Abstract
Context:
Diagnosis of congenital Bochdalek's hernia (BH) in adulthood is extremely rare and requires a fastidious surgical repair, the failure of which might result in a recurrence with severe complications. We report a rare case of a giant, right BH that recurred after surgical repair and was complicated with complete bowel obstruction.
Case Report:
A 51-year-old Saudi male, with past surgical history of laparotomy that failed to repair BH, presented to the emergency room with severe abdominal pain, vomiting, and hypovolemic shock. Computerized tomography (CT) showed an unusual picture of closed-loop bowel obstruction above and below the diaphragm. We carried out laparotomy and thoracotomy that achieved lysis of adhesions, reduction of bowel, and repair of diaphragmatic defect.
Conclusion:
Acute presentation of complicated BH poses a formidable challenge because of its rarity and complexity. The preferred approach for elective repair of adult BH is debatable, where surgeons—guided by hernia type and biased by their experience—recommend either laparotomy or thoracotomy. Nevertheless, a complicated, giant, recurrent BH typically requires both laparotomy and thoracotomy.
Keywords: Bowel obstruction, congenital Bochdalek hernia, laparotomy, recurrent, thoracotomy
Introduction
Congenital right Bochdalek hernia (BH) in adults is very rare, typically asymptomatic, and incidental. Congenital BH arises when embryonic communication between pleural and peritoneal compartments persists. The right diaphragmatic anlage fuses earlier than the left, and the liver protects the right diaphragm from herniation, which explains why right BH is very rare.[1] A review of 13138 [computerized tomography (CT)] reports documented an incidence of asymptomatic BH of 0.17%.[2] Approximately 200 cases of BH[3] and fewer than 20 cases of right BH have been reported in adults.[4] We report a rare case of recurrent, right BH that presented with acute bowel obstruction and required urgent laparotomy and thoracotomy.
Case Presentation
A 51-year-old Saudi man, with no history of trauma, misdiagnosed as eventration of diaphragm for 20 years, reported to the clinic with abdominal bloating and intermittent dyspnea. CT revealed large right BH that contained stomach, pancreas, mesenteric fat, hepatic flexure, and transverse colon. The patient underwent elective laparotomy that started with mobilization of the left lobe of the liver to the left hepatic vein. The small and large bowel were reduced into the abdomen and the hernia sac was partially excised. The surgeon identified a hiatal hernia, approximated the diaphragmatic crura, and created a partial fundoplication. No other diaphragmatic defect was detected. The postoperative course was complicated by pulmonary sepsis, fever, and leukocytosis. Nine days postoperatively, thoracic and abdominal CT showed no change in size, site, or contents of BH, which implied failure of surgical repair. For the next 2 years, the patient complained of intermittent dyspnea and recurrent chest infections. Chest X-ray showed massive herniation of the stomach and bowel into the thoracic cavity [Figure 1]. The patient was referred for surgery in another hospital. However, patient habitually failed to show up for his appointments despite repeated reminders and rescheduling. Eventually, the patient presented to the emergency room in hypovolemic shock with severe abdominal pain, retching, and vomiting. After the patient's resuscitation, a thoracoabdominal CT was obtained. A giant BH with mediastinal shift to the left was evident [Figure 2]. The small bowel showed a high-grade closed loop obstruction at two sites above and below the diaphragm. The duodenojejunal flexure was incarcerated in the chest and obstructed with adhesions; the jejunoileal junction was obstructed with adhesions in the abdomen [Figure 3]. Hepatic flexure and transverse colon were incarcerated in the right chest [Figure 4]. Emergency laparotomy was performed which was followed by right anterolateral thoracotomy. Laparotomy confirmed the incarceration of small and large bowel in the chest and the adhesive obstruction in the abdomen. After the lysis of adhesions, we could not reduce the bowel safely or delineate the diaphragmatic defect adequately. Therefore, we proceeded with right anterolateral thoracotomy that facilitated lysis of adhesions in the chest, resection of hernia sac, release of entrapped right lower lobe, and reduction of bowel into the abdomen. Tenuous flimsy tissue at the rim of the diaphragmatic defect was debrided. Tension-free primary approximation was accomplished with nonabsorbable suture and reinforced with polytetrafluoroethylene mesh. The patient recovered well and was discharged home 8 days postoperatively. He remains clinically and radiologically free from hernia recurrence 1 year later.
