Abstract
Background
Optimal Matching Theory (OMT; [1]) posits that the effects of social support are enhanced when its provision is matched with need for support. We hypothesized that matching received social support with the needs of persons with cancer and cancer survivors would be related to better psychosocial adjustment than a mismatched condition.
Method
In a cross-sectional design, Sample 1, 171 cancer patients, and Sample 2, 118 cancer survivors, completed measures of emotional and instrumental received support, physical debilitation, and psychological distress.
Results
The OMT model was confirmed; those needing support (i.e., greater physical debilitation), who did not receive it, experienced more distress than those who needed support and received it. Patients in treatment benefited from the matching of need and provision for both emotional and instrumental support; whereas, survivors only benefited from the matching of emotional support.
Conclusions
The results suggest that social support is contextualized by the degree of physical impairment and may be somewhat different for cancer patients in treatment compared to cancer survivors. The transition to cancer survivorship may involve a transformation in the need for as well as the type and amount of received social support.
Keywords: social support, cancer, survivorship, distress, optimal matching theory
Research on social support has a long history of elucidating the positive effects of the perception and provision of social support [2,3,4,5,6,7]. Moreover, early work in social support operated under the assumption that both the provider and the receiver of support shared the same goals and had a mutual understanding of “support.” However, widespread recognition of the multidimensional nature of the construct with respect to dimensions like source [8], type [9], amount [10], and the personal relationship [11] has fostered interest in the failed attempts at social support and challenged the assumption that both the provider and the receiver of support share the same goals and gather the same meaning from an interpersonal interaction. Thus, there are data reinforcing the notion that social support may have deleterious effects if the goals of the provider and receiver are incongruent [12].
In the realm of support for cancer patients, Helgeson and colleagues [13] found that for those who already possess high levels of social support, a peer support group had somewhat negative effects. And, Reynolds and Perrin [14] showed that among breast cancer patients, misalignment of support between the provider and receiver of social support significantly influenced psychosocial adjustment, and unwanted but received support was uniquely associated with poor psychosocial adjustment. From a broader perspective, negative interpersonal interactions have been associated with the onset of psychological disorder [15,16], exacerbation of autoimmune disorders [17] and poor response to cancer treatment [18]. Such findings are integral to the body of research in this area because the negative effects of social support may be just as impactful, if not more so, than the positive effects of social support [19].
Along these lines, Cutrona [1] and Cutrona and Russell [20] developed Optimal Matching Theory (OMT) in which they posit that the benefits, and perhaps the deleterious effects of social support are due to the matching (or mismatching) of support in different contexts and situations. With respect to cancer, variations in stage at diagnosis, the efficacy of medical intervention, accompanying side effects, and individuals’ capacity for coping may result in varying needs for social support. According to Optimal Matching Theory [1,20], if the proper type of support is provided in a particular context there will be an enhancement of quality of life and adjustment to the disease and its treatments compared to a situation in which the need and the provision of support are mismatched.
In the process of investigating OMT, it is critical to distinguish perceived and received support. Perceived support has been defined as “the belief that help would be available if needed” whereas received support is defined as “help that is actually received” [7,21]. Though not framed in OMT, Carpenter, Fowler, Maxwell, and Andersen [22] reported results consistent with OMT. In that study of cancer survivors, a moderator effect did indicate that for low levels of physical symptomatology there were no differences between those reporting high and low levels of perceived support on self-reported stress; in contrast, for high levels of physical symptomatology those with low levels of perceived support reported greater stress than those reporting high levels of perceived support. Finally, the moderator effect was found for belonging support (i.e., the availability of emotional support) but not for tangible support (i.e., the availability of material help). Thus, this study [22] sets the stage for whether the moderator effect, predicted by OMT theory, would hold for received support, and whether instrumental received support (i.e., tangible support) and emotional received support operate differently between patients in treatment and cancer survivors. Consistent with OMT, though not framed in that theory, Lepore et al., [23] concluded that, “Received social support may be beneficial when it matches one's needs and desires” (p. 1213), and they recommended further investigation of the complex conditions involved in the relationship between received support and distress.
