Abstract
Background/purpose
Emergency department thoracotomy (EDT) has been proposed to be futile in the pediatric patient population. This extreme procedure has survival rates of 0 to 26% in the non-adult population. When taking into consideration that the mechanism of injury is one of the strongest predictors of survival, we hypothesize that the low survival rate in pediatric patients is attributable to a higher rate of blunt trauma compared to their adolescent counterparts.
Methods
Prospective data collected from our level 1 trauma center from 1974 - 2014 on all patients undergoing EDT at our institution was evaluated for age 18 or younger. Patient predictor variables included injury mechanism, injury pattern, and detected cardiac activity in the field. Outcomes included successful resuscitation (re-establish of blood pressure and taken to operating room) and overall survival. Patients were dichotomized by age into pediatric (age ≤ 15 yrs) and adolescent (16-18yrs) categories.
Results
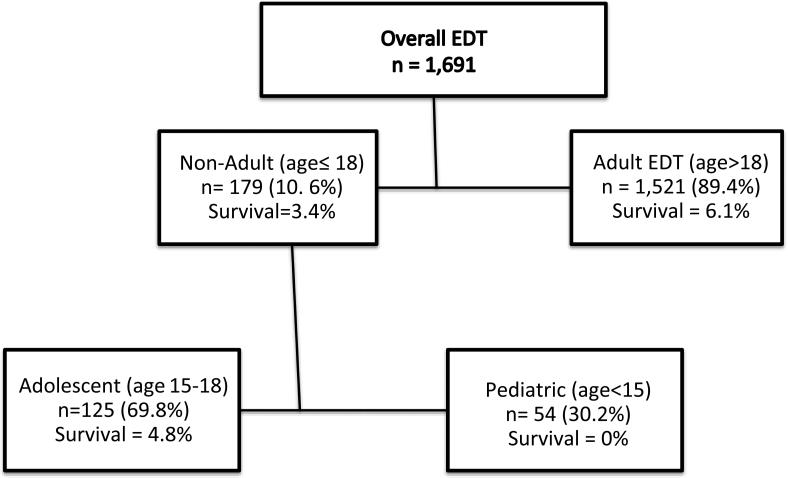
1691 patients who underwent EDT were evaluated for age of 18 or less, which included 179 patents (11%). Overall survival in the adult population was 6.1%, compared to 3.4% in the non-adult population (p=0.157). Pediatric patients were more likely to sustain blunt injury than adolescents (72% vs 32% p<0.001). This also corresponded to differences in anatomic injury patterns and more multisystem trauma (52% vs 44% p=0.001). Adolescents had significantly higher survival rates than pediatric patients (5% vs 0% p=0.036).
Conclusion
In non-adult patients undergoing EDT, adolescents have a higher survival rate than pediatric patients. The pediatric population had a significantly lower incidence of penetrating trauma and higher incidence of head injury. The discrepancy in survival between adolescent and pediatric patients appears to be attributable due to differences in mechanism. Therefore, those pediatric patients with penetrating thoracic injuries may still benefit from EDT.
Keywords: Emergency Department Thoracotomy, Futility, Pediatric, Adolescent, Survival, Trauma
1. Introduction
Hemorrhage is the most common cause of preventable death from trauma[1]. For nearly 50 years, the emergency department thoracotomy (EDT) has been utilized to attempt to salvage patients in circulatory arrest secondary to acute blood loss[2]. The largest study evaluating over 4,000 trauma patient undergoing this procedure reported a survival rate of 7.4% [3]. While this seems like a relatively low percentage of success, the alternative to this procedure is death. Shafi et al. [4] evaluating 5 major trauma centers during the last decade and identified that EDT was performed in only 13% of patients when indicated. This life saving procedure when implemented in salvageable adult trauma patients has an early role in resuscitation; however, EDT in pediatric patient remains controversial.