Figure 1.
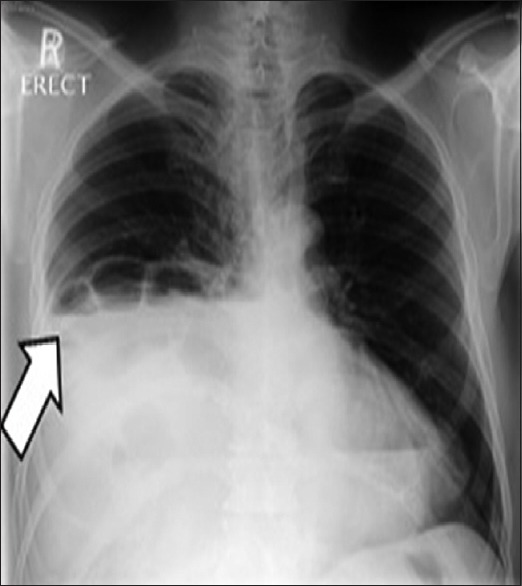
Chest X-ray demonstrates herniated loops of small and large bowel. Arrow shows dilated bowel with air-fluid levels
Figure 2.

Computerized tomography scan shows the right posterior thoracic cavity filled with bowel loops and a mediastinal shift to the left
Figure 3.

Computerized tomography scan shows dilated small bowel loops and a mediastinal shift to the left
Figure 4.

The superior mesenteric vein flipped into the thorax with the herniated small bowel and colon
Discussion
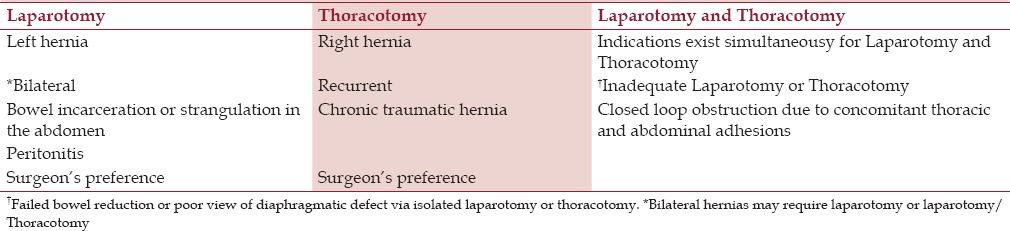
Adult diaphragmatic hernia without a previous history of trauma is very rare.[5] Right BH in an adult that contains colon and bowel is extremely rare.[6] Acute presentation of giant, recurrent, right BH poses a formidable challenge because of its rarity and complexity. Upon diagnosis of BH recurrence, our patient was referred for early, elective repair at another center, however, he repeatedly failed to show up for his appointments. Vigilant follow-up and early effective repair are required to prevent life-threatening complications that may arise from BH recurrence. Our case illustrates a giant BH that recurred after laparotomy that failed to demarcate all boundaries of a diaphragmatic defect hidden from view by the liver. The approximation of native diaphragmatic tissue under tension could have played a role in recurrence. As a result, BH repair was unsuccessful and complicated with pulmonary sepsis in the early postoperative period. Dense adhesions, which is a known sequel of abdominal surgery, triggered mechanical bowel obstruction. To prevent recurrence of giant, right BH hernias, where most of the abdominal viscera have shifted into the chest, thoracoabdominal approach is required to achieve lysis of adhesions, reduce the bowel, and facilitate meticulous repair of diaphragmatic defect. Giant BH most likely requires prosthetic mesh to ascertain sturdy repair with no tension. Pulmonary hygiene protocol, deep breathing, and coughing are of utmost importance in the early postoperative period to combat atelectasis and pulmonary sepsis. There is no consensus on the best surgical approach to repair BH. Some surgical authors favor thoracic or thoracoabdominal approach for BH that are right sided, recurrent, or traumatic [Table 1].[1] The selection of surgical approach could be biased by the surgeon's experience and training.[7] Myriad factors in our case warranted laparotomy and thoracotomy including chronicity, recurrence, right-sidedness, massive herniation of abdominal viscera, and incarceration and adhesions above and below the diaphragm. Thoracotomy facilitates the assessment of diaphragmatic defect unencumbered by intervening organs and simplifies lysis of adhesions between abdominal viscera, pleura, and pericardium. In contrast, laparotomy allows inspection of abdominal viscera, rules out malrotation, reduces hernia contents to their abdominal domicile, and facilitates repair of hernia sac.[2] A key advantage of laparotomy is the ability to view both diaphragmatic spaces simultaneously. Dissection of hernia sac reduces hernia recurrence and seroma formation, however, many surgeons leave the hernia sac in situ to avoid injury to the pleura and other thoracic viscera. The last few years have witnessed a surge of minimal access repairs of BH via laparoscopic or thoracoscopic approach. Compared to open repair, minimal access surgery is associated with less mortality, reduced postoperative ventilation and length of stay but longer operative time. Patients resume enteral nutrition earlier than open repair. The need of conversion in minimal access surgery varied widely from 3.4 to 75%.