Based on OMT and the results of Reynolds and Perrin [14], Carpenter et al. [22] and Lepore et al. [23], we hypothesized that the matching of the need for received support and its provision will be associated with better adjustment of persons with cancer and cancer survivors than the mismatching of the need for and provision of received support. Moreover, we hypothesized that emotional and instrumental support would show this moderator effect for patients in treatment; however, based on Carpenter et al., [22] for survivors the moderation would only hold for emotional support because they are less physically impaired and, therefore, less in need of the coordination of instrumental support with physical debilitation than patients in treatment.
Method
Participants
Sample 1
A total of 375 questionnaires were distributed to patients in treatment; 162 people decided not to participate, or did not return all of the questionnaire materials. Thus, 213 adults chose to participate (134 women). The patients were all in active cancer treatment (for first time or recurrence) and ranged in age from 20 to 87 with mean of 59.34. About one-third were between 0 and 6 months post initial diagnosis, one third between 6 and 12 months, and one-third, a year or more. The majority of the sample were married (68.08%), identified themselves as Caucasian (90.14%) and Protestant (53.99%). Most patients completed high school and some college (56.33%) and 49.76% had household incomes of $25,000 and above. The sample included persons with mixed diagnoses with breast (29.58%), lymphoma (11.27%) and lung cancer (9.39%) as the most common. In terms of treatments, 55% had surgery, 68% had chemotherapy, and 46% had radiation.
Sample 2
A total of 300 questionnaire packets were mailed to individuals in a survivor research database or given to leaders of survivor support groups to distribute to their constituents; 157 were returned, however, 6 were returned either blank or partially completed. Thus, Sample 2 consisted of 151 adult cancer survivors (95 women), who ranged in age from 22 to 86 with mean of 62.95. The majority of the participants were married (66.89%), identified themselves as white or Caucasian (76.82%) and Protestant (47.02%). Most patients had completed high school and some college (55.63%) and had household incomes of $25,000 and above (58.95%). The sample included many cancer diagnoses with the majority of participants diagnosed with cancer of breast (43.05%) or prostate (17.88%). In terms of treatments, 83% had surgery, 65% had chemotherapy, and 65% had radiation. The median time post-diagnosis was 6 years. In both samples there were no significant relationships between race or time since diagnosis and the main variables in the study.
Measures
In addition to a form that contained demographic and disease related items, all participants completed the measures described below.
Physical Debilitation
The Sickness Impact Profile (SIP) is a measure of the impact of any disease or disability [24,25]. Of importance to this study are the 45 items from the physical impact dimension, which relates to the following categories of physical functioning: ambulation, mobility, and body care and movement. Participants merely checked items that apply to them. Items have weighted scale values that are summed, divided by the sum of all 45 weighted scale values, and multiplied by 100 to yield a percent score. The SIP correlates strongly with other self-assessment measures of dysfunction and with clinical ratings of sickness [26]. In this study, internal consistency of the 45 items that constitute the physical impact score was .87 for Sample 1 and .92 for Sample 2.
Received Social Support
To measure received social support, the 40-item Inventory of Socially Supportive Behaviors (ISSB) was used [27]. The ISSB includes a rating of the frequency with which each item has occurred in the last month using a 5-point Likert scale: 1, “not at all”; 2, “once or twice”; 3, “about once a week”; 4, “several times a week”; 5, “about every day”. The total score is calculated by adding frequency ratings together. Internal consistency (Cronbach's alpha) for the ISSB in this study was .91 for Sample 1 and .90 for Sample 2. The subscales [28] of the ISSB are Directive Guidance (DG), Tangible Assistance (TA), Positive Social Exchange (PSE), and Nondirective Support (NDS). Instrumental support consisted of the aggregation of the DG and TA scales (r =.82), and aggregating the PSE and NDS (r =.74) scales formed emotional support. A 21-item brief version of the ISSB [29] was used in Sample 2, which correlated very highly with the longer version. The correlation of the scales of the ISSB between the long version (Sample 1) and the brief version (Sample 2) were .90, .99, .96, and .96 for the PSE, NDS, DG, and TA scales, respectively.
