7. doi: 10.1097/01.anes.0000296719.73450.52. [DOI] [PubMed] [Google Scholar]
- 16.Mégarbane B, Axler O, Chary I, Pompier R, Brivet FG. Hypothermia with indoor occurrence is associated with a worse outcome. Intensive Care Med. 2000;26:1843–9. doi: 10.1007/s001340000702. [DOI] [PubMed] [Google Scholar]
- 17.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: The TRISS method. Trauma score and the injury severity score. J Trauma. 1987;27:370–8. [PubMed] [Google Scholar]
- 18.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 19.McAnena OJ, Moore FA, Moore EE, Mattox KL, Marx JA, Pepe P. Invalidation of the APACHE II scoring system for patients with acute trauma. J Trauma. 1992;33:504–6. doi: 10.1097/00005373-199210000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Arts D, de Keizer N, Scheffer GJ, de Jonge E. Quality of data collected for severity of illness scores in the Dutch National Intensive Care Evaluation (NICE) registry. Intensive Care Med. 2002;28:656–9. doi: 10.1007/s00134-002-1272-z. [DOI] [PubMed] [Google Scholar]
- 21.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BJOG. 2015;122:434–43. doi: 10.1111/1471-0528.13244. [DOI] [PubMed] [Google Scholar]
- 22.9th ed. Chicago: Hearthside Publishing Services; 2012. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support; Student Course Manual. [Google Scholar]
- 23.Trentzsch H, Huber-Wagner S, Hildebrand F, Kanz KG, Faist E, Piltz S, et al. Hypothermia for prediction of death in severely injured blunt trauma patients. Shock. 2012;37:131–9. doi: 10.1097/SHK.0b013e318245f6b2. [DOI] [PubMed] [Google Scholar]
- 24.Langhelle A, Lockey D, Harris T, Davies G. Body temperature of trauma patients on admission to hospital: A comparison of anaesthetised and non-anaesthetised patients. Emerg Med J. 2012;29:239–42. doi: 10.1136/emj.2009.086967. [DOI] [PubMed] [Google Scholar]
- 25.Hirshberg A, Sheffer N, Barnea O. Computer simulation of hypothermia during “damage control” laparotomy. World J Surg. 1999;23:960–5. doi: 10.1007/s002689900607. [DOI] [PubMed] [Google Scholar]
- 26.Konstantinidis A, Inaba K, Dubose J, Barmparas G, Talving P, David JS, et al. The impact of nontherapeutic hypothermia on outcomes after severe traumatic brain injury. J Trauma. 2011;71:1627–31. doi: 10.1097/TA.0b013e3182159e31. [DOI] [PubMed] [Google Scholar]
- 27.Rutherford EJ, Fusco MA, Nunn CR, Bass JG, Eddy VA, Morris JA., Jr Hypothermia in critically ill trauma patients. Injury. 1998;29:605–8. doi: 10.1016/s0020-1383(98)00139-9. [DOI] [PubMed] [Google Scholar]
- 28.Steele MT, Nelson MJ, Sessler DI, Fraker L, Bunney B, Watson WA, et al. Forced air speeds rewarming in accidental hypothermia. Ann Emerg Med. 1996;27:479–84. doi: 10.1016/s0196-0644(96)70237-8. [DOI] [PubMed] [Google Scholar]
- 29.Gentilello LM, Jurkovich GJ, Stark MS, Hassantash SA, O’Keefe GE. Is hypothermia in the victim of major trauma protective or harmful. A randomized, prospective study? Ann Surg. 1997;226:439–47. doi: 10.1097/00000658-199710000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]