[8] Command of advanced laparoscopic skills, refinement of instruments, and enhancement of visualization have inspired surgeons to repair complex BH cases via minimal access. Nevertheless, we doubt that laparoscopic surgery is ideal for the repair of a giant, recurrent, incarcerated BH that is complicated with bowel obstruction above and below the diaphragm. The diaphragmatic defect varies but the total absence of diaphragm is rare.[9] Repair of diaphragmatic hernia must achieve good muscle apposition with or without pledgets—free from tension and contamination—and must obliterate dead space. When the diaphragmatic muscle is not robust or primary approximation of large defect is not possible without tension, surgeons resort to prosthetic patch or flap transfer. However, prosthetic repair should be abandoned in contaminated or infected cases because of its association with respiratory and infectious complications.[3] The prosthesis of choice is polytetrafluorethylene owing to its non-adhesive property and resilience against mechanical stress.[2]
Table 1.
Recommended Surgical Approaches for different types of Bochdalek’s Hernia
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors wish to thank Nashwah H. Massloom and Lara H. Massloom for their technical support during the manuscript production.
References
- 1.Bianchi E, Mancini P, De Vito S, Pompili E, Taurone S, Guerrisi I, et al. Congenital asymptomatic diaphragmatic hernias in adults: A case series. J Med Case Rep. 2013;7:125–32. doi: 10.1186/1752-1947-7-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toydemir T, Akıncı H, Tekinel M, Süleyman E, Acunaş B, Ali Yerde M. Laparoscopic repair of an incarcerated bochdalek hernia in an elderly man. Clinics. 2012;67:199–201. doi: 10.6061/clinics/2012(02)20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Watanabe M, Ishibashi O, Watanabe M, Kondo T, Ohkohchi N. Complicated adult right-sided Bochdalek hernia with Chilaiditi's syndrome: A case report. Surg Case Rep. 2015;1:95–9. doi: 10.1186/s40792-015-0100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: A case report. J Med Case Rep. 2009;3:9291. doi: 10.1186/1752-1947-3-9291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurt A, Yazıcıoğlu KR, İpek A, Tosun Ö, Coşkun M. Right sided diaphragmatic hernia in an adult without history of trauma: Unusual CT findings. Eur J Gen Med. 2004;1:55–7. [Google Scholar]
- 6.Slesser A, Ribbans H, Blunt D, Stanbridge R, Buchanan G. A spontaneous adult right-sided Bochdalek hernia containing perforated colon. J R Soc Med. 2011;2:54–9. doi: 10.1258/shorts.2011.011056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsao K, Lally P, Lally K. Minimally invasive repair of congenital diaphragmatic hernia. J Pediatr Surg. 2011;46:1158–64. doi: 10.1016/j.jpedsurg.2011.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vijfhuize S, Deden AC, Costerus SA, Sloots CE, Wijnen RM. Minimal access surgery for repair of congenital diaphragmatic hernia: Is it advantageous. An open review? Eur J Pediatr Surg. 2012;22:364–73. doi: 10.1055/s-0032-1329532. [DOI] [PubMed] [Google Scholar]
- 9.Sathyanarayana N, Rao R, Shivaprasada R. An adult recurrent diaphragmatic hernia with a near complete defect: A rare scenario. J Clin Diagn Res. 2012;6:1574–6. doi: 10.7860/JCDR/2012/4314.2567. [DOI] [PMC free article] [PubMed] [Google Scholar]