Psychological Distress
The Psychosocial Adjustment to Illness Scale, Self-report form (PAIS-SR [30]) was used to assess adjustment to cancer. The PAIS is correlated with the Global Adjustment to Illness Scale (GAIS; [30]) (r = .81) and with the SCL-90-R, a measure of psychological symptomatic distress (r = .60). For the sake of reducing overlap among the constructs in the study, only the Psychological Distress (PAIS-PD) scale was used as the dependent variable. Internal consistency (α) for the PAIS-PD scale was .85 in both Samples 1 and 2. In terms of the validity of the PAIS-D in the current research, for Sample 2 the PAIS-D was highly correlated with the Center for Epidemiologic Studies-Depressed Mood Scale (r=.79); [31]) and the Distress Scale of the Distress Screening Schedule (r=.80; [32]).
Procedures
Sample 1
Questionnaires were distributed to patients at an oncology clinic during their regularly scheduled appointments. Participants with any cancer diagnosis had to be at least 18 years old, able to read English, and on active treatment. Those who chose not to participate returned the packet unanswered. Those who did participate completed a HIPAA-compliant release of information form that allowed access to the patients ‘medical chart for the purpose of collecting information about the disease such as tumor site, metastases, stage of illness, and treatments received. A research assistant was present to answer questions and address concerns. Participation took approximately 30 minutes and participants were paid $20.
Sample 2
Individuals were recruited as part of a grant-funded study, which included placing ads in newspapers in major cities, as well as contacting national support groups, church-based support groups, alumni associations of universities, physicians, and wellness organizations. Participants represented most geographical regions of the United States, except the northeast. Participants had to be 18 years old, able to read English, and off active treatment. Individuals who consented to participate received a packet of materials and were asked to complete each questionnaire and return the packet using the postage paid envelope, which was provided. The questionnaires took approximately 40 minutes to complete and participants were compensated $20 for their effort. Participants were also asked to complete a HIPAA-compliant medical release to enable access to medical records for information regarding the patient's disease status; 70% of physicians’ offices responded to this request. In addition, patients were asked to provide medical information such as diagnosis and types of treatments they have received. Thus, descriptive information was accumulated from both sources.
Results
Data Analysis and Preliminary Analyses
The moderation analyses reported below were based on Aiken and West's [33] regression approach in which an interaction term is formed by the product of the independent variable and the moderator variable, which is entered in the regression equation to assess its influence on the relation between the dependent variable and the independent variable. A significant interaction is then plotted (cf., [33]) to test specific hypotheses. In Sample 1 there were more people whose income was below $15,000 than in Sample 2, and concomitantly Sample 2 had more people whose education included advanced degrees. Also, there were more African Americans in Sample 2 compared to Sample 1. However, when controlling for education and income, there were no significant differences as a function of race on the other variables in the study. In the following moderated regression models, age, income, and education were entered as covariates.
Sample 1: Patients in Treatment
A moderated multiple regression model was used to test the moderator hypothesis. The model included a dependent variable (distress; PAIS-PD), an independent variable (physical debilitation; SIP Physical Impact), a moderator (received emotional and instrumental support; ISSB), an interaction term (physical debilitation ×received support) and three covariates (age, income, education). Of the 213 patients, 171 gave full responses to the variables included in the study. In dealing with missing data, there were no differences in the effects derived from the listwise deletion and multiple imputation approaches to the moderation analysis [34]; the listwise approach is reported. Ordinary least squares was used to estimate the parameters of the model [33,35].
Moderation analysis based on listwise deletion
Assumptions of normality and homoscedasticity for residuals were confirmed. The covariates (age, income and education) were centered before estimating the model. Overall, the greater the physical debilitation the greater the distress. The moderator results (Table 1) indicated that received support was a significant moderator of the relationship between physical debilitation and distress (p<0.001). The tests of subscales of the ISSB indicate that both emotional support (p=0.007) and instrumental support (p<0.001) were significant moderators. When emotional support was the moderator, the variance in distress explained by the predictors was 15.98% and 23.84% (calculation: Interaction R2/Model R2 from Table 1) of this was attributed to the moderating effect. When instrumental support is the moderator, the variance in distress explained by the predictors was 21.44% and 33.26% of this was attributed to the moderating effect.
Table 1.
