Abstract
Background
In current study we aimed to examine the effect of a low-level laser therapy on the pain, mouth opening and swelling of patients whose impacted 3rd molar tooth was extracted in addition measurement volumetrically to the edema with 3dMD face system.
Methods
It was surveyed 15 patients who had bilateral symmetric lower 3rd molars. Surgical sides of patients were randomly separated into two groups: the study group and the control group. It was applied extra oral low-level laser therapy (LLLT, 0.3 W, 40 s, 4 J/cm2) to the study group (n = 15) after the surgical operation and on the 2nd day. Only routine postoperative recommendation (ice application) was made in the control (n = 15) group. The maximum mouth opening, pain level and facial swelling evaluated. 3dMD Face® (3dMD, Atlanta, GA) Photogrammetric System was used to evaluate volumetric changes of the swelling.
Results
There was no statistically significant difference in the edema and interincisal opening between the groups and the pain level in the laser group was significantly lower than in the control group on the 7th postoperative day.
Conclusions
Although there were decreasing trismus, swelling, and pain level, with this LLLT, there was significant difference only in the 7th day pain level in the laser group compared with the control group.
Keywords: Laser, 3rd molar, 3dMD, Pain, Swelling, Trismus
Background
The most frequently performed surgical procedure in maxillofacial surgery is impacted 3rd molar tooth extraction. It is a minor surgical procedure practiced mostly under local anaesthesia; difficulty varies according to the location of the tooth [1]. The anatomical location wound surface of the surgical area is in the mouth, and the area is constantly irritated due to the movement of the mouth, which may lead to postoperative complaints among patients rather than the surgery itself [2]. Patients’ main clinical complaints are postoperative pain, swelling, and limited opening of the mouth. To prevent these complaints, researchers have suggested many methods such as administering preoperative systemic and topical anti-inflammatory drugs and applying laser therapy [3–5].
Lasers are effectively used in dentistry as well as widely used in many areas of medicine. In dentistry, lasers are generally used in such practices as the treatment of aphtha, fracture healing, gingivoplasty, gingivectomy, frenectomy, biostimulation of soft and hard tissue wound, echodentography and dental imaging. [6–11].
Researchers have determined that laser therapy has analgesic, anti-inflammatory, and biostimulant effects, increases tissue nutrition and connective tissue elasticity, reduces edema, increases lymphatic drainage, and increases regeneration in the synovial membrane [12].
The effect of laser therapy depends on the wavelength and the dosage of the laser beam [13–19]. Low-energy lasers generally have less than 90 mW power. These lasers should be distinguished from the high-energy (10–100+ W) lasers used in surgery, dermatology, and ophthalmology. Low-dosage lasers emit the lowest level of energy and are a type of intensive, focal light therapy [20]. These lasers are also used for “biostimulation” at low dosages in tissue. Low-dosage lasers accelerate wound healing especially in diabetic patients by stimulating fibroblast proliferation with wavelengths ranging between 300 and 400 mw/cm2 [21, 22].
With the developing technology, the edema that occurs in patients can be numerically determined through computer systems. In this study, the three-dimensional (3D) photographic image method 3dMD Face® (3dMD, Atlanta, GA) was used to help quantify postoperative volumetric changes after removal of wisdom third molar. Several studies have shown the accuracy and reproducibility of the 3D imaging technique to measure facial appearances [23]. In 1944, Thalmaan was the first researcher to use the stereophotogrammetry technique in clinical studies [24]. Photogrammetry finds a point on a surface in space. Stereophotogrammetry is a more complex technique that provides the 3D coordinates of an object in space. In this method, depth information of the points in images from different cameras is obtained based on the distance from specific measurement areas. The location of all points on an object on the x, y, and z axes in space is given by the computer program. The object is thus called the point cloud. Then the point clouds are combined, and a wire cage-like view called a wireframe is obtained. The surface texture is obtained by covering this cage with a color photograph [25]. Data obtained using these views provide the opportunity to more clearly measure the edema and postoperative changes that occur.
