Abstract
Background:
The association between neurofibromatosis type 1 (NF-I) and Chiari I malformation (CMI) is rare, and not many studies are reported in the literature. Performing magnetic resonance imaging (MRI) in patients with NF-1 is essential because several cases of Chiari type I are completely asymptomatic. We emphasize the need for inclusion of Chiari I as diagnosis in association with NF-1.
Case Description:
The patient was a 51-year-old black man who presented with complaints of pain and decreased motion and sensibility of his hands, wrists, and forearms, along with progressive dysarthria. Even though the computed tomography (CT) scan of the skull did not show changes, the MRI showed hydro/syringomyelia in the cervical spine area. Midline suboccipital craniectomy with total laminectomy of c1 and partial laminectomy of c2 was performed; tonsillectomy was also performed for cistern expansion because of intense thickening and obliteration of the obex by the cerebellar tonsils. Following treatment, the patient showed remission of symptoms.
Conclusion:
NF-1 in association with CMI is rare, and early diagnosis and surgical treatment are essential to slow down the myelopathy; although they prevent neurological damages, patients with NF-1 must remain under doctor's attention in case of association with CMI. Our literature review showed that symptoms can vary and include headache, gait disturbance, and sensory/motor diminution, until asymptomatic patients. Moreover, the incidence of NF-1 is considerably higher in CMI patients in comparison to the global incidence (8.6–11.8% and 0.775%, respectively). The surgical technique must be evaluated case by case according to the degree of cerebrospinal fluid obstruction.
Keywords: Chiari 1 malformation, neurofibromatosis type 1, syringomyelia
INTRODUCTION
Neurofibromatosis type 1 (NF-1) or Von Recklinghausen's disease is one of the most common neurocutaneous disorders well-known to cause skin lesions (mainly tumors, cafe-au-lait spots, and a wide variety of brain dysplasia) in affected patients.[4,5,7,11,15] Individuals with the disease have a higher prevalence of learning deficit, even though cognitive dysfunctions are not well established.[1] The pathophysiology of NF-1 involves mutations in the gene of NF-1 located on the long arm of the chromosome 17, which changes neurofibromine, a protein that acts as a tumor suppressor. NF-1 is an autosomal dominant disease with complete penetrance, which can affect both men and women.[3,9]
Chiari I malformation (CMI) causes herniation of the cerebellar tonsils through the foramen magnum, generating diverse clinical conditions, which are usually complicated by syringomyelia.[7,15] By definition, CMI is the caudal displacement of the cerebellum with tonsillar herniation above 5 mm below the foramen magnum in magnetic resonance imaging (MRI), in addition to tonsil stretch in the shape of a pin. However, there are symptomatic patients with less than 5 mm and patients without any clinical symptoms despite herniation more than 5 mm.[14,15]
Several theories attempt to explain the origin of the Chiari's malformations such as the hindbrain dysgenesis, development arrest, caudal traction, hydrocephalus theory/Gardner theory, small posterior fossa, and lack of embryologic ventricular distention theories. Probably, the pathophysiology of CMI and Chiari's Malformation type II (CMII) are different, but with the same impaired cerebral spinal fluid (CSF) impairment flow through the foramen magnum.[13] CMI can be acquired or congenital, the former is caused by a mesodermal defect, which creates a small posterior fossa and consequently compression and herniation of neural components.[13] Moreover, it can be associated with other craniovertebral abnormalities and syndromes such as the Crouzon's syndrome. In addition, other medical conditions can cause posterior fossa impairment such as familial vitamin-D resistant rickets and growth hormone deficiency.[13] Acquired CMI can be due to lumboperitoneal shunts, CSF leaks, lumbar drainage, and repetitive iatrogenic punctions.[13] The frequency of this correlation is quite rare and it depends on the MRI findings of patients with NF-1 because several cases of Chiari type 1 are completely asymptomatic. We emphasize the need for inclusion of Chiari 1 as a diagnosis in association with NF-1.