Testing Optimal Matching Theory: Moderator analyses for patients in treatment (Sample 1) and survivors (Sample 2) in the prediction of psychological distress (PAIS-D)
| Sample 1 | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Moderator _→ | ISSB (total) | ISSB (emotional support) | ISSB (instrumental support) | ||||||
| Predictor ↓ | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p |
| Intercept | 1.140 | 1.263 | 0.368 | 2.474 | 1.443 | 0.088 | 1.811 | 1.031 | 0.081 |
| SIP | 0.170 | 0.040 | <0.001 | 0.163 | 0.048 | 0.001 | 0.144 | 0.033 | <0.001 |
| ISSB | 0.069 | 0.018 | <0.001 | 0.234 | 0.097 | 0.017 | 0.205 | 0.050 | <0.001 |
| ISSB×SIP | −0.002 | 0.0004 | <0.001 | −0.007 | 0.003 | 0.007 | −0.004 | 0.001 | <0.001 |
| Age | −0.071 | 0.025 | 0.006 | −0.081 | 0.026 | 0.002 | −0.070 | 0.025 | 0.006 |
| Income | 0.460 | 0.270 | 0.090 | 0.397 | 0.278 | 0.155 | 0.432 | 0.268 | 0.109 |
| Edu | −0.053 | 0.197 | 0.789 | −0.158 | 0.200 | 0.433 | −0.031 | 0.197 | 0.876 |
| Model R2 | 0.2068 | 0.1598 | 0.2144 | ||||||
| Interaction ΔR2 | 0.0680 | 0.0381 | 0.0713 | ||||||
| Sample 2 | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Moderator _→ | ISSB (total) | ISSB (emotional support) | ISSB (instrumental support) | ||||||
| Predictor ↓ | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p |
| Intercept | 2.729 | 0.759 | <0.001 | 3.180 | 0.632 | <0.001 | 2.394 | 0.725 | 0.001 |
| SIP | 1.639 | 0.485 | 0.001 | 1.727 | 0.382 | <0.001 | 1.146 | 0.503 | 0.025 |
| ISSB | 0.004 | 0.014 | 0.800 | −0.017 | 0.047 | 0.717 | 0.036 | 0.051 | 0.481 |
| ISSB×SIP | −0.015 | 0.010 | 0.143 | −0.081 | 0.034 | 0.020 | −0.010 | 0.039 | 0.790 |
| Age | −0.038 | 0.017 | 0.030 | −0.031 | 0.017 | 0.066 | −0.038 | 0.017 | 0.032 |
| Income | 0.004 | 0.117 | 0.975 | 0.029 | 0.114 | 0.796 | 0.002 | 0.118 | 0.986 |
| Edu | −0.089 | 0.144 | 0.538 | −0.100 | 0.140 | 0.478 | −0.081 | 0.145 | 0.577 |
| Model R2 | 0.2696 | 0.3090 | 0.2562 | ||||||
| Interaction ΔR2 | 0.0140 | 0.0341 | 0.0005 | ||||||
| AIC | 528.344 | 521.693 | 530.529 | ||||||
Note: SIP=Phy sical Impact - ambulation, mobility, and body care and movement scales from the Sickness Impact Profile; ISSB=Received support, Inventory of Socially Supportive Behaviors; ISSB-Emotional=Received emotional support; ISSB-Instrumental=Received Instrumental Support.
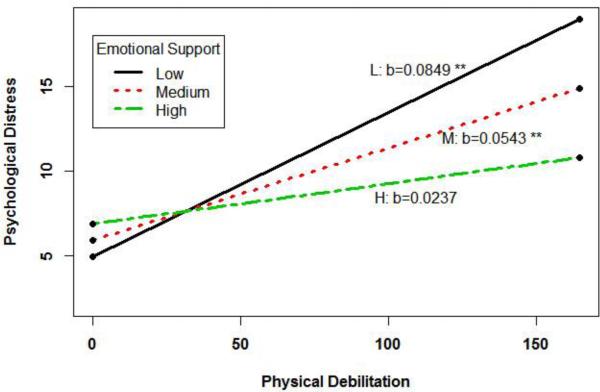
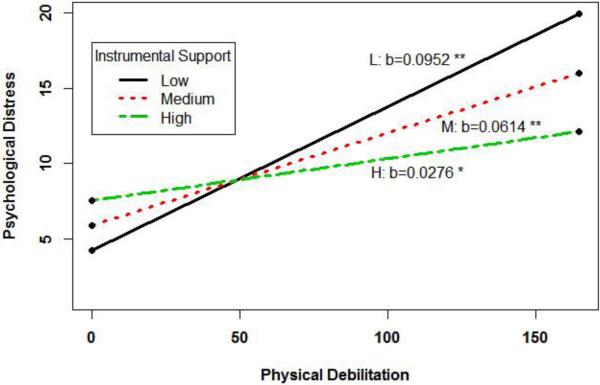
Figures 1 and 2 depict the interaction plots represented at three levels: low (one SD below the mean), moderate (the mean), and high (one SD above the mean). These figures reveal that consistent with OMT, the mismatched conditions, that is patients who were low in sickness impact but received high received/emotional/instrumental support and those who were high in sickness impact but received low received/emotional/instrumental support, had greater distress than the matched conditions. In all instances slope analyses indicated that the moderator effects were primarily driven by low levels of received support and were more dramatic at high levels of physical debilitation.