Although several studies have evaluated the efficiency of LLLT in preventing swelling, trismus and pain after the removal of impacted 3rd molars, there are still conflicting results of effect of LLLT on the edema, swelling and pain. However, in the literature there is no study that measured to edema with 3dMD face system. So, in this study we aimed to examine the effect of a LLLT on the pain, mouth opening and swelling of patients whose impacted 3rd molar tooth was extracted in addition measurement volumetrically to the edema with 3dMD face system.
Methods
Fifteen patients with asymptomatic bilateral wisdom mandibular 3rd molar participated in the study. Patients who had bilateral impacted, III B surgical difficulty grade and required the removal of lower 3rd molars in symmetrical position were included the study. The exclusion criteria included contraindications of laser therapy, systemic illness, current smoking habit, local infection, acute pericoronitis, pregnancy, or breastfeeding. All subjects were informed of the risks of oral surgery and empirical treatment, and they signed a consent form approved by the institution.
Surgery was performed under local anesthesia with 2 ml of 4 % articaine with epinephrine 1:100,000 (Ultracain® D-S Forte, Sanofi Aventis, Istanbul, Turkey) in two sessions separated by at least a month. A single surgeon performed all surgical procedures in order to avoid differences among different surgeons’ skills, which might have influenced the results. All patients required a similar surgical technique for both procedures, because the two 3rd molars were symmetric and had a similar degree of difficulty. A random side impacted tooth of the patients was extracted at the first appointment, and an extraoral laser was applied on the area of masseter muscle immediately after the surgical procedure and at the appointment 2 days after the surgical procedure. At the follow-up appointment 1 month later, it was determined that the patients had achieved their normal mouth opening, and there was complete healing in the area of the surgical procedure. The other side impacted 3rd molar tooth was then extracted. Ice was applied for the first 48 h.
After each surgical procedure, 500 mg paracetamol (Parol, Atabay, Istanbul, Turkey) and benzydamine HCL + chlorhexidine gluconate gargle antiseptic solution (Farhex, Santa Farma, Istanbul, Turkey) were administered two times per day for 7 days. All patients were advised not to use ice after the surgical procedure on the laser-applied side, to control the impact of the laser on facial edema.
In this study, a gallium–aluminum–arsenide (GaAlAs) diode laser device (CHEESE Dental Laser System, Wuhan GigaaOptronics Technology Company, China) with a continuous wavelength of 810 nm was used, and the laser therapy was applied by using a 1 × 3-cm hand piece with non-contact mode. Laser energy was applied to treatment group at 300 mW (0.3 W) for a total of 40 s. Patients in the low-level laser therapy (LLLT) group (n = 15) received 12 J (4 J/cm2) low-level laser irradiation at the insertion point of the masseter muscle immediately after the surgery and the 2nd day after the surgery.
The variables evaluated were gender, age, facial swelling, length of the surgical procedure, level of pain degree, and the maximum mouth opening. The length of the surgical procedure was defined as the time between the incision and the last suture.
The pain levels were recorded on the visual analogue scale (VAS) of 10 cm; the scores ranged from 0 (no pain) to 10 (the worst pain possible). The pain was recorded after surgery, 2nd day, and 7th day always at the same time. Mouth opening and facial swelling were recorded three times: before surgery, after 2 days, and after 7 days.
The maximum mouth opening (MMO) was determined by evaluating the interincisal distance with a compass, and facial edema was determined with 3D images of the patients.
The 3dMD Vultus program (3dMD, Atlanta, GA) was used to analyze the images. In this program, two different images can be aligned on the chosen surfaces. Linear and volumetric measurement can be made between the aligned images. The analysis began by transferring the records of the patients taken before the surgical procedure (T0), 2 days (T1) after the surgical procedure, and 7 days (T2) after the surgical procedure as a.tsb document to the Vultus program. Two images were aligned on the forehead and nasofrontal area in order to examine them after the images were adjusted. A quadrilateral area with the subnasale, tragion, gonion, and menton points as the corners was selected after the images were aligned (Fig. 1), and the volumetric difference between the two surfaces was measured by calculating the volumetric difference (Fig. 2).
Fig. 1.
