Abstract
Background
Diabetes mellitus (DM) appears to be a global epidemic and an increasingly major non-communicable disease threatening both affluent and non-affluent society. The study aimed to determine the knowledge of diabetic complications among diabetes mellitus clients visiting the Diabetic Clinical at Sampa Government Hospital, Ghana.
Method
This questionnaire-based descriptive study recruited a total 630 patients visiting the Diabetes Clinic at the Sampa Government Hospital. Structured questionnaire was used to obtain information such as socio-demographic and knowledge on complications of diabetes.
Results
Out of a total of 630 participants, 325 (51.5 %) knew diabetic foot as the most common complication followed by hypertension 223(35.4 %), neuropathy 184 (29.2 %), hypoactive sexual arousal 160(25.4 %), arousal disorder 135(21.5 %), eye diseases 112(17.7 %), heart disease 58(9.2 %), and renal disease 34(5.4 %). Comprehensive assessment of level of knowledge on the complications showed that majority 378(60.0 %) of T2D patients did not have knowledge on diabetes complications, 169(26.9 %) had inadequate knowledge on diabetics complication while 82(13.1 %) had adequate knowledge. The risk factors associated with the level of knowledge of diabetic complications were female gender adjusted odd ratio (AOR) =2.31 (1.56–3.41) married participants AOR = 3.37 (1.44–7.93), widowed AOR = 2.98 (1.10–8.08), basic level of education AOR =0.18 (0.082–0.50), Junior High School (JHS) and above of education level AOR = 0.035(0.017–0.75), 5–9 years of T2D duration AOR = 0.31(0.018–0.57), ≥10 years T2D duration AOR = 0.042 (0.02–0.10) and urban dwellers AOR = 0.36 (0.22–0.68) respectively.
Conclusion
Participants knew the individual complication of diabetic mellitus but lack an in-depth knowledge on the complications. Further expansion of diabetic educative programs like using mass media and involving national curriculum of education can improve self-regulatory awareness of diabetic complications which may reduce the morbidity and mortality of diabetic patients.
Electronic supplementary material
The online version of this article (doi:10.1186/s12889-016-3311-7) contains supplementary material, which is available to authorized users.
Keywords: Diabetic complication, Knowledge, Type 2 diabetics
Background
Diabetes mellitus (DM) appears to be a global epidemic and increasingly a major non-communicable disease threatening both affluent and non-affluent society [1, 2]. More than 170 million people worldwide have diabetes, and this figure is projected to more than double by the year 2030, if the current trend is allowed to continue further [3]. The potential severity of increasing prevalence rate of diabetes on the African continent may be translated into severe economic burden, high morbidity and mortality rates that will surpass the ravages [4]. Diabetes prevalence studies in southern Ghana have recorded a steady increase. The earliest studies in the 1960s recorded 0.2 % prevalence in a population of Ghanaian men in Ho [5]. The crude prevalence of diabetes in general population was 6.3 % in the late 1990s in Accra, Ghana and the age adjusted prevalence of diabetes and impaired glucose tolerance (IGT) were 6.1 and 10.7 % respectively [6]. Individual diagnosed with diabetes tend to have an increased risk of stroke and heart diseases compared to the general population and increased incidence of retinopathy, peripheral nerve damage and renal problems [7].
Adequate knowledge of diabetes is a key component of diabetic care. Many studies have shown that increasing patient knowledge regarding disease and its complications have significant benefits with regard to patient compliance to treatment and to decreasing complications associated with disease [8]. Some research have been done into the knowledge and management including health education of the disease [9–13] but the prevalence of the disease still keeps rising in Ghana [14]. In spite of these researches and health education done on diabetes, most Ghanaians are still less knowledgeable about the complications associated with the disease according to the international Diabetes Federation report [15]. There is no published data with regards to the knowledge of diabetic complications in the Sampa district, Ghana. It was against this background that we determine the level of knowledge of diabetes mellitus complications among diabetics visiting the diabetic clinic at the Sampa Government Hospital, Ghana.
Methods
Study Design/Setting
An exploratory and descriptive study design was used to determine the knowledge on the complications of diabetes mellitus among diabetic patients visiting the diabetic clinic at Sampa Government Hospital from February to April 2015. Sampa is the district capital of Jaman North shares local boundaries with Tain District to the north-east, Jaman South District to the south and Berekum District to the south-east. The Jaman North has a total population of 83, 059 out of which Sampa account for a total population of 26,909 and has a total land area of 502 square km (Ghana statistical service, 2012). The Sampa Government Hospital is the only district hospital which serves the health needs of the residents and nationals from adjoining towns of neighboring La Cote D’Ivoire. The hospital currently has about 156 staffs comprising of one doctor who is the medical superintendent of the hospital, four medical assistants, one pharmacist, four midwives and 20 nurses. Playing a significant role in rendering a proximal service to clients, the facility has an Out Patient Department Laboratory services, Scan, Eye Clinic, ENT services, Public Health Services, Maternity Department, Theatre and a Diabetes Clinic which was started last year and managed by one medical assistant, two staff nurses and a nutritionist, accessed by diabetics on only Wednesdays. Annually, the hospital has an average attendance of 35,002 out of which 943 cases are diagnosed of diabetes.