Case series reporting pediatric EDT survival rates range from 0 to 26% [5-12]. A recent meta analysis has compiled these studies and reported a significant survival advantage in patients who sustain penetrating versus blunt injury [6]. This is in agreement of the indications for EDT in adult patients, return of circulatory arrest following penetrating trauma is more favorable then blunt[13]. EDT performed in pediatric patients is infrequent [6] and as a result EDT case series are often small and some includes patients up to 18 years of age. Non-adult patients in the age range of 15-18 (adolescents) are arguably not pediatric patients[14] and add confusion to interpreting previously reported outcomes. Definitive recommendations regarding utility or futility of this procedure in non-adults trauma patients is highly problematic. By differentiating adolescent from pediatric trauma patients, we hypothesize that low EDT survival rate in younger patients is attributable to a higher rate of blunt trauma compared to their adolescent counterparts.
2. Methods
2.1 Patient Population
This prospective observations study includes continuously collected variables on all trauma patients presenting to our urban adult level one trauma center who underwent emergency department thoracotomy from January 1974 to December 2014 under approval of the Colorado Multiple Institution Review Board. The senior author (EEM) reviewed and verified all patient pre hospital characteristics and patient outcomes. Long-term neurologic outcome of survivors was determined by retrospective chart review.
2.2 Patient Selection
Trauma patients 18 years or younger were included in this analysis. Patients were dichotomized into pediatric (age <15) versus adolescent based on the American College of Surgeons criteria for pediatric patients. The categorization of adolescent patients was based off previously reported pediatric EDT series where patients up to the age of 18 were included in the analysis[6]
2.3 Patient Characteristics and Outcomes
Patient demographics included age and sex. Pre hospital variables included injury mechanism and anatomic location, in addition to detection of pre hospital cardiac activity by pre hospital healthcare provider, pre hospital cardio pulmonary resuscitation (CPR). Outcomes included success to rescue, defined as regain of spontaneous circulation and transfer of patient to operating room. Survival was assessed from the operating room and during hospitalization. Neurologic outcome were scored using the Glasgow Outcome Score (GOS)[15] which is a five category score ranging from death to good recovery.
2.4 Statistical Analysis
SPSS software version 22 (IBM, Armonk, NY) was used for statistical analysis. Categorical data was represented as percentage and contrasted between pediatric and adolescent patients. Continuous variable were described as median with 25th to 75th percentile range if data was not normally distributed and mean with standard deviation for normally distributed data. Differences in groups were contrasted using Pearson's Chi Square with five or more events per group, or Fishers Exact Tests if events were less than five. Significance was set to an alpha of 0.05. When comparing anatomic injury patterns due to multiple comparisons (five anatomic sites) a Bonferroni adjustment was used for a more conservative estimate and alpha was set to 0.01.
3. Results
3.1 Adult vs Non-Adult EDT
During the study period 1691 patients underwent EDT. 179 (10.6%) were 18 years old or younger. Overall survival in adults (age>18) was 6.1% versus 3.4% in younger patients (p=0.157). These adolescent/pediatric patients had a median age of 16 years with a range from 3 to 18 years. Penetrating injuries occurred in 56% of these patients and 78% were male. The majority of these patients were adolescent [n=125 (69.8%) versus n= 54 pediatric (30.2%)].