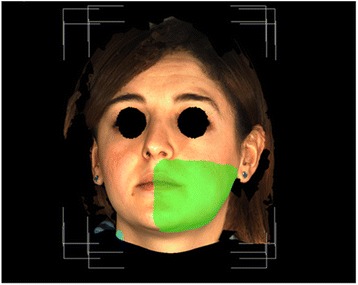
Selected area for measuring of swelling
Fig. 2.

Histogram image of swelling
IBM SPSS statistics 22.0 program was used in the statistical assessment. The data were summarized as the smallest and the biggest with the median. The compliance of the data with the normal distribution was assessed using the Shapiro-Wilcoxon test. The Mann–Whitney U test was used to compare the two groups. p < 0.05 was considered significant.
Results
The patients’ average age was 22.58 (17–29). Duration of surgery was similar between the laser and control groups (p > 0.05; see Table 1). The patients experienced no side effects of the applied treatment.
Table 1.
Duration of surgery
| Group 1 | Group 2 | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | p | |
| Duration of surgery | 12,9 ± 3,8 | 13,0 ± 4,0 | 0,959 |
There was a small decrease in pain intensity in the side on which LLLT was applied on the 2nd and 7th day after surgery; however, there was a statistically significant difference only on the 7th day (p < 0.05; Table 2).
Table 2.
Evaluation of VAS, swelling, and interincisal opening
| Laser group | Control group | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p | ||
| Edema | 2ndday | 24,1 ± 16,2 | 21,1 ± 12,9 | 0,618 |
| 7thday | 3,6 ± 3,9 | 5,6 ± 7,8 | 0,485 | |
| p | 0,002 | 0,002 | ||
| VAS | 2ndday | 4,8 ± 1,9 | 5,4 ± 1,7 | 0,440 |
| 7thday | 1,3 ± 1,2 | 2,7 ± 1,2 | 0,017 | |
| p | <0,001 | 0,001 | ||
| Mouth opening | 0 day | 45,5 ± 4,1 | 43,2 ± 5,5 | 0,250 |
| 2ndday | 26,3 ± 4,7 | 25,0 ± 3,3 | 0,430 | |
| 7thday | 39,0 ± 5,2 | 36,0 ± 4,1 | 0,129 | |
| p | p < 0,001 | p <0,001 |
Bold characters in each column represent the differences between the measurement periods
For facial swelling, although the laser group had less swelling than the control group on the 2nd day, there was no significant difference between the two groups after the 2nd and 7th postoperative days (p < 0.05; Table 2).
The LLLT group presented a greater degree of oral opening than the control group on the 2nd and the 7th day after surgery, but there was no statistically significant difference (p > 0.05; Table 2).
Discussion
The present study examined the effect of LLLT on swelling, pain, and trismus after lower 3rd molar extraction. In this study, we found that although the laser group had less swelling and a greater degree of oral opening there was no statistically significant difference (p > 0.05). There was a statistically significant difference only on the 7th day in the decrease in pain intensity (p < 0.05).
It was determined that laser application has analgesic, anti-inflammatory, and biostimulant effects, increases tissue nutrition and collagen tissue elasticity, reduces edema, increases lymphatic drainage, and increases regeneration in the synovial membrane [12, 26, 27]. The biostimulation effect of LLLT is controversial. The absence of constant parameters of physical and biological variables of the lasers applied in a previous study, for instance, the type of laser, frequency of pulse, output of power, time of application, wavelength, and distance of the source from the tissue, cause difficulties in calibrating the results [28].
Although several studies have evaluated the efficiency of LLLT in preventing swelling and trismus after the removal of impacted 3rd molars, some studies described a positive effect of laser, but others did not [26]. Therefore, until now, the parameters of optimal LLLT for biostimulation have not been known [29].