Figure 1.
Sample 1 – Patients in Treatment: Moderating effect of received emotional support on the relation between distressand physical debilitation
Figure 2.
Sample 1 – Patients in Treatment: Moderating effect of received instrumental support on the relation between distress and physical debilitation
Sample 2: Cancer Survivors
In Sample 2, as in Sample 1, the model included a dependent variable (distress: PAIS-PD), an independent variable (physical debilitation; SIP Physical Impact), a moderator (received emotional and instrumental support; ISSB), an interaction term (physical debilitation received support) and three covariates (age, income, education). As in Sample 1, greater distress is associated with higher levels of debilitation. Regression analyses comparing listwise deletion and multiple imputation for handling missing data resulted in the same significant effects; listwise deletion effects are reported. When examining the data, we found that the independent variable had severe skewness based on the fact that survivors were less impaired (i.e., lower physical impact scores) than patients in treatment. Thus, a log transformation was used on the measure of physical debilitation. The transformation was obtained by log(SIP+1) and is denoted as logSIP in the regression analysis.
After transformation, the normality assumption for residuals was met for the regression models. Furthermore, R2 increased for all three models and AIC goodness-of-fit improved over the models tested without the transformation. Thus, the interpretations were based on model fitting with the transformed data. As indicated in Table 1 (bottom half), total received support was not a significant moderator of the relationship between physical debilitation and distress (p=0.143). The tests of subscales of the ISSB indicate that emotional support was a significant moderator (p=0.020), whereas instrumental support was not (p=0.790). When emotional support was the moderator, the variance in distress explained by the predictors was 30.90% and 11.06% (calculation: Interaction R2 / Model R2 from bottom of Table 1) of this was attributed to the moderating effect.
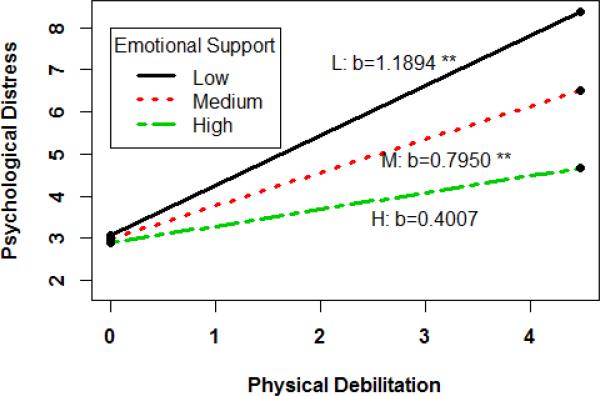
Figure 3 depicts the interactions plot for emotional support. The figure reveals that survivors who received lower emotional support always had greater distress than those who received higher emotional support. However, the difference in distress as a function of amount of received support was much smaller at low levels of physical debilitation than at high levels of physical debilitation. As in Sample 1, slope analyses indicated that the moderator effects were primarily driven by low levels of received support and were more dramatic at high levels of physical debilitation. Finally, the correlation between distress (PAIS-D) and received support (ISSB-Total) was positive in Sample 1 (r=.28; p<.01) but was negative in Sample 2 (r=−.20;p<.05).
Figure 3.