3.2 Adolescent vs Pediatric EDT
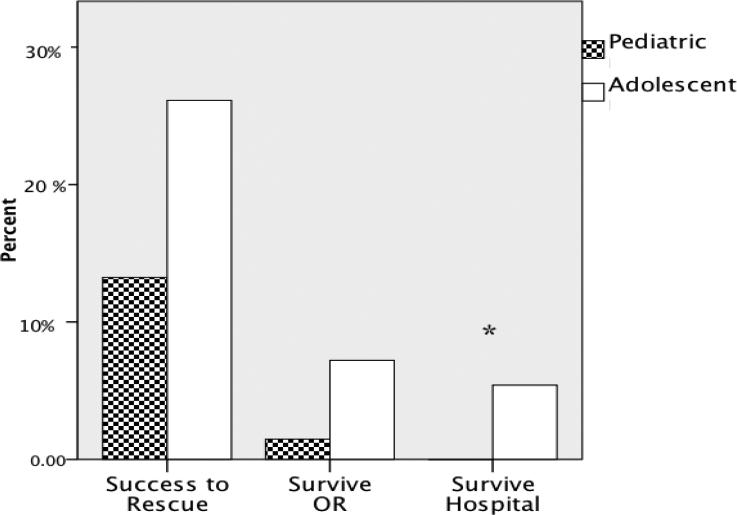
Pediatric patients were more likely to sustain blunt injury (72% vs 32% p<0.001). This also corresponded to differences in anatomic injury patterns (table 1) and more multisystem trauma (52% vs 44% p=0.001). Adolescent patients trended towards higher rate of success to rescue compared to pediatric patients (25% vs 13% p=0.075), although no significant difference was appreciated in patients that survived the operating room (5.6% vs 1.8% p=0.281). However overall survival was significantly higher in adolescent patients (4.8% vs 0% p=0.036 figure 1).
Table 1.
Injury Patterns in Pediatric vs Adolescent Patients
| Pediatric (n=54) | Adolescent (n=125) | P Value | |
|---|---|---|---|
| Head | 69% | 26% | P<0.001* |
| Neck | 33% | 18% | P=0.020 |
| Thoracic | 70% | 74% | P=0.576 |
| Abdominal | 50% | 46% | P=0.588 |
| Extremity | 39% | 20% | P=0.008* |
Figure 1.
Survival Patterns in Different Age Cohorts
3.3 Survivor Characteristics
The youngest survivor of EDT was 16 years old. Only one patient in this non-adult cohort survived a blunt injury mechanism. The specific injuries of these survivors are listed in table 2 along with their long-term neurologic outcome. All survivors had cardiac activity in the field, and 50% were undergoing pre hospital CPR, while the other half had circulatory arrest in the emergency department. The most common injury pattern that survived was a penetrating stab wound to the chest (table 3).
Table 2.
Survivor Characteristics
| Age (yr) | Mechanism | Injury Location | Field CPR | LOS | GOS | |
|---|---|---|---|---|---|---|
| 1 | 16 | Stabbing | Left Lung, Spleen, Brachial Artery | No | 7 | GR |
| 2 | 17 | Stabbing | Right Ventricle | No | 11 | PVS |
| 3 | 17 | Stabbing | Right Atrium | Yes | 7 | GR |
| 4 | 17 | Stabbing | Right Ventricle | No | 12 | MD |
| 5 | 17 | GSW | Left Pulmonary Hilum | Yes | 15 | GR |
| 6 | 18 | MVC | Bilateral Subdural Hematomas, Massive Left Hemothorax, Pelvic Fxr |
Yes | 19 | GR |
GSW= gun shot wound; MVC= motor vehicle crash; Fxr= Fracture; CPR= cardio pulmonary resuscitation ;LOS = length of stay; GOS = Glasgow Outcome Score; GR = good recovery; MD = moderate disability; PVS = persistent vegetative state;
Table 3.
Systems injured; blunt versus penetrating, survival (n = 61)
| Blunt | Penetrating | Survival | |
|---|---|---|---|
| CN3 | 0 | 0 | 0/0 |
| Chest/neck | 3 | 29 | 1/32 |
| Abdomen/pelvis | 0 | 7 | 1/7 |
| Extremity | 0 | 3 | 0/3 |
| Multiple | 4 | 15 | 0/19 |
| Survival | 0/7 | 2/54 | 2/61 |
Experience of Ryder Trauma Center 1991–2012.