Study Population/Subject selection
Non-probability sampling technique was used to recruit six hundred and thirty (630) Type 2 Diabetic (T2DM) patients visiting the diabetic clinic. Structured questionnaires were used to obtain information from all study respondents. Structured questionnaire was based on the review of related journals [16–18]. The pre-test or pilot study was conducted among twenty (20) diabetics to ascertain the contents and clarity of the questionnaire. The questions were asked based on one-on-one interview with patients. Reliability coefficients ranging from 0.00 to 1.00, with higher coefficients indicating higher levels of reliability was used to determine the validity and the reliability of the questionnaire. The reliability coefficients for all the questions were 0.903. The entire questionnaire was available in English version but interviewed carefully with the proper translation of the official local language of the study population. The responses of the participants were translated back to English in the correct meaning as was interpreted. The structured questionnaire was divided into two sections with close-ended questions. Section A: involved questions that elicited information on socio-demographic variables of the patients such as age, gender, educational status, work pattern, family history of diabetes mellitus, duration of diabetes mellitus in the individual, treatment, dietary pattern, presence of any complications. Section B: included questions which assessed their knowledge on complications of diabetes mellitus and the kind of complications they know.
Inclusion criteria
Type 2 diabetes patients who were not dumb or deaf, had no disabilities and had visited the hospital during the study period were included in the study.
Exclusion criteria
Participants with type 1 diabetes, those who did not give consent as well as those with type 2 diabetes who were dumb or deaf were excluded.
Knowledge of diabetes mellitus
Participant were said to have “adequate” knowledge of complication of Type 2 diabetes if they responded to at least three correct answers with a percentage score of 75–100 %; “inadequate “knowledge if they responded to at most one correct answer with a percentage score of <50 % and “no” knowledge (Don’t Know) if they did not know anything about the complications of diabetes (0 %).
Data analysis
The data entry and analysis were performed using IBM statistical package for social science (SPSS) version 20. Descriptive statistics such as frequencies, percentage and charts were used. Chi-square or Fischer’s exact test statistical methods were used as appropriate to test association between categorical variables. Multivariable logistic regression analysis, adjusting for age and duration T2D was performed to predict factors associated with knowledge of diabetic complication. P value less than 0.05 was considered statistically significant difference.
Results
Socio-demographics characteristics of participants
Table 1 shows a total of 630 T2D patients were enrolled. The mean age of the general type 2 diabetic (T2D) patients in this study was 55.28 ± 14.71 years. A higher proportion (46.9 %) of them was between the ages of 40–59 years. Among the T2D subjects, there were more female (61.5 %) than male (38.5 %). Four hundred and sixty-five (465) representing 73.8 % were married. Out of a total of 630 subjects, 615 (97.7 %) had no socio-economic income, 495 (78.5 %) were unschooled, 383 (60.8 %) were Akans, 450 (71.5 %) had less than 5 years duration of T2D, while 344 (54.6 %) were from rural residency [Table 1].
Table 1.