Clokie et al. [30], Fernando et al. [31], and Taube et al. [32] examined the effect of LLLT application on pain and swelling after the removal of the bilateral lower 3rd molar in the same surgical procedures, although Roynesdal et al. [33] examined the effect of LLLT application on swelling, pain, and trismus after the removal of the bilateral lower 3rd molar in two separate surgical procedures. The researchers used different laser parameters in these studies; all suggested that LLLT had no beneficial effect on swelling and trismus after extraction of the wisdom 3rd molar. Clokie et al. [30] reported that there was a statistically significant difference in the reduction of pain on the day of surgery and on the 1st postoperative day. In our study, we found that LLLT was effective in decreasing pain levels only on the 7th postoperative day. However, Carillo et al. [34] described that although there was a statistically significant difference in the decrease in the ratio of trismus in the laser group up to 7 days after surgery, there were no differences in the percentage of swelling and pain between the laser and placebo groups.
Aras et al. [35] investigated the impact of intraoral and extraoral applications of LLLT on swelling and trismus after the removal of mandibular 3rd molars. 48 patients were divided into 3 equal groups (16 each); as follows: extraoral LLLT, intraoral LLLT, and placebo. They used the GaAlAs diode laser device with a continuous wavelength of 808 nm in their study and applied laser energy at 100 mW (0.1 W) for a total of 120 s (12 J). They found that use of LLLT extraorally had a significantly positive effect on trismus and swelling. Kazancioglu et al. [36] examined and compared the effect of LLLT and ozone therapy after wisdom 3rd-molar surgery by applying 12 J (4 J/cm2) of energy with a GaAlAs diode laser at 808 nm extraorally immediately after the surgical procedure and on the postoperative 1st, 3rd, and 7th day in the laser group. They reported that the pain level was lower in the ozonated and LLLT applied groups than in the control group; however, trismus and swelling in the LLLT group were significantly lower than in the ozonated and control groups. Acar et al. [37] evaluated the efficacy of LLLT and low-intensity pulsed ultrasound (LIPUS), alone and in combination, in triggering new bone formation. They demonstrated the efficacy of LLLT or LIPUS in triggering bone regeneration. Lim et al. [38] investigated in vitro effects of low-intensity pulsed ultrasound stimulation on the osteogenic differentiation of human alveolar bone-derived mesenchymal stem cells (hABMSCs) for tooth tissue engineering. This study reported that LIPUS could enhance the cell viability and osteogenic differentiation of hABMSCs, and could be part of effective treatment methods for clinical applications. Ferrante et al. [26] studied 2 groups that treated removal of a lower 3rd molar, by applying 54 J of energy with a laser diode at 980 nm intraorally and extraorally immediately after surgery and at 24 h. They recorded the number of days and levels of postoperative pain. The statistical analysis showed significant differences between the laser group and the control group in terms of swelling and trismus, but there was no significant difference in terms of pain levels. These authors observed that LLLT was more effective when it was applied extraorally instead of intraorally. In contrast to these results, in our study, although LLLT was applied extraorally, there was no statistically significant difference in terms of trismus and swelling levels, but there was a significant decrease in the pain level on the 7th day.
The mechanism of the analgesic effect provided by LLLT is not yet certain. There is evidence that LLLT has significant neuropharmacological effects on the synthesis, release, and metabolism of such neurochemicals as serotonin and acetylcholine at the central level and histamine and prostaglandin at the peripheral level. This analgesic effect can be explained with the effect of LLLT on the synthesis of endorphin and the decrease in the activity or bradykining of C fibers [39].
Trismus, degree of inflammation, or pain intensity may differ among patients. Thus, the separate surgical procedure design of this study helped avoid bias in the data collection [29], different from when the experimental individuals and the controls are different [26, 34, 35]. This study was managed with similarly impacted lower 3rd molar tooth with an equal grade of difficulty; thus, each person was his or her own control.
Dimensional measurements were made in the assessment of the swelling that occurred after the surgical procedure in previous studies. The 3dMD Face method was used in our study in order to assess the volumetric increase in swelling. With this method, the 3dMD image of the patient was taken before the surgery (0) and on the 2nd and 7th days after the surgery, and the volume of the area between the 2 images was calculated using the 3DMD program by aligning the images from the 2nd day and day 0, and the 7th day and day 0. We believe that the assessment made using this method yields a more accurate result.
Conclusions
The procedures and outcomes of previous studies are too varied to describe the perfect parameters for use of LLLT or to assess its clinical efficiency. In this study, LLLT was applied extraorally and furthermore we used a different method to evaluate objectively volume changes. Although the results indicate that the proposed method reduces pain, swelling, and trismus, significant differences were observed only in the 7th day pain level in the laser group compared with the control group.