Sample 2 – Cancer Survivors: Moderating effect of emotional support on the relation between distress and physical debilitation (logSIP)
Conclusions
In general, results suggest that patients and survivors who were more physically debilitated had higher levels of distress. However, the relation between physical debilitation and distress was moderated by received support. Consistent with Optimal Matching Theory and recent findings based on or consistent with that theory [9,10,11,22,23], the results generally indicated that the matching of the need for received support and its provision optimizes the adjustment of persons with cancer. More specifically, results suggest that those patients in treatment who needed received support, both emotional and instrumental, and did not receive it, fared more poorly than those who needed it and received it. Also suggested in the results was the converse; those who did not need received support (i.e., low in disease impact) but received it fared more poorly than those who were low in disease impact and did not receive high levels of received support. It is also abundantly clear that the moderating effects are much more dramatic at high levels rather than at low levels of physical debilitation. Thus, the effects of matching (or mismatching) need and provision could have much more severe consequences with respect to distress at high levels of physical debilitation.These findings are consistent with those of Carpenter et al. [22].
The findings also indicated that the role of received support may differ between those in treatment and survivors, which was suggested by Philip et al. [36]. The comparative results suggest that coordination of physical debilitation and instrumental support is critical during the treatment phase when side-effects and symptoms are likely to be more disruptive than in the survivor phase when the impact of the disease and treatments is reduced. For survivors, these results roughly parallel the findings of Carpenter et al. [22] who found that for cancer survivors belonging support did moderate the relationship between physical debilitation and stress but tangible support did not. However, unlike those in treatment for survivors there was no matching or mismatching at low levels of physical debilitation only at high levels. Finally, consistent with Philip et al. [36], who suggested that the transition to survivorship may involve a change in the relationship of psychosocial resources to outcomes, the difference in valence of the correlation between distress and received support for those in treatment (Sample 1) and post-treatment (Sample 2) may signal shift in support in survivorship. However, longitudinal investigations would be needed to unambiguously study this phenomenon.
Generally, the findings indicate that the mere provision of support does not portend positive outcomes in all instances; in the mismatch conditions there may be attending processes that are not optimal for the person with cancer or cancer survivors. For example, in the situation where there is little impairment, the provision of high levels of received support is related to less effective adjustment than with the provision of low levels of received support. While it is speculative and the effects of matching are less dramatic at low levels of physical debilitation, these results may indicate that the provision of received support, when it is not needed, may foster the adoption of a “sick role” or a “helpless role” on the part of the person in cancer treatment [37] or impact self-esteem [23]
The limitations of this study include the cross-sectional design, which restricts the directional argument for the moderator model. The assumption in the model is that from physical debilitation arises the need for support, whereas, given the cross-sectional design, it may plausibly argued that distress accounts for the need for support. Thus, though the current study is consistent with the self-esteem model proposed by Lepore et al., [23] longitudinal studies could provide temporal confirmation of the OMT model. Future research efforts should focus in more depth on the contrasting needs of those with an initial/first diagnosis, those with recurrent disease, and those who are survivors as well as on the complexities of, among other things, different diagnoses, types of treatment, and personality. These fine-grained analyses of social support would lead to specific, and perhaps individualized and contextualized interpretations of the effects of social support for both patients in treatment and survivors.
The clinical implications of these data are consistent with Lepore et al. [23] in their emphasis on promoting open dialogue between support providers and support receivers about what is and is not helpful in the context of cancer treatment and survivorship. Also, it is important for the support receiver to give feedback to the provider about the need and appropriateness of the support offered. Moreover, there may be instances in which a support provider may refuse to provide support or modify the provision of support so as to not undermine the adjustment of the person with cancer. Thus, interventions based on this study would include improving communication between support providers and support receivers.
In sum, the studies reported provide confirmation of the utility of OMT in the context of cancer and cancer survivorship. The results also suggest that there is a need for future studies to refine the transition from active treatment to survivorship with the respect to the dynamics of the need and provision of social support.
Acknowledgments
This research was supported by a grant from the National Cancer Institute (CA94914). The authors would like to thank the patients and survivors from around the country, who participated in this study as well as the physicians and staff of Michiana Hematology-Oncology and the Northern Indiana Cancer Research Consortium, South Bend, Indiana.
Footnotes
Complete information on participants, as well as means, standard deviations, intercorrelations, residual diagnostics, and slope analyses are available from the first author.
Conflict of Interest and Compliance with Ethical Standards: The authors had no conflict of interest in the conduct of this research. All participants gave their informed consent before participating and all information gathered was handled in accordance with HIPAA regulations and the ethical standards of the American Psychological Association. This research was conducted with IRB approval.