General Characteristic of Type 2 diabetic patients
| Variables | Frequency | % Prevalence |
|---|---|---|
| Age (years) Mean ± SD | 55.28 ± 14.71 | |
| Age group | ||
| <19 | 5 | 0.8 % |
| 20–39 | 92 | 14.6 % |
| 40–59 | 295 | 46.9 % |
| 60–79 | 194 | 30.8 % |
| 80–99 | 44 | 6.9 % |
| Gender | ||
| Male | 243 | 38.5 % |
| Female | 387 | 61.5 % |
| Marital status | ||
| Single | 54 | 8.5 % |
| Married | 465 | 73.8 % |
| Widowed | 111 | 17.7 % |
| Economic income | ||
| None | 615 | 97.7 % |
| <500 (low) | 5 | 0.8 % |
| 500–1000 (medium) | 5 | 0.8 % |
| >1000 | 5 | 0.8 % |
| Highest level of education | ||
| None | 495 | 78.5 % |
| Basic | 43 | 6.9 % |
| JHS | 58 | 9.2 % |
| SHS | 24 | 3.8 % |
| Tertiary | 10 | 1.5 % |
| Ethnicity | ||
| Akan | 383 | 60.8 % |
| Mole-Dagbani | 247 | 39.2 % |
| Duration of diabetes (years) | ||
| <5 | 450 | 71.5 % |
| 5–10 | 126 | 20.0 % |
| 11–15 | 39 | 6.2 % |
| 16–20 | 15 | 2.3 % |
| Area of residence | ||
| Rural | 344 | 54.6 % |
| Urban | 286 | 45.4 % |
SD Standard deviation
Knowledge of diabetic mellitus complications
Table 2 shows the proportion of participants’ response on the knowledge on diabetic complications. The most common diabetic complication known by diabetic patients was diabetic foot (51.5 %), followed by hypertension (35.4 %), neuropathy (29.2 %), hypoactive sexual arousal (25.4 %), arousal disorder (21.5 %), retinopathy (17.7 %), heart disease (9.2 %), and nephropathy (5.4 %) In general higher proportions of them were not knowledgeable on diabetic complications. Out of 630 patients surveyed, 606 (96.2 %) had no knowledge on sexual pain disorder, 528 (83.8 %) had no knowledge on heart disease, 450 (71.5 %) had no knowledge on nephropathy, neuropathy 427 (67.7 %), arousal disorder 422 (66.9 %), retinopathy 412 (65.4 %), hypoactive sexual arousal 412 (65.4 %) and diabetic foot 296 (46.9 %) [Table 2].
Table 2.
Response of T2D participants on the complication of diabetes
| Complications | Participants responses | ||
|---|---|---|---|
| Yes | No | Don’t Know | |
| Hypertension | 223 (35.4 %) | 15 (2.3 %) | 392 (62.3 %) |
| Heart Disease | 58 (9.2 %) | 44 (6.9 %) | 528 (83.8 %) |
| Hypoactive sexual arousal | 160 (25.4 %) | 58 (9.2 %) | 412 (65.4 %) |
| Arousal disorder | 135 (21.5 %) | 73 (11.5 %) | 422 (66.9 %) |
| Sexual Pain disorder | 0 | 24(3.8 %) | 606 (96.2 %) |
| Retinopathy (Eye disease) | 112(17.7 %) | 106 (16.9 %) | 412 (65.4 %) |
| Nephropathy | 34 (5.4 %) | 146 (23.1 %) | 450 (71.5 %) |
| Diabetic Foot | 325 (51.5 %) | 9 (1.5 %) | 296 (46.9 %) |
| Neuropathy | 184(29.2 %) | 19(3.1 %) | 427 (67.7 %) |
Values are presented as N (%): frequency (percentage)
Level of knowledge of diabetic mellitus complications
Figure 1 shows levels of knowledge of complication of Type 2 Diabetes In general majority 378 (60.0 %) of T2D patients did not have knowledge on diabetes complications. One hundred and sixty-nine (169) of them representing 26.9 % had inadequate knowledge on diabetics complication while a few of them 82(13.1 %) had adequate knowledge [Fig. 1].
Fig. 1.
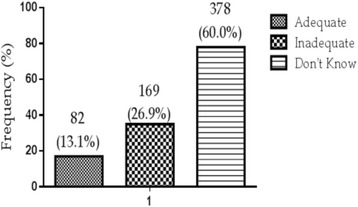
Overall knowledge score on complications of type 2 diabetes among diabetic patients
Association between levels of knowledge of diabetic mellitus complication and socio-demographic characteristics
Table 3 shows the association between age groups, gender, marital status, socioeconomic income, and duration of T2D, individual area of residency and level of understanding of diabetic complication. All patients 19 years and below knew nothing about diabetic complication. Higher proportion (22.2 %) of the elderly (80–99 year) had adequate knowledge on diabetic complications than 20–39 year (15.8 %), 40–59 year (13.1 %), and 60–79 (10.0 %). Age was not significantly associated with patient’s level of understanding of diabetic complications (p = 0.8198).
Table 3.