Abbreviations
3D, three-dimensional; GaAlAs, gallium–aluminum–arsenide; LLLT, low-level laser therapy; MMO, maximum mouth opening; VAS, visual analogue scale
Acknowledgments
We thank Cemil Çolak for his assistance in statistical analysis.
This study was presented as a poster presentation in Turkish Association of Oral and Maxillofacial Surgery (TAOMS) Congress 19–22 May, 2015.
Funding
There is no any source of funding for the research reported.
Availability of data and materials
The data will not be shared.
Authors’ contributions
HA conceived of the study, and participated in its design and coordination. Performed surgery. Helped to draft the manuscript. ÜY conceived of the study, and participated in its design and helped to draft the manuscript. MK conceived of the study, and participated in its design and helped to draft the manuscript. CÖ Applied LLLT and measured to interincisal opening, Data Collection, Literature Search, SAÖ Measured to swelling with 3DMD. SM conceived of the study, and participated in its design. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests in this work.
Consent for publication
We have received consent for publication from patients.
Ethics approval and consent to participate
The study protocol was approved by the Human Ethics Committee of Inonu University Faculty of Medicine (No: 2012/147), and the clinical trial was conducted in accordance with the Declaration of Helsinki. Each patient provided informed consent after receiving detailed information about the study.
Contributor Information
Hilal Alan, Phone: +90 422 3411106, Email: hilalturker@hotmail.com.
Ümit Yolcu, Phone: +90 422 3411106, Email: umityolcu28@hotmail.com.
Mahmut Koparal, Phone: + 90 416 225 1920, Email: drmahmutkoparal@gmail.com.
Cem Özgür, Phone: +90 422 3411106, Email: dr.ozgurcem86@hotmail.com.
Seyit Ahmet Öztürk, Phone: +90 422 3411106, Email: dt.s.ahmetozturk@gmail.com.
Sıddık Malkoç, Phone: +90 422 3411106, Email: siddikmalkoc@yahoo.com.
References
- 1.Leonard MS. Removing third molars: a review for the general practitioner. JADA. 1992;123:70–86. doi: 10.14219/jada.archive.1992.0041. [DOI] [PubMed] [Google Scholar]
- 2.Sisk AL, Mosley RO, Martin RP. Comparison of preoperative and postoperative diflunisal for suppression of postoperative pain. J Oral Maxillofac Surg. 1989;47:464–8. doi: 10.1016/0278-2391(89)90278-4. [DOI] [PubMed] [Google Scholar]
- 3.Sisk AL, Grover BJ. A comparison of pre-operative and postoperative naproxen sodium for suppression of postoperative pain. J Oral Maxillofac Surg. 1990;48:674–8. doi: 10.1016/0278-2391(90)90048-7. [DOI] [PubMed] [Google Scholar]
- 4.Bjørnsson GA, Haanaes HR, Skoglund LA. Ketoprofen 75 mg qid versus acetaminophen 1000 mg qid for 3 days on swelling, pain, and other postoperative events after third-molar surgery. J Clin Pharmacol. 2003;43:305–14. doi: 10.1177/0091270002250603. [DOI] [PubMed] [Google Scholar]
- 5.Ong KS, Seymour RA, Chen FG, et al. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg. 2004;33:771–6. doi: 10.1016/j.ijom.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 6.Alan H, Vardi N, Özgür C, Hüseyin A, Yolcu Ü, Doğan DO. Comparison of the effects of low-level laser therapy and ozone therapy on bone healing. J Craniofac Surg. 2015;26:e396–400. doi: 10.1097/SCS.0000000000001871. [DOI] [PubMed] [Google Scholar]