4. Discussion
In a our groups 40 year experience of emergency department thoracotomy nearly one in ten patients undergoing this procedure is an adolescent or pediatric patient. These non-adult trauma patients have lower (but not significantly different) survival rates compared to their adult counter parts. The worse outcomes in this patient population may be attributable to injury mechanism and anatomic injury pattern. By stratifying pediatric patients from adolescent patients these discrepancies become apparent. There were six-time as many adolescent patients (n=85) with penetrating injuries compared to pediatrics (n=14). In addition pediatric patients more frequently had multisystem injuries compared to adolescent patients. In this relatively large case series there were no survivors in the pediatric age group.
The prevalence of adolescent/pediatric EDT in our study is comparable to the Ryder trauma center in Miami which has a similarly high acuity of adult and pediatric trauma patients[6]. However, the minority (30%) of these non-adult patients are less than 15 years old. During our four-decade experience, the rate of pediatric EDT was 1.3 per year. When evaluating the entire state of Illinois, this rate was only increased to 2.3 EDT per year[5]. Survival has repeatedly been demonstrated to be poor in this age group. There are several studies that report 0% survival[8, 12]. These small case series only include 17 and 9 patients respectively. More recently Nicolson et al[5] evaluated a 10 year experience of EDT in the state of Illinois on pediatric patients and reported 25 cases with 2 survivors who had penetrating chest injuries with the youngest being 13 years old. Injury patterns and mechanism appear to play a role in the poor outcomes of the pediatric patients. Nearly seventy percent of pediatrics patient in our study had head injuries. The combination of circulatory arrest and head injuries is associated with a poor prognosis[16] and is supported by animal work in which hypo perfusion markedly exacerbates progression in head injury and systemic coagulopathy[17].
Due to the infrequent occurrence of pediatric EDT, many previous studies include adolescent patients in their analysis[6, 7, 9, 11]. Adolescent patient more frequently undergo EDT per year compared to pediatric patients, which is also observed at the Ryder trauma center's 11 year experience[6]. Adolescent patients in our study had a significantly high incidence of penetrating injuries. It has been repeated demonstrated that penetrating chest injuries that undergo EDT have favorable outcomes[5, 7, 10, 11]. This would be anticipated, as the EDT provides direct access to relieve tamponade, enables cardiac massage, and clamping of the aorta to shunt blood to the brain and cardiopulmonary system. Powell et al[7] reported the highest survival rate of survival rate of non-adult EDT (26%), but was limited to 19 patient, and no survivors under the age of 15. There are only 2 single center case series with more than 50 patients, and they that have survival rates between 3 and 4%[6, 9], which is comparable to our overall and adolescent survival rates.
From the existing literature it could be argued that EDT for patients under the age of 15 is a futile procedure. However, with only 14 patients sustaining penetrating injuries in this age cohort over a 40 year period, there is not enough statistical power to come to this conclusion. Gunshot wounds to children in this age group are infrequent and often unintentional from family members[18]. An age limitation should not preclude a resuscitation attempt with an EDT for penetrating thoracic injuries. The adult and adolescent data, which occur at a higher frequency supports the life saving efficacy of this procedure[6, 16]. The causality for poor outcomes in pediatric patients can be partially attributable to a predominantly blunt poly-system trauma. However, due to the low frequency of this procedure in pediatric patients, defining futility remains a challenge. In the adult population the extremes of surviving this procedure have been defined with multicenter data[16]. These guidelines for penetrating trauma are most likely still applicable to adolescent and pediatric patients. The EDTs role in resuscitation is not only to address thoracic injuries, but to provide proximal hemorrhage control for abdominal injuries. For patients with poly-system trauma, a less invasive resuscitation strategy such as a resuscitative endovascular balloon occlusion (REBOA) may have a future application as it provides the same proximal hemorrhage control without opening the chest. REBOA has been introduced clinically in adult trauma patients[19] and the skill set to perform this resuscitative procedure can be learned in a relatively short period of time without prior endovascular training[20]. The minimally invasive nature of REBOA may also reduce the adverse risks to providers associated with EDT, which have been argued to not outweigh the survival benefit[21, 22].