CASE PRESENTATION
The patient was a 51-year-old black man who was previously diagnosed with NF-1, however, there was no history of cutaneous biopsy performed earlier. He sought medical attention in July 2014 with complaints of pain and decreased motion and sensation of hands, wrists, and forearms, in addition to difficulty in articulating words. Upon first checkup, the patient had several cafe-au-lait spots in variable sizes, larger than 15 mm, and several neurofibromas, in particular on his thorax, arms, and face [Figure 1]. The neurological examination showed bilateral decreased thermal-tenderness around the shoulders, arms, and hands with right predominance, dysmetry1 in proof of index-nose on the left side, and decreased surface sensitivity in his left side of the face. In addition, the patient had bilateral distal strength diminution in the hands and forearm and hyperreflexive reflex in the arms and legs. Although there were no changes in the CT of the skull, the MRI showed hydro/syringomyelia in the cervical spine area [Figure 2]. In this case, the patient went to a subocciptal craniectomy with duroplasty and partial laminectomy of c2, along with tonsillectomy and expansion of cistern magna due to intense arachnoid thickening and obliteration of the obex by the cerebellar tonsils [Figure 3]. The patient had good recovery after the surgery and achieved the main goal of interruption the progression of the condition and improvement of the symptoms. The histology confirmed neurofibromas [Figure 4].
Figure 1.

From left to right: Café-au-lait spot in the right upper limb; neurofibromatosis multiple nodules in the lumbar region; neurofibromatosis nodules in the abdomen
Figure 2.
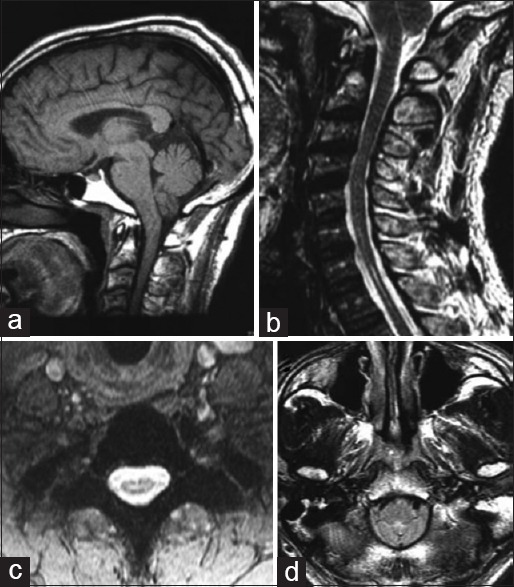
(a) Sagittal section: Herniation of the cerebellar tonsils of 4 mm; (b) Sagittal section: signs of cervical- thoracic syringomyelia; (c) axial section: Spinal cord syringomyelia; (d) axial section: Tonsillar herniation
Figure 3.

Surgical incision: Occipital craniotomy
Figure 4.
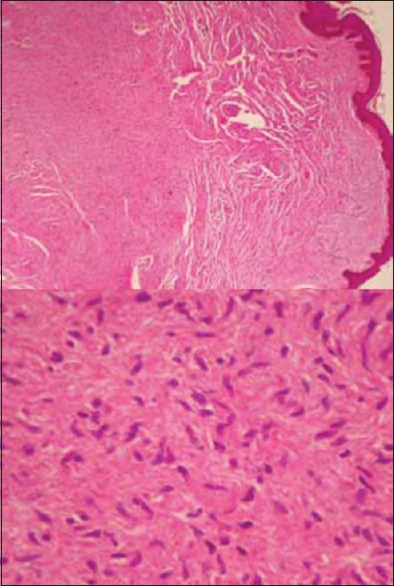
Histology: Hematoxylin-and-eosin stained sections show a dermal proliferation of spindle cells with wavy nuclei and inconspicuous nucleoli; presence of neurofibromas confirms the diagnosis
DISCUSSION
NF-1 is the most common neurocutaneous syndrome characterized by various cutaneous stigma associated with neurological manifestations and a greater susceptibility to tumors.[4,7,11] The association between NF-1 and CMI is rare with an incidence of approximately 1 case in 166,500,00 to 247,900,00 people.[11] CMI can be asymptomatic in up to 8% of patients with NF-1; the most common symptoms are pain/cluster headache 69%, syringomyelia 30%, sensitivity disorders, and hypostesia in mantle. It may also be associated with scoliosis 30%.[1,6]
The patient mentioned in this study had the central cord syndrome, a condition that affects neurons in the gray matter and spinothalamic tract, causing loss of motion and sensation in arms and hands. It can also cause segmental weakness and signs of long tract (upper motor neuron lesion). The paralysis of the lower cranial nerves occurs in 11% of cases (in this case, accessory nerve and hypoglossal nerve).[6]