Shows the association between age groups, gender, marital status, socioeconomic income, duration of T2D, individual area of residency and degree of understanding of diabetic complication
| Variables | Level of understanding for diabetic complications | ||||
|---|---|---|---|---|---|
| Total | Adequate (n = 82) | Inadequate (n = 170) | Don’t Know(n = 378) | P-value (X2, df) | |
| Age group (years) | |||||
| <19 | 5 | – | – | 5 (100.0 %) | 0.8198 (3.597, 8) |
| 20–39 | 92 | 14(15.8 %) | 34 (36.8 %) | 44(47.4 %) | |
| 40–59 | 295 | 39(13.1 %) | 68(22.9 %) | 188(63.9 %) | |
| 60–79 | 194 | 19(10.0 %) | 58(30.0 %) | 116(60.0 %) | |
| 80–99 | 44 | 10(22.2 %) | 10(22.2 %) | 24(55.6 %) | |
| Gender | |||||
| Male | 243 | 44(18.0 %) | 92(38.0 %) | 107(44.0 %) | 0.0131(8.675, 2) |
| Female | 387 | 39(10.0 %) | 77(20.0 %) | 271(70.0 %) | |
| Marital status | |||||
| Single | 54 | 10(18.2 %) | 29(54.5 %) | 15(27.3 %) | 0.2125 (5.826, 4) |
| Married | 465 | 58(12.5 %) | 112(24.0 %) | 295(63.5 %) | |
| Widowed | 111 | 14(13.0 %) | 29(26.1 %) | 63(56.5 %) | |
| Socioeconomic income | |||||
| None | 615 | 68(11.0 %) | 169(27.6 %) | 378(61.4 %) | 0.0023 (20.41, 6) |
| <500 (low) | 5 | 5(100.0 %) | |||
| 500–1000 (medium) | 5 | 5(100.0 %) | |||
| >1000 (high) | 5 | 5(100.0 %) | |||
| Highest level of education | |||||
| None | 495 | 33(6.6 %) | 114(23.1 %) | 348(70.3 %) | <0.0001 (34.80, 8) |
| Basic | 43 | 9(22.2 %) | 14(33.3 %) | 19(44.4) | |
| JHS | 58 | 19(33.3 %) | 24(41.7 %) | 15(25.0 %) | |
| SHS | 24 | 10(40.0 %) | 14(60.0 %) | ||
| Tertiary | 10 | 10(100.0 %) | |||
| Duration of T2D (years) | |||||
| <5 | 450 | 38 (8.6 %) | 97(21.5 %) | 315(69.9 %) | 0.0076 (17.51, 6) |
| 5–10 | 126 | 24(19.2 %) | 39(30.8 %) | 63(50.0 %) | |
| 10–15 | 39 | 15(37.5 %) | 15(37.5 %) | 9(12.5 %) | |
| 16–20 | 15 | 10(66.7 %) | 5(33.3 %) | ||
| Area of residence | |||||
| Rural | 344 | 29(8.4 %) | 92(26.8 %) | 223(64.8 %) | 0.206 (3.160, 2) |
| Urban | 286 | 53(18.6 %) | 78(27.1 %) | 155(54.2 %) | |
Values are presented as N (%) frequency (percentage), (X2, df) Chi-square, degree of freedom
More males (18.0 %) than female participants (10.0 %) had adequate knowledge on diabetic complications (p = 0.0131). Singles (18.2 %) followed by those widowed (13.0 %) and those who were married (12.5 %) had adequate knowledge on diabetic complications.
Marital status was not significantly associated with the degree of understanding of diabetic complications (p = 0.2125). Participants (100.0 %) who financially earned between 500 and 1000 Ghana cedis had adequate knowledge compared to 11.0 % of patients with no economic income (P =0.0023). All (100.0 %) participants who had completed tertiary education had adequate knowledge followed by those who had completed senior high school (40.0 %), junior high school (33.3 %), basic school (22.0 %) and those who were unschooled (6.8 %) (p <0.0001). The duration of patient’s diabetics was significantly (p = 0.0076) associated with the degree of understanding of diabetic complications. Approximately sixty seven percent (66.7 %) of participants with 16–20 years duration of diabetes had adequate knowledge on diabetic complications than to those with 11–15 year duration (37.5 %), 5–10 year (19.2 %) and below 5 years (8.6 %). There was no significant association between area of residence and the knowledge on diabetic complications (p = 0.2060). However, patients from the urban (18.6 %) had adequate knowledge than their counterparts from the rural settings (8.4 %) [Table 3].
Factors associated with understanding of diabetic complications
Table 4 shows the multivariable logistic regression analysis of level of understanding for diabetic complications. Female gender adjusted odd ratio (AOR) =2.31(1.56–3.40), married participants AOR = 3.37 (1.44–7.93) and widowed participants AOR = 2.98(1.10–8.08) were significantly (p <0.05) associated with increased level of understanding of diabetic complications. Basic educational level AOR = 0.18 (0.082–0.50) JHS and above of educational level AOR = 0.04 (0.02–0.08), 5–9 years of T2D duration AOR = 0.31 (0.18–0.57), ≥10 years of T2D duration AOR = 0.42 (0.20–0.62) and urban dwellers AOR = 0.36 (0.22–0.68) respectively were significantly associated (p <0.05) with reduced level of understanding of diabetic complication [Table 4].