Contributor Information
Thomas V. Merluzzi, Department of Psychology, University of Notre Dame
Errol J. Philip, Department of Psychiatry and Behavioral Sciences, Memorial Sloan-Kettering Cancer Center
Miao Yang, Department of Psychology, University of Notre Dame.
Carolyn A. Heitzmann, Counseling Services, University of Southern California
References
- 1.Cutrona CE. Stress and social support: In search of optimal matching. Journal of Social and Clinical Psychology. 1990;9:3–14. [Google Scholar]
- 2.Cohen S, Syme S. Issues in the study and application of social support. In: Cohen S, Syme S, editors. Social support and health. Academic Press; New York: 1985. [Google Scholar]
- 3.House JS, Umberson D, Landis KR. Structures and processes of social support. Annual Review of Sociology. 1998;14:293–318. [Google Scholar]
- 4.Lett HS, Blumenthal JA, Babyak MA, et al. Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychology. 2007;26:418–427. doi: 10.1037/0278-6133.26.4.418. [DOI] [PubMed] [Google Scholar]
- 5.Pierce GR, Sarason BR, Sarason IG. Integrating social support perspectives: Working models, personal relationships, and situational factors. In: Duck S, Silver R, editors. Personal relationships and social support. Sage; Newbury Park, CA: 1990. pp. 173–189. [Google Scholar]
- 6.Wills TA, Shinar O. Measuring perceived and received support. In: Cohen S, Underwood IG, Gottlieb BH, editors. Social support measurement and intervention: A guide for health and social scientists. Oxford University Press; New York: 2000. pp. 86–135. [Google Scholar]
- 7.Uchino B. Social Support and Physical Health: Understanding the Health Consequences of Relationships. Yale University Press; New Haven, CT: 2004. [Google Scholar]
- 8.Osman A, Lamis DA, Freedenthal S, Gutierrez P, McNaughton-Cassill M. The Multidimensional Scale of Perceived Social Support: Analyses of internal reliability, measurement Invariance, and correlates across gender. Journal of Personality Assessment. 2014;96(1):103–112. doi: 10.1080/00223891.2013.838170. DOI: 10.1080/00223891.2013.838170. [DOI] [PubMed] [Google Scholar]
- 9.Wright KB, Rains SA. Weak-tie support network preference, health-related stigma, and health outcomes in computer mediated support groups. Journal of Applied Communication Research. 2013;41:309–324. [Google Scholar]
- 10.Bar-Kalifa E, Rafaeli E. Disappointment's sting is greater than help's balm: Quasi-signal detection of daily support matching. Journal of Family Psychology. 2013;27:956–967. doi: 10.1037/a0034905. DOI: 10.1037/a0034905. [DOI] [PubMed] [Google Scholar]
- 11.Robinson JD, Tian Y. Cancer patients and the provision of informational social support. Health Communication. 2009;24:381–390. doi: 10.1080/10410230903023261. DOI:10.1080/10410230903023261. [DOI] [PubMed] [Google Scholar]
- 12.Horowitz LM, Krasnoperova EN, Tartar DG, Hansen MB, Person EA, Galvin KL, Nelson KL. The way to console may depend on the goal: Experimental studies of social support. Journal of Experimental Social Psychology. 2001;37:49–61. [Google Scholar]
- 13.Helgeson VS, Cohen S, Schulz R, Yasko J. Group support interventions for women with breast cancer: Who benefits from what? Health Psychology. 2000;19:107–114. doi: 10.1037//0278-6133.19.2.107. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds JS, Perrin NA. Mismatches in social support and psychosocial adjustment to breast cancer. Health Psychology. 2004;23(4):425–430. doi: 10.1037/0278-6133.23.4.425. [DOI] [PubMed] [Google Scholar]
- 15.Holeva V, Tarrier N, Wells A. Prevalence and predictors of acute stress disorder and PTSD following road traffic accidents: Thought control strategies and social support. Behavior Therapy. 2001;32:65–83. [Google Scholar]
- 16.Steketee G, Chambless DL. Does expressed emotion predict behavior therapy outcome at follow-up for obsessive-compulsive disorder and agoraphobia. Clinical Psychology & Psychotherapy. 2001;3:220–229. [Google Scholar]
- 17.Manne SL, Zautra AJ. Spouse criticism and support: Their association with coping and psychological adjustment among women with rheumatoid arthritis. Journal of Personality and Social Psychology. 1989;56(4):608–617. doi: 10.1037//0022-3514.56.4.608. [DOI] [PubMed] [Google Scholar]