The real incidence of CMI is not known, but a study of general population who underwent brain MRI showed that, in 22591 patients, approximately 175 (0.775%) presented tonsilar herniation greater than 5 mm.[13]
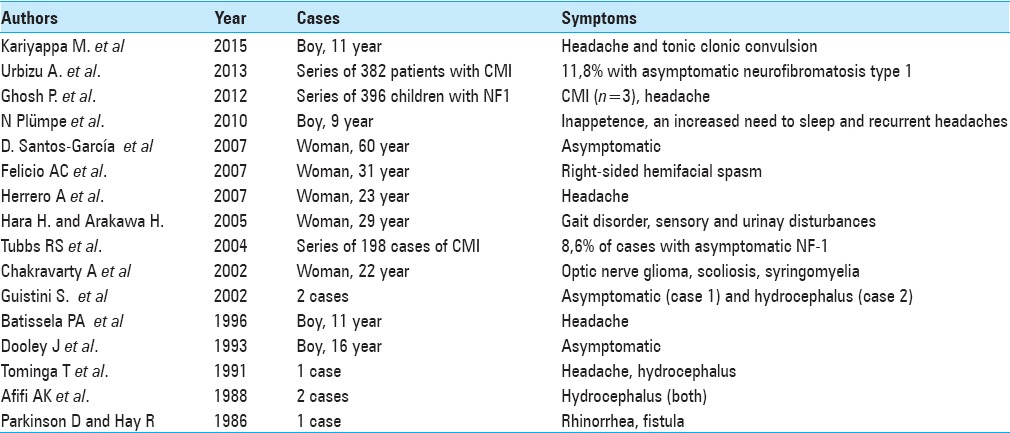
In the literature review, approximately 80 patients of both diseases were analyzed. Approximately 80% of the patients were asymptomatic, 9% only had cluster headache, and the others had various health problems such as facial spasms, tonic–clonic seizures, urinary disturbances, and sleep disorders. In the review, precocity of symptoms in males (children and teenagers mostly) was noticed compared to females (predominance in young adults)[16] Further, Tubbs et al.[14] and Urbizu et al.[15] who presented two large series CMI, showed a coexistence between the two syndromes to be about 8.6–11.8%, almost 14 times higher than the general population. This information suggests a correlation between the origin of both syndromes, however, no research has proven the possible mechanisms [Table 1]. Surgical decompression techniques can be divided into two less invasive subtypes, namely, craniocervical decompression and duroplastia without opening of the arachnoid membrane or decompression by the removal of the posterior edge bone of the foramen magnum and laminectomy of c1 and c2, though optional. In this case, midline occipital craniectomy with laminectomy of c1 and partial laminectomy of c2 was performed, along with tonsillectomy and expansion of cistern magna because of intense thickening and obliteration of the obex by the cerebellar tonsils. The patient had good recovery after the surgery and achieved the main goal of interruption the progression of the condition and improvement of the symptoms [Figures 2 and 4].
Table 1.
Cases or case series of Arnold Chiari Malformation type 1 associated with neurofibromatosis type 1 reported in the literature
CONCLUSION
NF-1 in combination with CMI is rare and early diagnosis and surgical treatment are essential to slow down myelopathy as well as to prevent neurological damages. Patients with NF-1 must remain under doctor's attention in case of association with CMI. Asymptomatic patients can be monitored and operated if they become symptomatic. In patients with recommendation of surgery, the surgical technique must be evaluated case by case according to the degree of CSF obstruction and the associated clinical condition.[2,10,12] Thus, the moment of CMI action could be questioned because there is no preventive surgery. However, symptomatic patients with syringomyelia benefit from early surgical intervention, even if it is not preventive.[8] Although the association between NF-1 and CMI is rare, if the basic pathology does not correlate with the expected natural history, further investigation should be done. If presented with progressive disease, early approach is essential to achieve a better prognosis. Further studies could possibly show the correlation between the two syndromes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Marianne Pozetti, Email: mari.pozetti@yahoo.com.br.
Telmo Augusto Barba Belsuzarri, Email: telmobelsuzarri@hotmail.com.
Natalia C. B. Belsuzarri, Email: nbelsuzarri@hotmail.com.
Naira B. Seixas, Email: na.bs@hotmail.com.
João F. M. Araujo, Email: jflavioaraujo@terra.com.br.