Table 4.
Multivariable Logistic Regression analysis of level of understanding of diabetic complications
| Regression analysis Level of understanding of diabetic complications | |||||
|---|---|---|---|---|---|
| Total | Adequate (n = 82) | Don’t Know(n = 378) | Adjusted OR (95 % CI) | P-Value | |
| Age group (years) | |||||
| <40 | 97 | 14(15.8 %) | 49(50.5 %) | 1 | |
| 40–59 | 295 | 39(13.1 %) | 188(63.9 %) | 1.36(0.68–2.75) | 0.361 |
| Above 60 | 238 | 29(12.18 %) | 140(58.82). | 1.34 (0.67–2.82) | 0.447 |
| Gender | |||||
| Male | 243 | 44(18.0 %) | 107(44.0 %) | 1.00 | |
| Female | 387 | 39(10.0 %) | 271(70.0 %) | 2.31 (1.56–3.41) | <0.0001 |
| Marital status | |||||
| Single | 54 | 10(18.2 %) | 15(27.3 %) | 1.00 | |
| Married | 465 | 58(12.5 %) | 295(63.5 %) | 3.37 (1.44–7.93) | 0.0060 |
| Widowed | 111 | 14(13.0 %) | 63(56.5 %) | 2.98 (1.10–8.08) | 0.0334 |
| Socioeconomic income | |||||
| No income | 615 | 68(11.0 %) | 378(61.4 %) | 1.00 | |
| Yes income | 15 | 15(100.0 %) | – | 0.06 (0.003–0.98) | <0.0001 |
| Highest level of education | |||||
| None | 495 | 33(6.6 %) | 348(70.3 %) | 1.00 | |
| Basic | 43 | 9(22.2 %) | 19(44.4 %) | 0.18(0.082–0.50) | 0.0009 |
| JHS and above | 92 | 39(42.39 %) | 15(16.30.0 %) | 0.04(0.02–0.08) | <0.0001 |
| Duration of T2D (years) | |||||
| <5 | 450 | 38 (8.6 %) | 315(69.9 %) | 1.00 | |
| 5–9 | 126 | 24(19.2 %) | 63(50.0 %) | 0.31 (0.18–0.57) | 0.0002 |
| ≥10 | 50 | 25(37.5 %) | 9(12.5 %) | 0.04 (0.23–0.62) | <0.0001 |
| Area of residence | |||||
| Rural | 344 | 29(8.4 %) | 223(64.8 %) | 1.00 | |
| Urban | 286 | 53(18.6 %) | 155(54.2 %) | 0.36 (0.22–0.68) | 0.0001 |
Values are presented as N (%) frequency (percentage), OR odds ratio, CI confidence interval variables
Discussion
This study aimed to determine the knowledge of complications of diabetes mellitus among diabetic patients visiting the diabetic clinic at the Sampa Government Hospital, Ghana.
In this study, the proportion of complication of type 2 diabetes commonly known by diabetic patients were diabetic foot (51.5 %), hypertension (35.4 %), neuropathy (29.2 %), hypoactive sexual arousal (25.4 %), arousal disorder (21.5 %), retinopathy (17.7 %), heart disease (9.2 %), and nephropathy (5.4 %).
A study conducted by Hoque and colleagues [17] among Indians visiting the Khulna Diabetic Centre, Bangladesh found heart disease (48.9 %) as the most common complication known by diabetic patient followed by cerebrovascular disease (15.2 %), renal disease (13 %), hypertension (5.4 %), and eye diseases (4.9 %) [17]. There was disparity of this study with another study where 53.5 % patients reported that heart disease was a potential complication of diabetes mellitus [19]. Another study observed that only 10 % of diabetic patients knew diabetic foot as a complication of diabetes [20]. Comparably, results of this present study differ from previous studies. The difference in response of patients’ knowledge on diabetic complication in this study compared to previous study may be explained by the difference in the diabetes education. Hoque and colleagues conducted their study among Indians population whiles our present study was among Ghanaian diabetic population. Reports indicate that differences in culture, race, and ethnic background may affect the pattern of knowledge on diabetic complication [21].