Non-adult trauma patients undergoing EDT are more frequently performed in adolescent patients compared to pediatric patients. Adolescent patients had significantly more penetrating injuries with a survival rate of 4.8% compared to no survivors in the pediatric cohort. The role of EDT in blunt trauma in pediatric patients appears to have no survival benefit. However, because of the low frequency of penetrating injuries, EDT is still indicated in this patient population as other case series have reported survival in this age cohort with a penetrating mechanism.
Figure 2.
Resuscitation Success and Survival in Pediatric and Adolescent Patients Undergoing Emergency Department Thoracotomy
Figure 2 demonstrates different patterns of success to rescue patient from circulatory arrest, survival from the operating room, and surviving hospitalization between adolescent and pediatric patients.
Acknowledgments
This study was supported in part by National Institute of Health Grants: T32-GM008315 (NIGMS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–93. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Beall AC, Jr., Diethrich EB, Cooley DA, DeBakey ME. Surgical management of penetrating cardiovascular trauma. South Med J. 1967;60:698–704. doi: 10.1097/00007611-196707000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190:288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 4.Shafi S, Barnes SA, Rayan N, Kudyakov R, Foreman M, Cryer HG, Alam HB, Hoff W, Holcomb J. Compliance with recommended care at trauma centers: association with patient outcomes. J Am Coll Surg. 2014;219:189–98. doi: 10.1016/j.jamcollsurg.2014.04.005. 10.1016/j.jamcollsurg.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Nicolson NG, Schwulst S, Esposito TA, Crandall ML. Resuscitative thoracotomy for pediatric trauma in Illinois, 1999 to 2009. Am J Surg. 2015 doi: 10.1016/j.amjsurg.2015.05.007. 10.1016/j.amjsurg.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Allen CJ, Valle EJ, Thorson CM, Hogan AR, Perez EA, Namias N, Zakrison TL, Neville HL, Sola JE. Pediatric emergency department thoracotomy: a large case series and systematic review. J Pediatr Surg. 2015;50:177–81. doi: 10.1016/j.jpedsurg.2014.10.042. 10.1016/j.jpedsurg.2014.10.042. [DOI] [PubMed] [Google Scholar]
- 7.Powell RW, Gill EA, Jurkovich GJ, Ramenofsky ML. Resuscitative thoracotomy in children and adolescents. Am Surg. 1988;54:188–91. [PubMed] [Google Scholar]
- 8.Beaver BL, Colombani PM, Buck JR, Dudgeon DL, Bohrer SL, Haller JA., Jr. Efficacy of emergency room thoracotomy in pediatric trauma. J Pediatr Surg. 1987;22:19–23. doi: 10.1016/s0022-3468(87)80007-6. [DOI] [PubMed] [Google Scholar]
- 9.Rothenberg SS, Moore EE, Moore FA, Baxter BT, Moore JB, Cleveland HC. Emergency Department thoracotomy in children--a critical analysis. J Trauma. 1989;29:1322–5. doi: 10.1097/00005373-198910000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Hofbauer M, Hupfl M, Figl M, Hochtl-Lee L, Kdolsky R. Retrospective analysis of emergency room thoracotomy in pediatric severe trauma patients. Resuscitation. 2011;82:185–9. doi: 10.1016/j.resuscitation.2010.09.475. 10.1016/j.resuscitation.2010.09.475. [DOI] [PubMed] [Google Scholar]