- 18.Tarrier N, Sommerfield C, Pilgrim H. Relatives’ expressed emotion (EE) and PTSD treatment outcome. Psychological Medicine. 1999;29:801–811. doi: 10.1017/s0033291799008569. [DOI] [PubMed] [Google Scholar]
- 19.Figueiredo MI, Fries E, Ingram KM. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psycho-oncology. 2004;13:96–105. doi: 10.1002/pon.717. [DOI] [PubMed] [Google Scholar]
- 20.Cutrona C, Russell D. Type of social support and specific stress: Toward a theory of optimal matching. In: Sarason B, Sarason I, Pierce G, editors. Social support: An interactional view. Wiley; New York: 1990. 1990. pp. 319–366. [Google Scholar]
- 21.Uchino BN, Carlisle MC, Birmingham W, Vaughn AA. Social support and the reactivity hypothesis: Conceptual issues in examining the efficacy of received support during acute psychological Stress. Biological Psychology. 2001;86:137–142. doi: 10.1016/j.biopsycho.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carpenter KM, Fowler JM, Maxwell GL, Andersen BL. Direct and bufferning effects of social support among gynecologic cancer survivors. Annals of Behavioral Medicine. 2010;39:79–90. doi: 10.1007/s12160-010-9160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lepore SJ, Glaser DB, Roberts K. On the positive relations between received social support and negative affect: A test of the triage and self-esteem threat models in women with breast cancer. Psycho-oncology. 2008;17:1210–1215. doi: 10.1002/pon.1347. [DOI] [PubMed] [Google Scholar]
- 24.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: Development and final revision of a health status measure. Medical Care. 1981;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Bergner M, Bobbitt RA, Pollard WE, Martin BP, Gilson BS. The Sickness Impact Profile: Validation of a health status measure. Medical Care. 1976;14(1):57–67. doi: 10.1097/00005650-197601000-00006. [DOI] [PubMed] [Google Scholar]
- 26.vanBaalen B, Odding E, vanWoensel MP, Roebroeck ME. Reliability and sensitivity to change of measurement instruments used in a traumatic brain injury population. Clinical Rehabilitation. 2006;20:686–700. doi: 10.1191/0269215506cre982oa. [DOI] [PubMed] [Google Scholar]
- 27.Barrera M, Sandler IN, Ramsay TB. Preliminary development of a scale of social support: Studies on college students. American Journal of Community Psychology. 1981;9(4):435–447. [Google Scholar]
- 28.Finch JF, Barrera M, Jr., Okun MA, Bryant WHM, Pool GJ, Snow-Turek AL. Factor structure of received social support: Dimensionality and the prediction of depression and life satisfaction. Journal of Social and Clinical Psychology. 1997;16:323–342. [Google Scholar]
- 29.Merluzzi TV, Heitzmann CA. Society of Behavioral Medicine. San Francisco: 2006. Matching of the need for social support and its actual provision optimizes adjustment to cancer. [Google Scholar]
- 30.Derogatis LR, Derogatis MF. The Psychosocial Adjustment to Illness Scale (PAIS & PAIS-SR): Administration, scoring & procedures manual II. Clinical Psychometric Research; Towson, Maryland: 1990. [Google Scholar]
- 31.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 32.Merluzzi TV, Philip EJ, Heitzmann CA. Development and validation of the Distress Screening Schedule. University of Notre Dame, Laboratory for Psycho-oncology Research; 2014. Working paper. [Google Scholar]
- 33.Aiken L, West S. Multiple regression: testing and interpreting interactions. Sage Publications; Thousand Oaks, CA, US: 1991. [Google Scholar]
- 34.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- 35.Aguinis H. Regression analysis for categorical moderators. Guilford; New York: 2004. [Google Scholar]
- 36.Philip EJ, Merluzzi TV, Zhang Z, Heitzmann CA. Depression and cancer survivorship: Importance of coping self-efficacy in post-treatment survivors. Psycho-Oncology. 2013;22:987–994. doi: 10.1002/pon.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parsons T. Action theory and the human condition. Free Press; New York: 1975. [Google Scholar]