Increased response of patients’ knowledge on diabetic foot as the most common complication (Table 2) indicates that majority of participants had experienced this complication. In this study the decreased proportion of patients’ knowledge on heart disease compared previous study could be explained that either the diabetic patients had inadequate knowledge. Results from the present study showed that majority (60.0 %) of T2D patients did not have knowledge on diabetes complications. One hundred and sixty-five (165) of them representing 26.9 % had inadequate knowledge on diabetics complication while only 13.1 % of the sample population (n = 630) had adequate knowledge. Previous study conducted by Kavitha and Aruna, in 2014 among diabetic mellitus patients in India observed that 3.0 % of diabetics had adequate knowledge on acute complication of diabetic mellitus, which is consistent with the present study findings [22]. In another study where knowledge, attitude and practice were assessed among diabetic patients found that about 63.0 % did not know what diabetes and it complications were [23].
This study also observed a significant association between gender and the degree of knowledge for diabetic complications. Male diabetic participants had adequate knowledge of diabetic complications compared to their female counterparts. These results are consistent with the findings of Nisar et al. [24] conducted among diabetics living in Pakistan. Another study conducted in rural Northwest of Pakistan regarding knowledge of diabetes among patients showed that high proportion of males have better understanding of diabetes symptoms, signs and complication as compared to females [21]. These findings are also consistent with findings made by several other authors in a descriptive cross-sectional study [25, 26].
Another interesting finding of this study was the association between levels of education and the degree of patient’s knowledge on diabetic complications. It was observed that patients with tertiary education had significantly higher proportions in terms of adequate knowledge on diabetic complications. The results agrees with findings by Nisar et al., [24] who observed that diabetic patients with higher level of education were associated with greater knowledge of diabetic symptoms, risk factors, complications and presentation [24]. Another study showed that education had a significant role in diabetic awareness to keep correct blood glucose level [17]. These findings are consistent with several other studies among diabetic population [21, 26, 27]. There are no epidemiological studies in Ghana assessing the level of education and knowledge on diabetic complications. The significant association between education especially tertiary education and knowledge on diabetic complications is expected because, patients who had completed tertiary education might have attended workshop, conference, seminar and health talk on health-related issue.
This study also found a significant association between socio-economic income and the level of knowledge on diabetic complication. In this present study, diabetic patients irrespective of low, moderate or high economic income were significantly associated with adequate knowledge on diabetic complication compared to patients without economic income. A higher household income has been found to be associated with adequate knowledge on diabetic complications [28]. Despite the finding of this study Hoque and colleagues [17] observed no significant association between patients’ socioeconomic income and degree of understanding for diabetic complications.
Again, the significant association between knowledge on complication and duration of diabetes cannot be overlooked. This finding is expected because the longer the duration of diabetes the more knowledge patient has on diabetic complication. Longer duration of diabetes development are known factors and shown in numerous studies to be associated with the development and progression of chronic complications in diabetes [20].
A study in Pakistan indicated that type 2 diabetic patients who were urban dwellers were more knowledgeable than their counterparts residing in the rural area [29]. This finding is consistent with the present study finding where about 35.4 % of urban settlers compared to 8.4 % of rural settlers had adequate knowledge on diabetic complication. A similar finding was observed by Hoque, Islam, Khan, Aziz, & Ahasan, [17]. In this study, there was no significant difference in knowledge on diabetic complications between rural and urban dwellers probably because diabetes targeted education was lacking in both the groups. There is the need for urgent diabetic education among participants in these areas.
There are good evidences that foot complications are preventable by appropriate foot care and education programme [30]. In this study diabetic patients have successfully highlighted diabetic foot as the most common complication among diabetes in Sampa Metropolis.
The major limitation of this study was the sampling technique and the low literacy of the people. Their health literacy is likely low and perhaps they did not fully understand the questions and thus the findings of this study cannot conclusively represent the general diabetic patients in the Sampa government Hospital. However, some findings of this study concur well with other previous studies.
Conclusion
In this study, the most common complication of type 2 diabetes known by diabetic patients was diabetic foot, followed by hypertension, neuropathy, hypoactive sexual arousal, arousal disorder, retinopathy, heart disease, and nephropathy. Higher proportion of the T2D patients did not have adequate knowledge on diabetic complications. Male gender, high income earners, higher level of education, and longer duration of T2D were significantly associated with degree of understanding for diabetic complications. It is incumbent on healthcare giver to provide early diabetic education regarding causes, management and preventive measures of diabetic complications. Organizing health education programmes as well as health outreaches on preventives measures such as adjusting to lifestyle and dietary modifications will enhance the level of knowledge of diabetic complications among diabetic patients.
Abbreviations
DM, diabetes mellitus; IFG, impaired fasting glycaemia; IGT, impaired glucose tolerance; T2D, type 2 diabetes
Acknowledgement
Gratitude goes to workers at Diabetic Clinic and authorities of Sampa Government Hospital and Nursing Departments in GCUC and Department of Molecular Medicine, KNUST, Kumasi-Ghana
Funding
No funding was obtained for this research.