- 7.Lim HM, Lew KKK, Tay DKL. A clinical investigation of the efficacy of low-level laser therapy in reducing orthodontic post adjustment pain. Am J Orthod Dentofacial Orthop. 1995;108:614–22. doi: 10.1016/S0889-5406(95)70007-2. [DOI] [PubMed] [Google Scholar]
- 8.Neiburger EJ. Rapid healing of gingival incisions by the helium-neon diode laser. J Mass Dent Soc. 1999;48:8–13. [PubMed] [Google Scholar]
- 9.Dos Santos S, Prevorovsky Z. Imaging of human tooth using ultrasound based chirp-coded nonlinear time reversal acoustics. Ultrasonics. 2011;51(6):667–74. doi: 10.1016/j.ultras.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Marotti J, Heger S, Tinschert J, Tortamano P, Chuembou F, Radermacher K, Wolfart S. Recent advances of ultrasound imaging in dentistry-a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(6):819–32. doi: 10.1016/j.oooo.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Ueda Y, Shimizu N. Effects of pulse frequency of Low-Level Laser Therapy (LLLT) on bone nodule formation in rat calvarial cells. J Clin Laser Med Surg. 2004;21(5):271–7. doi: 10.1089/104454703322564479. [DOI] [PubMed] [Google Scholar]
- 12.Alghadir A, Omar MT, Al-Askar AB, Al-Muteri NK. Effect of low level laser therapy in patients with chronic knee osteoarthritis: a single-blinded randomized clinical study. Lasers Med Sci. 2014;29:749e755. doi: 10.1007/s10103-013-1393-3. [DOI] [PubMed] [Google Scholar]
- 13.Fukuda VO, et al. Short-term efficacy of low-level laser therapy in patients with knee osteoarthritis: a randomized placebo controlled, double-blind clinical trial. Rev Bras Ortop. 2011;46(5):526e533. doi: 10.1590/S0102-36162011000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enwemeka CS. Standard parameters in laser phototherapy. Photomed Laser Surg. 2008;26:411–2. doi: 10.1089/pho.2008.9770. [DOI] [PubMed] [Google Scholar]
- 15.Enwemeka CS. Intricacies of dose in laser phototherapy for tissue repair and pain relief. Photomed Laser Surg. 2009;27:387–93. doi: 10.1089/pho.2009.2503. [DOI] [PubMed] [Google Scholar]
- 16.Huang YY, Chen ACH, Carroll JD, Hamblin MR. Biphasic dose response in low level ligh therapy. Dose Response. 2009;7:358–83. doi: 10.2203/dose-response.09-027.Hamblin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jenkins PA, Carroll JD. How to report low-level laser therapy (LLLT)/Photomedicine dose and beam parameters in clinical and laboratory studies. Photomed Laser Sur. 2001;29:785–7. doi: 10.1089/pho.2011.9895. [DOI] [PubMed] [Google Scholar]
- 18.World Association of Laser Therapy (WALT) Standards for the design and conduct of systematic reviews with low-level laser therapy for musculoskeletal pain and disorders. Photomed Laser Surg. 2006;24:759–60. doi: 10.1089/pho.2006.24.759. [DOI] [PubMed] [Google Scholar]
- 19.WALT recommended treatment doses for low level laser therapy. April 2010 Available at: http://waltza.co.za/documentation-links/recommendations. Accessed 10 Dec 2015.
- 20.WALT. Dose table 904 nm for low level laser therapy WALT 2010; April 2010. Available at: http://waltza.co.za/wp-content/uploads/2012/08/Dose_table_904nm_for_Low_Level_Laser_Therapy_WALT-2010.pdf. Accessed 10 Dec 2015.