- 11.Easter JS, Vinton DT, Haukoos JS. Emergent pediatric thoracotomy following traumatic arrest. Resuscitation. 2012;83:1521–4. doi: 10.1016/j.resuscitation.2012.05.024. 10.1016/j.resuscitation.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 12.Boatright DH, Byyny RL, Hopkins E, Bakes K, Hissett J, Tunson J, Easter JS, Sasson C, Vogel JA, Bensard D, Haukoos JS. Validation of rules to predict emergent surgical intervention in pediatric trauma patients. J Am Coll Surg. 2013;216:1094–102. 102, e1–6. doi: 10.1016/j.jamcollsurg.2013.02.013. 10.1016/j.jamcollsurg.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burlew CC, Moore EE, Moore FA, Coimbra R, McIntyre RC, Jr., Davis JW, Sperry J, Biffl WL. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012;73:1359–63. doi: 10.1097/TA.0b013e318270d2df. 10.1097/TA.0b013e318270d2df. [DOI] [PubMed] [Google Scholar]
- 14.Olson TA, Murray MJ, Rodriguez-Galindo C, Nicholson JC, Billmire DF, Krailo MD, Dang HM, Amatruda JF, Thornton CM, Arul GS, Stoneham SJ, Pashankar F, Stark D, Shaikh F, Gershenson DM, Covens A, Hurteau J, Stenning SP, Feldman DR, Grimison PS, Huddart RA, Sweeney C, Powles T, Lopes LF, Dos Santos Agular S, Chinnaswamy G, Khaleel S, Abouelnaga S, Hale JP, Frazier AL. Pediatric and Adolescent Extracranial Germ Cell Tumors: The Road to Collaboration. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2015;33:3018–28. doi: 10.1200/JCO.2014.60.5337. 10.1200/JCO.2014.60.5337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–85. doi: 10.1089/neu.1998.15.573. [DOI] [PubMed] [Google Scholar]
- 16.Moore EE, Knudson MM, Burlew CC, Inaba K, Dicker RA, Biffl WL, Malhotra AK, Schreiber MA, Browder TD, Coimbra R, Gonzalez EA, Meredith JW, Livingston DH, Kaups KL, Group WTAS Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011;70:334–9. doi: 10.1097/TA.0b013e3182077c35. 10.1097/TA.0b013e3182077c35. [DOI] [PubMed] [Google Scholar]
- 17.Sillesen M, Johansson PI, Rasmussen LS, Jin G, Jepsen CH, Imam AM, Hwabejire J, Lu J, Duggan M, Velmahos G, deMoya M, Alam HB. Platelet activation and dysfunction in a large-animal model of traumatic brain injury and hemorrhage. JTrauma Acute Ccre Surg. 2013;74:1252–9. doi: 10.1097/TA.0b013e31828c7a6b. 10.1097/TA.0b013e31828c7a6b. [DOI] [PubMed] [Google Scholar]
- 18.Senger C, Keijzer R, Smith G, Muensterer OJ. Pediatric firearm injuries: a 10-year single-center experience of 194 patients. J Pediatr Surg. 2011;46:927–32. doi: 10.1016/j.jpedsurg.2011.02.032. 10.1016/j.jpedsurg.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 19.Brenner ML, Moore LJ, DuBose JJ, Tyson GH, McNutt MK, Albarado RP, Holcomb JB, Scalea TM, Rasmussen TE. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg. 2013;75:506–11. doi: 10.1097/TA.0b013e31829e5416. 10.1097/TA.0b013e31829e5416. [DOI] [PubMed] [Google Scholar]
- 20.Brenner M, Hoehn M, Pasley J, Dubose J, Stein D, Scalea T. Basic endovascular skills for trauma course: bridging the gap between endovascular techniques and the acute care surgeon. J Trauma Acute Care Surg. 2014;77:286–91. doi: 10.1097/TA.0000000000000310. 10.1097/TA.0000000000000310. [DOI] [PubMed] [Google Scholar]
- 21.Esposito TJ, Jurkovich GJ, Rice CL, Maier RV, Copass MK, Ashbaugh DG. Reappraisal of emergency room thoracotomy in a changing environment. J Trauma. 1991;31:881–5. doi: 10.1097/00005373-199107000-00001. discussion 5-7. [DOI] [PubMed] [Google Scholar]
- 22.Brown SE, Gomez GA, Jacobson LE, Scherer T, 3rd, McMillan RA. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am Surg. 1996;62:530–3. discussion 3-4. [PubMed] [Google Scholar]