Availability of data and materials
Excel sheet of dataset on which conclusions of this manuscript were made has been submitted as an Additional file 1.
Authors’ contributions
YO contributed to the conception of the research idea, design data analysis and interpretation, paper drafting and revision. CO contributed to the conception of the research idea, design, data analysis and interpretation, paper drafting and revision. EOA contributed to the conception of the research idea, design, data collection, data analysis and interpretation, paper drafting and revision. EA contributed to research design, patient recruitment, collection data analysis and interpretation, paper drafting and revision. ADS contributed to research design, patient recruitment and collection. OC contributed to the conception of the research idea, design and data collection. ENB contributed to the conception of the research idea, design, and data collection. PKB contributed to data interpretation, paper drafting and revision. All authors approved the final manuscript before publication and agree to be accountable for all aspects of the work.
Competing interest
The authors declare that they have no competing interest.
Consent for publication
Not Applicable.
Ethics approval and consent to participate
Approval for this study was obtained from the committee on Human Research, Publication and Ethics of the School of Medical Sciences (SMS), Kwame Nkrumah University of Science and Technology (KNUST) as well as ethical review board of the Sampa Government Hospital. Participation was voluntary and verbal informed consent was obtained from each participants. Respondents were assured that the information gathered was to be used strictly for research and academic purpose only. In addition, respondents were given the freedom to opt out any time they think they cannot continue with the study.
Additional file
Data set on which conclusion of this manuscript was based upon. (XLSX 54 kb)
Contributor Information
Yaa Obirikorang, Email: obiriyaa@gmail.com.
Christian Obirikorang, Email: krisobiri@yahoo.com.
Enoch Odame Anto, Email: odameenoch@yahoo.com.
Emmanuel Acheampong, Phone: +233201346591, Email: emmanuelachea1990@yahoo.com.
Emmanuella Nsenbah Batu, Email: batuemmanuella@gmail.com.
Agyemang Duah Stella, Email: stellaagyemanduah@yahoo.com.
Omerige Constance, Email: constanceomerige@gmail.com.
Peter Kojo Brenya, Email: brenya.peter@yahoo.com.
References
- 1.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 2.Hjelm K, Mufunda E, Nambozi G, Kemp J. Preparing nurses to face the pandemic of diabetes mellitus: a literature review. J Adv Nurs. 2003;41(5):424–434. doi: 10.1046/j.1365-2648.2003.02548.x. [DOI] [PubMed] [Google Scholar]
- 3.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Bisiriyu GA. Non-adherence to lifestyle modifications (Diet and exercise) amongst type 2 diabetes mellitus patients attending extension II clinics in Gaborone. Botswana: University of Limpopo (Medunsa Campus); 2010. [Google Scholar]
- 5.Aikins A-G. Ghana’s neglected chronic disease epidemic: a developmental challenge. Ghana Med J. 2007;41(4):154. [PMC free article] [PubMed] [Google Scholar]
- 6.Cook-Huynh M, Ansong D, Christine Steckelberg R, Boakye I, Seligman K, Appiah L, Kumar N, Amuasi JH. Prevalence of hypertension and diabetes mellitus in adults from a rural community in Ghana. Ethn Dis. 2012;22(3):347. [PubMed] [Google Scholar]
- 7.Control CfD, Prevention, Control CfD, Prevention . National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. p. 201. [Google Scholar]
- 8.Murugesan N, Snehalatha C, Shobhana R, Roglic G, Ramachandran A. Awareness about diabetes and its complications in the general and diabetic population in a city in southern India. Diabetes Res Clin Pract. 2007;77(3):433–37. [DOI] [PubMed]
- 9.Kengne AP, Amoah AG, Mbanya J-C. Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation. 2005;112(23):3592–3601. doi: 10.1161/CIRCULATIONAHA.105.544312. [DOI] [PubMed] [Google Scholar]
- 10.Boulton AJ, Kirsner RS, Vileikyte L. Neuropathic diabetic foot ulcers. N Engl J Med. 2004;351(1):48–55. doi: 10.1056/NEJMcp032966. [DOI] [PubMed] [Google Scholar]
- 11.Hall V, Thomsen RW, Henriksen O, Lohse N. Diabetes in Sub Saharan Africa 1999–2011: epidemiology and public health implications. A systematic review. BMC Public Health. 2011;11(1):564. doi: 10.1186/1471-2458-11-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desalu O, Salawu F, Jimoh A, Adekoya A, Busari O, Olokoba A. Diabetic foot care: self reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. 2011;45(2):60–5. doi: 10.4314/gmj.v45i2.68930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aikins A-G. Healer shopping in Africa: new evidence from rural-urban qualitative study of Ghanaian diabetes experiences. BMJ. 2005;331(7519):737. doi: 10.1136/bmj.331.7519.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doherty ML, Owusu-Dabo E, Kantanka OS, Brawer RO, Plumb JD. Type 2 diabetes in a rapidly urbanizing region of Ghana, West Africa: a qualitative study of dietary preferences, knowledge and practices. BMC Public Health. 2014;14(1):1. doi: 10.1186/1471-2458-14-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.International Diabetes Federation (IDF) Global Guidelines Development. Global guideline for type 2 diabetes. Diabetes research and clinical practice. 2014;104(1):1.