- 21.Karu TM. Molecular mechanism of the therapeutic effect of low intensity laser radiation. Laser Life Sci. 1988;2:53–74. [Google Scholar]
- 22.Hansen H, Thor EU. Low power laser biostimulation of chronic oro-facial pain; a double-blind placebo-controlled cross-over study of 40 patients. Pain. 1990;43:169–75. doi: 10.1016/0304-3959(90)91070-Y. [DOI] [PubMed] [Google Scholar]
- 23.Lübbers HT, Medinger L, Kruse A, Grätz KW, Matthews F. Precision and accuracy of the 3dMD photogrammetric system in craniomaxillofacial application. J Craniofac Surg. 2010;21(3):763–7. doi: 10.1097/SCS.0b013e3181d841f7. [DOI] [PubMed] [Google Scholar]
- 24.Burke P. Stereophotogrammetric measurement of normal facial asymmetry in children. Hum Biol. 1971;43:536–48. [PubMed] [Google Scholar]
- 25.Thalmaan D. Die Stereogrammetrie: ein diagnostisches Hilfsmittel in der Kieferorthopaedie [Stereophotogrammetry: a diagnostic device in orthodontology] Zurich: University Zurich; 1944. [Google Scholar]
- 26.Ferrante M, Petrini M, Trentini P, Perfetti G, Spoto G. Effect of low-level laser therapy after extraction of impacted lower third molars. Lasers Med Sci. 2013;28:845–9. doi: 10.1007/s10103-012-1174-4. [DOI] [PubMed] [Google Scholar]
- 27.Sun G, Tunér J. Low-level laser therapy in dentistry. Dent Clin North Am. 2004;48:1061–76. doi: 10.1016/j.cden.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Amarillas-Escobar ED, et al. Use of therapeutic laser after surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2010;68:319–24. doi: 10.1016/j.joms.2009.07.037. [DOI] [PubMed] [Google Scholar]
- 29.López-Ramírez M, Vílchez-Pérez MA, Gargallo-Albiol J, Arnabat-Domínguez J, Gay-Escoda C. Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction. A preliminary study. Lasers Med Sci. 2012;27:559–66. doi: 10.1007/s10103-011-0936-8. [DOI] [PubMed] [Google Scholar]
- 30.Clokie C, Bentley KC, Head TW. The effects of the helium-neon laser on postsurgical discomfort: a pilot study. J Can Dent Assoc. 1991;57:584–6. [PubMed] [Google Scholar]
- 31.Fernando S, Hill CM, Walker R. A randomised double blind comparative study of low-level laser therapy following surgical extraction of lower third molar teeth. Br J Oral Maxillofac Surg. 1993;31:170–2. doi: 10.1016/0266-4356(93)90118-G. [DOI] [PubMed] [Google Scholar]
- 32.Taube S, Piironen J, Ylipaavalniemi P. Helium-neon laser therapy in the prevention of postoperative swelling and pain after wisdom tooth extraction. Proc Finn Dent Soc. 1990;86:23–7. [PubMed] [Google Scholar]
- 33.Røynesdal AK, Björnland T, Barkvoll P, Haanaes HR. The effect of soft-laser application on postoperative pain and swelling. A double-blind, cross over study. Int J Oral Maxillofac Surg. 1993;22:242–5. doi: 10.1016/S0901-5027(05)80646-0. [DOI] [PubMed] [Google Scholar]
- 34.Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J. 1990;40:31–6. [PubMed] [Google Scholar]
- 35.Aras MH, Güngörmüş M. Placebo-controlled randomized clinical trial of the effect two different low-level laser therapies (LLLT)—intraoral and extraoral—on trismus and facial swelling following surgical extraction of the lower third molar. Lasers Med Sci. 2010;25:641–5. doi: 10.1007/s10103-009-0684-1. [DOI] [PubMed] [Google Scholar]
- 36.Kazancioglu HO, Ezirganli S, Demirtas N. Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers Med Sci. 2014;29:1313–9. doi: 10.1007/s10103-013-1300-y. [DOI] [PubMed] [Google Scholar]
- 37.Acar AH, Yolcu Ü, Altındiş S, Gül M, Alan H, Malkoç S. Bone regeneration by low-level laser therapy and low-intensity pulsed ultrasound therapy in the rabbit calvarium. Arch Oral Biol. 2016;61:60–5. doi: 10.1016/j.archoralbio.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 38.Lim K, Kim J, Seonwoo H, Park SH, Choung PH, Chung JH. In vitro effects of low-intensity pulsed ultrasound stimulation on the osteogenic differentiation of human alveolar bone-derived mesenchymal stem cells for tooth tissue engineering. Biomed Res Int. 2013;2013:269724. doi: 10.1155/2013/269724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Nguyen T, Turcotte JY. Lasers in maxillofacial surgery and dentistry. J Can Dent Assoc. 1994;60:227–8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data will not be shared.