REFERENCES
- 1.Acosta MT, Walsh KS, Kardel PG, Kutteruf RE, Bhatt RR, Bouton TC, et al. Cognitive profiles of neurofibromatosis type 1 patients with minor brain malformations. Pediatr Neurol. 2012;46:231–4. doi: 10.1016/j.pediatrneurol.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis type I in children. Neurosurg Focus. 2006;20:E2. [PubMed] [Google Scholar]
- 3.Ars E, Kruyer H, Morell M, Pros E, Serra E, Ravella A, et al. Recurrent mutations in the NF1 gene are common among neurofibromatosis type 1 patients. J Med Genet. 2003;40:e82. doi: 10.1136/jmg.40.6.e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Battistella PA, Perilongo G, Carollo C. Neurofibromatosis type 1 and type I Chiari malformation: An unusual association. Childs Nerv Syst. 1996;12:336–8. doi: 10.1007/BF00301023. [DOI] [PubMed] [Google Scholar]
- 5.Boyd KP, Korf BR, Theos A. Neurofibromatosis type 1. J Am Acad Dermatol. 2009;61:1–16. doi: 10.1016/j.jaad.2008.12.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Felício AC, Godeiro-Junior CO, Borges V, Silva SMA, Ferraz HB. Hemifacial Spasm in a patient with neurofibromatosis and Arnold-Chiari malformation. Arq Neuropsiquiatr. 2007;65:855–7. doi: 10.1590/s0004-282x2007000500026. [DOI] [PubMed] [Google Scholar]
- 7.Hara H, Arakawa H. Coexistence of neurofibromatosis 1 and Chiari type I malformation: An unusual association. J Dermatol. 2005;32:34–7. doi: 10.1111/j.1346-8138.2005.tb00711.x. [DOI] [PubMed] [Google Scholar]
- 8.Incecık F, Ozlem HM, Altunbasak S. Optic pathway glioma, scoliosis, Chiari type 1 malformation, and syringomyelia in a patient with neurofibromatosis type 1. J Neurosci Rural Pract. 2013;4:141–3. doi: 10.4103/0976-3147.116473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korf BR, Schneider G, Poussaint TY. Structural anomalies revealed by neuroimaging studies in the brains of patients with neurofibromatosis type 1 and large deletions. Genet Med. 1999;1:136–40. doi: 10.1097/00125817-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Loukas M, Shayota BJ, Oelhafen K, Miller JH, Chern JJ, Tubbs RS, et al. Associated disorders of Chiari Type I malformations: A review. Neurosurg Focus. 2011;31:E3. doi: 10.3171/2011.6.FOCUS11112. [DOI] [PubMed] [Google Scholar]
- 11.Santos-García D, Cabanillas M, Suárez-Dono I, Monteagudo B, Fuente-Fernández RDL, Suárez-Amor O. Neurofibromatosis type 1 and Arnold-Chiari malformation. Actas Dermosifiliogr. 2009;100:817–32. doi: 10.1016/s0001-7310(09)72559-1. [DOI] [PubMed] [Google Scholar]
- 12.Tubbs RS, Beckman J, Naftel RP, Chern JJ, Wellons JC, 3rd, Rozzelle CJ, et al. Institutional experience with 500 cases of surgically treated pediatric Chiari malformation Type I. J Neurosurg Pediatr. 2011;7:248–56. doi: 10.3171/2010.12.PEDS10379. [DOI] [PubMed] [Google Scholar]
- 13.Tubbs RS, Pugh JA, Oakes WJ. Youmans Neurological Sugery. 6th edition. II. Philadelphia: Elsevier Saunders; 2011. Chiari Malformations; pp. 1918–27. [Google Scholar]
- 14.Tubbs RS, Rutledge SL, Kosentka A, Bartolucci AA, Oakes WJ. Chiari I malformation and neurofibromatosis type 1. Pediatr Neurol. 2004;30:278–80. doi: 10.1016/j.pediatrneurol.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Urbizu A, Toma C, Poca MA, Sahuquillo J, Cuenca-León E, Cormand B, et al. Chiari Malformation Type I: A Case-Control Association Study of 58 Developmental Genes. PLoS One. 2013;8:e57241. doi: 10.1371/journal.pone.0057241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitehouse D. Diagnostic Value of the Café-au-lait Spot in Children. Arch Dis Child. 1966;41:316–9. doi: 10.1136/adc.41.217.316. [DOI] [PMC free article] [PubMed] [Google Scholar]