- 16.Sorganvi V, Devarmani S, Angadi M, Udgiri R. Knowledge and its complications of diabetes amongst the known diabetic patients–a hospital based study. Int J Cur Res Rev. 2013;5(22):100–104. [Google Scholar]
- 17.Hoque MA, Islam MS, Khan MAM, Ahasan HN. Knowledge of diabetic complications in a diabetic population. J Med. 2009;10(2):90–93. doi: 10.3329/jom.v10i2.2821. [DOI] [Google Scholar]
- 18.Filip R, Lewandowska A, Szczepankiewicz M, Majda B. State of patients’ knowledge about treatment and proceedings in type 2 diabetes. Ann Agric Environ Med. 2014;21(2). [DOI] [PubMed]
- 19.O’Sullivan E, Bhargava A, O’Callaghan M, Buckley U, De Faoite T, Moynihan K, Thabit H, Walsh C, Sreenan S. Awareness of diabetes complications in an Irish population. Ir J Med Sci. 2009;178(4):401–406. doi: 10.1007/s11845-009-0301-0. [DOI] [PubMed] [Google Scholar]
- 20.Kavitha M, Aruna S. Knowledge on complications of diabetes mellitus among patients with diabetes mellitus – a descriptive study. International Journal Comprehensive Nursing. 2014;1(1):18–20.
- 21.Hawthorne K, Tomlinson S. Pakistani moslems with Type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self‐monitoring management and glycaemic control. Diabet Med. 1999;16(7):591–597. doi: 10.1046/j.1464-5491.1999.00102.x. [DOI] [PubMed] [Google Scholar]
- 22.Kavitha M, Aruna S. Knowledge on complications of diabetes mellitus among patients with diabetes mellitus – a descriptive study. Int J Compr Nurs. 2014;1(1):18–20. [Google Scholar]
- 23.Shah VN, Kamdar P, Shah N. Assessing the knowledge, attitudes and practice of type 2 diabetes among patients of Saurashtra region, Gujarat. Int J Diabetes Dev Ctries. 2009;29(3):118. doi: 10.4103/0973-3930.54288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nisar N, Khan IA, Qadri MH, Sher SA. Knowledge and risk assessment of diabetes mellitus at primary care level: a preventive approach required combating the disease in a developing country. Pak J Med Sci. 2008;24(5):667–672. [Google Scholar]
- 25.Gulabani M, John M, Isaac R. Knowledge of diabetes, its treatment and complications amongst diabetic patients in a tertiary care hospital. Indian J Community Med. 2008;33(3):204. doi: 10.4103/0970-0218.42068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehrotra R, Bajaj S, Kumar D, Singh K. Influence of education and occupation on knowledge about diabetes control. Natl Med J India. 1999;13(6):293–296. [PubMed] [Google Scholar]
- 27.Khamseh ME, Vatankhah N, Baradaran HR. Knowledge and practice of foot care in Iranian people with type 2 diabetes. Int Wound J. 2007;4(4):298–302. doi: 10.1111/j.1742-481X.2007.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al Shafaee MA, Al-Shukaili S, Rizvi SG, Al Farsi Y, Khan MA, Ganguly SS, Afifi M, Al Adawi S. Knowledge and perceptions of diabetes in a semi-urban Omani population. BMC Public Health. 2008;8(1):249. doi: 10.1186/1471-2458-8-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sabri AA, Qayyum MA, Saigol NU, Zafar K, Aslam F. Comparing knowledge of diabetes mellitus among rural and urban diabetics. McGill J Med. 2007;10(2):87. [PMC free article] [PubMed] [Google Scholar]
- 30.Dorresteijn JA, Valk GD. Patient education for preventing diabetic foot ulceration. Diabetes Metab Res Rev. 2012;28(S1):101–106. doi: 10.1002/dmrr.2237. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Excel sheet of dataset on which conclusions of this manuscript were made has been submitted as an Additional file 1.


